Moisture-Resistant Co-Spray-Dried Netilmicin with l-Leucine as Dry Powder Inhalation for the Treatment of Respiratory Infections
Abstract
:1. Introduction
2. Materials and Methods
2.1. Materials
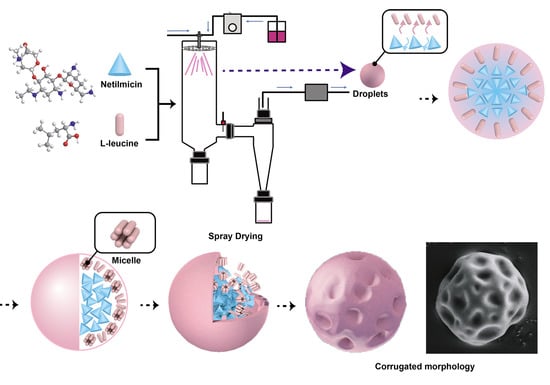
2.2. Preparation of NTM DPIs by Spray-Drying
2.3. Particle Size of NTM DPIs
2.4. Bulk Density and Tap Density
2.5. Scanning Electron Microscopy (SEM)
2.6. Powder X-ray Diffraction (PXRD)
2.7. Water Content Measurement
2.8. Hygroscopicity Investigation
2.9. Antibacterial Assay of NTM DPIs
2.10. Qualification by HPLC
2.11. In Vitro Aerosolization Performance Examination
2.12. Stability Under Accelerated Conditions
2.13. Statistical Analysis
3. Results and Discussion
3.1. Particle Size of NTM DPIs
3.2. Bulk Density and Tap Density
3.3. Scanning Electron Microscopy (SEM)
3.4. Powder X-ray Diffraction (PXRD)
3.5. Water Content and Hygroscopicity Test
3.6. Antibacterial Assay of NTM DPIs
3.7. In Vitro Aerosolization Performance Examination
3.8. Stability under Accelerated Conditions
4. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Parlati, C.; Colombo, P.; Buttini, F. Pulmonary Spray Dried Powders of Tobramycin Containing Sodium Stearate to Improve Aerosolization Efficiency. Pharm. Res. 2009, 26, 1084–1092. [Google Scholar] [CrossRef] [PubMed]
- Zhou, Q.; Gengenbach, T.; Denman, J.A. Synergistic Antibiotic Combination Powders of Colistin and Rifampicin Provide High Aerosolization Efficiency and Moisture Protection. AAPS J. 2014, 16, 37–47. [Google Scholar] [CrossRef] [PubMed]
- Fu, K.P.; Neu, H.C. In vitro study of netilmicin compared with other aminoglycosides. Antimicrob. Agents Chemother. 1976, 10, 526–534. [Google Scholar] [CrossRef] [PubMed]
- Snydman, D.R.; Tally, F.P.; Landesman, S.H. Netilmicin in gram-negative bacterial infections. Antimicrob. Agents Chemother. 1979, 15, 50–54. [Google Scholar] [CrossRef] [PubMed]
- Decker, B.S.; Molitoris, B.A. 14.12–Aminoglycoside-Induced Nephrotoxicity. Compr. Toxicol. 2018, 14, 256–273. [Google Scholar]
- Lindert, S.; Below, A.; Breitkreutz, J. Performance of Dry Powder Inhalers with Single Dosed Capsules in Preschool Children and Adults Using Improved Upper Airway Models. Pharmaceutics 2014, 6, 36–51. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Muralidharan, P.; Mallory, E.; Malapit, M. Inhalable PEGylated Phospholipid Nanocarriers and PEGylated Therapeutics for Respiratory Delivery as Aerosolized Colloidal Dispersions and Dry Powder Inhalers. Pharmaceutics 2014, 6, 333–353. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Huang, Z.W.; Wu, H.; Yang, B.B. Anhydrous reverse micelle nanoparticles: New strategy to overcome sedimentation instability of peptide-containing pressurized metered-dose inhalers. Drug Deliv. 2017, 24, 527–538. [Google Scholar] [CrossRef] [PubMed]
- Mam, M.; Tucker, I.G.; Doyle, C.S. Co-spray drying of hygroscopic kanamycin with the hydrophobic drug rifampicin to improve the aerosolization of kanamycin powder for treating respiratory infections. Int. J. Pharm. 2018, 541, 26–36. [Google Scholar]
- Okuda, T.; Suzuki, Y.; Kobayashi, Y. Development of Biodegradable Polycation-Based Inhalable Dry Gene Powders by Spray Freeze Drying. Pharmaceutics 2015, 7, 233–254. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Li, L.; Ssy, L.; Gengenbach, T. Investigation of l-leucine in reducing the moisture-induced deterioration of spray-dried salbutamol sulfate power for inhalation. Int. J. Pharm. 2017, 530, 30–39. [Google Scholar] [CrossRef] [PubMed]
