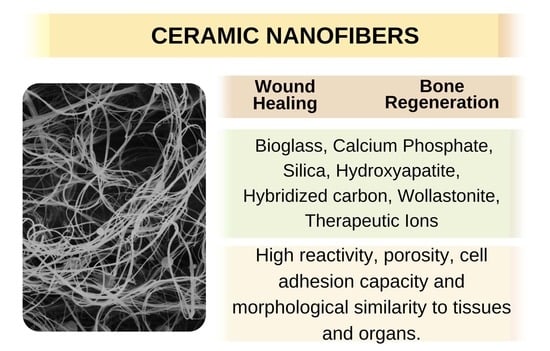
Ceramic Nanofiber Materials for Wound Healing and Bone Regeneration: A Brief Review
Abstract
:1. Introduction
2. Wound Healing
3. Bone Regeneration
4. Future Perspectives
Author Contributions
Funding
Conflicts of Interest
References
- Lauren, C.T. Bone Gratf Substitutes; ASTM International e American Academy of Orthopaedic Surgeons: West Conshohocken, PA, USA, 2003. [Google Scholar]
- World Health Organization (WHO). Available online: https://www.who.int/news-room/fact-sheets/detail/diabetes (accessed on 15 November 2021).
- Ribas, R.G.; Schatkoski, V.M.; do Amaral Montanheiro, T.L.; De Menezes, B.R.C.; Stegemann, C.; Leite, D.M.G.; Thim, G.P. Current advances in bone tissue engineering concerning ceramic and bioglass scaffolds: A review. Ceram. Int. 2019, 45, 21051–21061. [Google Scholar] [CrossRef]
- Qu, H.; Fu, H.; Han, Z.; Sun, Y. Biomaterials for bone tissue engineering scaffolds: A review. RSC Adv. 2019, 9, 26252–26262. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- World Health Organization (WHO). Available online: https://www.who.int/nutrition/topics/5_population_nutrient/en/index25.html (accessed on 19 November 2021).
- Kalyani, R.R.; Golden, S.H.; Cefalu, W.T. Diabetes and aging: Unique considerations and goals of care. Diabetes Care 2017, 40, 440–443. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Homaeigohar, S.; Boccaccini, A.R. Antibacterial biohybrid nanofibers for wound dressings. Acta Biomater. 2020, 107, 25–49. [Google Scholar] [CrossRef] [PubMed]
- Memic, A.; Abudula, T.; Mohammed, H.S.; Joshi Navare, K.; Colombani, T.; Bencherif, S.A. Latest progress in electrospun nanofibers for wound healing applications. ACS Appl. Bio. Mater. 2019, 2, 952–969. [Google Scholar] [CrossRef]
- Sylvester, M.A.; Amini, F.; Tan, C.K. Electrospun nanofibers in wound healing. Mater. Today Proc. 2020, 29, 1–6. [Google Scholar] [CrossRef]
- Caffrey, M. Diabetic Amputations My Be Rising in the United States. Available online: https://www.ajmc.com/view/diabetic-amputations-may-be-rising-in-the-united-states (accessed on 25 November 2021).
- Haugen, H.J.; Lyngstadaas, S.P.; Rossi, F.; Perale, G. Bone grafts: Which is the ideal biomaterial? J. Clin. Periodontol. 2019, 46, 92–102. [Google Scholar] [CrossRef]
- Miguel, S.P.; Figueira, D.R.; Simões, D.; Ribeiro, M.P.; Coutinho, P.; Ferreira, P.; Correia, I.J. Electrospun polymeric nanofibres as wound dressings: A review. Colloids Surf. B Biointerfaces 2018, 169, 60–71. [Google Scholar] [CrossRef]
- Simões, D.; Miguel, S.P.; Ribeiro, M.P.; Coutinho, P.; Mendonça, A.G.; Correia, I.J. Recent advances on antimicrobial wound dressing: A review. Eur. J. Pharm. Biopharm. 2018, 127, 130–141. [Google Scholar] [CrossRef]
- Figliomeni, A.; Signorini, V.; Mazzantini, M. One year in review 2018: Progress in osteoporosis treatment. Clin. Exp. Rheumatol. 2018, 36, 948–958. [Google Scholar]
- Iaquinta, M.R.; Mazzoni, E.; Manfrini, M.; D’Agostino, A.; Trevisiol, L.; Nocini, R.; Trombelli, L.; Barbanti-Brodano, G.; Martini, F.; Tognon, M. Innovative biomaterials for bone regrowth. Int. J. Mol. Sci. 2019, 20, 618. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Engel, E.; Michiardi, A.; Navarro, M.; Lacroix, D.; Planell, J.A. Nanotechnology in regenerative medicine: The materials side. Trends Biotechnol. 2008, 26, 39–47. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mouriño, V.; Cattalini, J.P.; Roether, J.A.; Dubey, P.; Roy, I.; Boccaccini, A.R. Composite polymer-bioceramic scaffolds with drug delivery capability for bone tissue engineering. Exp. Opin. Drug Deliv. 2013, 10, 1353–1365. [Google Scholar] [CrossRef]
- Suárez-Franco, J.L.; García-Hipólito, M.; Surárez-Rosales, M.Á.; Fernández-Pedrero, J.A.; Álvarez-Fregoso, O.; Juárez-Islas, J.A.; Álvarez-Pérez, M.A. Effects of Surface Morphology of Ceramic Materials on Osteoblastic Cells Responses. J. NanoMater. 2013, 2013, 2. [Google Scholar] [CrossRef] [Green Version]
- Lim, C.T. Nanofiber technology: Current status and emerging developments. Prog. Polymer. Sci. 2017, 70, 1–17. [Google Scholar]
- Das, I.; De, G.; Hupa, L.; Vallittu, P.K. Porous SiO2 nanofiber grafted novel bioactive glass–ceramic coating: A structural scaffold for uniform apatite precipitation and oriented cell proliferation on inert implant. Mater. Sci. Eng. C 2016, 62, 206–214. [Google Scholar] [CrossRef] [PubMed]
- Elangomannan, S.; Louis, K.; Dharmaraj, B.M.; Kandasamy, V.S.; Soundarapandian, K.; Gopi, D. Carbon nanofiber/polycaprolactone/mineralized hydroxyapatite nanofibrous scaffolds for potential orthopedic applications. ACS Appl. Mater. Interfaces 2017, 9, 6342–6355. [Google Scholar] [CrossRef]
- Penide, J.; Quintero, F.; del Val, J.; Comesaña, R.; Lusquiños, F.; Riveiro, A.; Pou, J. Bioactive glass nanofibers for tissue engineering. In Materials for Biomedical Engineering; Elsevier: Amsterdam, The Netherlands, 2019; pp. 329–356. [Google Scholar]
- Medeiros, E.L.; Gomes, D.S.; Santos, A.M.; Vieira, R.H.; de Lima, I.L.; Rocha, F.S.; Castro-Filice, L.D.S.; Medeiros, E.S.; Neves, G.A.; Menezes, R.R. 3D nanofibrous bioactive glass scaffolds produced by one-step spinning process. Ceram. Int. 2021, 47, 102–110. [Google Scholar] [CrossRef]
- Zhang, Y.; Li, J.; Soleimani, M.; Giacomini, F.; Friedrich, H.; Truckenmüller, R.; Habibovic, P. Biodegradable Elastic Sponge from Nanofibrous Biphasic Calcium Phosphate Ceramic as an Advanced Material for Regenerative Medicine. Adv. Funct. Mater. 2021, 31, 2102911. [Google Scholar] [CrossRef]
- Tan, A.W.; Pingguan-Murphy, B.; Ahmad, R.; Akbar, S.A. Advances in fabrication of TiO2 nanofiber/nanowire arrays toward the cellular response in biomedical implantations: A review. J. Mater. Sci. 2013, 48, 8337–8353. [Google Scholar] [CrossRef]
- Shitole, A.A.; Raut, P.W.; Sharma, N.; Giram, P.; Khandwekar, A.P.; Garnaik, B. Electrospun polycaprolactone/hydroxyapatite/ZnO nanofibers as potential biomaterials for bone tissue regeneration. J. Mater. Sci. Mater. Med. 2019, 30, 1–17. [Google Scholar] [CrossRef] [PubMed]
- Rana, D.; Ramalingam, M. Ceramic nanofiber composites. In Nanofiber Composites for Biomedical Applications; Elsevier: Amsterdam, The Netherlands, 2017; pp. 33–54. [Google Scholar]
- Kim, H.W.; Kim, H.E.; Knowles, J.C. Production and potential of bioactive glass nanofibers as a next-generation biomaterial. Adv. Funct. Mater. 2006, 16, 1529–1535. [Google Scholar] [CrossRef]
- Xia, W.; Zhang, D.; Chang, J. Fabrication and in vitro biomineralization of bioactive glass (BG) nanofibres. Nanotechnology 2007, 18, 135601. [Google Scholar] [CrossRef] [PubMed]
