Unveiling Therapeutic Targets for Esophageal Cancer: A Comprehensive Review
Abstract
:1. Introduction
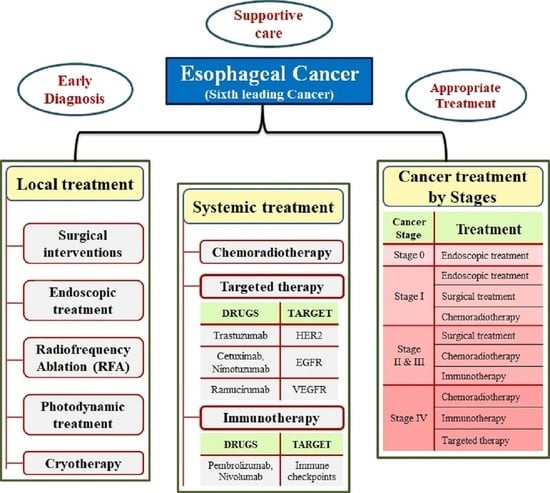
2. Local Treatment
2.1. Surgical Interventions
2.1.1. Esophagectomy
2.1.2. Types of Esophagectomy
Open Esophagectomy
Minimally Invasive Esophagectomy
Lymph Node Removal/Dissection
Resection
Risks and Complications of Esophagectomy
3. Treatments
3.1. Esophagogastrectomy
3.2. Endoscopic Treatment
3.2.1. Endoscopic Resection (ER)
3.2.2. Advances in Endoscopic Therapy
3.3. Radiofrequency Ablation (RFA)
3.4. Photodynamic Therapy
3.5. Cryotherapy/Cryoablation
4. Systemic Treatment
4.1. Chemo-Radiotherapy for Esophageal Cancer
4.2. Radiation Technique
4.2.1. Intensity-Modulated Radiotherapy (IMRT)
4.2.2. Intensity-Modulated Radiotherapy
4.2.3. Volumetric Modulated Arc Radiotherapy (VMAT)
4.2.4. Proton Beam Therapy (PBT)
4.3. Targeted Drug Therapy for EC
4.3.1. Human Epidermal Growth Factor Receptor 2
Trastuzumab
4.3.2. Epidermal Growth Factor Receptor
Cetuximab
Nimotuzumab
4.3.3. Vascular Endothelial Growth Factor
Ramucirumab
4.4. Immunotherapy for Esophageal Cancer
4.4.1. Immune Checkpoint Inhibitors
Nivolumab
Pembrolizumab
4.4.2. Toxicities Associated with Immunotherapy
5. Common Treatment Approaches
5.1. Cancer Treatment by Stage
5.2. Treating Esophageal Cancer by Stage
Treatment Options for Stage I Esophageal Cancer
5.3. Endoscopic Treatment
6. Treating Stages II and III Cancer of the Esophagus
7. Treating Stage IV of Esophagus Cancer
8. Post-Operative Complications and Rehabilitation Care for Esophageal Cancer
8.1. Pulmonary Complication
8.2. Reflux Esophagitis
8.3. Functional Gastric Emptying Disorder (FDGE)
9. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Yang, Y.-M.; Hong, P.; Xu, W.W.; He, Q.-Y.; Li, B. Advances in targeted therapy for esophageal cancer. Signal Transduct. Target. Ther. 2020, 5, 229. [Google Scholar] [CrossRef] [PubMed]
- Bray, F.; Ferlay, J.; Soerjomataram, I.; Siegel, R.L.; Torre, L.A.; Jemal, A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J. Clin. 2018, 68, 394–424. [Google Scholar] [CrossRef] [PubMed]
- Smyth, E.C.; Lagergren, J.; Fitzgerald, R.C.; Lordick, F.; Shah, M.A.; Lagergren, P.; Cunningham, D. Oesophageal cancer. Nat. Rev. Dis. Primers 2017, 3, 17048. [Google Scholar] [CrossRef]
- Chai, J. Introductory chapter: Esophagus and esophageal cancer. In Esophageal Cancer and Beyond; IntechOpen: London, UK, 2018. [Google Scholar]
- Hassan, M.S.; Makuru, V.; von Holzen, U.J.D.M.R. Targeted therapy in esophageal cancer. Dig. Med. Res. 2021, 4, 29. [Google Scholar] [CrossRef]
- Lowe, D.; Kudaravalli, P.; Hsu, R.J.S. Barrett metaplasia. Lancet 2020, 356, 2079–2085. [Google Scholar]
- Yang, J.; Liu, X.; Cao, S.; Dong, X.; Rao, S.; Cai, K. Understanding Esophageal Cancer: The Challenges and Opportunities for the Next Decade. Front. Oncol. 2020, 10, 1727. [Google Scholar] [CrossRef]
- Watanabe, M.; Otake, R.; Kozuki, R.; Toihata, T.; Takahashi, K.; Okamura, A.; Imamura, Y. Recent progress in multidisciplinary treatment for patients with esophageal cancer. Surg. Today 2020, 50, 12–20. [Google Scholar] [CrossRef]
- Ilson, D.H. Is there a future for EGFR targeted agents in esophageal cancer? Ann. Oncol. 2018, 29, 1343–1344. [Google Scholar] [CrossRef]
- Santos, E.D.S.; Nogueira, K.A.B.; Fernandes, L.C.C.; Martins, J.R.P.; Reis, A.V.F.; Neto, J.B.V.; Júnior, I.; Pessoa, C.; Petrilli, R.; Eloy, J.O. EGFR targeting for cancer therapy: Pharmacology and immunoconjugates with drugs and nanoparticles. Int. J. Pharm. 2021, 592, 12. [Google Scholar] [CrossRef]
- Triantafyllou, T.; Wijnhoven, B.P.L. Current status of esophageal cancer treatment. Chin. J. Cancer Res. 2020, 32, 271–286. [Google Scholar] [CrossRef]
- Bennett, A.N.; Huang, R.X.; He, Q.; Lee, N.P.; Sung, W.K.; Chan, K.H.K. Drug repositioning for esophageal squamous cell carcinoma. Front. Genet. 2022, 13, 991842. [Google Scholar] [CrossRef]
- Xu, C.; Lin, S.H. Esophageal cancer: Comparative effectiveness of treatment options. Comp. Eff. Res. 2016, 6, 1–12. [Google Scholar]
- Yu, J.; Kim, J.H.; Kim, S.-B.; Park, S.R.; Kim, Y.-H.; Kim, H.R.; Lee, H.J.; Song, H.J.; Song, K.J.; Jang, J.Y.; et al. Role of Esophagectomy after Chemoradiation Therapy in Patients with Locally Advanced Squamous Cell Carcinoma: A Comparative Analysis Stratified by Clinical Response to Chemoradiation Therapy. Cancer Res. Treat. 2022, 54, 1148–1156. [Google Scholar] [CrossRef] [PubMed]
- Bedenne, L.; Michel, P.; Bouché, O.; Milan, C.; Mariette, C.; Conroy, T.; Pezet, D.; Roullet, B.; Seitz, J.F.; Herr, J.P.; et al. Chemoradiation followed by surgery compared with chemoradiation alone in squamous cancer of the esophagus: FFCD 9102. J. Clin. Oncol. 2007, 25, 1160–1168. [Google Scholar] [CrossRef] [PubMed]
- Vellayappan, B.A.; Soon, Y.Y.; Ku, G.Y.; Leong, C.N.; Lu, J.J.; Tey, J.C. Chemoradiotherapy versus chemoradiotherapy plus surgery for esophageal cancer. Cochrane Database Syst. Rev. 2017, 8, Cd010511. [Google Scholar] [CrossRef]
- Lin, D.; Khan, U.; Goetze, T.O.; Reizine, N.; Goodman, K.A.; Shah, M.A.; Catenacci, D.V.; Al-Batran, S.-E.; Posey, J.A. Gastroesophageal Junction Adenocarcinoma: Is There an Optimal Management? Am. Soc. Clin. Oncol. Educ. Book 2019, 39, e88–e95. [Google Scholar] [CrossRef] [PubMed]
