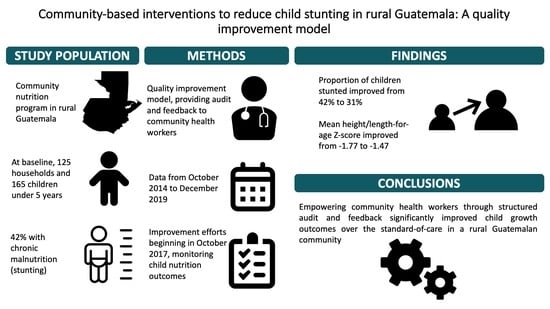
Community-Based Interventions to Reduce Child Stunting in Rural Guatemala: A Quality Improvement Model
Abstract
:1. Introduction
2. Materials and Methods
2.1. Participants and Setting
2.2. Description of Improvement Intervention
2.3. Data Collection and Measures
2.4. Analysis
3. Results
3.1. Baseline Characteristics of Participants and Caregivers
3.2. Monitoring of Process Improvement Indicators
3.3. Improvements in Child Growth Outcomes
3.4. Sensitivity Analysis
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- UNICEF. Malnutrition in Children. Available online: https://data.unicef.org/topic/nutrition/malnutrition/ (accessed on 26 November 2020).
- Lopez-Ridaura, S.; Barba-Escoto, L.; Reyna, C.; Hellin, J.; Gerard, B.; van Wijk, M. Food Security and Agriculture in the Western Highlands of Guatemala. Food Secur. 2019, 11, 817–833. [Google Scholar] [CrossRef] [Green Version]
- Government of Guatemala. Estrategia Nacional para la Prevención de la Desnutrición Crónica 2016–2020; Government of Guatemala: Guatemala City, Guatemala, 2016.
- Cordon, A.; Asturias, G.; De Vries, T.; Rohloff, P. Advancing Child Nutrition Science in the Scaling up Nutrition Era: A Systematic Scoping Review of Stunting Research in Guatemala. BMJ Paediatr. Open 2019, 3. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lovon, M. Evolución de las Estrategias de Reducción de la Desnutrición Crónica en Guatemala; Agropolis International, NIPN Global Support Facility: Montpellier, France, 2019. [Google Scholar]
- Ministerio de Salud Pública y Asistencia Social. Encuesta de Salud Materno Infantil 2014–2015; Ministerio de Salud Pública y Asistencia Social: Guatemala City, Guatemala, 2017.
- Sistema de Información Nacional de Seguridad Alimentaria y Nutricional. Situación de La Inseguridad Alimentaria Crónica En Guatemala; Sistema de Información Nacional de Seguridad Alimentaria y Nutricional: Guatemala City, Guatemala, 2018. [Google Scholar]
- Ola, A.L. La Cobertura del Primer Nivel de Atención en Salud Sigue Siendo Deficiente—13 September 2019, Prensa Libre. Available online: https://www.prensalibre.com/guatemala/comunitario/la-cobertura-del-primer-nivel-de-atencion-en-salud-sigue-siendo-deficiente/ (accessed on 26 November 2020).
- Maupin, J.N. “Fruit of the Accords”: Healthcare Reform and Civil Participation in Highland Guatemala. Soc. Sci. Med. 2009, 68, 1456–1463. [Google Scholar] [CrossRef] [PubMed]
- Scaling Up Nutrition. Homepage. Available online: https://scalingupnutrition.org/es/ (accessed on 26 November 2020).
- Martinez, B.; Webb, M.F.; Gonzalez, A.; Douglas, K.; Grazioso, M.D.P.; Rohloff, P. Complementary Feeding Intervention on Stunted Guatemalan Children: A Randomised Controlled Trial. BMJ Paediatr. Open 2018, 2, 213. [Google Scholar] [CrossRef] [PubMed]
- Pelletier, D.L.; Frongillo, E.A.; Gervais, S.; Hoey, L.; Menon, P.; Ngo, T.; Stoltzfus, R.J.; Ahmed, A.M.S.; Ahmed, T. Nutrition Agenda Setting, Policy Formulation and Implementation: Lessons from the Mainstreaming Nutrition Initiative. Health Policy Plan. 2012, 27, 19–31. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ballard, M.; Bonds, M.; Burey, J.; Dini, H.S.F.; Foth, J.; Furth, R.; Fiori, K.; Holeman, I.; Jacobs, T.; Johnson, A.; et al. CHW AIM: Updated Program Functionality Matrix for Optimizing Community Health Programs; USAID: Washington, DC, USA, 2018. [Google Scholar] [CrossRef]
- International Labor Organization. Convention C169—Indigenous and Tribal Peoples Convention, 1989 (No 169). Available online: https://www.ilo.org/dyn/normlex/en/f?p=NORMLEXPUB:12100:0::NO::P12100_ILO_CODE:C169 (accessed on 26 November 2020).
