Mid-Term Outcomes after Arthroscopic “Tear Completion Repair” of Partial Thickness Rotator Cuff Tears
Abstract
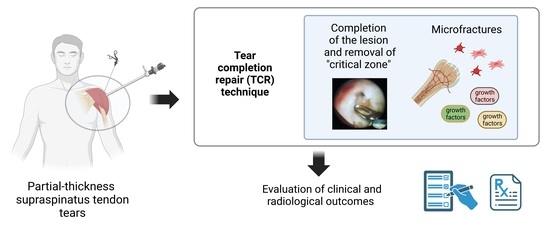
:1. Introduction
2. Materials and Methods
2.1. Study Population
2.2. Surgical Technique
2.3. Pre- and Postoperative Management
2.4. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Ellman, H. Diagnosis and treatment of incomplete rotator cuff tears. Clin. Orthop. Relat. Res. 1990, 254, 64–74. [Google Scholar] [CrossRef]
- Strauss, E.J.; Salata, M.J.; Kercher, J.; Barker, J.U.; McGill, K., Jr.; Bach, B.R.; Romeo, A.A.; Verma, N.N. The arthroscopic management of partial-thickness rotator cuff tears: A systematic review of the literature. Arthroscopy 2011, 27, 568–580. [Google Scholar] [CrossRef] [PubMed]
- Sher, J.S.; Uribe, J.W.; Posada, A.; Murphy, B.J.; Zlatkin, M.B. Abnormal findings on magnetic resonance images of asymptomatic shoulders. J. Bone Jt. Surg. Am. 1995, 77, 10–15. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Matava, M.J.; Purcell, D.B.; Rudzki, J.R. Partial-thickness rotator cuff tears. Am. J. Sports Med. 2005, 33, 1405–1417. [Google Scholar] [CrossRef] [PubMed]
- Cigolotti, A.; Biz, C.; Lerjefors, E.; de Iudicibus, G.; Belluzzi, E.; Ruggieri, P. Medium- to long-term clinical and functional outcomes of isolated and combined subscapularis tears repaired arthroscopically. Arch. Med. Sci. 2020, 16. [Google Scholar] [CrossRef]
- Connor, P.M.; Banks, D.M.; Tyson, A.B.; Coumas, J.S.; D’Alessandro, D.F. Magnetic resonance imaging of the asymptomatic shoulder of overhead athletes: A 5-year follow-up study. Am. J. Sports Med. 2003, 31, 724–727. [Google Scholar] [CrossRef]
- Fukuda, H. Partial-thickness rotator cuff tears: A modern view on Codman’s classic. J. Shoulder Elb. Surg. 2000, 9, 163–168. [Google Scholar] [CrossRef]
- Sano, H.; Ishii, H.; Trudel, G.; Uhthoff, H.K. Histologic evidence of degeneration at the insertion of 3 rotator cuff tendons: A comparative study with human cadaveric shoulders. J. Shoulder Elb. Surg. 1999, 8, 574–579. [Google Scholar] [CrossRef]
- Milgrom, C.; Schaffler, M.; Gilbert, S.; van Holsbeeck, M. Rotator-cuff changes in asymptomatic adults. The effect of age, hand dominance and gender. J. Bone Jt. Surg. Br. 1995, 77, 296–298. [Google Scholar] [CrossRef] [Green Version]
- Factor, D.; Dale, B. Current concepts of rotator cuff tendinopathy. Int. J. Sports Phys. 2014, 9, 274–288. [Google Scholar]
- Chambler, A.F.; Pitsillides, A.A.; Emery, R.J. Acromial spur formation in patients with rotator cuff tears. J. Shoulder Elb. Surg. 2003, 12, 314–321. [Google Scholar] [CrossRef]
- Levigne, C.; Garret, J.; Grosclaude, S.; Borel, F.; Walch, G. Surgical technique arthroscopic posterior glenoidplasty for posterosuperior glenoid impingement in throwing athletes. Clin. Orthop. Relat. Res. 2012, 470, 1571–1578. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zabrzyński, J.; Huri, G.; Gryckiewicz, S.; Çetik, R.M.; Szwedowski, D.; Łapaj, Ł.; Gagat, M.; Paczesny, Ł. Biceps Tenodesis versus Tenotomy with Fast Rehabilitation Protocol-A Functional Perspective in Chronic Tendinopathy. J. Clin. Med. 2020, 9, 3938. [Google Scholar] [CrossRef]
