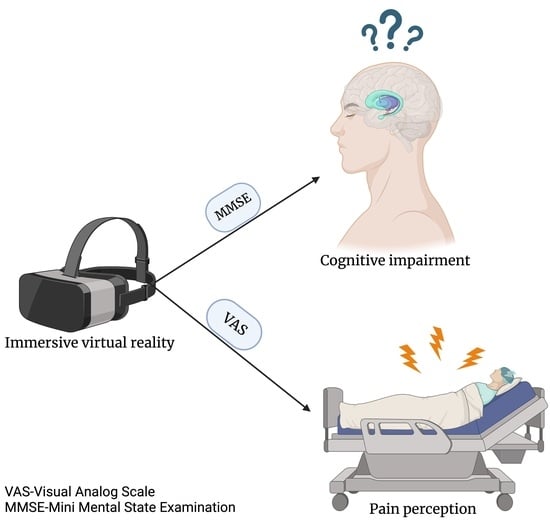
Postoperative Cognitive Impairment and Pain Perception after Abdominal Surgery—Could Immersive Virtual Reality Bring More? A Clinical Approach
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design: Inclusion/Exclusion Criteria
2.2. Statistical Analysis
3. Results
3.1. The Impact of VR on the MMSE and VAS Scores
3.2. Other Risk Factors for POCD
4. Discussion
Study Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Neimark, M.I.; Shmelev, V.V.; Rakhmonov, A.A.; Titova, Z.A. Etiology and Pathogenesis of Postoperative Cognitive Dysfunction (Review). Gen. Reanimatol. 2023, 19, 60–71. [Google Scholar] [CrossRef]
- Cole, D.J.; Kharasch, E.D. Postoperative Brain Function. Anesthesiology 2018, 129, 861–863. [Google Scholar] [CrossRef] [PubMed]
- Daiello, L.A.; Racine, A.M.; Yun Gou, R.; Marcantonio, E.R.; Xie, Z.; Kunze, L.J.; Vlassakov, K.V.; Inouye, S.K.; Jones, R.N. Postoperative Delirium and Postoperative Cognitive Dysfunction. Anesthesiology 2019, 131, 477–491. [Google Scholar] [CrossRef] [PubMed]
- Needham, M.; Webb, C.; Bryden, D. Postoperative cognitive dysfunction and dementia: What we need to know and do. Br. J. Anaesth. 2017, 119, i115–i125. [Google Scholar] [CrossRef] [PubMed]
- Powell, R.; Scott, N.W.; Manyande, A.; Bruce, J.; Vögele, C.; Byrne-Davis, L.M.; Unsworth, M.; Osmer, C.; Johnston, M. Psychological preparation and postoperative outcomes for adults undergoing surgery under general anaesthesia. Cochrane Database Syst. Rev. 2016, 2016, CD008646. [Google Scholar] [CrossRef]
- Valdelievre, T.; Zuo, Z. Do We Have Measures to Reduce Post-operative Cognitive Dysfunction? Front. Neurosci. 2022, 16, 850012. [Google Scholar] [CrossRef]
- Specht, B.J.; Buse, C.R.; Phelps, J.R.; Phillips, M.R.; Chiavacci, S.D.; Harrell, L.E.; Nelson, J.M.; Poulos, K.E.; Li, Q.; Liu, Y.; et al. Virtual Reality after Surgery—A Method to Decrease Pain After Surgery in Pediatric Patients. Am. Surg. 2021, 89, 596–602. [Google Scholar] [CrossRef]
- Peng, L.; Xu, L.; Ouyang, W. Role of Peripheral Inflammatory Markers in Postoperative Cognitive Dysfunction (POCD): A Meta-Analysis. PLoS ONE 2013, 8, e79624. [Google Scholar] [CrossRef]
- Deng, X.; Sun, T.; Zhao, D.; Sana, S.R.G.L.; Li, W. Stellate ganglion block potentially ameliorates postoperative cognitive decline in aged rats by regulating the neuroendocrine response to stress. Heliyon 2023, 9, e14337. [Google Scholar] [CrossRef]
- Fodale, V.; Santamaria, L.B.; Schifilliti, D.; Mandal, P.K. Anaesthetics and postoperative cognitive dysfunction: A pathological mechanism mimicking Alzheimer’s disease: Anaesthetics, postoperative cognitive decline and Alzheimer’s disease. Anaesthesia 2010, 65, 388–395. [Google Scholar] [CrossRef]
- Takamiya, S.; Honma, M.; Masaoka, Y.; Okada, M.; Ohashi, S.; Tanaka, Y.; Suzuki, K.; Uematsu, S.; Kitami, A.; Izumizaki, M. Preoperative state anxiety predicts postoperative health-related quality of life: A prospective observational study on patients undergoing lung cancer surgery. Front. Psychol. 2023, 14, 1161333. [Google Scholar] [CrossRef] [PubMed]
- Huai, X.; Jiao, Y.; Gu, X.; Zhu, H.; Chen, L.; Fan, Y.; Yu, W.; Su, D.; Xie, H. Preoperative Chronic Pain as a Risk Factor for Early Postoperative Cognitive Dysfunction in Elderly Patients Undergoing Hip Joint Replacement Surgery: A Prospective Observational Cohort Study. Front. Neurosci. 2021, 15, 747362. [Google Scholar] [CrossRef] [PubMed]
