Robust Operating Room Scheduling Model with Violation Probability Consideration under Uncertain Surgery Duration
Abstract
:1. Introduction
- ▲
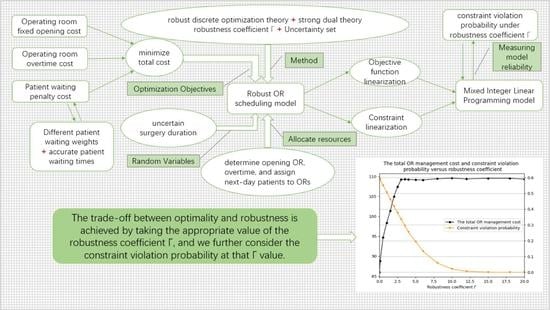
- The first contribution of this paper relates to the novelty of the optimization objective, which is formulated as the sum of the fixed OR opening cost, the patients’ waiting penalty cost, and the OR overtime cost to represent the operational cost of ORs. Thereinto, patients’ waiting times are calculated via the cumulative sum of the accurate patient’s surgery duration. Hence, with this formula, we demonstrate the influence of the uncertain surgery duration on the OR scheduling model.
- ▲
- Based on the developed optimization objective, we formulate the robust OR scheduling model by considering the patient’s uncertain surgery duration. Thereinto, the uncertain surgery duration is represented by a box uncertainty set, and a robustness coefficient is introduced to control the trade-off between the constraint violation probability and optimality. Then, the robust discrete optimization theory and strong dual theory are invoked to transform the robust model equivalently into a Mixed Integer Linear Programming (MILP) model, which is in a tractable analytical form. It is noteworthy that this paper solves the robust optimization problem with uncertain parameters in both the objective function and constraints. Moreover, by invoking the robust discrete theory, we derive the probability bounds of constraint violation for the OR overtime constraints, which is one of the early attempts to study the constraint violation probability based on the theoretical analysis of the OR scheduling model.
- ▲
- Third, we validate the performance of our model by calculating the upper bound of the constraint violation probability and the objective function at different robustness coefficients to investigate the trade-off among robustness, optimality, and reliability. In addition, some insights are provided on the influence of the robustness coefficient on the OR scheduling model. A sensitivity analysis of the uncertain perturbation factor is also performed to obtain variations in hospital cost sensitivity with the constraint violation probability.
2. OR Model and Assumptions
3. Robust OR Scheduling Approach
3.1. Deterministic Model
3.2. Robust Discrete Optimization Model and Transformation
3.2.1. Linearization of the Objective Function
3.2.2. The Overtime Constraints Transformation
3.3. Upper-Bound Constraint Violation Probability
4. Modeling and Analysis
4.1. The Performance Analysis against the Robustness Coefficient
4.2. Sensitivity Analysis
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Cardoen, B.; Demeulemeester, E.; Belin, J. Operating room planning and scheduling: A literature review. Eur. J. Oper. Res. 2010, 201, 921–932. [Google Scholar] [CrossRef] [Green Version]
- Du, S.; Xie, J.; Liu, Z. Progress and prospects in an emerging hot topic: Healthcare operations management. J. Manag. Sci. China 2013, 16, 921–932. [Google Scholar]
- Süleyman, E. Medical Data Analysis for Different Data Types. IJCESEN 2020, 6, 138–144. [Google Scholar] [CrossRef]
- Özgüven, Y.M.; Eken, S. Distributed messaging and light streaming system for combating pandemics. J. Ambient Intell. Humaniz. Comput. 2021, 1–15. [Google Scholar] [CrossRef] [PubMed]
- Zhu, S.; Fan, W.; Yang, S.; Pei, J.; Pardalos, P.M. Operating room planning and surgical case scheduling: A review of the literature. J. Comb. Optim. 2019, 37, 757–805. [Google Scholar] [CrossRef]
- Mengistu, B.; Ray, D.; Lockett, P.; Dorsey, V.; Phipps, R.A.; Subramanian, H.; Atkins, J.T.; El Osta, B.; Falchook, G.S.; Karp, D.D. Innovative strategies for decreasing blood collection wait times for patients in early-phase cancer clinical trials. J. Oncol. Pract. 2016, 12, e784–e791. [Google Scholar] [CrossRef]
- Wang, Y.; Tang, J. Overview and prospects of operating rooms management. Syst. Eng. Theory Pract. 2018, 38, 1778–1791. [Google Scholar] [CrossRef]
- Xiao, G.; Jaarsveld, W.; Dong, M.; Klundert, J. Stochastic programming analysis, and solutions to schedule overcrowded operating rooms in China. Comput. Oper. Res. 2010, 74, 78–91. [Google Scholar] [CrossRef] [Green Version]