- Mwesigwa, E.; Basit, A.W. An investigation into moisture barrier film coating efficacy and its relevance to drug stability in solid dosage forms. Int. J. Pharm. 2016, 497, 70–77. [Google Scholar] [CrossRef] [PubMed]
- Pilcer, G.; Amighi, K. Formulation strategy and use of excipients in pulmonary drug delivery. Int. J. Pharm. 2010, 392, 1–19. [Google Scholar] [CrossRef] [PubMed]
- Amaro, M.I.; Tajber, L.; Corrigan, O.I. Co-spray dried carbohydrate microparticles: Crystallisation delay/inhibition and improved aerosolization characteristics through the incorporation of hydroxypropyl-β-cyclodextrin with amorphous raffinose or trehalose. Pharm. Res. 2015, 32, 180–195. [Google Scholar] [CrossRef] [PubMed]
- Peng, T.; Zhang, X.; Ying, H. Nanoporous mannitol carrier prepared by non-organic solvent spray drying technique to enhance the aerosolization performance for dry powder inhalation. Sci. Rep. 2017, 7, 46517. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kinnunen, H.; Hebbink, G.; Peters, H. An investigation into the effect of fine lactose particles on the fluidization behaviour and aerosolization performance of carrier-based dry powder inhaler formulations. AAPS PharmSciTech 2014, 15, 898–909. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rudén, J.; Frenning, G.; Bramer, T. Relationships between surface coverage ratio and powder mechanics of binary adhesive mixtures for inhalation. Int. J. Pharm. 2018, 541, 143–156. [Google Scholar] [CrossRef] [PubMed]
- Yu, J.; Romeo, M.C.; Cavallaro, A.A. Protective Effect of Sodium Stearate on the Moisture-induced deterioration of Hygroscopic Spray-dried Powders. Int. J. Pharm. 2018, 541, 11–18. [Google Scholar] [CrossRef] [PubMed]
- Mangal, S.; Nie, H.; Xu, R. Physico-Chemical Properties, Aerosolization and Dissolution of Co-Spray Dried Azithromycin Particles with l-Leucine for Inhalation. Pharm. Res. 2018, 35, 28. [Google Scholar] [CrossRef] [PubMed]
- Yu, J.; Chan, H.K.; Gengenbach, T. Protection of hydrophobic amino acids against moisture-induced deterioration in the aerosolization performance of highly hygroscopic spray-dried powders. Eur. J. Pharm. Biopharm. 2017, 119, 224–234. [Google Scholar] [CrossRef] [PubMed]
- Aquino, R.P.; Prota, L.; Auriemma, G. Dry powder inhalers of gentamicin and leucine: Formulation parameters, aerosol performance and in vitro toxicity on CuFi1 cells. Int. J. Pharm. 2012, 426, 100–107. [Google Scholar] [CrossRef] [PubMed]
- Momin, M.A.M.; Sinha, S.; Tucker, I.G. Dry powder formulation of kanamycin with enhanced aerosolization efficiency for drug-resistant tuberculosis. Int. J. Pharm. 2017, 528, 107–117. [Google Scholar] [CrossRef] [PubMed]
- Wei, G.; Mangal, S.; Denman, J. Effects of Coating Materials and Processing Conditions on Flow Enhancement of Cohesive Acetaminophen Powders by High-Shear Processing With Pharmaceutical Lubricants. J. Pharm. Sci. 2017, 106, 3022–3032. [Google Scholar] [CrossRef] [PubMed]
- Otake, H.; Okuda, T.; Hira, D. Inhalable Spray-Freeze-Dried Powder with l-Leucine that Delivers Particles Independent of Inspiratory Flow Pattern and Inhalation Device. Pharm. Res. 2016, 33, 922–931. [Google Scholar] [CrossRef] [PubMed]