- Borggreve, A.S.; Kingma, B.F.; Domrachev, S.A.; Koshkin, M.A.; Ruurda, J.P.; van Hillegersberg, R.; Takeda, F.R.; Goense, L. Surgical treatment of esophageal cancer in the era of multimodality management. Ann. N. Y. Acad. Sci. 2018, 1434, 192–209. [Google Scholar] [CrossRef]
- Han, Y.; Zhang, Y.; Li, H. Application of different intrathoracic esophagogastric anastomosis in surgery for esophageal cancer. Zhonghua Wei Chang Wai Ke Za Zhi 2018, 21, 995–1000. [Google Scholar] [PubMed]
- Markar, S.R.; Lagergren, J. Surgical and Surgeon-Related Factors Related to Long-Term Survival in Esophageal Cancer: A Review. Ann. Surg. Oncol. 2020, 27, 718–723. [Google Scholar] [CrossRef]
- Yanasoot, A.; Yolsuriyanwong, K.; Ruangsin, S.; Laohawiriyakamol, S.; Sunpaweravong, S. Costs and benefits of different methods of esophagectomy for esophageal cancer. Asian Cardiovasc. Thorac. Ann. 2017, 25, 513–517. [Google Scholar] [CrossRef] [PubMed]
- Gurusamy, K.S.; Pallari, E.; Midya, S.; Mughal, M. Laparoscopic versus open transhiatal oesophagectomy for oesophageal cancer. Cochrane Database Syst. Rev. 2016, 3, Cd011390. [Google Scholar] [CrossRef] [PubMed]
- Van Hillegersberg, R.; Seesing, M.F.; Brenkman, H.J.; Ruurda, J.P. Robot-assisted minimally invasive esophagectomy. Chirurg 2017, 88, 7–11. [Google Scholar] [CrossRef] [PubMed]
- Van der Sluis, P.C.; van Hillegersberg, R. Robot assisted minimally invasive esophagectomy (RAMIE) for esophageal cancer. Best. Pract. Res. Clin. Gastroenterol. 2018, 36–37, 81–83. [Google Scholar] [CrossRef] [PubMed]
- Achim, F.; Constantinoiu, S. Recent Advances in Minimally Invasive Esophagectomy. Chirurgia 2018, 113, 19–37. [Google Scholar] [CrossRef] [PubMed]
- Van den Berg, J.W.; Luketich, J.D.; Cheong, E. Oesophagectomy: The expanding role of minimally invasive surgery in oesophageal cancer. Best. Pract. Res. Clin. Gastroenterol. 2018, 36–37, 75–80. [Google Scholar] [CrossRef]
- Van der Sluis, P.C.; Schizas, D.; Liakakos, T.; van Hillegersberg, R. Minimally Invasive Esophagectomy. Dig. Surg. 2020, 37, 93–100. [Google Scholar] [CrossRef]
- Yibulayin, W.; Abulizi, S.; Lv, H.; Sun, W. Minimally invasive oesophagectomy versus open esophagectomy for resectable esophageal cancer: A meta-analysis. World J. Surg. Oncol. 2016, 14, 304. [Google Scholar] [CrossRef]
- Na, K.J.; Kang, C.H. Current Issues in Minimally Invasive Esophagectomy. Korean J. Thorac. Cardiovasc. Surg. 2020, 53, 152–159. [Google Scholar] [CrossRef]
- Brady, J.J.; Witek, T.D.; Luketich, J.D.; Sarkaria, I.S. Patient reported outcomes (PROs) after minimally invasive and open esophagectomy. J. Thorac. Dis. 2020, 12, 6920–6924. [Google Scholar] [CrossRef]
- Van der Schaaf, M.; Johar, A.; Wijnhoven, B.; Lagergren, P.; Lagergren, J. Extent of lymph node removal during esophageal cancer surgery and survival. J. Natl. Cancer Inst. 2015, 107, djv043. [Google Scholar] [CrossRef]
- Deng, J.; Su, Q.; Ren, Z.; Wen, J.; Xue, Z.; Zhang, L.; Chu, X. Comparison of short-term outcomes between minimally invasive McKeown and Ivor Lewis esophagectomy for esophageal or junctional cancer: A systematic review and meta-analysis. Onco Targets Ther. 2018, 11, 6057–6069. [Google Scholar] [CrossRef] [PubMed]
- Zhu, Z.Y.; Yong, X.; Luo, R.J.; Wang, Y.Z. Clinical analysis of minimally invasive McKeown esophagectomy in a single center by a single medical group. J. Zhejiang Univ. Sci. B 2018, 19, 718–725. [Google Scholar] [CrossRef] [PubMed]
- Mu, J.W.; Gao, S.G.; Xue, Q.; Mao, Y.S.; Wang, D.L.; Zhao, J.; Gao, Y.S.; Huang, J.F.; He, J. Updated experiences with minimally invasive McKeown esophagectomy for esophageal cancer. World J. Gastroenterol. 2015, 21, 12873–12881. [Google Scholar] [CrossRef] [PubMed]
- Markar, S.; Santoni, G.; Maret-Ouda, J.; Lagergren, J. Hospital volume of esophageal cancer surgery in relation to outcomes from primary anti-reflux surgery. Dis. Esophagus 2021, 34, doaa075. [Google Scholar] [CrossRef]
- Chang, D.; Church, J. Evaluating the health-related quality of life of esophageal cancer patients. Pract. Radiat. Oncol. 2014, 4, 181–186. [Google Scholar] [CrossRef]
- Gockel, I.; Niebisch, S.; Ahlbrand, C.J.; Hoffmann, C.; Möhler, M.; Düber, C.; Lang, H.; Heid, F. Risk and Complication Management in Esophageal Cancer Surgery: A Review of the Literature. Thorac. Cardiovasc. Surg. 2016, 64, 596–605. [Google Scholar] [CrossRef]
- Mafune, T.; Mikami, S.; Otsubo, T.; Saji, O.; Matsushita, T.; Enomoto, T.; Maki, F.; Tochimoto, S. An Investigation of Factors Related to Food Intake Ability and Swallowing Difficulty After Surgery for Thoracic Esophageal Cancer. Dysphagia 2019, 34, 592–599. [Google Scholar] [CrossRef]
- Takatsu, J.; Higaki, E.; Hosoi, T.; Yoshida, M.; Yamamoto, M.; Abe, T.; Shimizu, Y. Clinical benefits of a swallowing intervention for esophageal cancer patients after esophagectomy. Dis. Esophagus 2021, 34, doaa094. [Google Scholar] [CrossRef]
- Buckle, G.C.; Mahapatra, R.; Mwachiro, M.; Akoko, L.; Mmbaga, E.J.; White, R.E.; Bent, S.; Van Loon, K. Optimal management of esophageal cancer in Africa: A systemic review of treatment strategies. Int. J. Cancer 2021, 148, 1115–1131. [Google Scholar] [CrossRef]