- Mancilla, C.; Storer, R.A. Sample average approximation approach to stochastic appointment sequencing and scheduling. IIE Trans. 2012, 44, 655–670. [Google Scholar] [CrossRef]
- Moreno, M.S.; Blanco, A.M. A fuzzy programming approach for the multi-objective patient appointment scheduling problem under uncertainty in a large hospital. Comput. Ind. Eng. 2018, 123, 33–41. [Google Scholar] [CrossRef]
- Khaniyev, T.; Kayış, E.; Güllü, R. Next-day operating room scheduling with uncertain surgery durations: Exact analysis and heuristics. Eur. J. Oper. Res. 2020, 286, 49–62. [Google Scholar] [CrossRef]
- Addis, B.; Carello, G.; Grosso, A.; Tànfani, E. Operating room scheduling and rescheduling: A rolling horizon approach. Flex. Serv. Manuf. J. 2015, 28, 206–232. [Google Scholar] [CrossRef] [Green Version]
- Erdogan, S.A.; Denton, B. Dynamic appointment scheduling of a stochastic server with uncertain demand. INFORMS J. Comput. 2013, 25, 116–132. [Google Scholar] [CrossRef] [Green Version]
- Issabakhsh, M.; Lee, S.; Kang, H. Scheduling patient appointment in an infusion center: A mixed integer robust optimization approach. Health Care Manag. Sci. 2020, 24, 117–139. [Google Scholar] [CrossRef]
- Castaing, J.; Cohn, A.; Denton, B.T.; Weizer, A. A stochastic programming approach to reduce patient wait times and overtime in an outpatient infusion center. IIE Trans. Health. Syst. Eng. 2016, 6, 111–125. [Google Scholar] [CrossRef]
- Lamar, M.; Xie, X.; Dolgui, A.; Grimaud, F. A stochastic model for operating room planning with elective and emergency demand for surgery. Eur. J. Oper. Res. 2008, 185, 1026–1037. [Google Scholar] [CrossRef]
- Wang, Y.; Tang, J.; Fung, R.Y.K. A column-generation-based heuristic algorithm for solving operating theater planning problems under stochastic demand and surgery cancellation risk. Int. J. Prod. Econ. 2014, 158, 28–36. [Google Scholar] [CrossRef]
- Lahijanian, B.; Zarandi, M.H.F.; Farahani, F.V. Proposing a model for operating room scheduling based on fuzzy surgical duration. In Proceedings of the 2016 Annual Conference of the North American Fuzzy Information Processing Society (NAFIPS), El Paso, TX, USA, 31 October–4 November 2016; Volume 201, pp. 1–5. [Google Scholar] [CrossRef]
- Wang, K.; Qin, H.; Huang, Y.; Luo, M.; Zhou, L. Surgery scheduling in outpatient procedure center with re-entrant patient flow and fuzzy service times. Omega 2021, 102, 102350. [Google Scholar] [CrossRef]
- Breuer, D.J.; Lahrichi, N.; Clark, D.E.; Benneyan, J.C. Robust combined operating room planning and personnel scheduling under uncertainty. Oper. Res. Health. Care. 2020, 27, 100276. [Google Scholar] [CrossRef]
- Moosavi, A.; Ebrahimnejad, S. Scheduling of elective patients considering upstream and downstream units and emergency demand using robust optimization. Comput. Ind. Eng. 2018, 120, 216–233. [Google Scholar] [CrossRef]
- Wang, Y.; Tang, J. A two-stage robust optimization method for solving surgery scheduling problems. J. Syst. Eng. 2016, 31, 431–440. [Google Scholar] [CrossRef]
- Denton, B.T.; Miller, A.J.; Balasubramanian, H.J.; Huschka, T.R. Optimal allocation of surgery blocks to operating rooms under uncertainty. Oper. Res. 2010, 58, 802–816. [Google Scholar] [CrossRef] [Green Version]
- Wang, J.; Guo, H.; Tsui, K.L. Two-stage robust optimization for surgery scheduling considering surgeon collaboration. Int. J. Prod. Res. 2021, 59, 6437–6450. [Google Scholar] [CrossRef]
- Vali-Siar, M.M.; Gholami, S.; Ramezanian, R. Multi-period and multi-resource operating room scheduling under uncertainty: A case study. Comput. Ind. Eng. 2018, 126, 549–568. [Google Scholar] [CrossRef]
- Bansal, A.; Berg, B.; Huang, Y.L. A distributionally robust optimization approach for coordinating clinical and surgical appointments. IISE Trans. 2021, 53, 1311–1323. [Google Scholar] [CrossRef]
- Peng, C.; Wang, S.; Ran, L. Robust surgery planning and scheduling with downstream bed capacity constraint in ICU. Syst. Eng. Theor. Pract. 2018, 38, 623–633. [Google Scholar] [CrossRef]