- Provost, L.P.; Murray, S.K. The Health Care Data Guide: Learning from Data for Improvement; Jossey-Bass: San Francisco, CA, USA, 2011. [Google Scholar]
- Leatherman, S.; Ferris, T.G.; Berwick, D.; Omaswa, F.; Crisp, N. The Role of Quality Improvement in Strengthening Health Systems in Developing Countries. Int. J. Qual. Heal. Care 2004, 16, 191–192. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ivers, N.; Jamtvedt, G.; Flottorp, S.; Young, J.M.; Odgaard-Jensen, J.; French, S.D.; O’Brien, M.A.; Johansen, M.; Grimshaw, J.; Oxman, A.D. Audit and Feedback: Effects on Professional Practice and Healthcare Outcomes. Cochrane Database Syst. Rev. 2012, 2012. [Google Scholar] [CrossRef] [PubMed]
- Martinez, B.; Flood, D.; Cnop, K.; Guzman, A.; Rohloff, P. Improving Infant and Young Child Nutrition in a Highly Stunted Rural Community: A Practical Case Study from Guatemala. In Handbook of Famine, Starvation, and Nutrient Deprivation; Springer International Publishing: Cham, Switzerland, 2017; pp. 1–19. [Google Scholar] [CrossRef]
- SQUIRE 2.0 Guidelines. Available online: http://squire-statement.org/ (accessed on 26 November 2020).
- World Health Organization. Indicators for Assessing Infant and Young Child Feeding Practices Part 2: Measurement; World Health Organization: Geneva, Switzerland, 2010. [Google Scholar]
- Coates, J.; Swindale, A.; Bilinsky, P. Household Food Insecurity Access Scale (HFIAS) for Measurement of Food Access: Indicator Guide: Version 3; FHI360/FANTA: Washington, DC, USA, 2007. [Google Scholar]
- Simple Poverty Scorecard, Guatemala 2006 Data. Available online: http://www.simplepovertyscorecard.com (accessed on 26 November 2020).
- INCAP. Guía Técnica para la Estandarización en Procesamiento, Análisis e Interpretación de Indicadores Antropometricos según los Patrones de Crecimiento de OMS para Menores de 5 Años. Available online: https://www.sdgfund.org/es/guía-técnica-para-la-estandarización-en-procesamiento-análisis-e-interpretación-de-indicadores (accessed on 24 November 2020).
- World Health Organization. WHO Child Growth Standards. Available online: https://www.who.int/childgrowth/en/ (accessed on 26 November 2020).
