How Do Hospital Medical and Nursing Managers Perceive Work-Related Strain on Their Employees?
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Recruitment
2.3. Design of Interview
2.4. Data Analysis
2.5. Sample
3. Results
3.1. Positive Short-Term Strain and Mid-Term Strain Consequences
3.2. Negative Short-Term Strain and Mid-Term Strain Consequences
3.3. Positive Long-Term Strain Consequences
3.4. Negative Long-Term Strain Consequences
4. Discussion
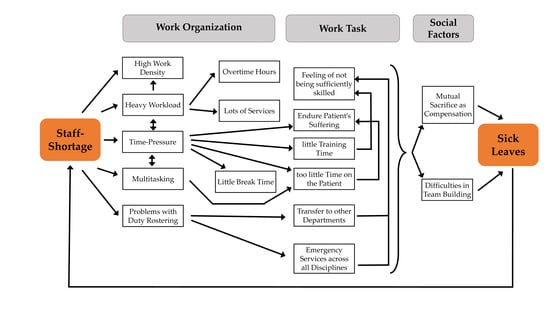
4.1. Sickness Absence as a Result of Work Stress due to Staff Shortage
4.2. Limitations of the Study
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Gregersen, S.; Kuhnert, S.; Zimber, A.; Nienhaus, A. Führungsverhalten und Gesundheit–Zum Stand der Forschung. Das Gesundheitswesen 2011, 73, 3–12. [Google Scholar] [CrossRef] [PubMed]
- Schmidt, B.; Herr, R.M.; Jarczok, M.N.; Baumert, J.; Lukaschek, K.; Emeny, R.T.; Ladwig, K.-H.; KORA Investigators. Lack of supportive leadership behavior predicts suboptimal self-rated health independent of job strain after 10 years of follow-up: Findings from the population-based MONICA/KORA study. Int. Arch. Occup. Environ. Health 2018, 91, 623–631. [Google Scholar] [CrossRef] [PubMed]
- Schmidt, B.; Loerbroks, A.; Herr, R.M.; Wilson, M.G.; Jarczok, M.N.; Litaker, D.; Mauss, D.; Bosch, J.A.; Fischer, J.E. Associations between supportive leadership and employees self-rated health in an occupational sample. Int. J. Behav. Med. 2014, 21, 750–756. [Google Scholar] [CrossRef]
- Montano, D.; Reeske, A.; Franke, F.; Hüffmeier, J. Leadership, followers’ mental health and job performance in organizations: A comprehensive meta-analysis from an occupational health perspective. J. Organ. Behav. 2016, 38, 327–350. [Google Scholar] [CrossRef]
- Theorell, T.; Hammarström, A.; Aronsson, G.; Träskman Bendz, L.; Grape, T.; Hogstedt, C.; Marteinsdottir, I.; Skoog, I.; Hall, C. A systematic review including meta-analysis of work environment and depressive symptoms. BMC Public Health 2015, 15, 738. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jarczok, M.N.; Jarczok, M.; Mauss, D.; Koenig, J.; Li, J.; Herr, R.M.; Thayer, J.F. Autonomic nervous system activity and workplace stressors—A systematic review. Neurosci. Biobehav. Rev. 2013, 37, 1810–1823. [Google Scholar] [CrossRef]
- Theorell, T.; Jood, K.; Järvholm, L.S.; Vingård, E.; Perk, J.; Östergren, P.O.; Hall, C.A. systematic review of studies in the contributions of the work environment to ischaemic heart disease development. Eur. J. Public Health 2016, 26, 470–477. [Google Scholar] [CrossRef] [Green Version]
- Angerer, P.; Petru, R.; Nowak, D.; Weigl, M. Arbeitsbedingungen und Depression bei Ärzten. Dtsch. Med. Wochenschr. 2008, 133, 26–29. [Google Scholar] [CrossRef]
- Pisljar, T.; Van der Lippe, T.; Den Dulk, L. Health among hospital employees in Europe: A cross-national study of the impact of work stress and work control. Soc. Sci. Med. 2011, 72, 899–906. [Google Scholar] [CrossRef]
- Coutinho, H.; Queirós, C.; Henriques, A.; Norton, P.; Alves, E. Work-related determinants of psychosocial risk factors among employees in the hospital setting. Work 2018, 61, 551–560. [Google Scholar] [CrossRef]
- Parent-Thirion, A.; Isabella, B.; Cabrita, J.; Vargas, O.; Vermeylen, G.; Wilczynska, A.; Wilkens, M. Sixth European Working Conditions Survey; Eurofound: Dublin, Ireland, 2017. [Google Scholar]
- Parent-Thirion, A.; Hurley, J.; Vermeylen, G. Fourth European Working Conditions Survey; European Foundation for the Improvement of Living and Working Conditions: Dublin, Ireland, 2007. [Google Scholar]
- Romani, M.; Ashkar, K. Burnout among physicians. Libyan J. Med. 2014, 9, 23556. [Google Scholar] [CrossRef]
- Von dem Knesebeck, O.; Klein, J.; Frie, K.G.; Blum, K.; Siegrist, J. Psychosoziale Arbeitsbelastungen bei chirurgisch tätigen Krankenhausärzten. Dtsch. Arztebl. Int. 2010, 107, 248–253. [Google Scholar] [CrossRef] [PubMed]
- Aiken, L.H.; Sermeus, W.; Van den Heede, K.; Sloane, D.M.; Busse, R.; McKee, M.; Bruyneel, L.; Rafferty, A.M.; Griffiths, P.; Moreno-Casbas, M.T.; et al. Patient safety, satisfaction, and quality of hospital care: Cross sectional surveys of nurses and patients in 12 countries in Europe and the United States. BMJ 2012, 344, e1717. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Viswesvaran, C.; Sanchez, J.I.; Fisher, J. The role of social support in the process of work stress: A meta-analysis. J. Vocat. Behav. 1999, 54, 314–334. [Google Scholar] [CrossRef]
- Stadler, P.; Spieß, E. Mit Verstand und Verständnis, Mitarbeiterorientiertes Führen und soziale Unterstützung am Arbeitsplatz, Bundesanstalt für Arbeitsschutz und Arbeitsmedizin, 4th ed.; Bonifatius: Berlin, Germany; Paderborn, Germany, 2003; p. 381. [Google Scholar]
- Heifetz, R.A. Leadership without Easy Answers; Belknap Press of Harvard University Press: Cambridge, MA, USA, 1994; Volume 465. [Google Scholar]
- Van der Wal, M.A.; Scheele, F.; Schönrock-Adema, J.; Jaarsma, A.D.; Cohen-Schotanus, J. Leadership in the clinical workplace: What residents report to observe and supervisors report to display: An exploratory questionnaire study. BMC Med. Educ. 2015, 15, 195. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chapman, A.L.; Johnson, D.; Kilner, K. Leadership styles used by senior medical leaders: Patterns, influences and implications for leadership development. Leadersh Health Serv. 2014, 27, 283–298. [Google Scholar] [CrossRef]
- Martin, W.; Keogh, T. Managing medical groups: 21st century challenges and the impact of physician leadership styles. J. Med. Pract. Manag 2004, 20, 102. [Google Scholar]
- CCL. Addressing the Leadership Gap in Healthcare. What’s Needed When it Comes to Leader Talent? A white paper; Center for Creative Leadership: Greensboro, NC, USA, 2010. [Google Scholar]
- Prezerakos, P.E. Nurse Managers’ Emotional Intelligence and Effective Leadership: A Review of the Current Evidence. Open Nurs. J. 2018, 12, 86–92. [Google Scholar] [CrossRef] [Green Version]
- Schreuder, J.A.; Roelen, C.A.; Van Zweeden, N.F.; Jongsma, D.; Van der Klink, J.J.; Groothoff, J.W. Leadership styles of nurse managers and registered sickness absence among their nursing staff. Health Care Manag. Rev. 2011, 36, 58–66. [Google Scholar] [CrossRef]
- DIN e.V. (Hrsg.). (DIN EN ISO 10075-1:2017): DIN EN ISO 10075-1:2018-01), Ergonomic Principles Related to Mental Workload—Part 1: General Issues and Concepts, Terms and Definitions; Beuth-Verlag: Berlin, Germany, 2017. [Google Scholar]
- Joiko, K.; Schmauder, M.; Wolff, G. Psychische Belastungen und Beanspruchung im Berufsleben, Erkennen und Gestalten, Bundesanstalt für Arbeitsschutz und Arbeitsmedizin, 5; Auflage, Bundesanstalt für Arbeitsschutz und Arbeitsmedizin: Dortmund, Germany, 2010. [Google Scholar]
- Lazarus, R.S.; Folkman, S. Transactional theory and research on emotions and coping. Eur. J. Pers. 1987, 1, 141–169. [Google Scholar] [CrossRef]
- Genrich, M.; Worringer, B.; Angerer, P.; Müller, A. Hospital Medical and Nursing Managers’ Perspectives on Health-Related Work Design Interventions. A Qualitative Study. Front. Psychol. 2020, 11, 869. [Google Scholar] [CrossRef] [PubMed]
- Worringer, B.; Genrich, M.; Müller, A.; Gündel, H. Contributors of the SEEGEN Consortium, Angerer, P. Hospital Medical and Nursing Managers’ Perspective on the Mental Stress of Employees. IJERPH. submitted.
- Glaser, B.; Strauss, A. The Discovery of Grounded Theory: Strategies for Qualitative Research; Aldine Publishing Company: New York, NY, USA, 1967. [Google Scholar]
- Guest, G.; Bunce, A.; Johnson, L. How Many Interviews Are Enough? Field Methods 2016, 18, 59–82. [Google Scholar] [CrossRef]
- Hsieh, H.F.; Shannon, S.E. Three approaches to qualitative content analysis. Qual. Health Res. 2015, 15, 1277–1288. [Google Scholar] [CrossRef]