- Jacobs, M.; Macefield, R.C.; Elbers, R.G.; Sitnikova, K.; Korfage, I.J.; Smets, E.M.; Henselmans, I.; van Berge Henegouwen, M.I.; de Haes, J.C.; Blazeby, J.M.; et al. Meta-analysis shows clinically relevant and long-lasting deterioration in health-related quality of life after esophageal cancer surgery. Qual. Life Res. 2014, 23, 1097–1115. [Google Scholar] [CrossRef]
- Schlottmann, F.; Strassle, P.D.; Nayyar, A.; Herbella, F.A.M.; Cairns, B.A.; Patti, M.G. Postoperative outcomes of esophagectomy for cancer in elderly patients. J. Surg. Res. 2018, 229, 9–14. [Google Scholar] [CrossRef] [PubMed]
- Kauppila, J.H.; Lagergren, J. The surgical management of esophago-gastric junctional cancer. Surg. Oncol. 2016, 25, 394–400. [Google Scholar] [CrossRef] [PubMed]
- Mönig, S.P.; Chevallay, M.; Niclauss, N.; Toso, C.; Frossard, J.L.; Koessler, T.; Jung, M.K. Esophageal and esophago-gastric junction cancer : Management and multimodal treatment. Rev. Med. Suisse 2020, 16, 1292–1299. [Google Scholar]
- Haverkamp, L.; Seesing, M.F.; Ruurda, J.P.; Boone, J.; Hillegersberg, R.V. Worldwide trends in surgical techniques in the treatment of esophageal and gastroesophageal junction cancer. Dis. Esophagus 2017, 30, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Xu, Q.-L.; Li, H.; Zhu, Y.-J.; Xu, G. The treatments and postoperative complications of esophageal cancer: A review. J. Cardiothorac. Surg. 2020, 15, 163. [Google Scholar] [CrossRef]
- Kim, H.K.; Ko, W.J.; Kwon, C.-I.; Song, G.W.; Yoo, I.K.; Song, J.H.; Kim, H.S.; Cho, J.Y. Endoscopic Submucosal Dissection Followed by Concurrent Chemoradiotherapy in Patients with Early Esophageal Cancer with a High Risk of Lymph Node Metastasis. Clin. Endosc. 2019, 52, 502–505. [Google Scholar] [CrossRef]
- Li, Q.; Zhong, Y.; Chen, W.; He, M.J.; Zhou, P.H. New Endoscopic Diagnosis and Treatment Options for Early Esophageal Cancer. J. Gastroint. Dig. Syst. 2012, 2, 2. [Google Scholar] [CrossRef]
- Naveed, M.; Kubiliun, N. Endoscopic Treatment of Early-Stage Esophageal Cancer. Curr. Oncol. Rep. 2018, 20, 71. [Google Scholar] [CrossRef]
- Harada, K.; Rogers, J.E.; Iwatsuki, M.; Yamashita, K.; Baba, H.; Ajani, J.A. Recent advances in treating oesophageal cancer. F1000Research 2020, 9, 1189. [Google Scholar] [CrossRef]
- Berger, A.; Rahmi, G.; Perrod, G.; Pioche, M.; Canard, J.M.; Cesbron-Métivier, E.; Boursier, J.; Samaha, E.; Vienne, A.; Lépilliez, V.; et al. Long-term follow-up after endoscopic resection for superficial esophageal squamous cell carcinoma: A multicenter Western study. Endoscopy 2019, 51, 298–306. [Google Scholar] [CrossRef]
- Sami, S.S.; Subramanian, V.; Butt, W.M.; Bejkar, G.; Coleman, J.; Mannath, J.; Ragunath, K. High definition versus standard definition white light endoscopy for detecting dysplasia in patients with Barrett’s esophagus. Dis. Esophagus 2015, 28, 742–749. [Google Scholar] [CrossRef]
- Ahmed, O.; Ajani, J.A.; Lee, J.H. Endoscopic management of esophageal cancer. World J. Gastrointest. Oncol. 2019, 11, 830–841. [Google Scholar] [CrossRef] [PubMed]
- Mocanu, A.; Bârla, R.; Hoara, P.; Constantinoiu, S. Endoscopic palliation of advanced esophageal cancer. J. Med. Life 2015, 8, 193–201. [Google Scholar] [PubMed]
- Fokas, E.; Rödel, C. Definitive, Preoperative, and Palliative Radiation Therapy of Esophageal Cancer. Visc. Med. 2015, 31, 347–353. [Google Scholar] [CrossRef]
- Kruszewski, W. Endoscopic methods in the treatment of early-stage esophageal cancer. Videosurg. Other Miniinvasive Tech. 2014, 9, 125–130. [Google Scholar] [CrossRef] [PubMed]
- Inoue, H.; Endo, M.; Takeshita, K.; Yoshino, K.; Muraoka, Y.; Yoneshima, H. A new simplified technique of endoscopic esophageal mucosal resection using a cap-fitted panendoscope (EMRC). Surg. Endosc. 1992, 6, 264–265. [Google Scholar] [CrossRef]
- Soehendra, N.; Seewald, S.; Groth, S.; Omar, S.; Seitz, U.; Zhong, Y.; de Weerth, A.; Thonke, F.; Schroeder, S. Use of modified multiband ligator facilitates circumferential EMR in Barrett’s esophagus (with video). Gastrointest. Endosc. 2006, 63, 847–852. [Google Scholar] [CrossRef]
- Di Pietro, M.; Canto, M.I.; Fitzgerald, R.C. Endoscopic Management of Early Adenocarcinoma and Squamous Cell Carcinoma of the Esophagus: Screening, Diagnosis, and Therapy. Gastroenterology 2018, 154, 421–436. [Google Scholar] [CrossRef]
- Ning, B.; Abdelfatah, M.M.; Othman, M.O. Endoscopic submucosal dissection and endoscopic mucosal resection for early stage esophageal cancer. Ann. Cardiothorac. Surg. 2017, 6, 88–98. [Google Scholar] [CrossRef]
- Aadam, A.A.; Abe, S. Endoscopic submucosal dissection for superficial esophageal cancer. Dis. Esophagus 2018, 31, doy021. [Google Scholar] [CrossRef]
- Nishizawa, T.; Suzuki, H. Long-Term Outcomes of Endoscopic Submucosal Dissection for Superficial Esophageal Squamous Cell Carcinoma. Cancers 2020, 12, 2849. [Google Scholar] [CrossRef] [PubMed]
- Guo, H.M.; Zhang, X.Q.; Chen, M.; Huang, S.L.; Zou, X.P. Endoscopic submucosal dissection vs endoscopic mucosal resection for superficial esophageal cancer. World J. Gastroenterol. 2014, 20, 5540–5547. [Google Scholar] [CrossRef] [PubMed]
- Probst, A.; Aust, D.; Märkl, B.; Anthuber, M.; Messmann, H. Early esophageal cancer in Europe: Endoscopic treatment by endoscopic submucosal dissection. Endoscopy 2015, 47, 113–121. [Google Scholar] [CrossRef]