- Makboul, S.; Kharraja, S.; Abbassi, A.; Alaoui, A. A two-stage robust optimization approach for the master surgical schedule problem under uncertainty considering downstream resources. Health Care Manag Sci. 2021, 25, 63–88. [Google Scholar] [CrossRef]
- Wang, J.; Dai, Z.; Chang, A.; Shi, J. Surgical scheduling by Fuzzy model considering inpatient beds shortage under uncertain surgery durations. Ann. Oper. Res. 2022, 315, 463–505. [Google Scholar] [CrossRef]
- Soyster, A.L. Convex programming with set-inclusive constraints and applications to inexact linear programming. Oper. Res. 1973, 21, 1154–1157. [Google Scholar] [CrossRef] [Green Version]
- Bertsimas, D.; Brown, D.B.; Caramanis, C. Theory and applications of robust optimization. SIAM Rev. 2011, 53, 464–501. [Google Scholar] [CrossRef]
- Ben-Tal, A.; Nemirovski, A. Robust convex optimization. Math. Oper. Res. 1998, 23, 769–805. [Google Scholar] [CrossRef] [Green Version]
- Bertsimas, D.; Doan, X.V. Robust and data-driven approaches to call centers. Eur. J. Oper. Res. 2010, 207, 1072–1085. [Google Scholar] [CrossRef]
- Bertsimas, D.; Sim, M. The price of robustness. Oper. Res. 2010, 52, 35–53. [Google Scholar] [CrossRef] [Green Version]
- Liu, H.; Yang, C. Robust Research on Service Facility Network Design Problem with Demand Uncertainty. Oper. Res. Manag. Sci. 2016, 25, 117–125. [Google Scholar] [CrossRef]
- Chen, Y.; Zhou, W.; Hua, Z.; Shan, M. Pricing and capacity planning of the referral system with delay-sensitive patients. J. Manag. Sci. China 2015, 18, 73–83. [Google Scholar]
- Bam, M.; Denton, B.T.; Van Oyen, M.P.; Cowen, M.E. Surgery scheduling with recovery resources. IISE Trans. 2017, 49, 942–955. [Google Scholar] [CrossRef]







| Parameters | Descriptions |
|---|---|
| the set of patients who need to undergo surgery on the next-day. | |
| the expected duration of patient i’s surgery. | |
| i-th patient’s waiting time weight, we carve out per patient’s waiting cost by the product of and per patient’s actual waiting time. | |
| the OR set, in which OR is functionally identical. | |
| fixed opening cost of the j-th OR. | |
| T | fixed daily opening hours for each OR. |
| unit overtime cost. | |
| P | constraint violation probability. |
| decision variable, variable, if i-th patient is operated in the j-th OR, = 1; otherwise, . | |
| decision variable, variable, if j-th OR is open on next-day, . otherwise . | |
| decision variable, the overtime of j-th OR, . |
| Robust Coefficient | Minimum Total OR Management Cost | Total OR Overtime | Total Patients’ Waiting Time | Constraint Violation Probability |
|---|---|---|---|---|
| = 0 | 85.95 | 1.99 | 29.84 | 0.59 |
| = 0.1 | 88.76 | 2.33 | 29.79 | 0.58 |
| = 0.5 | 94.71 | 4.33 | 30.69 | 0.55 |
| = 1 | 98.37 | 6.23 | 30.63 | 0.50 |
| = 1.5 | 101.37 | 7.86 | 30.52 | 0.46 |
| = 2 | 104.97 | 9.66 | 30.50 | 0.41 |
| = 2.5 | 107.40 | 10.69 | 31.20 | 0.37 |
| = 3 | 109.23 | 10.94 | 32.64 | 0.33 |
| = 4 | 109.24 | 11.00 | 32.61 | 0.25 |
| = 5 | 109.17 | 11.02 | 32.43 | 0.195 |
| = 6 | 109.13 | 11.03 | 32.52 | 0.13 |
| 109.63 | 11.06 | 32.77 | 0.05 | |
| 109.87 | 11.09 | 32.89 | 0.02 | |
| = 15 | 109.54 | 11.11 | 32.75 | 0.0008 |
| = 18 | 109.74 | 11.12 | 32.71 | 0.00002 |
| = 20 | 109.35 | 11.13 | 32.65 | 0 1 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ma, Y.; Liu, K.; Li, Z.; Chen, X. Robust Operating Room Scheduling Model with Violation Probability Consideration under Uncertain Surgery Duration. Int. J. Environ. Res. Public Health 2022, 19, 13685. https://doi.org/10.3390/ijerph192013685
Ma Y, Liu K, Li Z, Chen X. Robust Operating Room Scheduling Model with Violation Probability Consideration under Uncertain Surgery Duration. International Journal of Environmental Research and Public Health. 2022; 19(20):13685. https://doi.org/10.3390/ijerph192013685
Chicago/Turabian StyleMa, Yanbo, Kaiyue Liu, Zheng Li, and Xiang Chen. 2022. "Robust Operating Room Scheduling Model with Violation Probability Consideration under Uncertain Surgery Duration" International Journal of Environmental Research and Public Health 19, no. 20: 13685. https://doi.org/10.3390/ijerph192013685