- Varacallo, M.; Seaman, T.J.; Mair, S.D. Biceps Tendon Dislocation and Instability. In StatPearls; StatPearls Publishing LLC.: Treasure Island, FL, USA, 2020. [Google Scholar]
- Lazarides, A.L.; Alentorn-Geli, E.; Choi, J.H.; Stuart, J.J.; Lo, I.K.; Garrigues, G.E.; Taylor, D.C. Rotator cuff tears in young patients: A different disease than rotator cuff tears in elderly patients. J. Shoulder Elb. Surg. 2015, 24, 1834–1843. [Google Scholar] [CrossRef] [PubMed]
- Fukuda, H. The management of partial-thickness tears of the rotator cuff. J. Bone Jt. Surg. Br. 2003, 85, 3–11. [Google Scholar] [CrossRef] [PubMed]
- Seitz, A.L.; McClure, P.W.; Finucane, S.; Boardman, N.D., III; Michener, L.A. Mechanisms of rotator cuff tendinopathy: Intrinsic, extrinsic, or both? Clin. Biomech. 2011, 26, 1–12. [Google Scholar] [CrossRef]
- Ogawa, K.; Yoshida, A.; Inokuchi, W.; Naniwa, T. Acromial spur: Relationship to aging and morphologic changes in the rotator cuff. J. Shoulder Elb. Surg. 2005, 14, 591–598. [Google Scholar] [CrossRef]
- Clavert, P.; Le Coniat, Y.; Kempf, J.F.; Walch, G. Intratendinous rupture of the supraspinatus: Anatomical and functional results of 24 operative cases. Eur. J. Orthop. Surg. Traumatol. 2016, 26, 133–138. [Google Scholar] [CrossRef]
- Lee, S.B.; Nakajima, T.; Luo, Z.P.; Zobitz, M.E.; Chang, Y.W.; An, K.N. The bursal and articular sides of the supraspinatus tendon have a different compressive stiffness. Clin. Biomech. 2000, 15, 241–247. [Google Scholar] [CrossRef]
- Yamanaka, K.; Matsumoto, T. The joint side tear of the rotator cuff. A followup study by arthrography. Clin. Orthop. Relat. Res. 1994, 68–73. [Google Scholar]
- Lo, I.K.; Denkers, M.R.; More, K.D.; Nelson, A.A.; Thornton, G.M.; Boorman, R.S. Partial-thickness rotator cuff tears: Clinical and imaging outcomes and prognostic factors of successful nonoperative treatment. Open Access J. Sports Med. 2018, 9, 191–197. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Oliva, F.; Piccirilli, E.; Bossa, M.; Via, A.G.; Colombo, A.; Chillemi, C.; Gasparre, G.; Pellicciari, L.; Franceschetti, E.; Rugiero, C.; et al. IS Mu. LT—Rotator Cuff Tears Guidelines. Muscles Ligaments Tendons J. 2015, 5, 227–263. [Google Scholar] [CrossRef] [PubMed]
- Biz, C.; Vinanti, G.B.; Rossato, A.; Arnaldi, E.; Aldegheri, R. Prospective study of three surgical procedures for long head biceps tendinopathy associated with rotator cuff tears. Muscles Ligaments Tendons J. 2012, 2, 133–136. [Google Scholar] [PubMed]
- Liem, D.; Alci, S.; Dedy, N.; Steinbeck, J.; Marquardt, B.; Mollenhoff, G. Clinical and structural results of partial supraspinatus tears treated by subacromial decompression without repair. Knee Surg. Sports Traumatol. Arthrosc. 2008, 16, 967–972. [Google Scholar] [CrossRef]
- Park, J.Y.; Yoo, M.J.; Kim, M.H. Comparison of surgical outcome between bursal and articular partial thickness rotator cuff tears. Orthopedics 2003, 26, 387–390. [Google Scholar] [CrossRef]
- Kim, Y.S.; Lee, H.J.; Bae, S.H.; Jin, H.; Song, H.S. Outcome Comparison Between in Situ Repair Versus Tear Completion Repair for Partial Thickness Rotator Cuff Tears. Arthroscopy 2015, 31, 2191–2198. [Google Scholar] [CrossRef]
- Rossi, L.A.; Atala, N.A.; Bertona, A.; Bongiovanni, S.; Tanoira, I.; Maignon, G.; Ranalletta, M. Long-Term Outcomes After In Situ Arthroscopic Repair of Partial Rotator Cuff Tears. Arthroscopy 2019, 35, 698–702. [Google Scholar] [CrossRef]