- Elo, S.; Kyngas, H. The qualitative content analysis process. J. Adv. Nurs. 2008, 62, 107–115. [Google Scholar] [CrossRef] [PubMed]
- Mayring, P. Qualitative Inhaltsanalyse: Grundlagen und Techniken, 12th ed.; Beltz: Weinheim, Germany, 2015. [Google Scholar]
- Potter, W.J.; Levine-Donnerstein, D. Rethinking validity and reliability in content analysis. J. Appl. Commun. Res. 1999, 27, 258–284. [Google Scholar] [CrossRef]
- Creswell, J.W. Research design: Qualitative, quantitative, and mixed methods approaches, 4th ed.; Sage: Los Angeles, CA, USA, 2014. [Google Scholar]
- McHugh, M.L. Interrater reliability: The kappa statistic. Biochem. Med. 2012, 276–282. [Google Scholar] [CrossRef]
- Duijts, S.F.; Kant, I.; Swaen, G.M.; Van den Brandt, P.A.; Zeegers, M.P. A meta-analysis of observational studies identifies predictors of sickness absence. J. Clin. Epidemiol. 2007, 60, 1105–1115. [Google Scholar] [CrossRef]
- Nieuwenhuijsen, K.; Bruinvels, D.; Frings-Dresen, M. Psychosocial work environment and stress-related disorders, a systematic review. Occup. Med. 2010, 60, 277–286. [Google Scholar] [CrossRef] [Green Version]
- Stansfeld, S.; Candy, B. Psychosocial work environment and mental health—A meta-analytic review. Scand. J. Work Environ. Health 2006, 32, 443–462. [Google Scholar] [CrossRef]
- Netterstrøm, B.; Conrad, N.; Bech, P.; Fink, P.; Olsen, O.; Rugulies, R.; Stansfeld, S. The relation between work-related psychosocial factors and the development of depression. Epidemiol. Rev. 2008, 30, 118–132. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Schreuder, J.A.H. Managing Sickness Absence: Leadership and Sickness Absence Behaviour in Hospital Care; University Medical Center Groningen, University of Groningen: Groningen, The Netherlands, 2012. [Google Scholar]
- Ones, D.S.; Viswesvaran, C.; Schmidt, F.L. Personality and absenteeism: A meta-analysis of integrity tests. Eur. J. Pers. 2003, 17, S19–S38. [Google Scholar] [CrossRef]
- Wattles, M.G.; Harris, C. The relationship between fitness levels and employee’s perceived productivity, job satisfaction, and absenteeism. J. Exerc. Physiol. Online 2003, 6, 24–32. [Google Scholar]
- Sagherian, K.; Geiger-Brown, J.; Rogers, V.E.; Ludeman, E. Fatigue and risk of sickness absence in the working population: A systematic review and meta-analysis of longitudinal studies. Scand. J. Work Environ. Health 2019, 45, 333–345. [Google Scholar] [CrossRef] [PubMed]
- van Oostrom, S.H.; Driessen, M.T.; De Vet, H.C.; Franche, R.L.; Schonstein, E.; Loisel, P.; Van Mechelen, W.; Anema, J.R. Workplace interventions for preventing work disability. Cochrane Database Syst. Rev. 2009, 2, CD006955. [Google Scholar] [CrossRef]
- Vargas-Prada, S.; Demou, E.; Lalloo, D.; Avila-Palencia, I.; Sanati, K.A.; Sampere, M.; Freer, K.; Serra, C.; Macdonald, E.B. Effectiveness of very early workplace interventions to reduce sickness absence: A systematic review of the literature and meta-analysis. Scand. J. Work Environ. Health 2016, 42, 261–272. [Google Scholar] [CrossRef] [Green Version]
- Hall, G.B.; Dollard, M.F.; Winefield, A.H.; Dormann, C.; Bakker, A.B. Psychosocial safety climate buffers effects of job demands on depression and positive organizational behaviors. Anxiety Stress Coping 2013, 26, 355–377. [Google Scholar] [CrossRef]
- Biron, C.; Baril-Gingras, G.; Lefebvre, R.; Chabot, S.; Boulay-Leclerc, S. Factors influencing managers’ ownership of organisational health interventions. In Psychosocial Safety Climate. A New Work Stress Theory, 1st ed.; Dolard, M.F., Dormann, C., Idris, M.A., Eds.; Springer Nature: Cham, Switzerland, 2019; pp. 365–384. [Google Scholar]
- Mulfinger, N.; Sander, A.; Stuber, F.; Brinster, R.; Junne, F.; Limprecht, R.; Jarczok, M.N.; Seifried-Dübon, T.; Rieger, M.A.; Zipfel, S.; et al. Cluster-randomised trial evaluating a complex intervention to improve mental health and well-being of employees working in hospital—A protocol for the SEEGEN trial. BMC Public Health 2019, 19, 1694. [Google Scholar] [CrossRef]