- Benneyan, J.C. Use and Interpretation of Statistical Quality Control Charts. Int. J. Qual. Healthc. 1998, 10, 69–73. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Nelson, L.S. Shewhart control chart—Tests for special causes. J. Qual. Technol. 1984, 16, 237–239. [Google Scholar] [CrossRef]
- Hossain, M.; Choudhury, N.; Adib, K.; Abdullah, B.; Mondal, P.; Jackson, A.A.; Walson, J.; Ahmed, T. Evidence-Based Approaches to Childhood Stunting in Low and Middle Income Countries: A Systematic Review. Arch. Dis. Child. 2017, 102, 903–909. [Google Scholar] [CrossRef] [PubMed]
- Cleaves, C.; Tuy, H.; Parens, C. Análisis Sistémico y Territorial de La Seguridad Alimentaria y Nutricional En Guatemala: Consideraciones Para Mejorar Prácticas y Políticas Públicas; Universidad Rafael Landivar: Guatemala City, Guatemala, 2015. [Google Scholar]
- ASIES. Revisión Estratégica de la Situación de Seguridad Alimentaria y Nutricional en Guatemala; World Food Program: Guatemala City, Guatemala, 2017. [Google Scholar]
- Tuti, T.; Nzinga, J.; Njoroge, M.; Brown, B.; Peek, N.; English, M.; Paton, C.; van der Veer, S.N. A Systematic Review of Electronic Audit and Feedback: Intervention Effectiveness and Use of Behaviour Change Theory. Implement. Sci. 2017, 12. [Google Scholar] [CrossRef] [PubMed]
- Ayieko, P.; Irimu, G.; Ogero, M.; Mwaniki, P.; Malla, L.; Julius, T.; Chepkirui, M.; Mbevi, G.; Oliwa, J.; Agweyu, A.; et al. Effect of Enhancing Audit and Feedback on Uptake of Childhood Pneumonia Treatment Policy in Hospitals That Are Part of a Clinical Network: A Cluster Randomized Trial. Implement. Sci. 2019, 14, 20. [Google Scholar] [CrossRef] [PubMed]
- Rowe, S.Y.; Peters, D.H.; Holloway, K.A.; Chalker, J.; Ross-Degnan, D.; Rowe, A.K. A Systematic Review of the Effectiveness of Strategies to Improve Health Care Provider Performance in Low- and Middle-Income Countries: Methods and Descriptive Results. PLoS ONE 2019, 14, e0217617. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Pérez-Cuevas, R.; Guiscafré, H.; Muñoz, O.; Reyes, H.; Tomé, P.; Libreros, V.; Gutiérrez, G. Improving Physician Prescribing Patterns to Treat Rhinopharyngitis. Intervention Strategies in Two Health Systems of Mexico. Soc. Sci. Med. 1996, 42, 1185–1194. [Google Scholar] [CrossRef]
- Kafle, K.K.; Shrestha, N.; Karkee, S.B.; Prasad, R.R.; Bhuju, G.B.; Das, P.L. Intervention Studies on Rational Use of Drugs in Public and Private Sector in Nepal. Nepal Med. Coll. J. 2005, 7, 47–50. [Google Scholar] [PubMed]
- Chowdhury, A.K.A.; Khan, O.F.; Matin, M.A.; Begum, K.; Galib, M.A. Effect of standard treatment guidelines with or without prescription audit on prescribing for acute respiratory tract infection (ARI) and diarrhoea in some thana health complexes (THCs) of Bangladesh. Bangladesh Med. Res. Counc. Bull. 2007, 33, 21–30. [Google Scholar] [PubMed]
- Garba, M.A.; Mustapha, G.M.; Rejoice, C.; Mustapha, B.; Alhaji, M.A.; Bello, I.A.; Hassan, A.E. Competency-Based Learning: The Effectiveness of Targeted Resident Education and Clinical Auditing Feedback on Completed Death Certificate Accuracy Rates. Niger. J. Paediatr. 2015, 42, 132–136. [Google Scholar]
- Bazant, E.; Sarkar, S.; Banda, J.; Kanjipite, W.; Reinhardt, S.; Shasulwe, H.; Mulilo, J.M.C.; Kim, Y.M. Effects of a Performance and Quality Improvement Intervention on the Work Environment in HIV-Related Care: A Quasi-Experimental Evaluation in Zambia. Hum. Resour. Health 2014, 12, 73. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Feyissa, G.T.; Balabanova, D.; Woldie, M. How Effective Are Mentoring Programs for Improving Health Worker Competence and Institutional Performance in Africa? A Systematic Review of Quantitative Evidence. J. Multidiscip. Healthc. 2019, 12, 989–1005. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Malaria Consortium. Scalable Interventions to Increase Community Health Worker Motivation and Performance: Randomised Controlled Trials in Mozambique and Uganda. Available online: https://www.malariaconsortium.org/media-downloads/1218/Scalable%20interventions%20to%20increase%20community%20health%20worker%20motivation%20and%20performance:%20Randomised%20controlled%20trials%20in%20Mozambique%20and%20Uganda (accessed on 26 November 2020).
