High Prevalence of Antimicrobial Resistance Among Gram-Negative Isolated Bacilli in Intensive Care Units at a Tertiary-Care Hospital in Yucatán Mexico
Abstract
:1. Introduction
2. Materials and Methods
2.1. Site and Period of Study
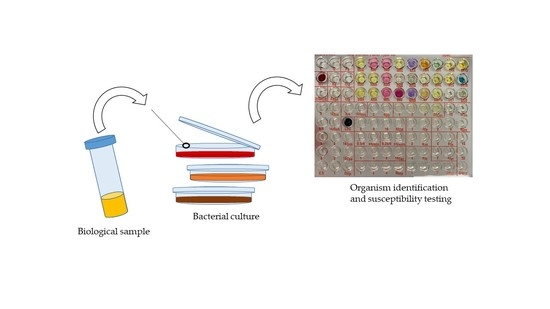
2.2. Microbiology
2.2.1. Culture and Identification
2.2.2. Test Drugs
2.2.3. Antimicrobial Susceptibility Testing
2.2.4. Detection of Extended-Spectrum Beta-Lactamases (ESBL)
2.3. Statistical Analysis
3. Results
3.1. Bacterial Isolates
3.2. AMR of the Clinical Isolates
3.3. MDR, HRMO Profiles, and ESBL-Producing
4. