Sports Participation and Anti-Epidemic: Empirical Evidence on the Influence of Regular Physical Activity on the COVID-19 Pandemic in Mainland China
Abstract
:1. Introduction
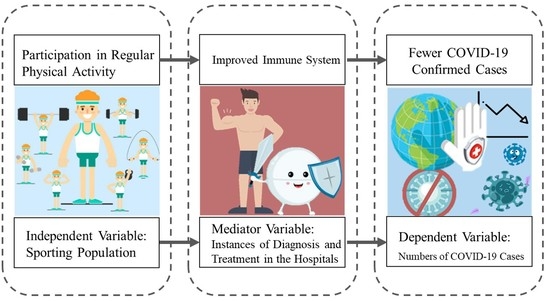
2. Conceptual Framework
3. Materials and Methods
3.1. Empirical Strategy
3.1.1. Baseline: Ordinary Least Squares Regression
3.1.2. IV Approach: Two-Stage Least Squares Regression
3.1.3. Mechanism Exploration: Mediating Effect Model
3.2. Data Collection
4. Results
4.1. Does Regular Physical Activity Matter?
4.2. Robustness
4.3. Regular Physical Activity, Immunity, and COVID-19
4.4. When and Where Is Physical Activity More Important?
5. Discussion
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Prompetchara, E.; Ketloy, C.; Palaga, T. Immune responses in COVID-19 and potential vaccines: Lessons learned from SARS and MERS epidemic. Asian Pac. J. Allergy Immunol. 2020, 38, 1–9. [Google Scholar] [PubMed]
- Huang, C.; Huang, L.; Wang, Y.; Li, X.; Ren, L.; Gu, X.; Kang, L.; Guo, L.; Liu, M.; Zhou, X.; et al. 6-month consequences of COVID-19 in patients discharged from hospital: A cohort study. Lancet 2021, 397, 220–232. [Google Scholar] [CrossRef]
- Mlcochova, P.; Kemp, S.A.; Dhar, M.S.; Papa, G.; Meng, B.; Ferreira, I.A.T.M.; Datir, R.; Collier, D.A.; Albecka, A.; Singh, S.; et al. SARS-CoV-2 B.1.617.2 Delta variant replication and immune evasion. Nature 2021, 599, 114–119. [Google Scholar] [CrossRef] [PubMed]
- Shuai, H.; Chan, J.F.W.; Hu, B.; Chai, Y.; Yuen, T.T.T.; Yin, F.; Huang, X.; Yoon, C.; Hu, J.-C.; Liu, H.; et al. Attenuated replication and pathogenicity of SARS-CoV-2 B. 1.1. 529 Omicron. Nature 2022, 603, 693–699. [Google Scholar] [CrossRef]
- Laddu, D.R.; Lavie, C.J.; Phillips, S.A.; Arena, R. Physical activity for immunity protection: Inoculating populations with healthy living medicine in preparation for the next pandemic. Prog. Cardiovasc. Dis. 2021, 64, 102–104. [Google Scholar] [CrossRef]
- Woods, J.A.; Hutchinson, N.T.; Powers, S.K.; Roberts, W.O.; Gomez-Cabrera, M.C.; Radak, Z.; Berkes, I.; Boros, A.; Boldogh, I.; Leeuwenburgh, C.; et al. The COVID-19 pandemic and physical activity. Sports Med. Health Sci. 2020, 2, 55–64. [Google Scholar] [CrossRef]
- Pedersen, B.K. Influence of Physical Activity on the Cellular Immune System: Mechanisms of Action. Int. J. Sports Med. 1991, 12, S23–S29. [Google Scholar] [CrossRef]
- Shephard, R.J.; Shek, P.N. Potential impact of physical activity and sport on the immune system--a brief review. Br. J. Sports Med. 1994, 28, 247–255. [Google Scholar] [CrossRef]
- Ayres, J.S. A metabolic handbook for the COVID-19 pandemic. Nat. Metab. 2020, 2, 572–585. [Google Scholar] [CrossRef]
- Siordia, J.A., Jr. Epidemiology and clinical features of COVID-19: A review of current literature. J. Clin. Virol. 2020, 127, 104357. [Google Scholar] [CrossRef]
- Huang, J.; Lin, S.; Hu, X.; Lin, R. Are Sports Champions Also Anti-Epidemic Heroes? Quantitative Research on the Influence of Sports Champions’ Demonstration Effect on the COVID-19 Epidemic in China. Int. J. Environ. Res. Public Health 2022, 19, 2438. [Google Scholar] [CrossRef]