- Pimentel-Nunes, P.; Dinis-Ribeiro, M.; Ponchon, T.; Repici, A.; Vieth, M.; De Ceglie, A.; Amato, A.; Berr, F.; Bhandari, P.; Bialek, A.; et al. Endoscopic submucosal dissection: European Society of Gastrointestinal Endoscopy (ESGE) Guideline. Endoscopy 2015, 47, 829–854. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.A.; Shah, P.M. Screening and prevention strategies and endoscopic management of early esophageal cancer. Chin. Clin. Oncol. 2017, 6, 50. [Google Scholar] [CrossRef]
- Tuttle, R.; Nurkin, S.J.; Hochwald, S.N. Ablative therapy for esophageal dysplasia and early malignancy: Focus on RFA. Biomed. Res. Int. 2014, 2014, 642063. [Google Scholar] [CrossRef]
- Belghazi, K.; Bergman, J.; Pouw, R.E. Endoscopic Resection and Radiofrequency Ablation for Early Esophageal Neoplasia. Dig. Dis. 2016, 34, 469–475. [Google Scholar] [CrossRef]
- Yano, T.; Hatogai, K.; Morimoto, H.; Yoda, Y.; Kaneko, K. Photodynamic therapy for esophageal cancer. Ann. Transl. Med. 2014, 2, 29. [Google Scholar] [CrossRef]
- Wu, H.; Minamide, T.; Yano, T. Role of photodynamic therapy in the treatment of esophageal cancer. Dig. Endosc. 2019, 31, 508–516. [Google Scholar] [CrossRef]
- Lal, P.; Thota, P.N. Cryotherapy in the management of premalignant and malignant conditions of the esophagus. World J. Gastroenterol. 2018, 24, 4862–4869. [Google Scholar] [CrossRef]
- Dhaliwal, A.; Saghir, S.M.; Mashiana, H.S.; Braseth, A.; Dhindsa, B.S.; Ramai, D.; Taunk, P.; Gomez-Esquivel, R.; Dam, A.; Klapman, J.; et al. Endoscopic cryotherapy: Indications, techniques, and outcomes involving the gastrointestinal tract. World J. Gastrointest. Endosc. 2022, 14, 17–28. [Google Scholar] [CrossRef]
- Hanada, Y.; Leggett, C.L.; Iyer, P.G.; Linn, B.; Mangels-Dick, T.; Wang, K.K. Spray cryotherapy prevents need for palliative stenting in patients with esophageal cancer-associated dysphagia. Dis. Esophagus 2021, 35, doab051. [Google Scholar] [CrossRef] [PubMed]
- American Cancer Society Medical Information: Chemotherapy for Esophageal Cancer. Available online: https://www.cancer.org/cancer/esophagus-cancer/treating/chemotherapy.html (accessed on 25 August 2023).
- Radiological Society of North America: Esophageal Cancer. Available online: https://www.radiologyinfo.org/en/info/esophageal-cancer (accessed on 1 September 2023).
- Ma, M.W.; Gao, X.S.; Gu, X.B.; Xie, M.; Cui, M.; Zhang, M.; Liu, L.; Yin, H.; Chen, L.Q. The role of definitive chemoradiotherapy versus surgery as initial treatments for potentially resectable esophageal carcinoma. World J. Surg. Oncol. 2018, 16, 018–1470. [Google Scholar] [CrossRef]
- Cleveland Clinic: Esophageal Cancer. Available online: https://my.clevelandclinic.org/health/diseases/6137-esophageal-cancer (accessed on 19 August 2023).
- Li, Q.-Q.; Liu, M.-Z.; Hu, Y.-H.; Liu, H.; He, Z.-Y.; Lin, H.-X. Definitive concomitant chemoradiotherapy with docetaxel and cisplatin in squamous esopheageal carcinoma. Dis. Esophagus 2010, 23, 253–259. [Google Scholar] [CrossRef]
- Herskovic, A.; Martz, K.; Al-Sarraf, M.; Leichman, L.; Brindle, J.; Vaitkevicius, V.; Cooper, J.; Byhardt, R.; Davis, L.; Emami, B. Combined Chemotherapy and Radiotherapy Compared with Radiotherapy Alone in Patients with Cancer of the Esophagus. N. Engl. J. Med. 1992, 326, 1593–1598. [Google Scholar] [CrossRef] [PubMed]
- Conroy, T.; Galais, M.-P.; Raoul, J.-L.; Bouché, O.; Gourgou-Bourgade, S.; Douillard, J.-Y.; Etienne, P.-L.; Boige, V.; Martel-Lafay, I.; Michel, P.; et al. Definitive chemoradiotherapy with FOLFOX versus fluorouracil and cisplatin in patients with oesophageal cancer (PRODIGE5/ACCORD17): Final results of a randomised, phase 2/3 trial. Lancet Oncol. 2014, 15, 305–314. [Google Scholar] [CrossRef]
- Cooper, J.S.; Guo, M.D.; Herskovic, A.; Macdonald, J.S.; Martenson, J.; James, A.; Al-Sarraf, M.; Byhardt, R.; Russell, A.H.; Beitler, J.J.; et al. Chemoradiotherapy of Locally Advanced Esophageal CancerLong-term Follow-up of a Prospective Randomized Trial (RTOG 85-01). JAMA 1999, 281, 1623–1627. [Google Scholar] [CrossRef] [PubMed]
- Shapiro, J.; van Lanschot, J.J.B.; Hulshof, M.C.C.M.; van Hagen, P.; van Berge Henegouwen, M.I.; Wijnhoven, B.P.L.; van Laarhoven, H.W.M.; Nieuwenhuijzen, G.A.P.; Hospers, G.A.P.; Bonenkamp, J.J.; et al. Neoadjuvant chemoradiotherapy plus surgery versus surgery alone for oesophageal or junctional cancer (CROSS): Long-term results of a randomised controlled trial. Lancet Oncol. 2015, 16, 1090–1098. [Google Scholar] [CrossRef]
- Lin, S.H.; Wang, L.; Myles, B.; Thall, P.F.; Hofstetter, W.L.; Swisher, S.G.; Ajani, J.A.; Cox, J.D.; Komaki, R.; Liao, Z. Propensity Score-based Comparison of Long-term Outcomes With 3-Dimensional Conformal Radiotherapy vs Intensity-Modulated Radiotherapy for Esophageal Cancer. Int. J. Radiat. Oncol. Biol. Phys. 2012, 84, 1078–1085. [Google Scholar] [CrossRef]
- Wang, D.; Yang, Y.; Zhu, J.; Li, B.; Chen, J.; Yin, Y. 3D-Conformal RT, Fixed-Field IMRT and RapidArc, Which One is Better for Esophageal Carcinoma Treated with Elective Nodal Irradiation. Technol. Cancer Res. Treat. 2011, 10, 487–494. [Google Scholar] [CrossRef]
- Vivekanandan, N.; Sriram, P.; Syam Kumar, S.A.; Bhuvaneswari, N.; Saranya, K. Volumetric modulated arc radiotherapy for esophageal cancer. Med. Dosim. 2012, 37, 108–113. [Google Scholar] [CrossRef] [PubMed]