- Loreto-Quijada, D.; Gutiérrez-Maldonado, J.; Nieto, R.; Gutiérrez-Martínez, O.; Ferrer-García, M.; Saldaña, C.; Fusté-Escolano, A.; Liutsko, L. Differential effects of two virtual reality interventions: Distraction versus pain control. Cyberpsychol. Behav. Soc. Netw. 2014, 17, 353–358. [Google Scholar] [CrossRef] [PubMed]
- Gupta, A.; Scott, K.; Dukewich, M. Innovative Technology Using Virtual Reality in the Treatment of Pain: Does It Reduce Pain via Distraction, or Is There More to It? Pain Med. 2018, 19, 151–159. [Google Scholar] [CrossRef]
- Gold, J.I.; Belmont, K.A.; Thomas, D.A. The Neurobiology of Virtual Reality Pain Attenuation. CyberPsychol. Behav. 2007, 10, 536–544. [Google Scholar] [CrossRef]
- Sun, Y.; Feng, H.; Zou, T.; Hou, M.; Jin, Y.; Gu, C.; Wang, Y.; Li, J.; Liu, M.; Zhang, M.; et al. Assessment of risk factors for postoperative cognitive dysfunction after coronary artery bypass surgery: A single-center retrospective cohort study. Biosci. Rep. 2021, 41, BSR20190719. [Google Scholar] [CrossRef]
- Ingustu, D.G.; Pavel, B.; Paltineanu, S.I.; Mihai, D.I.; Cotorogea-Simion, M.; Martac, C.; Florescu, M.M.; Cobilinschi, C.; Isac, S.; Droc, G. The Management of Postoperative Cognitive Dysfunction in Cirrhotic Patients: An Overview of the Literature. Medicina 2023, 59, 465. [Google Scholar] [CrossRef]
- Jipa, M.; Isac, S.; Klimko, A.; Simion-Cotorogea, M.; Martac, C.; Cobilinschi, C.; Droc, G. Opioid-Sparing Analgesia Impacts the Perioperative Anesthetic Management in Major Abdominal Surgery. Medicina 2022, 58, 487. [Google Scholar] [CrossRef]
- Gerber, S.M.; Jeitziner, M.M.; Knobel, S.E.J.; Mosimann, U.P.; Müri, R.M.; Jakob, S.M.; Nef, T. Perception and Performance on a Virtual Reality Cognitive Stimulation for Use in the Intensive Care Unit: A Non-randomized Trial in Critically Ill Patients. Front. Med. 2019, 6, 287. [Google Scholar] [CrossRef]
- Ding, L.; Hua, H.; Zhu, H.; Zhu, S.; Lu, J.; Zhao, K.; Xu, Q. Effects of virtual reality on relieving postoperative pain in surgical patients: A systematic review and meta-analysis. Int. J. Surg. 2020, 82, 87–94. [Google Scholar] [CrossRef]
- Payne, O.; Smith, V.; Rolnik, D.L.; Davies-Tuck, M.; Warty, R.; Seo, D.; Wetherell, L.; Murday, H.K.; Nair, A.; Kaur, R.; et al. Virtual reality and its use in post-operative pain following laparoscopy: A feasibility study. Sci. Rep. 2022, 12, 13137. [Google Scholar] [CrossRef] [PubMed]
- Olbrecht, V.A.; O’Conor, K.T.; Williams, S.E.; Boehmer, C.O.; Marchant, G.W.; Glynn, S.M.; Geisler, K.J.; Ding, L.; Yang, G.; King, C.D. Guided Relaxation-Based Virtual Reality for Acute Postoperative Pain and Anxiety in a Pediatric Population: Pilot Observational Study. J. Med. Internet Res. 2021, 23, e26328. [Google Scholar] [CrossRef] [PubMed]
- García-Sánchez, M.; García-Robles, P.; Osuna-Pérez, M.C.; Lomas-Vega, R.; Obrero-Gaitán, E.; Cortés-Pérez, I. Effectiveness of Virtual Reality-Based Early Postoperative Rehabilitation after Total Knee Arthroplasty: A Systematic Review with Meta-Analysis of Randomized Controlled Trials. Appl. Sci. 2023, 13, 4597. [Google Scholar] [CrossRef]
- Mahrer, N.E.; Gold, J.I. The use of virtual reality for pain control: A review. Curr. Pain Headache Rep. 2009, 13, 100–109. [Google Scholar] [CrossRef]
- Parsons, T.D.; Rizzo, A.A. Affective outcomes of virtual reality exposure therapy for anxiety and specific phobias: A meta-analysis. J. Behav. Ther. Exp. Psychiatry 2008, 39, 250–261. [Google Scholar] [CrossRef]
- Gershon, J.; Zimand, E.; Lemos, R.; Rothbaum, B.O.; Hodges, L. Use of virtual reality as a distractor for painful procedures in a patient with pediatric cancer: A case study. Cyberpsychol. Behav. Impact Internet Multimed. Virtual Real. Behav. Soc. 2003, 6, 657–661. [Google Scholar] [CrossRef]