- Kim, H.W.; Kim, H.E. Nanofiber generation of hydroxyapatite and fluor-hydroxyapatite bioceramics. J. Biomed. Mater. Res. Part B Appl. Biomater. Off. J. Soc. Biomater. Jap. Soc. Biomater. Aust. Soc. Biomater. Korean Soc. Biomater. 2006, 77, 323–328. [Google Scholar] [CrossRef] [PubMed]
- Gazquez, G.C.; Chen, H.; Moroni, L.; Boukamp, B.A.; Johan, E. β-Tricalcium phosphate nanofiber scaffolds with fine unidirectional grains. Mater. Lett. 2017, 208, 118–121. [Google Scholar] [CrossRef]
- Xiao, J.; Wan, Y.; Yao, F.; Huang, Y.; Zhu, Y.; Yang, Z.; Luo, H. Constructing 3D scaffold with 40-nm-diameter hollow mesoporous bioactive glass nanofibers. Mater. Lett. 2019, 248, 201–203. [Google Scholar] [CrossRef]
- Alghoraibi, I.; Alomari, S. Different methods for nanofiber design and fabrication. In Handbook of Nanofibers; Springer: Cham, Switzerland, 2018; pp. 1–46. [Google Scholar]
- Nayak, R.; Padhye, R.; Kyratzis, I.L.; Truong, Y.B.; Arnold, L. Recent advances in nanofibre fabrication techniques. Text. Res. J. 2012, 82, 129–147. [Google Scholar] [CrossRef]
- Luiten-Olieman, M.W.J.; Winnubst, L.; Nijmeijer, A.; Wessling, M.; Benes, N.E. Porous stainless steel hollow fiber membranes via dry–wet spinning. J. Membr. Sci. 2011, 370, 124–130. [Google Scholar] [CrossRef]
- Yaari, A.; Schilt, Y.; Tamburu, C.; Raviv, U.; Shoseyov, O. Wet spinning and drawing of human recombinant collagen. ACS BioMater. Sci. Eng. 2016, 2, 349–360. [Google Scholar] [CrossRef]
- Kim, S.-W.; Kwon, S.-N.; Na, S.-I. Stretchable and electrically conductive polyurethane-silver/graphene composite fibers prepared by wet-spinning process. Compos. Part B Eng. 2019, 167, 573–581. [Google Scholar] [CrossRef]
- Mohanty, S.; Rameshbabu, A.P.; Dhara, S. α-Alumina fiber with platelet morphology through wet spinning. J. Am. Ceramic Soc. 2012, 95, 1234–1240. [Google Scholar] [CrossRef]
- Dadol, G.C.; Kilic, A.; Tijing, L.D.; Lim, K.J.A.; Cabatingan, L.K.; Tan, N.P.B.; Stojanovska, E.; Polat, Y. Solution blow spinning (SBS) and SBS-spun nanofibers: Materials, methods, and applications. Mater. Today Commun. 2020, 25, 101656. [Google Scholar] [CrossRef]
- Guo, Y.; Jian, X.; Zhang, L.; Mu, C.; Yin, L.; Xie, J.; Mahmood, N.; Dou, S.; Che, R.; Deng, L. Plasma-induced FeSiAl@ Al2O3@ SiO2 core–shell structure for exceptional microwave absorption and anti-oxidation at high temperature. Chem. Eng. J. 2020, 384, 123371. [Google Scholar] [CrossRef]
- Sista, D. New Perspective of Nano Fibers: Synthesis and Applications. In Nanofibers; Intechopen: London, UK, 2021. [Google Scholar]
- Yonezawa, T.; Čempel, D.; Nguyen, M.T. Microwave-induced plasma-in-liquid process for nanoparticle production. Bull. Chem. Soc. Jap. 2018, 91, 1781–1798. [Google Scholar] [CrossRef]
- Weitz, R.T.; Harnau, L.; Rauschenbach, S.; Burghard, M.; Kern, K. Polymer nanofibers via nozzle-free centrifugal spinning. Nano Lett. 2008, 8, 1187–1191. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ren, L.; Kotha, S.P. Centrifugal jet spinning for highly efficient and large-scale fabrication of barium titanate nanofibers. Mater. Lett. 2014, 117, 153–157. [Google Scholar] [CrossRef] [Green Version]
- Aminirastabi, H.; Weng, Z.; Xue, H.; Yu, Y.; Ji, G.; Mitic, V.V.; Guan, R. Evaluation of nano grain growth of TiO2 fibers fabricated via centrifugal jet spinning. Nano Struct. Nano Obj. 2020, 21, 100413. [Google Scholar] [CrossRef]
- Zhang, X.; Lu, Y. Centrifugal spinning: An alternative approach to fabricate nanofibers at high speed and low cost. Polym. Rev. 2014, 54, 677–701. [Google Scholar] [CrossRef]
- Noroozi, S.; Taghavi, S.M. 5 Ultrafine Nanofiber Formation by Centrifugal Spinning. In Advanced Materials; De Gruyter: Berlin, Germany, 2020; p. 143. [Google Scholar]
- Khalili, S.; Chenari, H.M. Successful electrospinning fabrication of ZrO2 nanofibers: A detailed physical–chemical characterization study. J. Alloys Compd. 2020, 828, 154414. [Google Scholar] [CrossRef]
- Wen, Z.; Song, X.; Chen, D.; Fan, T.; Liu, Y.; Cai, Q. Electrospinning preparation and microstructure characterization of homogeneous diphasic mullite ceramic nanofibers. Ceram. Int. 2020, 46, 12172–12179. [Google Scholar] [CrossRef]
- Calisir, M.D.; Kilic, A. A comparative study on SiO2 nanofiber production via two novel non-electrospinning methods: Centrifugal spinning vs. solution blowing. Mater. Lett. 2020, 258, 126751. [Google Scholar] [CrossRef]
- Xue, J.; Xie, J.; Liu, W.; Xia, Y. Electrospun nanofibers: New concepts, materials, and applications. Acc. Chem. Res. 2017, 50, 1976–1987. [Google Scholar] [CrossRef] [PubMed]
- Ashraf, R.; Sofi, H.S.; Akram, T.; Rather, H.A.; Abdal-hay, A.; Shabir, N.; Vasita, R.; Alrokayan, S.H.; Khan, H.A.; Sheikh, F.A. Fabrication of multifunctional cellulose/TiO2/Ag composite nanofibers scaffold with antibacterial and bioactivity properties for future tissue engineering applications. J. Biomed. Mater. Res. Part A 2020, 108, 947–962. [Google Scholar] [CrossRef] [PubMed]
- Balas, F.; Perez-Pariente, J.; Vallet-Regi, M. In vitro bioactivity of silicon-substituted hydroxyapatites. J. Biomed. Mater. Res. Part B Appl. Biomater. Off. J. Soc. Biomater. Jap. Soc. Biomater. Aust. Soc. Biomater. Korean Soc. Biomater. 2003, 66, 364–375. [Google Scholar]
- Cheng, D.; Liu, D.; Tang, T.; Zhang, X.; Jia, X.; Cai, Q.; Yang, X. Effects of Ca/P molar ratios on regulating biological functions of hybridized carbon nanofibers containing bioactive glass nanoparticles. Biomed. Mater. 2017, 12, 025019. [Google Scholar] [CrossRef] [PubMed]
- Luo, H.; Li, W.; Ao, H.; Li, G.; Tu, J.; Xiong, G.; Zhu, Y.; Wan, Y. Preparation, structural characterization, and in vitro cell studies of three-dimensional SiO2–CaO binary glass scaffolds built ofultra-small nanofibers. Mater. Sci. Eng. C 2017, 76, 94–101. [Google Scholar] [CrossRef]
- Oliveira, M.J.C.D.; Bonan, R.F.; Campos, S.G.; Neves, G.D.A.; Menezes, R.R. Calcium phosphate submicrometric fibers produced by solution blow spinning. Mater. Res. 2019, 22. [Google Scholar] [CrossRef]
- Mota, M.; Santos, A.; Farias, R.; Neves, G.; Menezes, R. Synthesis and characterization of alumina fibers using solution blow spinning. Cerâmica 2019, 65, 190–193. [Google Scholar] [CrossRef]
- Ding, J.; Zhang, J.; Li, J.; Li, D.; Xiao, C.; Xiao, H.; Yang, H.; Zhuang, X.; Chen, X. Electrospun polymer biomaterials. Progr. Polym. Sci. 2019, 90, 1–34. [Google Scholar] [CrossRef]
- Moeini, A.; Pedram, P.; Makvandi, P.; Malinconico, M.; d’Ayala, G.G. Wound healing and antimicrobial effect of active secondary metabolites in chitosan-based wound dressings: A review. Carbohydr. Polym. 2020, 233, 115839. [Google Scholar] [CrossRef]
- Gangawane, A.; Bhatt, B.; Sunmeet, M. Skin infections in diabetes: A review. Diabetes Metab. 2016, 7, 130–141. [Google Scholar]