- Luzi, L.; Radaelli, M.G. Influenza and obesity: Its odd relationship and the lessons for COVID-19 pandemic. Acta Diabetol. 2020, 57, 759–764. [Google Scholar] [CrossRef] [PubMed]
- Boni, M.F.; Lemey, P.; Jiang, X.; Lam TT, Y.; Perry, B.W.; Castoe, T.A.; Robertson, D.L. Evolutionary origins of the SARS-CoV-2 sarbecovirus lineage responsible for the COVID-19 pandemic. Nat. Microbiol. 2020, 5, 1408–1417. [Google Scholar] [CrossRef] [PubMed]
- Domingo, J.L. What we know and what we need to know about the origin of SARS-CoV-2. Environ. Res. 2021, 200, 111785. [Google Scholar] [CrossRef] [PubMed]
- Makarenkov, V.; Mazoure, B.; Rabusseau, G.; Legendre, P. Horizontal gene transfer and recombination analysis of SARS-CoV-2 genes helps discover its close relatives and shed light on its origin. BMC Ecol. Evol. 2021, 21, 1–18. [Google Scholar] [CrossRef]
- Yang, L.; Liu, S.; Liu, J.; Zhang, Z.; Wan, X.; Huang, B.; Chen, Y.; Zhang, Y. COVID-19: Immunopathogenesis and Immunotherapeutics. Signal Transduct. Target. Ther. 2020, 5, 1–8. [Google Scholar] [CrossRef]
- Rendeiro, A.F.; Ravichandran, H.; Bram, Y.; Chandar, V.; Kim, J.; Meydan, C.; Park, J.; Foox, J.; Hether, T.; Warren, S.; et al. The spatial landscape of lung pathology during COVID-19 progression. Nature 2021, 593, 564–569. [Google Scholar] [CrossRef]
- Shereen, M.A.; Khan, S.; Kazmi, A.; Bashir, N.; Siddique, R. COVID-19 infection: Emergence, transmission, and characteristics of human coronaviruses. J. Adv. Res. 2020, 24, 91–98. [Google Scholar] [CrossRef]
- Iba, T.; Levy, J.H.; Connors, J.M.; Warkentin, T.E.; Thachil, J.; Levi, M. The unique characteristics of COVID-19 coagulopathy. Crit. Care 2020, 24, 360. [Google Scholar] [CrossRef]
- Tian, S.; Hu, N.; Lou, J.; Chen, K.; Kang, X.; Xiang, Z.; Chen, H.; Wang, D.; Liu, N.; Liu, D.; et al. Characteristics of COVID-19 infection in Beijing. J. Infect. 2020, 80, 401–406. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cohen, M.S. Hydroxychloroquine for the Prevention of COVID-19—Searching for Evidence. New Engl. J. Med. 2020, 383, 585–586. [Google Scholar] [CrossRef] [PubMed]
- Chowdhury, R.; Luhar, S.; Khan, N.; Choudhury, S.R.; Matin, I.; Franco, O.H. Long-term strategies to control COVID-19 in low and middle-income countries: An options overview of community-based, non-pharmacological inter-ventions. Eur. J. Epidemiol. 2020, 35, 743–748. [Google Scholar] [CrossRef] [PubMed]
- Lopez Bernal, J.; Andrews, N.; Gower, C.; Gallagher, E.; Simmons, R.; Thelwall, S.; Stowe, J.; Tessier, E.; Groves, N.; Dabrera, G.; et al. Effectiveness of COVID-19 Vaccines against the B.1.617.2 (Delta) Variant. N. Engl. J. Med. 2021, 385, 585–594. [Google Scholar] [CrossRef]
- Yamada, M.; Kimura, Y.; Ishiyama, D.; Otobe, Y.; Suzuki, M.; Koyama, S.; Kikuchi, T.; Kusumi, H.; Arai, H. Effect of the COVID-19 Epidemic on Physical Activity in Community-Dwelling Older Adults in Japan: A Cross-Sectional Online Survey. J. Nutr. Health Aging 2020, 24, 948–950. [Google Scholar] [CrossRef] [PubMed]
- Katewongsa, P.; Widyastari, D.A.; Saonuam, P.; Haemathulin, N.; Wongsingha, N. The effects of the COVID-19 pandemic on the physical activity of the Thai population: Evidence from Thailand’s Surveillance on Physical Activity 2020. J. Sport Health Sci. 2021, 10, 341–348. [Google Scholar] [CrossRef]
- Caputo, E.L.; Reichert, F.F. Studies of Physical Activity and COVID-19 During the Pandemic: A Scoping Review. J. Phys. Act. Health 2020, 17, 1275–1284. [Google Scholar] [CrossRef] [PubMed]
- Pieh, C.; Budimir, S.; Probst, T. The effect of age, gender, income, work, and physical activity on mental health during coronavirus disease (COVID-19) lockdown in Austria. J. Psychosom. Res. 2020, 136, 110186. [Google Scholar] [CrossRef] [PubMed]
- Faulkner, J.; O’Brien, W.J.; McGrane, B.; Wadsworth, D.; Batten, J.; Askew, C.D.; Badenhorst, C.; Byrd, E.; Coulter, M.; Draper, N.; et al. Physical activity, mental health and well-being of adults during initial COVID-19 containment strategies: A multi-country cross-sectional analysis. J. Sci. Med. Sport 2021, 24, 320–326. [Google Scholar] [CrossRef] [PubMed]
- da Silveira, M.P.; da Silva Fagundes, K.K.; Bizuti, M.R.; Starck, É.; Rossi, R.C.; de Resende ESilva, D.T. Physical exercise as a tool to help the immune system against COVID-19: An integrative review of the current literature. Clin. Exp. Med. 2021, 21, 15–28. [Google Scholar] [CrossRef]
- Dixit, S. Can moderate intensity aerobic exercise be an effective and valuable therapy in preventing and controlling the pandemic of COVID-19? Med Hypotheses 2020, 143, 109854. [Google Scholar] [CrossRef]
- Shahrbanian, S.; Alikhani, S.; Kakavandi, M.A.; Hackney, A.C. Physical Activity for Improving the Immune System of Older Adults During the COVID-19 Pandemic. Altern. Ther. Health Med. 2020, 26, 117–125. [Google Scholar] [PubMed]
- Dwyer, M.J.; Pasini, M.; De Dominicis, S.; Righi, E. Physical activity: Benefits and challenges during the COVID-19 pandemic. Scand. J. Med. Sci. Sports 2020, 30, 1291–1294. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Y.; Zhang, H.; Ma, X.; Di, Q. Mental Health Problems during the COVID-19 Pandemics and the Mitigation Effects of Exercise: A Longitudinal Study of College Students in China. Int. J. Environ. Res. Public Health 2020, 17, 3722. [Google Scholar] [CrossRef] [PubMed]
- Marconcin, P.; Werneck, A.O.; Peralta, M.; Ihle, A.; Gouveia, R.; Ferrari, G.; Sarmento, H.; Marques, A. The association between physical activity and mental health during the first year of the COVID-19 pandemic: A systematic review. BMC Public Heal. 2022, 22, 1–14. [Google Scholar] [CrossRef]
- Cunningham, G.B. Physical activity and its relationship with COVID-19 cases and deaths: Analysis of U.S. counties. J. Sport Health Sci. 2021, 10, 570–576. [Google Scholar] [CrossRef]
- Chen, P.; Mao, L.; Nassis, G.P.; Harmer, P.; Ainsworth, B.E.; Li, F. Coronavirus disease (COVID-19): The need to maintain regular physical activity while taking precautions. J. Sport Health Sci. 2020, 9, 103–104. [Google Scholar] [CrossRef] [PubMed]
- Sallis, R.; Young, D.R.; Tartof, S.Y.; Sallis, J.F.; Sall, J.; Li, Q.; Smith, G.N.; Cohen, D.A. Faculty Opinions recommendation of Physical inactivity is associated with a higher risk for severe COVID-19 outcomes: A study in 48 440 adult patients. Brit. J. Sport Med. 2021, 55, 1099–1105. [Google Scholar] [CrossRef] [PubMed]
- Jiménez-Pavón, D.; Carbonell-Baeza, A.; Lavie, C.J. Physical exercise as therapy to fight against the mental and physical consequences of COVID-19 quarantine: Special focus in older people. Prog. Cardiovasc. Dis. 2020, 63, 386–388. [Google Scholar] [CrossRef]
- Tamminen, N.; Reinikainen, J.; Appelqvist-Schmidlechner, K.; Borodulin, K.; Mäki-Opas, T.; Solin, P. Associations of physical activity with positive mental health: A population-based study. Ment. Health Phys. Act. 2020, 18, 100319. [Google Scholar] [CrossRef]
- Antonakis, J.; Bendahan, S.; Jacquart, P.; Lalive, R. Causality and Endogeneity: Problems and Solutions. The Oxford Handbook of Leadership and Organizations; Oxford University Press: Oxford, UK, 2014; Volume 1, pp. 93–117. [Google Scholar]
- Angrist, J.D.; Pischke, J.S. Mostly Harmless Econometrics; Princeton University Press: Princeton, NJ, USA, 2008; pp. 88–157. [Google Scholar]
- Ruseski, J.E.; Humphreys, B.R.; Hallman, K.; Wicker, P.; Breuer, C. Sport Participation and Subjective Well-Being: Instrumental Variable Results from German Survey Data. J. Phys. Act. Health 2014, 11, 396–403. [Google Scholar] [CrossRef] [Green Version]
- Huang, H.; Humphreys, B.R. Sports participation and happiness: Evidence from US microdata. J. Econ. Psychol. 2012, 33, 776–793. [Google Scholar] [CrossRef]
- Jia, J.S.; Lu, X.; Yuan, Y.; Xu, G.; Jia, J.; Christakis, N.A. Population flow drives spatio-temporal distribution of COVID-19 in China. Nature 2020, 582, 389–394. [Google Scholar] [CrossRef] [PubMed]
- Brockmann, D.; Helbing, D. The hidden geometry of complex, network-driven contagion phenomena. Science 2013, 342, 1337–1342. [Google Scholar] [CrossRef]
- Hsiang, S.; Allen, D.; Annan-Phan, S.; Bell, K.; Bolliger, I.; Chong, T.; Druckenmiller, H.; Huang, L.Y.; Hultgren, A.; Krasovich, E.; et al. The effect of large-scale anti-contagion policies on the COVID-19 pandemic. Nature 2020, 584, 262–267. [Google Scholar] [CrossRef] [PubMed]
- Lin, R.; Lin, S.; Yan, N.; Huang, J. Do prevention and control measures work? Evidence from the outbreak of COVID-19 in China. Cities 2021, 118, 103347. [Google Scholar] [CrossRef] [PubMed]
- Pu, B.; Zhang, L.; Tang, Z.; Qiu, Y. The Relationship between Health Consciousness and Home-Based Exercise in China during the COVID-19 Pandemic. Int. J. Environ. Res. Public Health 2020, 17, 5693. [Google Scholar] [CrossRef] [PubMed]
- Lin, R.; Wang, X.; Huang, J. The influence of weather conditions on the COVID-19 epidemic: Evidence from 279 prefec-ture-level panel data in China. Environ. Res. 2022, 206, 112272. [Google Scholar] [CrossRef]
- Sato, M.; DU, J.; Inoue, Y. Rate of Physical Activity and Community Health: Evidence from U.S. Counties. J. Phys. Act. Health 2016, 13, 640–648. [Google Scholar] [CrossRef]
- Blanks, A.M.; Wagamon, T.T.; Lafratta, L.; Sisk, M.G.; Senter, M.B.; Pedersen, L.N.; Bohmke, N.; Shah, A.; Mihalick, V.L.; Franco, R.L. Impact of physical activity on monocyte subset CCR2 expression and mac-rophage polarization following moderate intensity exercise. Brain Behav. Immun. 2020, 2, 100033. [Google Scholar]