- Zhang, W.-Z.; Zhai, T.-T.; Lu, J.-Y.; Chen, J.-Z.; Chen, Z.-J.; Li, D.-R.; Chen, C.-Z. Volumetric Modulated Arc Therapy vs. c-IMRT for the Treatment of Upper Thoracic Esophageal Cancer. PLoS ONE 2015, 10, e0121385. [Google Scholar] [CrossRef]
- Ogitani, Y.; Aida, T.; Hagihara, K.; Yamaguchi, J.; Ishii, C.; Harada, N.; Soma, M.; Okamoto, H.; Oitate, M.; Arakawa, S.; et al. DS-8201a, A Novel HER2-Targeting ADC with a Novel DNA Topoisomerase I Inhibitor, Demonstrates a Promising Antitumor Efficacy with Differentiation from T-DM1. Clin. Cancer Res. 2016, 22, 5097–5108. [Google Scholar] [CrossRef]
- Fatehi Hassanabad, A.; Chehade, R.; Breadner, D.; Raphael, J. Esophageal carcinoma: Towards targeted therapies. Cell Oncol. 2020, 43, 195–209. [Google Scholar] [CrossRef] [PubMed]
- Pozzi, V.; Campagna, R.; Sartini, D.; Emanuelli, M. Nicotinamide N-Methyltransferase as Promising Tool for Management of Gastrointestinal Neoplasms. Biomolecules 2022, 12, 1173. [Google Scholar] [CrossRef]
- Van Haren, M.J.; Zhang, Y.; Thijssen, V.; Buijs, N.; Gao, Y.; Mateuszuk, L.; Fedak, F.A.; Kij, A.; Campagna, R.; Sartini, D.; et al. Macrocyclic peptides as allosteric inhibitors of nicotinamide N-methyltransferase (NNMT). RSC Chem. Biol. 2021, 2, 1546–1555. [Google Scholar] [CrossRef]
- Abdo, J.; Agrawal, D.K.; Mittal, S.K. “Targeted” Chemotherapy for Esophageal Cancer. Front. Oncol. 2017, 7, 63. [Google Scholar] [CrossRef]
- Bang, Y.J.; Van Cutsem, E.; Feyereislova, A.; Chung, H.C.; Shen, L.; Sawaki, A.; Lordick, F.; Ohtsu, A.; Omuro, Y.; Satoh, T.; et al. Trastuzumab in combination with chemotherapy versus chemotherapy alone for treatment of HER2-positive advanced gastric or gastro-oesophageal junction cancer (ToGA): A phase 3, open-label, randomised controlled trial. Lancet 2010, 376, 687–697. [Google Scholar] [CrossRef]
- Van Cutsem, E.; Bang, Y.J.; Feng-Yi, F.; Xu, J.M.; Lee, K.W.; Jiao, S.C.; Chong, J.L.; López-Sanchez, R.I.; Price, T.; Gladkov, O.; et al. HER2 screening data from ToGA: Targeting HER2 in gastric and gastroesophageal junction cancer. Gastric Cancer 2015, 18, 476–484. [Google Scholar] [CrossRef]
- Almhanna, K.; Meredith, K.L.; Hoffe, S.E.; Shridhar, R.; Coppola, D. Targeting the human epidermal growth factor receptor 2 in esophageal cancer. Cancer Control 2013, 20, 111–116. [Google Scholar] [CrossRef]
- Iqbal, N.; Iqbal, N. Human Epidermal Growth Factor Receptor 2 (HER2) in Cancers: Overexpression and Therapeutic Implications. Mol. Biol. Int. 2014, 2014, 852748. [Google Scholar] [CrossRef] [PubMed]
- Gowryshankar, A.; Nagaraja, V.; Eslick, G.D. HER2 status in Barrett’s esophagus & esophageal cancer: A meta analysis. J. Gastrointest. Oncol. 2014, 5, 25–35. [Google Scholar] [CrossRef] [PubMed]
- Zhao, D.; Klempner, S.J.; Chao, J. Progress and challenges in HER2-positive gastroesophageal adenocarcinoma. J. Hematol. Oncol. 2019, 12, 50. [Google Scholar] [CrossRef] [PubMed]
- Doi, T.; Shitara, K.; Naito, Y.; Shimomura, A.; Fujiwara, Y.; Yonemori, K.; Shimizu, C.; Shimoi, T.; Kuboki, Y.; Matsubara, N.; et al. Safety, pharmacokinetics, and antitumour activity of trastuzumab deruxtecan (DS-8201), a HER2-targeting antibody-drug conjugate, in patients with advanced breast and gastric or gastro-oesophageal tumours: A phase 1 dose-escalation study. Lancet Oncol. 2017, 18, 1512–1522. [Google Scholar] [CrossRef] [PubMed]
- Wagner, A.D.; Grabsch, H.I.; Mauer, M.; Marreaud, S.; Caballero, C.; Thuss-Patience, P.; Mueller, L.; Elme, A.; Moehler, M.H.; Martens, U.; et al. EORTC-1203-GITCG—The “INNOVATION”-trial: Effect of chemotherapy alone versus chemotherapy plus trastuzumab, versus chemotherapy plus trastuzumab plus pertuzumab, in the perioperative treatment of HER2 positive, gastric and gastroesophageal junction adenocarcinoma on pathologic response rate: A randomized phase II-intergroup trial of the EORTC-Gastrointestinal Tract Cancer Group, Korean Cancer Study Group and Dutch Upper GI-Cancer group. BMC Cancer 2019, 19, 494. [Google Scholar] [CrossRef]
- Gerson, J.N.; Skariah, S.; Denlinger, C.S.; Astsaturov, I. Perspectives of HER2-targeting in gastric and esophageal cancer. Expert. Opin. Investig. Drugs 2017, 26, 531–540. [Google Scholar] [CrossRef]
- Chong, C.R.; Jänne, P.A. The quest to overcome resistance to EGFR-targeted therapies in cancer. Nat. Med. 2013, 19, 1389–1400. [Google Scholar] [CrossRef]
- Yamaoka, T.; Ohba, M.; Ohmori, T. Molecular-Targeted Therapies for Epidermal Growth Factor Receptor and Its Resistance Mechanisms. Int. J. Mol. Sci. 2017, 18, 2420. [Google Scholar] [CrossRef]
- Huang, Z.H.; Ma, X.W.; Zhang, J.; Li, X.; Lai, N.L.; Zhang, S.X. Cetuximab for esophageal cancer: An updated meta-analysis of randomized controlled trials. BMC Cancer 2018, 18, 1170. [Google Scholar] [CrossRef]
- Ruhstaller, T.; Thuss-Patience, P.; Hayoz, S.; Schacher, S.; Knorrenschild, J.R.; Schnider, A.; Plasswilm, L.; Budach, W.; Eisterer, W.; Hawle, H.; et al. Neoadjuvant chemotherapy followed by chemoradiation and surgery with and without cetuximab in patients with resectable esophageal cancer: A randomized, open-label, phase III trial (SAKK 75/08). Ann. Oncol. 2018, 29, 1386–1393. [Google Scholar] [CrossRef]
- Rades, D.; Bartscht, T.; Hunold, P.; Schmidberger, H.; König, L.; Debus, J.; Belka, C.; Homann, N.; Spillner, P.; Petersen, C.; et al. Radiochemotherapy with or without cetuximab for unresectable esophageal cancer: Final results of a randomized phase 2 trial (LEOPARD-2). Strahlenther. Und Onkol. 2020, 196, 795–804. [Google Scholar] [CrossRef] [PubMed]