- Vap, A.R.; Mannava, S.; Katthagen, J.C.; Horan, M.P.; Fritz, E.M.; Pogorzelski, J.; Millett, P.J. Five-Year Outcomes After Arthroscopic Repair of Partial-Thickness Supraspinatus Tears. Arthroscopy 2018, 34, 75–81. [Google Scholar] [CrossRef]
- Codman, E.A. The Shoulder: Rupture of the Supraspinatus Tendon and Other Lesions in or About the Subacromial Bursa; Thomas Todd Copany, Printers: Boston, MA, USA, 1934. [Google Scholar]
- Snyder, S.J.; Burns, J. Rotator cuff healing and the bone marrow “crimson duvet” from clinical observations to science. Tech. Shoulder Elb. Surg. 2009, 10, 130–137. [Google Scholar] [CrossRef]
- Baumgarten, K.M.; Chang, P.S.; Foley, E.K. Patient-determined outcomes after arthroscopic rotator cuff repair with and without biceps tenodesis utilizing the PITT technique. J. Shoulder Elb. Surg. 2019, 28, 1049–1055. [Google Scholar] [CrossRef]
- Sekiya, J.K.; Elkousy, H.A.; Rodosky, M.W. Arthroscopic biceps tenodesis using the percutaneous intra-articular transtendon technique. Arthroscopy 2003, 19, 1137–1141. [Google Scholar] [CrossRef] [PubMed]
- Neer, C.S., II. Anterior acromioplasty for the chronic impingement syndrome in the shoulder: A preliminary report. J. Bone Jt. Surg. Am. 1972, 54, 41–50. [Google Scholar] [CrossRef]
- Aguado, G.; Obando, D.V.; Herrera, G.A.; Ramirez, A.; Llinas, P.J. Retears of the Rotator Cuff: An Ultrasonographic Assessment During the First Postoperative Year. Orthop. J. Sports Med. 2019, 7, 2325967119889049. [Google Scholar] [CrossRef] [PubMed]
- Kamath, G.; Galatz, L.M.; Keener, J.D.; Teefey, S.; Middleton, W.; Yamaguchi, K. Tendon integrity and functional outcome after arthroscopic repair of high-grade partial-thickness supraspinatus tears. J. Bone Jt. Surg. Am. 2009, 91, 1055–1062. [Google Scholar] [CrossRef]
- Franceschi, F.; Papalia, R.; Del Buono, A.; Vasta, S.; Costa, V.; Maffulli, N.; Denaro, V. Articular-sided rotator cuff tears: Which is the best repair? A three-year prospective randomised controlled trial. Int. Orthop. 2013, 37, 1487–1493. [Google Scholar] [CrossRef] [Green Version]
- Kim, K.C.; Shin, H.D.; Cha, S.M.; Park, J.Y. Repair integrity and functional outcome after arthroscopic conversion to a full-thickness rotator cuff tear: Articular- versus bursal-side partial tears. Am. J. Sports Med. 2014, 42, 451–456. [Google Scholar] [CrossRef]
- Jordan, R.W.; Bentick, K.; Saithna, A. Transtendinous repair of partial articular sided supraspinatus tears is associated with higher rates of stiffness and significantly inferior early functional scores than tear completion and repair: A systematic review. Orthop. Traumatol. Surg. Res. 2018, 104, 829–837. [Google Scholar] [CrossRef]
- Cordasco, F.A.; Backer, M.; Craig, E.V.; Klein, D.; Warren, R.F. The partial-thickness rotator cuff tear: Is acromioplasty without repair sufficient? Am. J. Sports Med. 2002, 30, 257–260. [Google Scholar] [CrossRef]
- Weber, S.C. Arthroscopic debridement and acromioplasty versus mini-open repair in the treatment of significant partial-thickness rotator cuff tears. Arthroscopy 1999, 15, 126–131. [Google Scholar] [CrossRef]