- Mello, C.; Aguayo, E.; Rodriguez, M.; Lee, G.; Jordan, R.; Cihlar, T.; Birkus, G. Multiple Classes of Antiviral Agents Exhibit In Vitro Activity against Human Rhinovirus Type C. Antimicrob. Agents Chemother. 2014, 58, 1546–1555. [Google Scholar] [CrossRef]
- Li, X.; Geng, M.; Peng, Y.; Meng, L.; Lu, S. Molecular immune pathogenesis and diagnosis of COVID-19. J. Pharm. Anal. 2020, 10, 102–108. [Google Scholar] [CrossRef] [PubMed]
- Li, H.; Liu, L.; Zhang, D.; Xu, J.; Dai, H.; Tang, N.; Su, X.; Cao, B. SARS-CoV-2 and viral sepsis: Observations and hypotheses. Lancet 2020, 395, 1517–1520. [Google Scholar] [CrossRef]
- Cao, X. COVID-19: Immunopathology and its implications for therapy. Nat. Rev. Immunol. 2020, 20, 269–270. [Google Scholar] [CrossRef] [PubMed]
- Li, G.; Fan, Y.; Lai, Y.; Han, T.; Li, Z.; Zhou, P.; Pan, P.; Wang, W.; Hu, D.; Liu, X.; et al. Coronavirus infections and immune responses. J. Med Virol. 2020, 92, 424–432. [Google Scholar] [CrossRef] [PubMed]
- Warburton, D.E.R.; Nicol, C.W.; Bredin, S.S.D. Health benefits of physical activity: The evidence. Can. Med. Assoc. J. 2006, 174, 801–809. [Google Scholar] [CrossRef]
- Rossi, A.; Dikareva, A.; Bacon, S.L.; Daskalopoulou, S.S. The impact of physical activity on mortality in patients with high blood pressure: A systematic review. J. Hypertens. 2012, 30, 1277–1288. [Google Scholar] [CrossRef]
- Bouchard, C.; Blair, S.N.; Haskell, W.L. Physical Activity and Health; Human Kinetics: Champaign, IL, USA, 2012. [Google Scholar]
- Boreham, C.; Riddoch, C. The physical activity, fitness and health of children. J. Sports Sci. 2001, 19, 915–929. [Google Scholar] [CrossRef]
- Rasciute, S.; Downward, P. Health or Happiness? What Is the Impact of Physical Activity on the Individual? Kyklos 2010, 63, 256–270. [Google Scholar] [CrossRef]
- Pascoe, A.R.; Singh, M.A.; Edwards, K.M. The effects of exercise on vaccination responses: A review of chronic and acute ex-ercise interventions in humans. Brain Behav. Immun. 2014, 39, 33–41. [Google Scholar] [CrossRef]
- Martin, S.A.; Pence, B.; Woods, J.A. Exercise and Respiratory Tract Viral Infections. Exerc. Sport Sci. Rev. 2009, 37, 157–164. [Google Scholar] [CrossRef]
- Pedersen, B.K.; Hoffman-Goetz, L. Exercise and the Immune System: Regulation, Integration, and Adaptation. Physiol. Rev. 2000, 80, 1055–1081. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Leandro, C.G.; Castro, R.M.D.; Nascimento, E.; Pithon-Curi, T.C.; Curi, R. Adaptative mechanisms of the immune system in response to physical training. Rev. Bras. Med. Esporte. 2007, 13, 343–348. [Google Scholar] [CrossRef]
- Simpson, R.J.; Katsanis, E. The immunological case for staying active during the COVID-19 pandemic. Brain. Behav. Immun. 2020, 87, 6–7. [Google Scholar] [CrossRef]
- Nieman, D.C. Coronavirus disease-2019: A tocsin to our aging, unfit, corpulent, and immunodeficient society. J. Sport Health Sci. 2020, 9, 293–301. [Google Scholar] [CrossRef]
- Lu, R.; Zhao, X.; Li, J.; Niu, P.; Yang, B.; Wu, H.; Wang, W.; Song, H.; Huang, B.; Zhu, N.; et al. Genomic characterisation and epidemiology of 2019 novel coronavirus: Implications for virus origins and receptor binding. Lancet 2020, 395, 565–574. [Google Scholar] [CrossRef]