- Zhang, X.; Jia, J.; Lu, M.; Wang, X.; Gong, J.; Li, J.; Li, J.; Li, Y.; Zhang, X.; Lu, Z.; et al. Nimotuzumab Plus Paclitaxel and Cisplatin as a 1(st)-Line Treatment for Esophageal Cancer: Long Term Follow-up of a Phase II Study. J. Cancer 2019, 10, 1409–1416. [Google Scholar] [CrossRef] [PubMed]
- Qi, S.; Mao, Y.; Jiang, M. A phase I study evaluating combined nimotuzumab and neoadjuvant chemoradiotherapy followed by surgery in locally advanced esophageal cancer. Cancer Chemother. Pharmacol. 2019, 84, 1115–1123. [Google Scholar] [CrossRef] [PubMed]
- Han, X.; Lu, N.; Pan, Y.; Xu, J. Nimotuzumab Combined with Chemotherapy is a Promising Treatment for Locally Advanced and Metastatic Esophageal Cancer. Med. Sci. Monit. 2017, 23, 412–418. [Google Scholar] [CrossRef]
- Kleespies, A.; Guba, M.; Jauch, K.W.; Bruns, C.J. Vascular endothelial growth factor in esophageal cancer. J. Surg. Oncol. 2004, 87, 95–104. [Google Scholar] [CrossRef] [PubMed]
- Peng, J.; Shao, N.; Peng, H.; Chen, L.Q. Prognostic significance of vascular endothelial growth factor expression in esophageal carcinoma: A meta-analysis. J. Buon 2013, 18, 398–406. [Google Scholar]
- Khan, U.; Shah, M.A. Ramucirumab for the treatment of gastric or gastro-esophageal junction cancer. Expert. Opin. Biol. Ther. 2019, 19, 1135–1141. [Google Scholar] [CrossRef]
- Vennepureddy, A.; Singh, P.; Rastogi, R.; Atallah, J.P.; Terjanian, T. Evolution of ramucirumab in the treatment of cancer—A review of literature. J. Oncol. Pharm. Pract. 2017, 23, 525–539. [Google Scholar] [CrossRef] [PubMed]
- Abbas, G.; Krasna, M. Overview of esophageal cancer. Ann. Cardiothorac. Surg. 2017, 6, 131–136. [Google Scholar] [CrossRef]
- De Mello, R.A.; Lordick, F.; Muro, K.; Janjigian, Y.Y. Current and Future Aspects of Immunotherapy for Esophageal and Gastric Malignancies. Am. Soc. Clin. Oncol. Educ. Book. 2019, 39, 237–247. [Google Scholar] [CrossRef]
- Gajewski, T.F.; Schreiber, H.; Fu, Y.X. Innate and adaptive immune cells in the tumor microenvironment. Nat. Immunol. 2013, 14, 1014–1022. [Google Scholar] [CrossRef]
- Sharma, P.; Allison, J.P. The future of immune checkpoint therapy. Science 2015, 348, 56–61. [Google Scholar] [CrossRef] [PubMed]
- Topalian, S.L.; Drake, C.G.; Pardoll, D.M. Immune checkpoint blockade: A common denominator approach to cancer therapy. Cancer Cell 2015, 27, 450–461. [Google Scholar] [CrossRef] [PubMed]
- Ricklefs, F.L.; Alayo, Q.; Krenzlin, H.; Mahmoud, A.B.; Speranza, M.C.; Nakashima, H.; Hayes, J.L.; Lee, K.; Balaj, L.; Passaro, C.; et al. Immune evasion mediated by PD-L1 on glioblastoma-derived extracellular vesicles. Sci. Adv. 2018, 4, eaar2766. [Google Scholar] [CrossRef] [PubMed]
- Shi, T.; Ma, Y.; Yu, L.; Jiang, J.; Shen, S.; Hou, Y.; Wang, T. Cancer immunotherapy: A focus on the regulation of immune checkpoints. Int. J. Mol. Sci. 2018, 19, 1389. [Google Scholar] [CrossRef] [PubMed]
- Kim, E.S.; Kim, J.E.; Patel, M.A.; Mangraviti, A.; Ruzevick, J.; Lim, M.J.J.o.i.r. Immune checkpoint modulators: An emerging antiglioma armamentarium. J. Immunol. Res. 2016, 2016, 4683607. [Google Scholar] [CrossRef]
- Pardoll, D.M. The blockade of immune checkpoints in cancer immunotherapy. Cancer 2012, 12, 252–264. [Google Scholar] [CrossRef]
- Vivaldi, C.; Catanese, S.; Massa, V.; Pecora, I.; Salani, F.; Santi, S.; Lencioni, M.; Vasile, E.; Falcone, A.; Fornaro, L. Immune checkpoint inhibitors in esophageal cancers: Are we finally finding the right path in the mist? Int. J. Mol. Sci. 2020, 21, 1658. [Google Scholar] [CrossRef]
- Kojima, T.; Shah, M.A.; Muro, K.; Francois, E.; Adenis, A.; Hsu, C.-H.; Doi, T.; Moriwaki, T.; Kim, S.-B.; Lee, S.-H.; et al. Randomized Phase III KEYNOTE-181 Study of Pembrolizumab Versus Chemotherapy in Advanced Esophageal Cancer. J. Clin. Oncol. 2020, 38, 4138–4148. [Google Scholar] [CrossRef] [PubMed]
- Goode, E.F.; Smyth, E.C. Immunotherapy for Gastroesophageal Cancer. J. Clin. Med. 2016, 5, 84. [Google Scholar] [CrossRef]
- Patel, S.P.; Kurzrock, R. PD-L1 Expression as a Predictive Biomarker in Cancer Immunotherapy. Mol. Cancer Ther. 2015, 14, 847–856. [Google Scholar] [CrossRef]
- Marchetti, A.; Di Lorito, A.; Buttitta, F. Why anti-PD1/PDL1 therapy is so effective? Another piece in the puzzle. J. Thorac. Dis. 2017, 9, 4863. [Google Scholar] [CrossRef]
- Joshi, S.S.; Maron, S.B.; Catenacci, D.V. Pembrolizumab for treatment of advanced gastric and gastroesophageal junction adenocarcinoma. Future Oncol. 2018, 14, 417–430. [Google Scholar] [CrossRef] [PubMed]
- Fuchs, C.S.; Doi, T.; Jang, R.W.; Muro, K.; Satoh, T.; Machado, M.; Sun, W.; Jalal, S.I.; Shah, M.A.; Metges, J.P.; et al. Safety and Efficacy of Pembrolizumab Monotherapy in Patients With Previously Treated Advanced Gastric and Gastroesophageal Junction Cancer: Phase 2 Clinical KEYNOTE-059 Trial. JAMA Oncol. 2018, 4, e180013. [Google Scholar] [CrossRef] [PubMed]
- Jin, Z.; Shen, J.; Wang, C.; Chen, D.; Zhang, B.; Zhang, J.; Ajani, J.A.; Bennouna, J.; Chao, J.; Yoon, H.H.; et al. Narrative review of pembrolizumab for the treatment of esophageal cancer: Evidence and outlook. Ann. Transl. Med. 2021, 9, 1189. [Google Scholar] [CrossRef] [PubMed]