- Rice, H.E.; Lou-Meda, R.; Saxton, A.T.; Johnston, B.E.; Ramirez, C.C.; Mendez, S.; Rice, E.N.; Aidar, B.; Taicher, B.; Baumgartner, J.N.; et al. Building a Safety Culture in Global Health: Lessons from Guatemala. BMJ Glob. Health 2018, 3. [Google Scholar] [CrossRef] [PubMed] [Green Version]






| Component | Rationale | Example Interaction |
|---|---|---|
| Refresher group trainings, focused on role-play of worker-caregiver interactions | Small groups of frontline workers simulate challenging clinical encounters, allowing for peer feedback on body language, counselling strategy, and other skills | A frontline worker demonstrates a skilled approach to caregivers’ concerns that they “don’t have time” to peers |
| Individual audit/feedback of home visits by nutrition supervisor | Supervision of home visits, if conducted respectfully, can provide opportunities to reflect and improve interpersonal skills | Supervisor notes frontline worker struggling with a loud home environment, together they work to strategize how best to delivery content when multiple children are present |
| Automatic To-Do lists for pending growth monitoring, nutrition supplements, and clinical visits generated from electronic health record | Manually tracking program tasks is time-consuming and prone to error, leading to beneficiaries and program components being missed | Frontline worker has a busy work day and doesn’t notice that a child with severe malnutrition misses their appointment. After checking the task list, they notice the pending item and make a special home visit. |
| Automatic dashboard of process indicators (proportions of children receiving recommended growth monitoring, clinical visits, and nutrition supplements), with monthly individual review with supervisor | Visualization of process indicators, with the help of a supportive supervisor, can help identify “what’s working” and “what’s not working” and leading to creative problem solving | Supervisor points out that frontline worker’s home visit numbers were much higher than in previous months. Frontline work notes that phone calls the night before planned visits were effective at ensuring caregivers were prepared, and resolves to adopt this strategy going forward. |
| Outcome Indicators | Description |
| Prevalence of stunting | Proportion of children under 5 years of age with a height/length-for-age Z-score of less than—2 |
| Height/length for age Z-score | Quarterly mean of height/length-for-age Z-score measures on all children under 5 years of age |
| Process Indicators | Description |
| Micronutrient Delivery | Proportion of eligible children with monthly documentation of micronutrient dosing in electronic health record |
| Growth Monitoring | Proportion of eligible children with monthly visits where weight and height were taken and documented in electronic health record |
| Program Enrollment/Stability | Quarterly number of children under 5 years enrolled in the community nutrition program |
| Characteristic 1 | Value |
|---|---|
| Household characteristics | |
| Household size, n | 4 (3, 5) |
| Children under 5 years in home, n | 1 (1, 2) |
| Grows food for home consumption, % | 29 |
| Raw poverty score 2 | 32 (25, 37) |
| Moderate or severe food insecurity, % | 50 |
| Child characteristics | |
| Child age, months | 23 (16, 33) |
| Female sex, % | 54 |
| Height/length-for-age Z score | −2.15 (−2.91, −1.39) |
| Weight-for-age Z score | −1.25 (−1.95, 0.46) |
| Stunted, % 3 | 52 |
| Meets minimum dietary diversity, % 4,5 (n = 71) | 58 |
| Meets minimum meal frequency, % 4,6 | 56 |
| Diarrhea in last two weeks, % | 36 |
| Fever in last two weeks, % | 29 |
| Respiratory symptoms in last two weeks, % | 58 |
| Caregiver characteristics | |
| Head of household works as agricultural day-laborer, % | 71 |
| Paternal education, primary school or less | 57 |
| Maternal education, primary school or less | 74 |
| Maternal pregnancies, n | 2 (2, 4) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Juarez, M.; Dionicio, C.; Sacuj, N.; Lopez, W.; Miller, A.C.; Rohloff, P. Community-Based Interventions to Reduce Child Stunting in Rural Guatemala: A Quality Improvement Model. Int. J. Environ. Res. Public Health 2021, 18, 773. https://doi.org/10.3390/ijerph18020773
Juarez M, Dionicio C, Sacuj N, Lopez W, Miller AC, Rohloff P. Community-Based Interventions to Reduce Child Stunting in Rural Guatemala: A Quality Improvement Model. International Journal of Environmental Research and Public Health. 2021; 18(2):773. https://doi.org/10.3390/ijerph18020773
Chicago/Turabian StyleJuarez, Michel, Carlos Dionicio, Neftali Sacuj, Waleska Lopez, Ann C. Miller, and Peter Rohloff. 2021. "Community-Based Interventions to Reduce Child Stunting in Rural Guatemala: A Quality Improvement Model" International Journal of Environmental Research and Public Health 18, no. 2: 773. https://doi.org/10.3390/ijerph18020773