- Rezvani Ghomi, E.; Khalili, S.; Nouri Khorasani, S.; Esmaeely Neisiany, R.; Ramakrishna, S. Wound dressings: Current advances and future directions. J. Appl. Polymer. Sci. 2019, 136, 47738. [Google Scholar] [CrossRef] [Green Version]
- Gao, Y.; Zhang, J.; Su, Y.; Wang, H.; Wang, X.-X.; Huang, L.-P.; Yu, M.; Ramakrishna, S.; Long, Y.-Z. Recent progress and challenges in solution blow spinning. Mater. Horiz. 2021, 8, 426–446. [Google Scholar] [CrossRef] [PubMed]
- Li, W.J.; Laurencin, C.T.; Caterson, E.J.; Tuan, R.S.; Ko, F.K. Electrospun nanofibrous structure: A novel scaffold for tissue engineering. J. Biomed. Mater. Res. Part B Appl. Biomater. Off. J. Soc. Biomater. Jap. Soc. Biomater. Aust. Soc. Biomater. Korean Soc. Biomater. 2002, 60, 613–621. [Google Scholar] [CrossRef]
- Barnes, C.P.; Sell, S.A.; Boland, E.D.; Simpson, D.G.; Bowlin, G.L. Nanofiber technology: Designing the next generation of tissue engineering scaffolds. Adv. Drug Deliv. Rev. 2007, 59, 1413–1433. [Google Scholar] [CrossRef]
- Zhong, S.P.; Zhang, Y.Z.; Lim, C.T. Tissue scaffolds for skin wound healing and dermal reconstruction. Wiley Interdisc. Rev. Nanomed. Nanobiotechnol. 2010, 2, 510–525. [Google Scholar] [CrossRef]
- Shahhosseininia, M.; Bazgir, S.; Joupari, M.D. Fabrication and investigation of silica nanofibers via electrospinning. Mater. Sci. Eng. C 2018, 91, 502–511. [Google Scholar] [CrossRef]
- Wan, M.; Zhao, H.; Peng, L.; Zhao, Y.; Sun, L. Facile One-Step Deposition of Ag Nanoparticles on SiO2 Electrospun Nanofiber Surfaces for Label-Free SERS Detection and Antibacterial Dressing. ACS Appl. Bio. Mater. 2021, 4, 6549–6557. [Google Scholar] [CrossRef]
- Norris, E.; Ramos-Rivera, C.; Poologasundarampillai, G.; Clark, J.P.; Ju, Q.; Obata, A.; Hanna, J.V.; Kasuga, T.; Mitchell, C.A.; Jell, G. Electrospinning 3D bioactive glasses for wound healing. Biomed. Mater. 2020, 15, 015014. [Google Scholar] [CrossRef]
- Solanki, A.K.; Lali, F.V.; Autefage, H.; Agarwal, S.; Nommeots-Nomm, A.; Metcalfe, A.D.; Stevens, M.M.; Jones, J.R. Bioactive glasses and electrospun composites that release cobalt to stimulate the HIF pathway for wound healing applications. BioMater. Res. 2021, 25, 1–16. [Google Scholar] [CrossRef]
- Garibay-Alvarado, J.A.; Espinosa-Cristóbal, L.F.; Reyes-López, S.Y. Fibrous silica-hydroxyapatite composite by electrospinning. Int. J. Res. Granthaalayah 2017, 5, 39–47. [Google Scholar] [CrossRef]
- Ahmed, M.K.; Ramadan, R.; El-Dek, S.I.; Uskoković, V. Complex relationship between alumina and selenium-doped carbonated hydroxyapatite as the ceramic additives to electrospun polycaprolactone scaffolds for tissue engineering applications. J. Alloys Comp. 2019, 801, 70–81. [Google Scholar] [CrossRef]
- Ma, Z.; Ji, H.; Tan, D.; Teng, Y.; Dong, G.; Zhou, J.; Qiu, J.; Zhang, M. Silver nanoparticles decorated, flexible SiO2 nanofibers with long-term antibacterial effect as reusable wound cover. Colloids Surf. A Physicochem. Eng. Asp. 2011, 387, 57–64. [Google Scholar] [CrossRef]
- Yamaguchi, T.; Sakai, S.; Kawakami, K. Application of silicate electrospun nanofibers for cell culture. J. Sol. Gel Sci. Technol. 2008, 48, 350–355. [Google Scholar] [CrossRef]
- Garibay-Alvarado, J.A.; Herrera-Ríos, E.B.; Vargas-Requena, C.L.; de Jesús Ruíz-Baltazar, Á.; Reyes-López, S.Y. Cell behavior on silica-hydroxyapatite coaxial composite. PLoS ONE 2021, 16, e0246256. [Google Scholar] [CrossRef]
- Kaur, G. Clinical Applications of Biomaterials: State-of-the-Art Progress, Trends, and Novel Approaches; Springer: Cham, Switzerland, 2017. [Google Scholar]
- Ranga, N.; Gahlyan, S.; Duhan, S. Antibacterial efficiency of Zn, Mg and Sr doped bioactive glass for bone tissue engineering. J. NanoSci. Nanotechnol. 2020, 20, 2465–2472. [Google Scholar] [CrossRef]
- Firmino, H.C.; Nascimento, E.P.; Bonan, R.F.; Maciel, P.P.; Castellano, L.R.; Santana, L.N.; Neves, G.A.; Menezes, R.R. Antifungal activity of TiO2-CeO2 nanofibers against Candida fungi. Mater. Lett. 2021, 283, 128709. [Google Scholar] [CrossRef]
- Safiaghdam, H.; Nokhbatolfoghahaei, H.; Khojasteh, A. Therapeutic metallic ions in bone tissue engineering: A systematic review of the literature. Iran. J. Pharm. Res. IJPR 2019, 18, 101. [Google Scholar]
- Alberti, T.; Coelho, D.; Voytena, A.; Pitz, H.; De Pra, M.; Mazzarino, L.; Kuhnen, S.; Ribeiro-do-Valle, R.; Maraschin, M.; Veleirinho, B. Nanotechnology: A promising tool towards wound healing. Curr. Pharm. Des. 2017, 23, 3515–3528. [Google Scholar] [CrossRef]
- Zhang, Q.; Wang, Y.; Zhang, W.; Hickey, M.E.; Lin, Z.; Tu, Q.; Wang, J. In situ assembly of well-dispersed Ag nanoparticles on the surface of polylactic acid-Au@ polydopamine nanofibers for antimicrobial applications. Colloids Surf. B Biointer. 2019, 184, 110506. [Google Scholar] [CrossRef]
- Münchow, E.A.; Pankajakshan, D.; Albuquerque, M.T.P.; Kamocki, K.; Piva, E.; Gregory, R.L.; Bottino, M.C. Synthesis and characterization of CaO-loaded electrospun matrices for bone tissue engineering. Clin. Oral Inv. 2016, 20, 1921–1933. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Liu, X.; Rahaman, M.N.; Day, D.E. In vitro degradation and conversion of melt-derived Microfibrous borate (13-93B3) bioactive glass doped with metal ions. J. Am. Ceram. Soc. 2014, 97, 3501–3509. [Google Scholar] [CrossRef]
- Ostomel, T.A.; Shi, Q.; Tsung, C.K.; Liang, H.; Stucky, G.D. Spherical bioactive glass with enhanced rates of hydroxyapatite deposition and hemostatic activity. Small 2006, 2, 1261–1265. [Google Scholar] [CrossRef] [PubMed]
- Tokoro, S.; Satoh, T.; Okubo, Y.; Igawa, K.; Yokozeki, H. Latent dystrophic subcutaneous calcification in patients with chronic venous insufficiency. Acta Derm. Venereol. 2009, 89, 505–508. [Google Scholar] [CrossRef]
- Wollina, U.; Hasenöhrl, K.; Köstler, E.; Schönlebe, J.; Heinig, B.; Haroske, G.; Kittner, T. Dystrophic calcification in chronic leg ulcers—A clinicopathologic study. Dermatol. Surg. 2009, 35, 457–461. [Google Scholar] [CrossRef]
- Milas, M.; Bush, R.L.; Lin, P.; Brown, K.; Mackay, G.; Lumsden, A.; Weber, C.; Dodson, T.F. Calciphylaxis and nonhealing wounds: The role of the vascular surgeon in a multidisciplinary treatment. J. Vasc. Surg. 2003, 37, 501–507. [Google Scholar] [CrossRef] [Green Version]
- Jung, S.B.; Day, D.E. Scaffolds with Trace Element for Tissue Regeneration in Mammals. U.S. Patent No. 8,287,896, 16 October 2012. [Google Scholar]
- Saha, S.; Bhattacharjee, A.; Rahaman, S.H.; Ray, S.; Marei, M.K.; Jain, H.; Chakraborty, J. Prospects of antibacterial bioactive glass nanofibers for wound healing: An in vitro study. Int. J. Appl. Glass Sci. 2020, 11, 320–328. [Google Scholar] [CrossRef]