- Maleki Vareki, S.; Garrigós, C.; Duran, I. Biomarkers of response to PD-1/PD-L1 inhibition. Crit. Rev. Oncol. Hematol. 2017, 116, 116–124. [Google Scholar] [CrossRef] [PubMed]
- Thompson, J.A.; Schneider, B.J.; Brahmer, J.; Andrews, S.; Armand, P.; Bhatia, S.; Budde, L.E.; Costa, L.; Davies, M.; Dunnington, D.; et al. Management of Immunotherapy-Related Toxicities, Version 1.2019. J. Natl. Compr. Canc Netw. 2019, 17, 255–289. [Google Scholar] [CrossRef]
- Kennedy, L.B.; Salama, A.K.S. A review of cancer immunotherapy toxicity. CA Cancer J. Clin. 2020, 70, 86–104. [Google Scholar] [CrossRef]
- Reid, P.D.; Cifu, A.S.; Bass, A.R. Management of Immunotherapy-Related Toxicities in Patients Treated With Immune Checkpoint Inhibitor Therapy. JAMA 2021, 325, 482–483. [Google Scholar] [CrossRef]
- Rice, T.W.; Rusch, V.W.; Ishwaran, H.; Blackstone, E.H. Cancer of the esophagus and esophagogastric junction: Data-driven staging for the seventh edition of the American Joint Committee on Cancer/International Union Against Cancer Cancer Staging Manuals. Cancer 2010, 116, 3763–3773. [Google Scholar] [CrossRef]
- Berry, M.F. Esophageal cancer: Staging system and guidelines for staging and treatment. J. Thorac. Dis. 2014, 6 (Suppl. S3), S289–S297. [Google Scholar] [CrossRef]
- Shi, G.D.; Luo, Z.L.; Fu, M.Y.; Tian, D.; Zhang, L.; Zhang, K.P. Evaluation of the value of 7th editions of UICC-AJCC esophageal and gastric cancer TNM staging systems for prognostic prediction of adenocarcinoma of esophagogastric junction (Siewert type II). Zhonghua Zhong Liu Za Zhi 2014, 36, 916–921. [Google Scholar] [CrossRef] [PubMed]
- Rice, T.W.; Ishwaran, H.; Blackstone, E.H.; Hofstetter, W.L.; Kelsen, D.P.; Apperson-Hansen, C. Recommendations for clinical staging (cTNM) of cancer of the esophagus and esophagogastric junction for the 8th edition AJCC/UICC staging manuals. Dis. Esophagus 2016, 29, 913–919. [Google Scholar] [CrossRef] [PubMed]
- Greene, F.L.; Balch, C.; Fleming, I.D.; April, F. Eztnm for the Ajcc Cancer Staging Manual; Springer: Berlin/Heidelberg, Germany, 2003. [Google Scholar]
- Maes, S.; Haidry, R.; Bisschops, R. Can the depth of invasion of early esophageal cancer be predicted based on endoscopic evidence? Minerva Chir. 2018, 73, 385–393. [Google Scholar] [CrossRef]
- Suzuki, G.; Yamazaki, H.; Aibe, N.; Masui, K.; Sasaki, N.; Shimizu, D.; Kimoto, T.; Shiozaki, A.; Dohi, O.; Fujiwara, H.; et al. Endoscopic submucosal dissection followed by chemoradiotherapy for superficial esophageal cancer: Choice of new approach. Radiat. Oncol. 2018, 13, 246. [Google Scholar] [CrossRef] [PubMed]
- Goense, L.; Meziani, J.; Borggreve, A.S.; van Rossum, P.S.; Meijer, G.J.; Ruurda, J.P.; van Hillegersberg, R.; Weusten, B.L. Role of adjuvant chemoradiotherapy after endoscopic treatment of early-stage esophageal cancer: A systematic review. Minerva Chir. 2018, 73, 428–436. [Google Scholar] [CrossRef] [PubMed]
- Tomita, Y.; Moldovan, M.; Chang Lee, R.; Hsieh, A.H.; Townsend, A.; Price, T. Salvage systemic therapy for advanced gastric and oesophago-gastric junction adenocarcinoma. Cochrane Database Syst. Rev. 2020, 11, Cd012078. [Google Scholar] [CrossRef]
- Ronellenfitsch, U.; Schwarzbach, M.; Hofheinz, R.; Kienle, P.; Kieser, M.; Slanger, T.E.; Jensen, K. Perioperative chemo(radio)therapy versus primary surgery for resectable adenocarcinoma of the stomach, gastroesophageal junction, and lower esophagus. Cochrane Database Syst. Rev. 2013, 5, Cd008107. [Google Scholar] [CrossRef]
- Janmaat, V.T.; Steyerberg, E.W.; van der Gaast, A.; Mathijssen, R.H.; Bruno, M.J.; Peppelenbosch, M.P.; Kuipers, E.J.; Spaander, M.C. Palliative chemotherapy and targeted therapies for esophageal and gastroesophageal junction cancer. Cochrane Database Syst. Rev. 2017, 11, Cd004063. [Google Scholar] [CrossRef]
- Li, C.; Wang, Z.; Duan, A.; Jiang, Q. Analysis on plausible factors related to the prognosis of stage IV esophageal cancer. Medicine 2020, 99, e18529. [Google Scholar] [CrossRef]
- O’Neill, L.; Guinan, E.; Doyle, S.L.; Elliott, J.A.; O’Sullivan, J.; Reynolds, J.V.; Hussey, J. Rehabilitation strategies following esophageal cancer (the ReStOre trial): A feasibility study. Dis. Esophagus 2017, 30, 1. [Google Scholar] [CrossRef]
- Feeney, C.; Reynolds, J.V.; Hussey, J. Preoperative physical activity levels and postoperative pulmonary complications post-esophagectomy. Dis. Esophagus 2011, 24, 489–494. [Google Scholar] [CrossRef] [PubMed]
- Chang, Y.L.; Tsai, Y.F.; Wu, Y.C.; Hsieh, M.J. Factors relating to quality of life after esophagectomy for cancer patients in Taiwan. Cancer Nurs. 2014, 37, 4–13. [Google Scholar] [CrossRef] [PubMed]
- Xu, Y.J.; Cheng, J.C.; Lee, J.M.; Huang, P.M.; Huang, G.H.; Chen, C.C. A Walk-and-Eat Intervention Improves Outcomes for Patients With Esophageal Cancer Undergoing Neoadjuvant Chemoradiotherapy. Oncologist 2015, 20, 1216–1222. [Google Scholar] [CrossRef]
- Yoshida, N.; Baba, Y.; Shigaki, H.; Harada, K.; Iwatsuki, M.; Kurashige, J.; Sakamoto, Y.; Miyamoto, Y.; Ishimoto, T.; Kosumi, K.; et al. Preoperative Nutritional Assessment by Controlling Nutritional Status (CONUT) is Useful to estimate Postoperative Morbidity After Esophagectomy for Esophageal Cancer. World J. Surg. 2016, 40, 1910–1917. [Google Scholar] [CrossRef] [PubMed]