- Li, L.; Sun, S.; Parumasivam, T. l-Leucine as an excipient against moisture on in vitro aerosolization performances of highly hygroscopic spray-dried powders. Eur. J. Pharm. Biopharm. 2016, 102, 132–141. [Google Scholar] [CrossRef] [PubMed]
- Chang, Y.X.; Yang, J.J.; Pan, R.L. Anti-hygroscopic effect of leucine on spray-dried herbal extract powders. Powder Technol. 2014, 266, 388–395. [Google Scholar] [CrossRef]
- Molina, C.; Kaialy, W.; Chen, Q. Agglomerated novel spray-dried lactose-leucine tailored as a carrier to enhance the aerosolization performance of salbutamol sulfate from DPI formulations. Drug Deliv. Transl. Res. 2017, 1–12. [Google Scholar] [CrossRef] [PubMed]
- Healy, A.M.; Mcdonald, B.F.; Tajber, L. Characterisation of excipient-free nanoporous microparticles (NPMPs) of bendroflumethiazide. Eur. J. Pharm. Biopharm. 2008, 69, 1182–1186. [Google Scholar] [CrossRef] [PubMed]
- Zhou, Q.T.; Qu, L.; Gengenbach, T. Effect of surface coating with magnesium stearate via mechanical dry powder coating approach on the aerosol performance of micronized drug powders from dry powder inhalers. AAPS PharmSciTech 2013, 14, 38–44. [Google Scholar] [CrossRef] [PubMed]
- Manca, M.L.; Valenti, D.; Sales, O.D. Fabrication of polyelectrolyte multilayered vesicles as inhalable dry powder for lung administration of rifampicin. Int. J. Pharm. 2014, 472, 102–109. [Google Scholar] [CrossRef] [PubMed]
- Zhao, Z.; Huang, Z.; Zhang, X. Low density, good flowability cyclodextrin-raffinose binary carrier for dry powder inhaler: Anti-hygroscopicity and aerosolization performance enhancement. Expert Opin. Drug Deliv. 2018, 15, 443–457. [Google Scholar] [CrossRef] [PubMed]
- Gradon, L.; Sosnowski, T.R. Formation of particles for dry powder inhalers. Adv. Powder Technol. 2014, 25, 43–55. [Google Scholar] [CrossRef]
- Jetzer, M.W.; Morrical, B.D.; Schneider, M. Probing the particulate microstructure of the aerodynamic particle size distribution of dry powder inhaler combination products. Int. J. Pharm. 2017, 538, 30–39. [Google Scholar] [CrossRef] [PubMed]
- Hassan, M.S.; Lau, R. Effect of particle formulation on dry powder inhalation efficiency. Curr. Pharm. Des. 2010, 16, 2377–2387. [Google Scholar] [CrossRef] [PubMed]
- Kho, K.; Hadinoto, K. Dry powder inhaler delivery of amorphous drug nanoparticles: Effects of the lactose carrier particle shape and size. Powder Technol. 2013, 233, 303–311. [Google Scholar] [CrossRef]
- Telko, M.J.; Hickey, A.J. Dry powder inhaler formulation. Respir. Care 2005, 50, 1209–1227. [Google Scholar] [PubMed]
- Castellanos, A. The relationship between attractive interparticle forces and bulk behaviour in dry and uncharged fine powders. Adv. Phys. 2005, 54, 263–376. [Google Scholar] [CrossRef]
- Young, P.M.; Kwok, P.; Adi, H. Lactose Composite Carriers for Respiratory Delivery. Pharm. Res. 2009, 26, 802–810. [Google Scholar] [CrossRef] [PubMed]
- Yang, M.Y.; Chan, J.G.Y.; Chan, H.K. Pulmonary drug delivery by powder aerosols. J. Control Release 2014, 193, 228–240. [Google Scholar] [CrossRef] [PubMed]
- Ohta, A.; Nakashima, S.; Matsuyanagi, H. Krafft temperature and enthalpy of solution of N-acyl amino acid surfactants and their racemic modifications: Effect of the counter ion. Colloid Polym. Sci. 2003, 282, 162–169. [Google Scholar] [CrossRef]
- Emery, E.; Oliver, J.; Pugsley, T. Flowability of moist pharmaceutical powders. Powder Technol. 2009, 189, 409–415. [Google Scholar] [CrossRef]