- Tsai, S.-W.; Huang, S.-S.; Yu, W.-X.; Hsu, Y.-W.; Hsu, F.-Y. Fabrication and characteristics of porous hydroxyapatite-CaO composite nanofibers for biomedical applications. NanoMaterials 2018, 8, 570. [Google Scholar] [CrossRef] [Green Version]
- Gérard, C.; Bordeleau, L.-J.; Barralet, J.; Doillon, C.J. The stimulation of angiogenesis and collagen deposition by copper. BioMaterials 2010, 31, 824–831. [Google Scholar] [CrossRef]
- Barralet, J.; Gbureck, U.; Habibovic, P.; Vorndran, E.; Gerard, C.; Doillon, C.J. Angiogenesis in calcium phosphate scaffolds by inorganic copper ion release. Tissue Eng. Part A 2009, 15, 1601–1609. [Google Scholar] [CrossRef]
- Zhao, S.; Wang, H.; Zhang, Y.; Huang, W.; Rahaman, M.N.; Liu, Z.; Wang, D.; Zhang, C. RETRACTED: Copper-doped borosilicate bioactive glass scaffolds with improved angiogenic and osteogenic capacity for repairing osseous defects. Acta Biomater. 2015, 14, 185–196. [Google Scholar] [CrossRef] [PubMed]
- Giavaresi, G.; Torricelli, P.; Fornasari, P.; Giardino, R.; Barbucci, R.; Leone, G. Blood vessel formation after soft-tissue implantation of hyaluronan-based hydrogel supplemented with copper ions. BioMaterials 2005, 26, 3001–3008. [Google Scholar] [CrossRef] [PubMed]
- Gorter, R.W.; Butorac, M.; Cobian, E.P. Examination of the cutaneous absorption of copper after the use of copper-containing ointments. Am. J. Therap. 2004, 11, 453–458. [Google Scholar] [CrossRef] [PubMed]
- Borkow, G.; Gabbay, J.; Lyakhovitsky, A.; Huszar, M. Improvement of facial skin characteristics using copper oxide containing pillowcases: A double-blind, placebo-controlled, parallel, randomized study. Int. J. Cosmet. Sci. 2009, 31, 437–443. [Google Scholar] [CrossRef]
- Zhao, S.; Li, L.; Wang, H.; Zhang, Y.; Cheng, X.; Zhou, N.; Rahaman, M.N.; Liu, Z.; Huang, W.; Zhang, C. Wound dressings composed of copper-doped borate bioactive glass microfibers stimulate angiogenesis and heal full-thickness skin defects in a rodent model. BioMaterials 2015, 53, 379–391. [Google Scholar] [CrossRef]
- Alonzo, M.; Primo, F.A.; Kumar, S.A.; Mudloff, J.A.; Dominguez, E.; Fregoso, G.; Ortiz, N.; Weiss, W.M.; Joddar, B. Bone tissue engineering techniques, advances, and scaffolds for treatment of bone defects. Curr. Opin. Biomed. Eng. 2021, 17, 100248. [Google Scholar] [CrossRef]
- Turnbull, G.; Clarke, J.; Picard, F.; Riches, P.; Jia, L.; Han, F.; Li, B.; Shu, W. 3D bioactive composite scaffolds for bone tissue engineering. Bioact. Mater. 2018, 3, 278–314. [Google Scholar] [CrossRef] [Green Version]
- Rahman, M.A.; Islam, M.S.; Haque, P.; Khan, M.N.; Takafuji, M.; Begum, M.; Chowdhury, G.W.; Khan, M.; Rahman, M.M. Calcium ion mediated rapid wound healing by nano-ZnO doped calcium phosphate-chitosan-alginate biocomposites. Materialia 2020, 13, 100839. [Google Scholar] [CrossRef]
- Mouriño, V.; Vidotto, R.; Cattalini, J.; Boccaccini, A. Enhancing biological activity of bioactive glass scaffolds by inorganic ion delivery for bone tissue engineering. Curr. Opin. Biomed. Eng. 2019, 10, 23–34. [Google Scholar] [CrossRef]
- Antoniac, I.V. Handbook of Bioceramics and Biocomposites; Springer: Berlin, Germany, 2016. [Google Scholar]
- Wu, Y.; Jiang, W.; Wen, X.; He, B.; Zeng, X.; Wang, G.; Gu, Z. A novel calcium phosphate ceramic–magnetic nanoparticle composite as a potential bone substitute. Biomed. Mater. 2010, 5, 015001. [Google Scholar] [CrossRef]
- Wen, W.; Zou, Z.; Luo, B.; Zhou, C. In vitro degradation and cytocompatibility of g-MgO whiskers/PLLA composites. J. Mater. Sci. 2017, 52, 2329–2344. [Google Scholar] [CrossRef]
- Xing, X.; Cheng, G.; Yin, C.; Cheng, X.; Cheng, Y.; Ni, Y.; Zhou, X.; Deng, H.; Li, Z. Magnesium-containing silk fibroin/polycaprolactone electrospun nanofibrous scaffolds for accelerating bone regeneration. Arab. J. Chem. 2020, 13, 5526–5538. [Google Scholar] [CrossRef]
- Shalumon, K.; Sowmya, S.; Sathish, D.; Chennazhi, K.; Nair, S.V.; Jayakumar, R. Effect of incorporation of nanoscale bioactive glass and hydroxyapatite in PCL/chitosan nanofibers for bone and periodontal tissue engineering. J. Biomed. Nanotechnol. 2013, 9, 430–440. [Google Scholar] [CrossRef] [PubMed]
- Gandolfi, M.G.; Zamparini, F.; Degli Esposti, M.; Chiellini, F.; Aparicio, C.; Fava, F.; Fabbri, P.; Taddei, P.; Prati, C. Polylactic acid-based porous scaffolds doped with calcium silicate and dicalcium phosphate dihydrate designed for biomedical application. Mater. Sci. Eng. C 2018, 82, 163–181. [Google Scholar] [CrossRef]
- Kharaziha, M.; Fathi, M.; Edris, H. Development of novel aligned nanofibrous composite membranes for guided bone regeneration. J. Mech. Beh. Biomed. Mater. 2013, 24, 9–20. [Google Scholar] [CrossRef] [PubMed]
- Augustine, A.; Augustine, R.; Hasan, A.; Raghuveeran, V.; Rouxel, D.; Kalarikkal, N.; Thomas, S. Development of titanium dioxide nanowire incorporated poly (vinylidene fluoride–trifluoroethylene) scaffolds for bone tissue engineering applications. J. Mater. Sci. Mater. Med. 2019, 30, 1–13. [Google Scholar] [CrossRef] [Green Version]
- Ramírez-Cedillo, E.; Ortega-Lara, W.; Rocha-Pizaña, M.R.; Gutierrez-Uribe, J.A.; Elías-Zúñiga, A.; Rodríguez, C.A. Electrospun polycaprolactone fibrous membranes containing Ag, TiO2 and Na2Ti6O13 particles for potential use in bone regeneration. Membranes 2019, 9, 12. [Google Scholar] [CrossRef] [Green Version]
- Bagchi, A.; Meka, S.R.K.; Rao, B.N.; Chatterjee, K. Perovskite ceramic nanoparticles in polymer composites for augmenting bone tissue regeneration. Nanotechnology 2014, 25, 485101. [Google Scholar] [CrossRef]
- Meng, J.; Zhang, Y.; Qi, X.; Kong, H.; Wang, C.; Xu, Z.; Xie, S.; Gu, N.; Xu, H. Paramagnetic nanofibrous composite films enhance the osteogenic responses of pre-osteoblast cells. Nanoscale 2010, 2, 2565–2569. [Google Scholar] [CrossRef]
- Wei, Y.; Zhang, X.; Song, Y.; Han, B.; Hu, X.; Wang, X.; Lin, Y.; Deng, X. Magnetic biodegradable Fe3O4/CS/PVA nanofibrous membranes for bone regeneration. Biomed. Mater. 2011, 6, 055008. [Google Scholar] [CrossRef] [Green Version]
- Dos Santos, V.; Brandalise, R.N.; Savaris, M. Engineering of Biomatterials; Springer: Cham, Switzerland, 2017. [Google Scholar]
- Wu, C.; Chang, J. Degradation, bioactivity, and cytocompatibility of diopside, akermanite, and bredigite ceramics. J. Biomed. Mater. Res. Part B Appl. Biomater. Off. J. Soc. Biomater. Jap. Soc. Biomater. Aust. Soc. Biomater. Korean Soc. Biomater. 2007, 83, 153–160. [Google Scholar] [CrossRef] [PubMed]