- Ouattara, M.; D’Journo, X.B.; Loundou, A.; Trousse, D.; Dahan, L.; Doddoli, C.; Seitz, J.F.; Thomas, P.A. Body mass index kinetics and risk factors of malnutrition one year after radical oesophagectomy for cancer. Eur. J. Cardiothorac. Surg. 2012, 41, 1088–1093. [Google Scholar] [CrossRef]
- Harada, K.; Ida, S.; Baba, Y.; Ishimoto, T.; Kosumi, K.; Tokunaga, R.; Izumi, D.; Ohuchi, M.; Nakamura, K.; Kiyozumi, Y.; et al. Prognostic and clinical impact of sarcopenia in esophageal squamous cell carcinoma. Dis. Esophagus 2016, 29, 627–633. [Google Scholar] [CrossRef] [PubMed]
- Anandavadivelan, P.; Lagergren, P. Cachexia in patients with oesophageal cancer. Nat. Rev. Clin. Oncol. 2016, 13, 185–198. [Google Scholar] [CrossRef] [PubMed]
- Elliott, J.A.; Doyle, S.L.; Murphy, C.F.; King, S.; Guinan, E.M.; Beddy, P.; Ravi, N.; Reynolds, J.V. Sarcopenia: Prevalence, and Impact on Operative and Oncologic Outcomes in the Multimodal Management of Locally Advanced Esophageal Cancer. Ann. Surg. 2017, 266, 822–830. [Google Scholar] [CrossRef]
- Low, D.E.; Alderson, D.; Cecconello, I.; Chang, A.C.; Darling, G.E.; DʼJourno, X.B.; Griffin, S.M.; Hölscher, A.H.; Hofstetter, W.L.; Jobe, B.A.; et al. International Consensus on Standardization of Data Collection for Complications Associated With Esophagectomy: Esophagectomy Complications Consensus Group (ECCG). Ann. Surg. 2015, 262, 286–294. [Google Scholar] [CrossRef]
- Lunardi, A.C.; Miranda, C.S.; Silva, K.M.; Cecconello, I.; Carvalho, C.R. Weakness of expiratory muscles and pulmonary complications in malnourished patients undergoing upper abdominal surgery. Respirology 2012, 17, 108–113. [Google Scholar] [CrossRef] [PubMed]
- Grotenhuis, B.A.; Wijnhoven, B.P.; Grüne, F.; van Bommel, J.; Tilanus, H.W.; van Lanschot, J.J. Preoperative risk assessment and prevention of complications in patients with esophageal cancer. J. Surg. Oncol. 2010, 101, 270–278. [Google Scholar] [CrossRef]
- Low, D.E.; Kuppusamy, M.K.; Alderson, D.; Cecconello, I.; Chang, A.C.; Darling, G.; Davies, A.; D’Journo, X.B.; Gisbertz, S.S.; Griffin, S.M.; et al. Benchmarking Complications Associated with Esophagectomy. Ann. Surg. 2019, 269, 291–298. [Google Scholar] [CrossRef] [PubMed]
- Rostas, J.W., 3rd; Mai, T.T.; Richards, W.O. Gastric motility physiology and surgical intervention. Surg. Clin. N. Am. 2011, 91, 983–999. [Google Scholar] [CrossRef] [PubMed]
- Poghosyan, T.; Gaujoux, S.; Chirica, M.; Munoz-Bongrand, N.; Sarfati, E.; Cattan, P. Functional disorders and quality of life after esophagectomy and gastric tube reconstruction for cancer. J. Visc. Surg. 2011, 148, e327–e335. [Google Scholar] [CrossRef] [PubMed]
- O’Neill, L.; Gannon, J.; Guinan, E.; Reynolds, J.V.; Hussey, J. Multidisciplinary rehabilitation across the esophageal cancer journey. J. Thorac. Dis. 2017, 9, E1140–E1142. [Google Scholar]

| T status | |
| Tis | High-grade dysplasia |
| T1 | Invasion into the lamina propria, muscularis mucosae, or submucosa |
| T2 | Invasion into muscularis propria |
| T3 | Invasion into adventitia |
| T4a | Invades resectable adjacent structures (pleura, pericardium, and diaphragm) |
| T4b | Invades unresectable adjacent structures (aorta, vertebral body, tracheae) |
| N status | |
| N0 | No regional lymph node metastases |
| N1 | 1 to 2 positive regional lymph nodes |
| N2 | 3 to 6 positive regional lymph nodes |
| N3 | 7 or more positive regional lymph nodes |
| M status | |
| M0 | No distant metastases |
| M1 | Distant metastases |
| Histologic grade | |
| G1 | Well differentiated |
| G2 | Moderately differentiated |
| G3 | Poorly differentiated |
| G4 | Undifferentiated |
| Stage | T | N | M | Grade |
|---|---|---|---|---|
| 0 | Is | 0 | 0 | 1 |
| IA | 1 | 0 | 0 | 1–2 |
| IB | 1 | 0 | 0 | 3 |
| 2 | 0 | 0 | 1–2 | |
| IIA | 2 | 0 | 0 | 3 |
| IIB | 3 | 0 | 0 | Any |
| 1–2 | 1 | 0 | Any | |
| IIIA | 1–2 | 2 | 0 | Any |
| 3 | 1 | 0 | Any | |
| 4a | 0 | 0 | Any | |
| IIIB | 3 | 2 | 0 | Any |
| IIIC | 4a | 1–2 | 0 | Any |
| 4b | Any | 0 | Any | |
| Any | 3 | 0 | Any | |
| IV | Any | Any | 1 | Any |
| Stage | T | N | M | Grade |
|---|---|---|---|---|
| 0 | 1 | 0 | 0 | 1 |
| IA | 1 | 0 | 0 | 1 |
| IB | 1 | 0 | 0 | 2–3 |
| 2–3 | 0 | 0 | 1 | |
| IIA | 2–3 | 0 | 0 | 1 |
| 2–3 | 0 | 0 | 2–3 | |
| IIB | 2–3 | 0 | 0 | 2–3 |
| 1–2 | 1 | 0 | Any | |
| IIIA | 1–2 | 2 | 0 | Any |
| 3 | 1 | 0 | Any | |
| 4a | 0 | 0 | Any | |
| IIIB | 3 | 2 | 0 | Any |
| IIIC | 4a | 1–2 | 0 | Any |
| 4b | Any | 0 | Any | |
| Any | 3 | 0 | Any | |
| IV | Any | Any | 1 | Any |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Acharya, R.; Mahapatra, A.; Verma, H.K.; Bhaskar, L.V.K.S. Unveiling Therapeutic Targets for Esophageal Cancer: A Comprehensive Review. Curr. Oncol. 2023, 30, 9542-9568. https://doi.org/10.3390/curroncol30110691
Acharya R, Mahapatra A, Verma HK, Bhaskar LVKS. Unveiling Therapeutic Targets for Esophageal Cancer: A Comprehensive Review. Current Oncology. 2023; 30(11):9542-9568. https://doi.org/10.3390/curroncol30110691
Chicago/Turabian StyleAcharya, Rakesh, Ananya Mahapatra, Henu Kumar Verma, and L. V. K. S. Bhaskar. 2023. "Unveiling Therapeutic Targets for Esophageal Cancer: A Comprehensive Review" Current Oncology 30, no. 11: 9542-9568. https://doi.org/10.3390/curroncol30110691