| Main Categories | Definition |
|---|---|
| Positive Short-term Strain and Mid-term Strain Consequences | The managers’ perception of positive reactions of employees to stressors, such as thoughts, feelings, physical reactions, behavior, and professional performance |
| Negative Short-term Strain and Mid-term Strain Consequences | The managers’ perception of negative reactions of employees to stressors, such as thoughts, feelings, physical reactions, behavior, and professional performance |
| Positive Long-term Strain Consequences | The managers’ perception of positive long-term reactions of employees to strain, such as psychosomatic disorders and diseases |
| Negative Long-term Strain Consequences | The managers’ perception of negative long-term reactions of employees to strain, such as psychosomatic disorders and diseases |
| Chief Physicians | Senior Physicians | Senior Nurses | |
|---|---|---|---|
| Female | 2 | 2 | 9 |
| Male | 12 | 7 | 5 |
| Total | 14 | 9 | 14 |
| Age range [years] | 43–60 | 38–60 | 34–60 |
| Mean age [years] | 51.9 | 43.6 | 47.9 |
| Mean number of years employed | 5.4 | 8.7 | 23.4 |
| Positive Short-Term Strain and Mid-Term Strain Consequences (PST) |
| PST-1: There are still people who do, who like to come and work. This means not only these average planned services, but also when we really need and look for someone, they still come. Then of course we try to support them a little bit. And financially arrange it somehow. They are also in agreement with that. And also satisfied, actually. (SN 22) |
| Negative Short-term Strain and Mid-term Strain Consequences (NST) |
| NST-1: This, so to say this low staffing level, also leads to an I would say disproportionately high amount of on-call duties of individual employees. And this makes rest time almost impossible. And the employees appear extremely exhausted. (SP 33) |
| NST-2: But I think that many people would affirm the fact that you somehow feel unbalanced or other. (SP 35) |
| NST-3: That you really calm down, that is, in my opinion, such an important aspect. That you also learn how to switch off. A lot of nurses can’t do that either, they go home and they can’t get what happened at work out of their minds, it keeps them busy for hours. (SN 25). NST-4: You often call here from home, because you get some rest there and then you realize what you have forgotten, for example. (SN 28) NST-5: You go home in the evening with so many things in mind and feel like you’ve forgotten 20 things. (SP 34). |
| NST-6: Now we have to meet many, many, many demands and that makes some of the employees insecure and nervous. (SN 17) NST-7: My colleague quickly becomes restless in that case and is then briefly tied up, a bit grumpy towards the patients or towards me, when she feels a bit stressed. (SN 21) |
| NST-8: Yeah, so they either get indignant or they work even more slowly. (CP 2) NST-9: The colleagues are annoyed. ... That means that the colleagues simply become aggressive in tone at some point. Among each other. (SN 24) |
| NST-10: I think that a little bit of resignation resonates with everyone, because the moment someone fails, you have to fill this gap somehow. (SN 18) NST-11: So, the tasks are not carried out in the way you would have wanted, because the day has only 24 h and not 27 h to complete. And then, there is a really bad mood sometimes. …This means that from this side there is always a certain potential for conflict and this leads to a yes, resignation, an ‘I-don’t-care-mentality’, and then to a complete switch-off in the end. (CP 6) |
| NST-12: Yes, sometimes this is immediately reflected, that sometimes some employees reach their limits and say, I don’t know what to do first. (SP 40) |