- Gleeson, M.; Bishop, N.C.; Stensel, D.J.; Lindley, M.R.; Mastana, S.S.; Nimmo, M.A. The anti-inflammatory effects of exercise: Mechanisms and implications for the prevention and treatment of disease. Nat. Rev. Immunol. 2011, 11, 607–615. [Google Scholar] [CrossRef]
- Cannon, J.G. Inflammatory Cytokines in Nonpathological States. Physiology 2000, 15, 298–303. [Google Scholar] [CrossRef]
- Hamer, M.; Kivimäki, M.; Gale, C.R.; Batty, G.D. Lifestyle risk factors, inflammatory mechanisms, and COVID-19 hospitaliza-tion: A community-based cohort study of 387,109 adults in UK. Brain. Behav. Immun. 2020, 87, 184–187. [Google Scholar] [CrossRef]
- Nieman, D.C.; Wentz, L.M. The compelling link between physical activity and the body’s defense system. J. Sport. Health Sci. 2019, 8, 201–217. [Google Scholar] [CrossRef]
- Damiot, A.; Pinto, A.J.; Turner, J.E.; Gualano, B. Immunological Implications of Physical Inactivity among Older Adults during the COVID-19 Pandemic. Gerontology 2020, 66, 431–438. [Google Scholar] [CrossRef]
- Li, Q.; Guan, X.; Wu, P.; Wang, X.; Zhou, L.; Tong, Y.; Ren, R.; Leung, K.S.M.; Lau, E.H.Y.; Wong, J.Y.; et al. Early transmission dynamics in Wuhan, China, of novel coronavirus–infected pneumonia. New. Engl. J. Med. 2020, 382, 1199–1207. [Google Scholar] [CrossRef] [PubMed]
- Cameron, A.C.; Miller, D.L. A Practitioner’s Guide to Cluster-Robust Inference. J. Hum. Resour. 2015, 50, 317–372. [Google Scholar] [CrossRef]
- Baron, R.M.; Kenny, D.A. The moderator–mediator variable distinction in social psychological research: Conceptual, strategic, and statistical considerations. J. Pers. Soc. Psychol. 1986, 51, 1173. [Google Scholar] [CrossRef] [PubMed]
- Ferreira, M.J.; Irigoyen, M.C.; Consolim-Colombo, F.; Saraiva, J.F.; Angelis, K.D. Physically active lifestyle as an approach to confronting COVID-19. Arq. Bras. Cardiol. 2020, 114, 601–602. [Google Scholar] [PubMed]
| Type | Name | Obs | Mean | Std. Dev. | Min | Max |
|---|---|---|---|---|---|---|
| dependent variable | case | 19,989 | 2.1221 | 1.8792 | 0 | 10.8199 |
| independent variable | RPA | 19,989 | 3.4891 | 0.8286 | 1.5586 | 6.8084 |
| control variable | measure | 19,989 | 5.2923 | 3.9634 | 0 | 10 |
| pop density | 19,989 | 4.7855 | 0.7808 | 2.8332 | 7.8047 | |
| information | 19,989 | 0.3730 | 0.4836 | 0 | 1 | |
| traffic | 19,989 | 6.7557 | 1.0995 | 4.1431 | 10.4860 | |
| effective distance | 19,989 | 5.7160 | 1.8739 | 0 | 7.7846 | |
| instrumental variable | sports establishments | 19,989 | 2.7952 | 1.9651 | 0 | 6.4061 |
| mediating variable | immunity | 19,989 | 18.2574 | 0.6818 | 16.0217 | 19.5768 |
| (1) | (2) | (3) | (4) | |
|---|---|---|---|---|
| OLS | 2SLS | First Stage | Reduced Form | |
| Case | Case | RPA | Case | |
| RPA | −0.4376 *** | −3.0335 *** | ||
| (0.0352) | (0.2918) | |||
| IV: sports establishments | 0.0004 *** | −0.0011 *** | ||
| (0.0000) | (0.0001) | |||
| public health | −0.1699 *** | −0.5043 *** | −0.0993 *** | −0.0948 *** |
| (0.0250) | (0.0409) | (0.0057) | (0.0287) | |
| pop density | 0.5948 *** | 3.2329 *** | 1.0382 *** | 0.0983 *** |
| (0.0408) | (0.3030) | (0.0044) | (0.0220) | |
| information | −0.2441 *** | 0.1090 *** | 0.0835 *** | −0.2015 *** |
| (0.0209) | (0.0362) | (0.0048) | (0.0238) | |