- Zhou, T.; Liu, X.; Sui, B.; Liu, C.; Mo, X.; Sun, J. Development of fish collagen/bioactive glass/chitosan composite nanofibers as a GTR/GBR membrane for inducing periodontal tissue regeneration. Biomed. Mater. 2017, 12, 055004. [Google Scholar] [CrossRef] [PubMed]
- Hoppe, A.; Güldal, N.S.; Boccaccini, A.R. A review of the biological response to ionic dissolution products from bioactive glasses and glass-ceramics. BioMaterials 2011, 32, 2757–2774. [Google Scholar] [CrossRef]
- Samadian, H.; Mobasheri, H.; Azami, M.; Faridi-Majidi, R. Osteoconductive and electroactive carbon nanofibers/hydroxyapatite nanocomposite tailored for bone tissue engineering: In vitro and in vivo studies. Sci. Rep. 2020, 10, 1–14. [Google Scholar] [CrossRef] [PubMed]
- Habibovic, P.; Barralet, J. Bioinorganics and biomaterials: Bone repair. Acta Biomater. 2011, 7, 3013–3026. [Google Scholar] [CrossRef]
- Weng, L.; Boda, S.K.; Teusink, M.J.; Shuler, F.D.; Li, X.; Xie, J. Binary doping of strontium and copper enhancing osteogenesis and angiogenesis of bioactive glass nanofibers while suppressing osteoclast activity. ACS Appl. Mater. Int. 2017, 9, 24484–24496. [Google Scholar] [CrossRef] [PubMed]
- Bonnelye, E.; Chabadel, A.; Saltel, F.; Jurdic, P. Dual effect of strontium ranelate: Stimulation of osteoblast differentiation and inhibition of osteoclast formation and resorption in vitro. Bone 2008, 42, 129–138. [Google Scholar] [CrossRef]
- Li, Y.; Pan, Q.; Xu, J.; He, X.; Li, H.A.; Oldridge, D.A.; Li, G.; Qin, L. Overview of methods for enhancing bone regeneration in distraction osteogenesis: Potential roles of biometals. J. Orthop. Trans. 2021, 27, 110–118. [Google Scholar] [CrossRef]
- Holopainen, J.; Ritala, M. Rapid production of bioactive hydroxyapatite fibers via electroblowing. J. Eur. Ceramic Soc. 2016, 36, 3219–3224. [Google Scholar] [CrossRef]
- Shin, M.; Yoshimoto, H.; Vacanti, J.P. In vivo bone tissue engineering using mesenchymal stem cells on a novel electrospun nanofibrous scaffold. Tissue Eng. 2004, 10, 33–41. [Google Scholar] [CrossRef]
- Pasuri, J.; Holopainen, J.; Kokkonen, H.; Persson, M.; Kauppinen, K.; Lehenkari, P.; Santala, E.; Ritala, M.; Tuukkanen, J. Osteoclasts in the interface with electrospun hydroxyapatite. Colloids Surf. B Biointer. 2015, 135, 774–783. [Google Scholar] [CrossRef] [PubMed]
- Hong, Y.; Chen, X.; Jing, X.; Fan, H.; Gu, Z.; Zhang, X. Fabrication and drug delivery of ultrathin mesoporous bioactive glass hollow fibers. Adv. Funct. Mater. 2010, 20, 1503–1510. [Google Scholar] [CrossRef]
- Tsai, S.-W.; Chang, Y.-H.; Yu, J.-L.; Hsu, H.-W.; Rau, L.-R.; Hsu, F.-Y. Preparation of nanofibrous structure of mesoporous bioactive glass microbeads for biomedical applications. Materials 2016, 9, 487. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lian, H.; Meng, Z. Fabrication, characterization and osteoblast responses of poly (octanediol citrate)/bioglass nanofiber composites. Mater. Sci. Eng. C 2018, 84, 123–129. [Google Scholar] [CrossRef]
- Du, Z.; Zhao, Z.; Liu, H.; Liu, X.; Zhang, X.; Huang, Y.; Leng, H.; Cai, Q.; Yang, X. Macroporous scaffolds developed from CaSiO3 nanofibers regulating bone regeneration via controlled calcination. Mater. Sci. Eng. C 2020, 113, 111005. [Google Scholar] [CrossRef]
- Dai, X.; Shivkumar, S. Electrospinning of PVA-Calcium Phosphate Sol Precursors for the Production of Fibrous Hydroxyapatite. J. Am. Ceramic Soc. 2007, 90, 1412–1419. [Google Scholar] [CrossRef]
- LeGeros, R.Z.; Legeros, J.P. Phosphate minerals in human tissues. In Phosphate Minerals; Springer: Berlin, Germany, 1984; pp. 351–385. [Google Scholar]
- Klein, C.P.; Patka, P.; Den Hollander, W. Macroporous calcium phosphate bioceramics in dog femora: A histological study of interface and biodegration. BioMaterials 1989, 10, 59–62. [Google Scholar] [CrossRef]
- Gauthier, O.; Goyenvalle, E.; Bouler, J.-M.; Guicheux, J.; Pilet, P.; Weiss, P.; Daculsi, G. Macroporous biphasic calcium phosphate ceramics versus injectable bone substitute: A comparative study 3 and 8 weeks after implantation in rabbit bone. J. Mater. Sci. Mater. Med. 2001, 12, 385–390. [Google Scholar] [CrossRef]
- Rahaman, M.N.; Day, D.E.; Bal, B.S.; Fu, Q.; Jung, S.B.; Bonewald, L.F.; Tomsia, A.P. Bioactive glass in tissue engineering. Acta Biomater. 2011, 7, 2355–2373. [Google Scholar] [CrossRef] [Green Version]
- Yi, Z.; Wang, K.; Tian, J.; Shu, Y.; Yang, J.; Xiao, W.; Li, B.; Liao, X. Hierarchical porous hydroxyapatite fibers with a hollow structure as drug delivery carriers. Ceram. Int. 2016, 42, 19079–19085. [Google Scholar] [CrossRef]
- Yuan, H.; Fernandes, H.; Habibovic, P.; De Boer, J.; Barradas, A.M.; De Ruiter, A.; Walsh, W.R.; Van Blitterswijk, C.A.; De Bruijn, J.D. Osteoinductive ceramics as a synthetic alternative to autologous bone grafting. Proc. Natl. Acad. Sci. USA 2010, 107, 13614–13619. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Champion, E. Sintering of calcium phosphate bioceramics. Acta Biomater. 2013, 9, 5855–5875. [Google Scholar] [CrossRef] [PubMed]
- Jeong, J.; Kim, J.H.; Shim, J.H.; Hwang, N.S.; Heo, C.Y. Bioactive calcium phosphate materials and applications in bone regeneration. BioMater. Res. 2019, 23, 1–11. [Google Scholar]
- Basu, B.; Balani, K. Advanced Structural Ceramics; John Wiley & Sons: Hoboken, NJ, USA, 2011. [Google Scholar]
- Min, B.-M.; Lee, G.; Kim, S.H.; Nam, Y.S.; Lee, T.S.; Park, W.H. Electrospinning of silk fibroin nanofibers and its effect on the adhesion and spreading of normal human keratinocytes and fibroblasts in vitro. BioMaterials 2004, 25, 1289–1297. [Google Scholar] [CrossRef] [PubMed]
- Teixeira, A.I.; Nealey, P.F.; Murphy, C.J. Responses of human keratocytes to micro-and nanostructured substrates. J. Biomed. Mater. Res. Part B Appl. Biomater. Off. J. Soc. Biomater. Jap. Soc. Biomater. Aust. Soc. Biomater. Korean Soc. Biomater. 2004, 71, 369–376. [Google Scholar] [CrossRef]
- Yousefi, A.-M.; Oudadesse, H.; Akbarzadeh, R.; Wers, E.; Lucas-Girot, A. Physical and biological characteristics of nanohydroxyapatite and bioactive glasses used for bone tissue engineering. Nanotechnol. Rev. 2014, 3, 527–552. [Google Scholar] [CrossRef]
- Hench, L.L. Bioceramics: From concept to clinic. J. Am. Ceram. Soc. 1991, 74, 1487–1510. [Google Scholar] [CrossRef]
- Hench, L.L. Glass and glass-ceramic technologies to transform the world. Int. J. Appl. Glass Sci. 2011, 2, 162–176. [Google Scholar] [CrossRef]
- Jones, J.R. Review of bioactive glass: From Hench to hybrids. Acta Biomater. 2013, 9, 4457–4486. [Google Scholar] [CrossRef]
- Lobel, K.; Hench, L. In vitro adsorption and activity of enzymes on reaction layers of bioactive glass substrates. J. Biomed. Mater. Res. Part B Appl. Biomater. Off. J. Soc. Biomater. Jap. Soc. Biomater. Aust. Soc. Biomater. Korean Soc. Biomater. 1998, 39, 575–579. [Google Scholar]