| NST-13: But it is often the case that this feeling of injustice then becomes very strong. My burden is very great, and it is less great with the others. (SP 35). NST-14: Stress, yes, it does not necessarily help to maintain the team climate. And a bad team climate, I would say, messes up everyday life even more, and then there is a downward spiral. (CP 5) NST-15: But it is indeed the case that we sometimes resign ourselves to the clinical picture and are then frustrated that we have not managed to save human life. …Sometimes I see tears in the faces of the nurses or even doctors, for example when a course of treatment has not developed so well.… This is also noticeable not only visually, but you also feel that the mood is tilting. It becomes quiet. People are less open-minded towards each other. The many nurses and also doctors take this with them. And you notice a certain silence. And this silence always proofs that we were of course very dissatisfied and unhappy with the course of events. (SP 37) |
| NST-16: They are looking for a conversation with me, because then they often try to pass the tasks on to the next higher level and say, ‘Can you please decide that, I can’t do that. (SP 35) |
| NST-17: So, there are conflicts, it is rarely the case that there is rejection and open conflict and ‘I’m not doing that! Then I quit. (CP 13) |
| NST-18: Because just when they are really on their last legs, sometimes a little thing is forgotten, or they just can’t give 100%, different from what you are usually used to from your employees. (SN 26) NST-19: We can no longer give the medication, give tablets, care is omitted, only when really needed, and this is different from what we have learned in our training. (SN20) |
| NST-20: …and you can also tell by the mistakes. So now not treatment errors, but errors in the processes, uncertainties in the processes, which occur as a result. (CP 10) |
| NST-21: A colleague was doing a procedure on a patient. A complication occurred with this procedure. And this patient then became lifeless because of this measure, which was actually a very simple one, not such a highly dramatic one. He had to be resuscitated. And while we are carrying out the resuscitation measures on this patient, this colleague not only leaves the room, not only the intensive care unit, no, he leaves the hospital without saying a word, without signing out, but simply because he is dealing with this emotional situation, he has just been responsible for this event. (SP 37) |
| Positive Long-Term Strain Consequences (PLT) |
| PLT-1: When people come up to me and tell me that they think it’s great what we have here. And what we do here. And that they feel good, and that they like working here. (ID 15) PLT-2: …at the moment I have the feeling that the mood in the team, at least with 90 percent, is very good. (ID 10) PLT-3: I have the impression that everything is working quite evenly in our department at the moment, and I would simply assume that they are all emotionally stable. (ID 12) |
| PLT-4: But the tendency, and I’m not alone now, is rather that rather, we have little downtime, so hardly anyone here is sick because of a little cold. (ID 11) |
| PLT-5: …many of them have already been there for a long time in these five years. And so, for once, the ones I took over, but also those who came after. They all like being here too. That is the case. Those who left had a hard time leaving. It was mostly for family reasons. (ID 2). PLT-6: We actually do not have such a high turnover of employees. (ID 9) |
| Negative Long-term Strain Consequences (NLT) |