- Bravo-Osuna, I.; Ferrero, C.; Jiménez-Castellanos, M.R. Influence of moisture content on the mechanical properties of methyl methacrylate-starch copolymers. Eur. J. Pharm. Biopharm. 2007, 66, 63–72. [Google Scholar] [CrossRef] [PubMed]
- Mehta, P. Imagine the Superiority of Dry Powder Inhalers from Carrier Engineering. J. Drug Deliv. 2018, 2018, 1–19. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hickey, A.J.; Gonda, I.; Irwin, W.J. Effect of hydrophobic coating on the behavior of a hygroscopic aerosol powder in an environment of controlled temperature and relative humidity. J. Pharm. Sci. 2010, 79, 1009–1014. [Google Scholar] [CrossRef]
- Prota, L.; Santoro, A.; Bifulco, M. Leucine enhances aerosol performance of Naringin dry powder and its activity on cystic fibrosis airway epithelial cells. Int. J. Pharm. 2011, 412, 8–19. [Google Scholar] [CrossRef] [PubMed]
- Yang, J.C.; Wu, C.Y.; Adams, M. DEM analysis of the effect of electrostatic interaction on particle mixing for carrier-based dry powder inhaler formulations. Particuology 2015, 23, 25–30. [Google Scholar] [CrossRef]
- Cordts, E. Capabilities and limitations of using powder rheology and permeability to predict dry powder inhaler performance. Eur. J. Pharm. Biopharm. 2012, 82, 417–423. [Google Scholar] [CrossRef] [PubMed]








| Formulation | ND0 | ND1 | ND2 | ND3 |
|---|---|---|---|---|
| NTM:LL | 100:0 | 50:1 | 30:1 | 10:1 |
| Formulation | d0.1 (μm) | d0.5 (μm) | d0.9 (μm) | D4.3 (μm) | Span | dae (μm) |
|---|---|---|---|---|---|---|
| ND0 | 1.46 ± 0.04 | 3.07 ± 0.12 | 6.60 ± 0.99 | 7.56 ± 3.23 | 2.42 ± 0.01 | 1.50 ± 0.07 |
| ND1 | 1.39 ± 0.01 | 3.07 ± 0.04 | 6.05 ± 0.07 | 3.44 ± 0.04 | 2.35 ± 0.01 | 1.63 ± 0.04 |
| ND2 | 1.36 ± 0.01 | 2.89 ± 0.02 | 5.42 ± 0.04 | 3.17 ± 0.02 | 2.40 ± 0.01 | 1.44 ± 0.05 |
| ND3 | 1.36 ± 0.01 | 3.07 ± 0.01 | 6.00 ± 0.03 | 3.41 ± 0.01 | 2.38 ± 0.01 | 1.84 ± 0.03 |
| Formulation | RD a (%) | FPF b (%) |
|---|---|---|
| ND0 | 69.3 ± 2.2 | 30.60 ± 7.56 |
| ND1 | 93.3 ± 1.7 | 64.93 ± 6.36 |
| ND2 | 98.2 ± 1.2 | 85.14 ± 8.97 |
| ND3 | 82.7 ± 1.8 | 47.82 ± 7.44 |
| Month(s) of Storage | RD (%) | FPF (%) |
|---|---|---|
| 0 | 98.2 ± 1.2 | 85.14 ± 8.97 |
| 1 | 97.9 ± 1.6 | 83.26 ± 5.88 |
| 2 | 97.7 ± 1.4 | 84.78 ± 6.49 |
| 3 | 97.3 ± 2.0 | 83.31 ± 6.72 |
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cui, Y.; Zhang, X.; Wang, W.; Huang, Z.; Zhao, Z.; Wang, G.; Cai, S.; Jing, H.; Huang, Y.; Pan, X.; et al. Moisture-Resistant Co-Spray-Dried Netilmicin with l-Leucine as Dry Powder Inhalation for the Treatment of Respiratory Infections. Pharmaceutics 2018, 10, 252. https://doi.org/10.3390/pharmaceutics10040252
Cui Y, Zhang X, Wang W, Huang Z, Zhao Z, Wang G, Cai S, Jing H, Huang Y, Pan X, et al. Moisture-Resistant Co-Spray-Dried Netilmicin with l-Leucine as Dry Powder Inhalation for the Treatment of Respiratory Infections. Pharmaceutics. 2018; 10(4):252. https://doi.org/10.3390/pharmaceutics10040252
Chicago/Turabian StyleCui, Yingtong, Xuejuan Zhang, Wen Wang, Zhengwei Huang, Ziyu Zhao, Guanlin Wang, Shihao Cai, Hui Jing, Ying Huang, Xin Pan, and et al. 2018. "Moisture-Resistant Co-Spray-Dried Netilmicin with l-Leucine as Dry Powder Inhalation for the Treatment of Respiratory Infections" Pharmaceutics 10, no. 4: 252. https://doi.org/10.3390/pharmaceutics10040252