| traffic | 0.0940 *** | 0.1397 *** | −0.0167 *** | 0.1879 *** |
| (0.0131) | (0.0177) | (0.0035) | (0.0174) | |
| effective distance | −0.3847 *** | −0.2727 *** | 0.0329 *** | −0.3778 *** |
| (0.0061) | (0.0118) | (0.0014) | (0.0070) | |
| Control Variables | YES | YES | YES | YES |
| Province FE | YES | YES | YES | YES |
| Time FE | YES | YES | YES | YES |
| Observations | 19,989 | 19,989 | 19,989 | 19,989 |
| R-squared | 0.697 | 0.572 | 0.725 | 0.695 |
| F-statistics | 292.668 |
| (1) | (2) | (3) | (4) | (5) | |
|---|---|---|---|---|---|
| Exclude Hubei Province | Exclude January | Incubation = 4 | Incubation = 6 | Add Polynomial | |
| RPA | −0.2082 *** | −0.7163 *** | −0.4361 *** | −0.4390 *** | −0.5535 *** |
| (0.0312) | (0.0345) | (0.0343) | (0.0362) | (0.0275) | |
| quadratic term | −0.0003 | ||||
| (0.0001) | |||||
| cubic term | −2.5364 | ||||
| (1.1169) | |||||
| Control Variables | YES | YES | YES | YES | YES |
| Province FE | YES | YES | YES | YES | YES |
| Time FE | YES | YES | YES | YES | YES |
| Observations | 19,125 | 11,372 | 19,989 | 19,989 | 19,989 |
| R-squared | 0.734 | 0.733 | 0.703 | 0.690 | 0.792 |
| (1) | (2) | (3) | |
|---|---|---|---|
| Case | Immunity | Case | |
| RPA | −0.4376 *** | −0.0008 *** | −0.5032 *** |
| (0.0352) | (0.0001) | (0.0357) | |
| immunity | 0.0655 *** | ||
| (0.0081) | |||
| Control Variables | YES | YES | YES |
| Province FE | YES | YES | YES |
| Time FE | YES | YES | YES |
| Observations | 19,989 | 19,989 | 19,989 |
| R-squared | 0.697 | 0.475 | 0.698 |
| (1) | (2) | (3) | (4) | (5) | (6) | |
|---|---|---|---|---|---|---|
| Medical Resource_H | Medical Resource_L | Prevention Awareness_H | Prevention Awareness_L | Public Health_H | Public Health_L | |
| RPA | −0.4052 *** | −0.7668 *** | −0.2514 *** | −0.7213 *** | −0.4285 *** | −0.8546 *** |
| (0.0411) | (0.0534) | (0.0366) | (0.0354) | (0.0453) | (0.0472) | |
| Control Variables | YES | YES | YES | YES | YES | YES |
| Province FE | YES | YES | YES | YES | YES | YES |
| Time FE | YES | YES | YES | YES | YES | YES |
| Observations | 10,080 | 9909 | 9259 | 10,730 | 10,008 | 9981 |
| R-squared | 0.718 | 0.692 | 0.610 | 0.621 | 0.695 | 0.713 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lin, R.; Hu, X.; Chen, S.; Huang, J. Sports Participation and Anti-Epidemic: Empirical Evidence on the Influence of Regular Physical Activity on the COVID-19 Pandemic in Mainland China. Int. J. Environ. Res. Public Health 2022, 19, 10689. https://doi.org/10.3390/ijerph191710689
Lin R, Hu X, Chen S, Huang J. Sports Participation and Anti-Epidemic: Empirical Evidence on the Influence of Regular Physical Activity on the COVID-19 Pandemic in Mainland China. International Journal of Environmental Research and Public Health. 2022; 19(17):10689. https://doi.org/10.3390/ijerph191710689
Chicago/Turabian StyleLin, Ruofei, Xiaoli Hu, Shijun Chen, and Junpei Huang. 2022. "Sports Participation and Anti-Epidemic: Empirical Evidence on the Influence of Regular Physical Activity on the COVID-19 Pandemic in Mainland China" International Journal of Environmental Research and Public Health 19, no. 17: 10689. https://doi.org/10.3390/ijerph191710689