| NLT-1: Well, I am sure that a relevant part of the sick days is like a call for help or dissatisfaction or maybe also caused by some kind of pressure. (CP 13) NLT-2: You could say they get sick if you push them too hard. Well, call in sick then. (CP 2) NLT-3: And work strain leads to reoccurring sick certificates, so that a very well-planned duty schedule has to be rescheduled all of a sudden. (SN 27) NLT-4: In the field of nursing, it must be said, there is understaffing, which favors overwork, sickness absence, so that the rat tail then, people always get sick. I believe that this is a problem of staffing, a personnel staffing problem. (SN38) NLT-5: We spend a large part of our lifetime here in the hospital or at work, and it is certainly the case that the employees are burdened by this daily work routine, by this stress and possibly also become mentally ill. The subject of burnout certainly also exists in the medical field and this hospital, the department not excluded, it is a topic. We somewhat notice this when employees are absent for longer periods of time because of somatic illnesses in fact, which are difficult to diagnose and record. For example, if I go into detail, myocarditis or myocarditis after an untreated flu is always something like that. This might sound strange now, but often employees who already are a bit older are absent for a long period of time. In the past years, in six years I have been here, we have had two employees who had been absent for six to eight weeks because of these complaints. This could actually be seen as some kind of new form of burnout or stress. (SP 40) |
| NLT-6: The load is so high that they can no longer relax at all. Because they’re required to step in constantly. You have to organize yourself. To jump in on weekends or days off, to come back from vacation, that certainly is a burden, because the body can no longer calm down. (SN 19) |
| NLT-7: The resistance to, let’s say, general illnesses is lowered when I basically have to work all the time in a state of exhaustion. (CP 11) |
| NLT-8: A permanent strain that cannot be overcome naturally makes you ill. Unfortunately, I have just experienced this with a long-time secretary. (CP 7) |
| NLT-9: And then even a slight headache can sometimes be like that, I will say now. Or a general feeling of unease. (CP 6) NLT-10: And since the workload is significantly higher and I then hear directly from the nursing staff, sometimes verbally, that there is dissatisfaction, relatively often, I also see nursing staff who present themselves with complaints here, where there is little organic correlation. At that point, you must already assume that there is a certain stress situation causing physical symptoms. (SP 36) NLT-11: That they simply also have physical complaints from time to time due to the mental strain. It’s all connected. Soul and body. And that they then also simply say they have headaches, one or two days in a row, but basically, it’s the great strain as an example. It happens. (SN 25) |
| NLT-12: There are colleagues who simply complain about sleep disorders. (SN 24). NLT-13: …she has got teeth grinding and also received a bite splint from the physician. She can barely relax at home either and still thinks, ‘Did I forget anything?’ She has trouble falling asleep and sometimes wakes up in the middle of the night, which she didn’t have before when she was working on another ward, with more staff and where things were not as concentrated on one person. (SN 21) |
| NLT-14: …there has been a real, yes disease state in the past years so that you could have equipped the whole hospital. For years, I have had more than thousand sick days every year in one single ward. People were indeed massively ill. On the one hand there were, typical illnesses for our professional life, slipped discs yes, this kind of issues. But there were also psychological stresses. Starting with burn-out. (SN 22) NLT-15: So, they may get physically sick faster, but I think they also become less resilient and that, I think, is always an expression of a yes, I would take it as exhaustion. You can take it to the point of exhaustion depression, which basically means that you lose motivation. (CP 11) NLT-16: So, it starts with you thinking, oh god, today again, probably it will come back, yes, I think so, it has something to do with the mood. Well, it is certainly not as good as it used to be. (SN29) NLT-17: Burnout. Yeah. And especially someone I would have never thought of. (SN 16) |