- Zhu, B.; Zhou, Y.; Weng, Q.; Luo, W.; He, X.; Jin, L.; Wang, Q.; Gao, B.; Harb, A.K.A.; Wang, J. Effects of biophilic virtual reality on cognitive function of patients undergoing laparoscopic surgery: Study protocol for a sham randomised controlled trial. BMJ Open 2022, 12, e052769. [Google Scholar] [CrossRef]
- Thapa, N.; Park, H.J.; Yang, J.G.; Son, H.; Jang, M.; Lee, J.; Kang, S.W.; Park, K.W.; Park, H. The Effect of a Virtual Reality-Based Intervention Program on Cognition in Older Adults with Mild Cognitive Impairment: A Randomized Control Trial. J. Clin. Med. 2020, 9, 1283. [Google Scholar] [CrossRef]
- Zhang, Q.; Fu, Y.; Lu, Y.; Zhang, Y.; Huang, Q.; Yang, Y.; Zhang, K.; Li, M. Impact of Virtual Reality-Based Therapies on Cognition and Mental Health of Stroke Patients: Systematic Review and Meta-analysis. J. Med. Internet Res. 2021, 23, e31007. [Google Scholar] [CrossRef]
- Yang, S.; Chun, M.; Son, Y. Effect of Virtual Reality on Cognitive Dysfunction in Patients with Brain Tumor. Ann. Rehabil. Med. 2014, 38, 726–733. [Google Scholar] [CrossRef]
- Pezzi, L.; di Matteo, A.; Insabella, R.; Mastrogiacomo, S.; Baldari, C.; MacHado Reiss, V.; Paolucci, T. How Cognitive Reserve should Influence Rehabilitation Choices using Virtual Reality in Parkinson’s Disease. Park. Dis. 2022, 2022, 7389658. [Google Scholar] [CrossRef]
- Jin, R.; Pilozzi, A.; Huang, X. Current Cognition Tests, Potential Virtual Reality Applications, and Serious Games in Cognitive Assessment and Non-Pharmacological Therapy for Neurocognitive Disorders. J. Clin. Med. 2020, 9, 3287. [Google Scholar] [CrossRef] [PubMed]
- Lanitis, S.; Mimigianni, C.; Raptis, D.; Sourtse, G.; Sgourakis, G.; Karaliotas, C. The Impact of Educational Status on the Postoperative Perception of Pain. Korean J. Pain 2015, 28, 265–274. [Google Scholar] [CrossRef] [PubMed]
- Feinkohl, I.; Winterer, G.; Spies, C.D.; Pischon, T. Cognitive Reserve and the Risk of Postoperative Cognitive Dysfunction. Dtsch. Ärztebl. Int. 2017, 114, 110–117. [Google Scholar] [PubMed]
- Richard, H.M.; Cerza, S.P.; De La Rocha, A.; Podeszwa, D.A. Preoperative mental health status is a significant predictor of postoperative outcomes in adolescents treated with hip preservation surgery. J. Child. Orthop. 2020, 14, 259–265. [Google Scholar] [CrossRef] [PubMed]



Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Droc, G.; Isac, S.; Nita, E.; Martac, C.; Jipa, M.; Mihai, D.I.; Cobilinschi, C.; Badea, A.-G.; Ojog, D.; Pavel, B.; et al. Postoperative Cognitive Impairment and Pain Perception after Abdominal Surgery—Could Immersive Virtual Reality Bring More? A Clinical Approach. Medicina 2023, 59, 2034. https://doi.org/10.3390/medicina59112034
Droc G, Isac S, Nita E, Martac C, Jipa M, Mihai DI, Cobilinschi C, Badea A-G, Ojog D, Pavel B, et al. Postoperative Cognitive Impairment and Pain Perception after Abdominal Surgery—Could Immersive Virtual Reality Bring More? A Clinical Approach. Medicina. 2023; 59(11):2034. https://doi.org/10.3390/medicina59112034
Chicago/Turabian StyleDroc, Gabriela, Sebastian Isac, Elisabeta Nita, Cristina Martac, Miruna Jipa, Diana Irene Mihai, Cristian Cobilinschi, Andrada-Georgiana Badea, Damiana Ojog, Bogdan Pavel, and et al. 2023. "Postoperative Cognitive Impairment and Pain Perception after Abdominal Surgery—Could Immersive Virtual Reality Bring More? A Clinical Approach" Medicina 59, no. 11: 2034. https://doi.org/10.3390/medicina59112034