- Chung, S.W.; Kim, J.Y.; Yoon, J.P.; Lyu, S.H.; Rhee, S.M.; Oh, S.B. Arthroscopic repair of partial-thickness and small full-thickness rotator cuff tears: Tendon quality as a prognostic factor for repair integrity. Am. J. Sports Med. 2015, 43, 588–596. [Google Scholar] [CrossRef]
- Budoff, J.E.; Rodin, D.; Ochiai, D.; Nirschl, R.P. Arthroscopic rotator cuff debridement without decompression for the treatment of tendinosis. Arthroscopy 2005, 21, 1081–1089. [Google Scholar] [CrossRef] [PubMed]
- Kartus, J.; Kartus, C.; Rostgard-Christensen, L.; Sernert, N.; Read, J.; Perko, M. Long-term clinical and ultrasound evaluation after arthroscopic acromioplasty in patients with partial rotator cuff tears. Arthroscopy 2006, 22, 44–49. [Google Scholar] [CrossRef] [PubMed]
- Nathani, A.; Smith, K.; Wang, T. Partial and Full-Thickness RCT: Modern Repair Techniques. Curr. Rev. Musculoskelet. Med. 2018, 11, 113–121. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sharma, P.; Maffulli, N. Biology of tendon injury: Healing, modeling and remodeling. J. Musculoskelet. Neuronal Interact. 2006, 6, 181–190. [Google Scholar]
- Bonutti, P.M.; Hawkins, R.J. Rotator cuff disorders. Bailliere Clin. Rheumatol. 1989, 3, 535–550. [Google Scholar] [CrossRef]
- Jensen, P.T.; Lambertsen, K.L.; Frich, L.H. Assembly, maturation, and degradation of the supraspinatus enthesis. J. Shoulder Elb. Surg. 2018, 27, 739–750. [Google Scholar] [CrossRef] [Green Version]
- Ju, Y.J.; Muneta, T.; Yoshimura, H.; Koga, H.; Sekiya, I. Synovial mesenchymal stem cells accelerate early remodeling of tendon-bone healing. Cell Tissue Res. 2008, 332, 469–478. [Google Scholar] [CrossRef]
- Karthikeyan, S.; Griffin, D.R.; Parsons, N.; Lawrence, T.M.; Modi, C.S.; Drew, S.J.; Smith, C.D. Microvascular blood flow in normal and pathologic rotator cuffs. J. Shoulder Elb. Surg. 2015, 24, 1954–1960. [Google Scholar] [CrossRef]
- Hegedus, E.J.; Cook, C.; Brennan, M.; Wyland, D.; Garrison, J.C.; Driesner, D. Vascularity and tendon pathology in the rotator cuff: A review of literature and implications for rehabilitation and surgery. Br. J. Sports Med. 2010, 44, 838–847. [Google Scholar] [CrossRef]
- Brooks, C.H.; Revell, W.J.; Heatley, F.W. A quantitative histological study of the vascularity of the rotator cuff tendon. J. Bone Jt. Surg. Br. 1992, 74, 151–153. [Google Scholar] [CrossRef]
- Lin, T.W.; Cardenas, L.; Soslowsky, L.J. Biomechanics of tendon injury and repair. J. Biomech. 2004, 37, 865–877. [Google Scholar] [CrossRef] [PubMed]
- Rudzki, J.R.; Adler, R.S.; Warren, R.F.; Kadrmas, W.R.; Verma, N.; Pearle, A.D.; Lyman, S.; Fealy, S. Contrast-enhanced ultrasound characterization of the vascularity of the rotator cuff tendon: Age- and activity-related changes in the intact asymptomatic rotator cuff. J. Shoulder Elb. Surg. 2008, 17, S96–S100. [Google Scholar] [CrossRef] [PubMed]
- Biberthaler, P.; Wiedemann, E.; Nerlich, A.; Kettler, M.; Mussack, T.; Deckelmann, S.; Mutschler, W. Microcirculation associated with degenerative rotator cuff lesions. In vivo assessment with orthogonal polarization spectral imaging during arthroscopy of the shoulder. J. Bone Jt. Surg. Am. 2003, 85, 475–480. [Google Scholar] [CrossRef]