| NLT-18: And if this continues for days, the entire immune system collapses…don’t dare go back to the ward either. Some people also get scared of their jobs. (SN 20). NLT-19: You just come with a certain yes, also fear, I would say, no fear of work, but fear of what awaits me. Can I manage the work at all? (SN 24) |
| NLT-20: In individual situations, this can of course lead to such a heavy burden for the affected person that he or she says, ‘I don’t feel well there, I’m afraid to do emergency services. And then they withdraw. …So, there is a very clear threat to employees, who can then also develop personal fear. (CP 9) |
| NLT-21: We have had a time where the conversational tone among each other has also been very bad. (CP 10) NLT-22: And I think this uncertainty also leads to unrest in the team and to many people looking at each other, comparing each other, who does more of this or that.’ …’ you already notice this in rush hours, that people then go at each other’s throats for a little something, and you think they would not have done that at all under normal circumstances. (SN 17) NLT-23: They feel totally overloaded. And they officially say so. Of course, this also leads to stress situations in the team, with the same people being affected over and over again, because the stronger people naturally assert themselves and they simply don’t come. (SN 22) |
| NLT-24: And in nursing, the areas are being expanded, so that there is actually more and more anonymity, which has the advantage, from a business point of view, that people are interchangeable. And if somebody gets sick, I can very quickly swap with someone else. In my opinion, the quality and satisfaction of the individual colleagues also decreases. Simply because this appreciation is missing in my everyday life. (SP 36) |
| NLT-25: The connection then with the company, the connection with your employer or your clinic, which was perhaps always the case in the past, does certainly not exist today. (CP 6) |
| NLT-26: Because of course there are also certain colleagues of mine with whom one perhaps cannot discuss such things constructively. But even a little bit of resignation yes, so when they do, I often have the impression that the assistants simply have to go out into the street a bit, to put it in a figurative way, and nobody complains. There are no complaints. (SP 38) |
| NLT-27: The market works in such a way that doctors in the medical sector are then able to change employers. You can also see that if the fluctuation in the individual departments is high, then you can see that there might also be a need for action in these areas. (CP 2) NLT-28: One employee in December certainly left because she could not handle this workload. (CP 10) NLT-29: There used to be a few of them, but they left. At some point they drew a line under it and said they had to work somewhere else. (SN 17) |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Worringer, B.; Genrich, M.; Müller, A.; Junne, F.; Contributors of the SEEGEN Consortium; Angerer, P. How Do Hospital Medical and Nursing Managers Perceive Work-Related Strain on Their Employees? Int. J. Environ. Res. Public Health 2020, 17, 4660. https://doi.org/10.3390/ijerph17134660
Worringer B, Genrich M, Müller A, Junne F, Contributors of the SEEGEN Consortium, Angerer P. How Do Hospital Medical and Nursing Managers Perceive Work-Related Strain on Their Employees? International Journal of Environmental Research and Public Health. 2020; 17(13):4660. https://doi.org/10.3390/ijerph17134660
Chicago/Turabian StyleWorringer, Britta, Melanie Genrich, Andreas Müller, Florian Junne, Contributors of the SEEGEN Consortium, and Peter Angerer. 2020. "How Do Hospital Medical and Nursing Managers Perceive Work-Related Strain on Their Employees?" International Journal of Environmental Research and Public Health 17, no. 13: 4660. https://doi.org/10.3390/ijerph17134660