- Ohgushi, H.; Dohi, Y.; Yoshikawa, T.; Tamai, S.; Tabata, S.; Okunaga, K.; Shibuya, T. Osteogenic differentiation of cultured marrow stromal stem cells on the surface of bioactive glass ceramics. J. Biomed. Mater. Res. Off. J. Soc. BioMater. Jap. Soc. BioMater. 1996, 32, 341–348. [Google Scholar] [CrossRef]
- Day, R.M.; Boccaccini, A.R.; Shurey, S.; Roether, J.A.; Forbes, A.; Hench, L.L.; Gabe, S.M. Assessment of polyglycolic acid mesh and bioactive glass for soft-tissue engineering scaffolds. BioMaterials 2004, 25, 5857–5866. [Google Scholar] [CrossRef] [PubMed]
- Keshaw, H.; Forbes, A.; Day, R.M. Release of angiogenic growth factors from cells encapsulated in alginate beads with bioactive glass. BioMaterials 2005, 26, 4171–4179. [Google Scholar]
- Roether, J.; Gough, J.; Boccaccini, A.R.; Hench, L.; Maquet, V.; Jérôme, R. Novel bioresorbable and bioactive composites based on bioactive glass and polylactide foams for bone tissue engineering. J. Mater. Sci. Mater. Med. 2002, 13, 1207–1214. [Google Scholar] [CrossRef] [PubMed]
- Zhao, J.; Han, W.; Chen, H.; Tu, M.; Huan, S.; Miao, G.; Zeng, R.; Wu, H.; Cha, Z.; Zhou, C. Fabrication and in vivo osteogenesis of biomimetic poly (propylene carbonate) scaffold with nanofibrous chitosan network in macropores for bone tissue engineering. J. Mater. Sci. Mater. Med. 2012, 23, 517–525. [Google Scholar] [CrossRef] [PubMed]
- Shirosaki, Y.; Tsuru, K.; Hayakawa, S.; Osaka, A.; Lopes, M.A.; Santos, J.D.; Fernandes, M.H. In vitro cytocompatibility of MG63 cells on chitosan-organosiloxane hybrid membranes. BioMaterials 2005, 26, 485–493. [Google Scholar] [CrossRef]
- Ramaswamy, Y.; Wu, C.; Van Hummel, A.; Combes, V.; Grau, G.; Zreiqat, H. The responses of osteoblasts, osteoclasts and endothelial cells to zirconium modified calcium-silicate-based ceramic. BioMaterials 2008, 29, 4392–4402. [Google Scholar] [CrossRef]
- Rhee, S.-H.; Hwang, M.-H.; Si, H.-J.; Choi, J.-Y. Biological activities of osteoblasts on poly (methyl methacrylate)/silica hybrid containing calcium salt. BioMaterials 2003, 24, 901–906. [Google Scholar] [CrossRef]
- Luo, H.; Ji, D.; Li, W.; Xiao, J.; Li, C.; Xiong, G.; Zhu, Y.; Wan, Y. Constructing a highly bioactive 3D nanofibrous bioglass scaffold via bacterial cellulose-templated sol-gel approach. Mater. Chem. Phys. 2016, 176, 1–5. [Google Scholar] [CrossRef]
- Luo, H.; Zhang, Y.; Li, G.; Tu, J.; Yang, Z.; Xiong, G.; Wang, Z.; Huang, Y.; Wan, Y. Sacrificial template method for the synthesis of three-dimensional nanofibrous 58S bioglass scaffold and its in vitro bioactivity and cell responses. J. BioMater. Appl. 2017, 32, 265–275. [Google Scholar] [CrossRef]
- Wen, C.; Hong, Y.; Wu, J.; Luo, L.; Qiu, Y.; Ye, J. The facile synthesis and bioactivity of a 3D nanofibrous bioglass scaffold using an amino-modified bacterial cellulose template. RSC Adv. 2018, 8, 14561–14569. [Google Scholar] [CrossRef] [Green Version]
- Wu, C.; Ramaswamy, Y.; Kwik, D.; Zreiqat, H. The effect of strontium incorporation into CaSiO3 ceramics on their physical and biological properties. BioMaterials 2007, 28, 3171–3181. [Google Scholar] [CrossRef] [PubMed]
- Gandolfi, M.; Spagnuolo, G.; Siboni, F.; Procino, A.; Rivieccio, V.; Pelliccioni, G.; Prati, C.; Rengo, S. Calcium silicate/calcium phosphate biphasic cements for vital pulp therapy: Chemical-physical properties and human pulp cells response. Clin. Oral Inv. 2015, 19, 2075–2089. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mazón, P.; Piedad, N. Porous scaffold prepared from α′ L-Dicalcium silicate doped with phosphorus for bone grafts. Ceram. Int. 2018, 44, 537–545. [Google Scholar] [CrossRef]
- Lin, K.; Xia, L.; Li, H.; Jiang, X.; Pan, H.; Xu, Y.; Lu, W.W.; Zhang, Z.; Chang, J. Enhanced osteoporotic bone regeneration by strontium-substituted calcium silicate bioactive ceramics. BioMaterials 2013, 34, 10028–10042. [Google Scholar] [CrossRef] [PubMed]
- Liu, S.; Jin, F.; Lin, K.; Lu, J.; Sun, J.; Chang, J.; Dai, K.; Fan, C. The effect of calcium silicate on in vitro physiochemical properties and in vivo osteogenesis, degradability and bioactivity of porous β-tricalcium phosphate bioceramics. Biomed. Mater. 2013, 8, 025008. [Google Scholar] [CrossRef]
- Wang, C.; Lin, K.; Chang, J.; Sun, J. The stimulation of osteogenic differentiation of mesenchymal stem cells and vascular endothelial growth factor secretion of endothelial cells by β-CaSiO3/β-Ca3 (PO4) 2 scaffolds. J. Biomed. Mater. Res. Part A 2014, 102, 2096–2104. [Google Scholar] [CrossRef]
- Xiong, K.; Zhang, J.; Shi, H.; Liu, J.; Wu, H.; Li, H.; Ye, J. Preparation and in vitro cell-biological performance of sodium alginate/nano-zinc silicate co-modified calcium silicate bioceramics. RSC Adv. 2015, 5, 8329–8339. [Google Scholar] [CrossRef]
- Lin, K.; Lin, C.; Zeng, Y. High mechanical strength bioactive wollastonite bioceramics sintered from nanofibers. RSC Adv. 2016, 6, 13867–13872. [Google Scholar] [CrossRef]
- Lin, K.; Chang, J.; Lu, J.; Wu, W.; Zeng, Y. Properties of β-Ca3 (PO4) 2 bioceramics prepared using nano-size powders. Ceramics Int. 2007, 33, 979–985. [Google Scholar] [CrossRef]
- Kokubo, T.; Takadama, H. How useful is SBF in predicting in vivo bone bioactivity? BioMaterials 2006, 27, 2907–2915. [Google Scholar] [CrossRef] [PubMed]
- Turdean-Ionescu, C.; Stevensson, B.; Grins, J.; Izquierdo-Barba, I.; Garcia, A.; Arcos, D.; Vallet-Regí, M.; Edén, M. Composition-dependent in vitro apatite formation at mesoporous bioactive glass-surfaces quantified by solid-state NMR and powder XRD. RSC Adv. 2015, 5, 86061–86071. [Google Scholar] [CrossRef] [Green Version]
- Liu, S.; Gong, W.; Dong, Y.; Hu, Q.; Chen, X.; Gao, X. The effect of submicron bioactive glass particles on in vitro osteogenesis. Rsc Adv. 2015, 5, 38830–38836. [Google Scholar] [CrossRef]
- Lin, K.; Zhang, M.; Zhai, W.; Qu, H.; Chang, J. Fabrication and characterization of hydroxyapatite/wollastonite composite bioceramics with controllable properties for hard tissue repair. J. Am. Ceram. Soc. 2011, 94, 99–105. [Google Scholar] [CrossRef]
- Du, Z.; Guo, L.; Zheng, T.; Cai, Q.; Yang, X. Formation of core-shell structured calcium silicate fiber via sol-gel electrospinning and controlled calcination. Ceram. Int. 2019, 45, 23975–23983. [Google Scholar] [CrossRef]
- Geng, M.; Zhang, Q.; Gu, J.; Yang, J.; Du, H.; Jia, Y.; Zhou, X.; He, C. Construction of a nanofiber network within 3D printed scaffolds for vascularized bone regeneration. BioMater. Sci. 2021, 9, 2631–2646. [Google Scholar] [CrossRef]
- Kołbuk, D.; Heljak, M.; Choińska, E.; Urbanek, O. Novel 3D hybrid nanofiber scaffolds for bone regeneration. Polymers 2020, 12, 544. [Google Scholar] [CrossRef] [Green Version]