- Fukuda, H.; Hamada, K.; Yamanaka, K. Pathology and pathogenesis of bursal-side rotator cuff tears viewed from en bloc histologic sections. Clin. Orthop. Relat. Res. 1990, 75–80. [Google Scholar] [CrossRef]
- Goodmurphy, C.W.; Osborn, J.; Akesson, E.J.; Johnson, S.; Stanescu, V.; Regan, W.D. An immunocytochemical analysis of torn rotator cuff tendon taken at the time of repair. J. Shoulder Elb. Surg. 2003, 12, 368–374. [Google Scholar] [CrossRef]
- Matthews, T.J.; Hand, G.C.; Rees, J.L.; Athanasou, N.A.; Carr, A.J. Pathology of the torn rotator cuff tendon. Reduction in potential for repair as tear size increases. J. Bone Jt. Surg. Br. 2006, 88, 489–495. [Google Scholar] [CrossRef] [PubMed]
- Kim, K.C.; Lee, W.-Y.; Shin, H.D.; Joo, Y.-B.; Han, S.-C.; Chung, H.-J. Repair integrity and functional outcomes of arthroscopic repair for intratendinous partial-thickness rotator cuff tears. J. Orthop. Surg. 2019, 27, 2309499019847227. [Google Scholar] [CrossRef] [Green Version]
- Randelli, P.; Margheritini, F.; Cabitza, P.; Dogliotti, G.; Corsi, M.M. Release of growth factors after arthroscopic acromioplasty. Knee Surg. Sports Traumatol. Arthrosc. 2009, 17, 98–101. [Google Scholar] [CrossRef]
- Galliera, E.; Randelli, P.; Dogliotti, G.; Dozio, E.; Colombini, A.; Lombardi, G.; Cabitza, P.; Corsi, M.M. Matrix metalloproteases MMP-2 and MMP-9: Are they early biomarkers of bone remodelling and healing after arthroscopic acromioplasty? Injury 2010, 41, 1204–1207. [Google Scholar] [CrossRef]
- Lorbach, O.; Baums, M.H.; Kostuj, T.; Pauly, S.; Scheibel, M.; Carr, A.; Zargar, N.; Saccomanno, M.F.; Milano, G. Advances in biology and mechanics of rotator cuff repair. Knee Surg. Sports Traumatol. Arthrosc. 2015, 23, 530–541. [Google Scholar] [CrossRef]
- Bilsel, K.; Yildiz, F.; Kapicioglu, M.; Uzer, G.; Elmadag, M.; Pulatkan, A.; Esrefoglu, M.; Bozdag, E.; Milano, G. Efficacy of bone marrow-stimulating technique in rotator cuff repair. J. Shoulder Elb. Surg. 2017, 26, 1360–1366. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zabrzyński, J.; Łapaj, Ł.; Paczesny, Ł.; Zabrzyńska, A.; Grzanka, D. Tendon—function-related structure, simple healing process and mysterious ageing. Folia Morphol. 2018, 77, 416–427. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Milano, G.; Saccomanno, M.F.; Careri, S.; Taccardo, G.; De Vitis, R.; Fabbriciani, C. Efficacy of marrow-stimulating technique in arthroscopic rotator cuff repair: A prospective randomized study. Arthroscopy 2013, 29, 802–810. [Google Scholar] [CrossRef] [PubMed]






| Variable | Value (n = 87) |
|---|---|
| Age (years) | 56.0 ± 9.5; 57.0 [18.0–73.0] |
| Sex, number (%) | |
| Female Male | 44 (50.6%) 43 (49.4%) |
| BMI | 25.0 ± 2.9; 24.9 [18.7–33.3] |
| Time (months) to surgery | 5.1 ± 1.6; 5.0 [2.0–11.0] |
| Follow-up (years) | 4.7 ± 1.4; 5.0 [2.0–7.1] |
| Side of involvement | |
| D, number (%): ND, number (%) | 53 (60.9%): 34 (39.1) |
| Traumatic onset, number (%) | 26 (29.9%) |
| Corticosteroid injections | 20 (23.0%) |
| Tear location (Ellman classification) number (%) | |
| articular bursal intratendinous | 61 (70.1%) 17 (19.6%) 9 (10.3%) |
| Comorbidities, number (%) | |
| Diabetes Hypertension Dyslipidemia Osteoporosis | 5 (5.7%) 19 (21.8%) 23 (26.3%) 5 (5.7%) |
| Smoking, number (%) | 13 (14.9%) |
| Capsulitis, number (%) | 7 (8%) |
| Return to work, days | 110.85 ± 70.25; 90 [30–365] |
| Satisfaction | 9.26 ± 1.28; 10 [4–10] |
| Preoperative | Postoperative (Last Follow-Up) | p Value | |
|---|---|---|---|
| VAS pain (mean ± SD; median [min-max]) | 8.6 ± 1.6; 9.0 [3.0–10.0] | 0.9 ± 1.3; 0 [0–5.0] | <0.0001 |
| Constant score (mean ± SD; median [min-max]) | 53.5 ± 9.0; 53.5 [23.0–68.5] | 91.3 ± 11.0; 94.0 [37.5–100.0] | <0.0001 |
| Pain (mean ± SD; median [min-max]) | 2.5 ± 1.9; 2.0 [0–7.5] | 12.7 ± 2.9; 15.0 [4.0–15.0] | <0.0001 |
| Activity level (mean ± SD; median [min-max]) | 8.6 ± 2.9; 8.0 [0–17.0] | 18.7 ± 2.9; 20.0 [8.0–20.0] | <0.0001 |
| ROM (mean ± SD; median [min-max]) | 32.6 ± 4.5; 32.0 [16.0–40.0] | 38.0 ± 3.9; 40.0 [14.0–40.0] | <0.0001 |
| Strength (mean ± SD; median [min-max]) | 9.7 ± 3.1; 10.0 [4.0–18.0] | 21.7 ± 4.2; 23.0 [8.0–25.0] | <0.0001 |
| Articular (n = 61) | Bursal (n = 17) | Intratendinous (n = 9) | p-Value | |
|---|---|---|---|---|
| Age (years) (mean ± SD; median [min-max]) | 56.2 ± 10.3; 59 [18.0–73.0] | 56.6 ± 7.6; 56.0 [45.0–72.0] | 53.4 ± 7.9; 53.0 [40.0–67.0] | n.s |
| Sex, number (%) | 0.038 | |||
| Females Males | 34 (55.7) 27 (44.3) | 4 (56.4) 13 (76.5) | 6 (66.7) 3 (33.3) | |
| Traumatic onset, number (%) | n.s | |||
| Yes No | 12 (70.6) 5 (29.4) | 41 (67.2) 20 (32.8) | 8 (88.9) 1 (11.1) | |
| BMI (mean ± SD; median) [min-max]) | 25.1 ± 3.1; 24.9 [18.7–33.3] | 24.8 ± 2.2; 24.6 [21.5–28.4] | 24.9 ± 2.8; 24.7 [20.8–29.5] | n.s |
| Return to work | n.s | |||
| (mean ± SD; median) [min-max] | 115.3 ± 74.3; 90.0 [30.0–365.0] | 98.8 ± 71.2; 80.0 [40.0–365.0] | 103.3 ± 30.8; 90.0 [60.0–150.0] | |
| Satisfaction | n.s | |||
| (mean ± SD; median) [min-max] | 9.1 ± 1.4; 10.0 [4.0–10.0] | 9.5 ± 0.9; 10.0 [7.0–10.0] | 9.7 ± 0.5; 10.0 [9.0–10.0] | |
| Constant score pre- | n.s | |||
| (mean ± SD; median) [min-max] | 53.4 ± 8.9; 53.0 [28.0–68.0] | 56.2 ± 5.8; 58.0 [40.5–65.0] | 49.0 ± 13.4; 52.5 [23.0–68.5] | |
| Constant score post- | n.s | |||
| (mean ± SD; median) [min-max] | 90.7 ± 12.4; 94.0 [37.5–100.0] | 95.0 ± 4.5; 95.0 [83.0–100.0] | 88.6 ± 7.7; 92.0 [75.0–100.0] | |
| VAS pain pre- | n.s | |||
| (mean ± SD; median) [min-max] | 8.7 ± 1.5; 9.0 [4.0–10.0] | 7.9 ± 1.5; 8.0 [5.0–10.0] | 8.9 ± 2.3; 10.0 [3.0–10.0] | |
| VAS pain post- | n.s | |||
| (mean ± SD; median) [min-max] | 1.0 ± 1.2; 0 [0–5.0] | 0.8 ± 1.5; 0 [0–5.0] | 1.3 ± 1.4; 1.0 [0–3.0] |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Fama, G.; Tagliapietra, J.; Belluzzi, E.; Pozzuoli, A.; Biz, C.; Ruggieri, P. Mid-Term Outcomes after Arthroscopic “Tear Completion Repair” of Partial Thickness Rotator Cuff Tears. Medicina 2021, 57, 74. https://doi.org/10.3390/medicina57010074
Fama G, Tagliapietra J, Belluzzi E, Pozzuoli A, Biz C, Ruggieri P. Mid-Term Outcomes after Arthroscopic “Tear Completion Repair” of Partial Thickness Rotator Cuff Tears. Medicina. 2021; 57(1):74. https://doi.org/10.3390/medicina57010074
Chicago/Turabian StyleFama, Giuseppe, Jacopo Tagliapietra, Elisa Belluzzi, Assunta Pozzuoli, Carlo Biz, and Pietro Ruggieri. 2021. "Mid-Term Outcomes after Arthroscopic “Tear Completion Repair” of Partial Thickness Rotator Cuff Tears" Medicina 57, no. 1: 74. https://doi.org/10.3390/medicina57010074