- Xiao, L.; Wu, M.; Yan, F.; Xie, Y.; Liu, Z.; Huang, H.; Yang, Z.; Yao, S.; Cai, L. A radial 3D polycaprolactone nanofiber scaffold modified by biomineralization and silk fibroin coating promote bone regeneration in vivo. Int. J. Biol. Macromol. 2021, 172, 19–29. [Google Scholar] [CrossRef]
- Pedrosa, M.C.G.; dos Anjos, S.A.; Mavropoulos, E.; Bernardo, P.L.; Granjeiro, J.M.; Rossi, A.M.; Dias, M.L. Structure and biological compatibility of polycaprolactone/zinc-hydroxyapatite electrospun nanofibers for tissue regeneration. J. Bioact. Comp. Polym. 2021, 36, 314–333. [Google Scholar] [CrossRef]
- Fraczek-Szczypta, A.; Rabiej, S.; Szparaga, G.; Pabjanczyk-Wlazlo, E.; Krol, P.; Brzezinska, M.; Blazewicz, S.; Bogun, M. The structure and properties of the carbon non-wovens modified with bioactive nanoceramics for medical applications. Mater. Sci. Eng. C 2015, 51, 336–345. [Google Scholar] [CrossRef]
- Rajzer, I.; Menaszek, E.; Bacakova, L.; Rom, M.; Blazewicz, M. In vitro and in vivo studies on biocompatibility of carbon fibres. J. Mater. Sci. Mater. Med. 2010, 21, 2611–2622. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- De Oliveira, A.A.R.; De Souza, D.A.; Dias, L.L.S.; De Carvalho, S.M.; Mansur, H.S.; de Magalhães Pereira, M. Synthesis, characterization and cytocompatibility of spherical bioactive glass nanoparticles for potential hard tissue engineering applications. Biomed. Mater. 2013, 8, 025011. [Google Scholar] [CrossRef] [PubMed]
- Yang, J.; Long, T.; He, N.-F.; Guo, Y.-P.; Zhu, Z.-A.; Ke, Q.-F. Fabrication of a chitosan/bioglass three-dimensional porous scaffold for bone tissue engineering applications. J. Mater. Chem. B 2014, 2, 6611–6618. [Google Scholar] [CrossRef] [PubMed]
- Smolka, W.; Dlugon, E.; Jelen, P.; Niemiec, W.; Panek, A.; Paluszkiewicz, C.; Zagrajczuk, B.; Menaszek, E.; Markowski, J.; Blazewicz, M. Carbon nanofibers coated with silicon/calcium-based compounds for medical application. J. NanoMater. 2019, 2019, 7172641. [Google Scholar] [CrossRef]
- Waisi, B.I.; Al-Jubouri, S.M.; McCutcheon, J.R. Fabrication and characterizations of silica nanoparticle embedded carbon nanofibers. Ind. Eng. Chem. Res. 2019, 58, 4462–4467. [Google Scholar] [CrossRef]
- Nekounam, H.; Kandi, M.R.; Shaterabadi, D.; Samadian, H.; Mahmoodi, N.; Hasanzadeh, E.; Faridi-Majidi, R. Silica nanoparticles-incorporated carbon nanofibers as bioactive biomaterial for bone tissue engineering. Diam. Rel. Mater. 2021, 115, 108320. [Google Scholar] [CrossRef]
- Nekounam, H.; Allahyari, Z.; Gholizadeh, S.; Mirzaei, E.; Shokrgozar, M.A.; Faridi-Majidi, R. Simple and robust fabrication and characterization of conductive carbonized nanofibers loaded with gold nanoparticles for bone tissue engineering applications. Mater. Sci. Eng. C 2020, 117, 111226. [Google Scholar] [CrossRef]
- Thompson, K.H.; Orvig, C. Boon and bane of metal ions in medicine. Science 2003, 300, 936–939. [Google Scholar] [CrossRef]
- Esteban-Tejeda, L.; Malpartida, F.; Esteban-Cubillo, A.; Pecharromán, C.; Moya, J. Antibacterial and antifungal activity of a soda-lime glass containing copper nanoparticles. Nanotechnology 2009, 20, 505701. [Google Scholar] [CrossRef]
- Lang, C.; Murgia, C.; Leong, M.; Tan, L.-W.; Perozzi, G.; Knight, D.; Ruffin, R.; Zalewski, P. Anti-inflammatory effects of zinc and alterations in zinc transporter mRNA in mouse models of allergic inflammation. Am. J. Phys. Lung Cell. Mol. Phys. 2007, 292, L577–L584. [Google Scholar] [CrossRef] [Green Version]
- Hoppe, A.; Mouriño, V.; Boccaccini, A.R. Therapeutic inorganic ions in bioactive glasses to enhance bone formation and beyond. BioMater. Sci. 2013, 1, 254–256. [Google Scholar] [CrossRef] [PubMed]
- Vallet-Regí, M.; Arcos, D. Silicon substituted hydroxyapatites. A method to upgrade calcium phosphate based implants. J. Mater. Chem. 2005, 15, 1509–1516. [Google Scholar] [CrossRef]
- Gentleman, E.; Fredholm, Y.C.; Jell, G.; Lotfibakhshaiesh, N.; O’Donnell, M.D.; Hill, R.G.; Stevens, M.M. The effects of strontium-substituted bioactive glasses on osteoblasts and osteoclasts in vitro. BioMaterials 2010, 31, 3949–3956. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ahmed, I.; Parsons, A.; Jones, A.; Walker, G.; Scotchford, C.; Rudd, C. Cytocompatibility and effect of increasing MgO content in a range of quaternary invert phosphate-based glasses. J. BioMater. Appl. 2010, 24, 555–575. [Google Scholar] [CrossRef] [PubMed]
- Su, Y.; Cockerill, I.; Wang, Y.; Qin, Y.-X.; Chang, L.; Zheng, Y.; Zhu, D. Zinc-based biomaterials for regeneration and therapy. Trends Biotechnol. 2019, 37, 428–441. [Google Scholar] [CrossRef]
- Deliormanlı, A.M. Electrospun cerium and gallium-containing silicate based 13-93 bioactive glass fibers for biomedical applications. Ceram. Int. 2016, 42, 897–906. [Google Scholar] [CrossRef]
- Chen, L.; Pan, H.; Zhuang, C.; Peng, M.; Zhang, L. Joint wound healing using polymeric dressing of chitosan/strontium-doped titanium dioxide with high antibacterial activity. Mater. Lett. 2020, 268, 127555. [Google Scholar] [CrossRef]
- Sen, C.K.; Khanna, S.; Venojarvi, M.; Trikha, P.; Ellison, E.C.; Hunt, T.K.; Roy, S. Copper-induced vascular endothelial growth factor expression and wound healing. Am. J. Phys. Heart Circ. Phys. 2002, 282, H1821–H1827. [Google Scholar] [CrossRef] [Green Version]
- Frangoulis, M.; Georgiou, P.; Chrisostomidis, C.; Perrea, D.; Dontas, I.; Kavantzas, N.; Kostakis, A.; Papadopoulos, O. Rat epigastric flap survival and VEGF expression after local copper application. Plast. Reconst. Surg. 2007, 119, 837–843. [Google Scholar] [CrossRef]
- Tsai, S.-W.; Yu, W.-X.; Hwang, P.-A.; Huang, S.-S.; Lin, H.-M.; Hsu, Y.-W.; Hsu, F.-Y. Fabrication and characterization of strontium-substituted hydroxyapatite-CaO-CaCO3 nanofibers with a mesoporous structure as drug delivery carriers. Pharmaceutics 2018, 10, 179. [Google Scholar] [CrossRef] [Green Version]
- Zaichick, V.; Zaichick, S.; Karandashev, V.; Nosenko, S. The effect of age and gender on Al, B, Ba, Ca, Cu, Fe, K, Li, Mg, Mn, Na, P, S, Sr, V, and Zn contents in rib bone of healthy humans. Biol. Trace Elem. Res. 2009, 129, 107–115. [Google Scholar] [CrossRef] [PubMed]
- Zheng, T.; Zhao, H.; Huang, Y.; Gao, C.; Zhang, X.; Cai, Q.; Yang, X. Piezoelectric calcium/manganese-doped barium titanate nanofibers with improved osteogenic activity. Ceram. Int. 2021, 47, 28778–28789. [Google Scholar] [CrossRef]












| Nanofiber | Method | Composition (mol) | Physical–Chemical Properties | Diameter (nm) | Biological Properties | Reference |
|---|---|---|---|---|---|---|
| Silica hybrids | Electrospinning | Sílica (SiO2) Sílica (SiO2)–Bioactive glass (58% SiO2, 38% CaO, 4% P2O5) | Withstand autoclave sterilization Porosity: 93.2% | 107–500 | Non-cytotoxic, biocompatible, it facilitates the homogeneous growth of floclayer-type carbonated hydroxyapatite within a short period of immersion. Rapid cell growth with specific functions of hepatocytes per volume of substrates. They promote an increase in the hydrophilicity of the material, improving cell adhesion. | [20,66] |
| Hydroxyapatite hybrids | Electrospinning | Hydroxyapatite (Ca10(PO4)6(OH)2)–Silica (SiO2) | Surface area: 6.57 m2/g Pore volume: 0.025 cm3/g | 110 | Non-cytotoxic, biocompatible, bioactive, they have a high percentage of viability in a fibroblast lineage, stimulate cell growth, serve as cell support and allow cells to anchor. They promote the reduction in incision inflammation in vivo test after six weeks of surgical intervention. | [74] |
| Silver-containing nanofiber | Electrospinning | Silica (SiO2)-Silver (0.05, 0.1 and 0.15 Ag) Silver- Bioactive glass (2% B2O3, 68–69% SiO2, ~1 × 10−3 Ag2O, 29–30% CaO) | Properties not informed | 200–390 | They inhibit the proliferation of Escherichia coli with a long-term antibacterial effect, providing antibacterial potential to the wound bed. Non-cytotoxic, promoting cell growth over a wide concentration range. They allow the loading of drugs such as Tetracycline (TC) and have the ability to delay the release of TC and maintain antibacterial activity, inhibiting bacterial growth for a period of seven days. | [67,72,88] |
| Calcium-containing nanofiber | Electrospinning | Silica (100-X% SiO2)–Calcium (X% CaO), with X: 0, 20, 30, 40 | Surface area: 40–43.1 m2/g | 210–340 | Increases the production of human vascular endothelial growth factor (VEGF) in a human dermal fibroblast cell line (CD-18CO) and promotes improved wound healing when compared to control. | [68] |
| Boron-containing nanofiber | Electrospinning | Bioactive glass–Boron (2% B2O3, 68–69% SiO2, 29–30% CaO) | Properties not informed | 200–900 | Higher wound healing rates after 24 h of testing. The presence of boron promoted healing of 82% and increased cell proliferation. | [88] |
| Cobalt-containing nanofiber | Electrospinning | Bioactive glass–Cobalt (50% SiO2, 24% Na2O, 24% MgO, 2% CoO) | The ability to act as both a network modifier and a network former | 1000 | They provided more sustained ion release compared to bioactive glass particles alone. Exposure of fibroblasts to the conditioned medium of these composites did not have a deleterious effect on metabolic activity, but the cobalt-containing glasses stabilized HIF-1α and caused significantly increased expression of VEGF (not observed in controls without Co). | [69] |
| Copper-containing nanofiber | Electrospinning | Borate bioactive glass- copper (6% Na2O, 8% K2O, 8% MgO, 22% CaO, 54% B2O3, 2% P2O5, 3% CuO) | Thermal stability | 0.4–1.2 μm | Promising ability to stimulate angiogenesis and heal full-thickness skin defects. | [96] |
| Nanofiber | Method | Composition (mol) | Physicochemical Properties | Diameter (nm) | Biological Properties | Reference |
|---|---|---|---|---|---|---|
| Calcium Phosphate | Electrospinning, Solution Blow Spinning | Hydroxyapatite (Ca10(PO4)6(OH)2) β-Tricalcium phosphate (Ca₃(PO₄)₂) Hydroxyapatite (Ca10(PO4)6(OH)2)-Silica (SiO2) Hydroxyapatite (Ca10(PO4)6(OH)2)–CaO Hydroxyapatite-Calcium (66.3% Ca10(PO4)6(OH)2), 21.1% CaO, 12.6% CaCO3) | Low strength and fracture toughness Surface area: 6.57–8 m2/g Pore volume: 0.025 cm3/g Pore size: 15.75–25 nm | 100–460 | High bioactivity, non-cytotoxic, and good biocompatibility, in addition to having good drug control release properties. | [31,56,74,89,122,195] |
| Bioactive glass | Electrospinning, Solution Blow Spinning, Template-Assisted Sol–Gel | Binary glass (60% Si, 40% Ca) | Surface area: 144.60–579 m2/g Porosity: 63.8% Pore size: 3.5–45 nm Pore volume: 0.21 cm3 g−1 | 16–358 | Excellent biocompatibility, high bioactivity in SBF, high ALP activity, good degradation rate, promotes cell adhesion, and accelerates osteoblast proliferation and differentiation. | [32,55,154,156] |
| Wollastonite | Electrospinning, Hydrothermal Synthesis | β-wollastonite (β-CaSiO3) Wollastonite (CaSiO3)–Silica (SiO4)–Zinc (10% Zn) | High bending strength of 145.70 ± 2.74 MPa Porosity: 9.5–22.8% | 10–500 | Excellent bioactivity, good osteogenic differentiation of mesenchymal stromal cells, ability to release bioactive, and slowly degradable ions in inducing bone regeneration. | [128,164,170] |
| Hybridized carbon | Electrospinning, electrospinning/electrospraying | Carbon-Bioactive glass (89.65% C, 7.61% O, 2.28% Si, 0.10% P, 0.35% Ca) Carbon-Silica (5–10% SiO2) Carbon–Gold (1–2.5–5% Au) Carbon-Hydroxyapatite (34% C, 23% O, 11% P 32% Ca) | Higher dissolution rate High surface area and flexibility Porosity: 76% | 190–320 | Rapid cell proliferation and differentiation (indicating a strong osteoactive behavior), high ALP expression, biocompatible, and low level of cytotoxicity. | [54,117,179,181,182] |
| Therapeutic ions-containing nanofiber (Ce, Ga, Sr, Cu, Ca and Mn) | Electrospinning | Hydroxyapatite–Calcium (96.1% Ca10(PO4)6(OH)2), 1.4% CaO, 2.5% CaCO3)–Strontium (30% Sr) Bioactive glass (53% SiO2, 6% Na2O, 12% K2O, 5% MgO, 20% CaO e 4% P2O5) -Cerium-gallium (1–5% Ce and Ga) Barium titanate (BaTiO3)–Calcium-Manganese (10% Ca, 2% Mn) | Piezoelectricity, ion release and degradation behaviors. Pore size: 20–25 nm | 103–582 | Good biocompatibility, showed no cytotoxicity, improving bioactivity by promoting the activity of osteoblastic and endothelial cells, and inhibiting the formation of osteoclasts or bone resorption cells. | [119,191,195,197] |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
dos Santos Gomes, D.; de Sousa Victor, R.; de Sousa, B.V.; de Araújo Neves, G.; de Lima Santana, L.N.; Menezes, R.R. Ceramic Nanofiber Materials for Wound Healing and Bone Regeneration: A Brief Review. Materials 2022, 15, 3909. https://doi.org/10.3390/ma15113909
dos Santos Gomes D, de Sousa Victor R, de Sousa BV, de Araújo Neves G, de Lima Santana LN, Menezes RR. Ceramic Nanofiber Materials for Wound Healing and Bone Regeneration: A Brief Review. Materials. 2022; 15(11):3909. https://doi.org/10.3390/ma15113909
Chicago/Turabian Styledos Santos Gomes, Déborah, Rayssa de Sousa Victor, Bianca Viana de Sousa, Gelmires de Araújo Neves, Lisiane Navarro de Lima Santana, and Romualdo Rodrigues Menezes. 2022. "Ceramic Nanofiber Materials for Wound Healing and Bone Regeneration: A Brief Review" Materials 15, no. 11: 3909. https://doi.org/10.3390/ma15113909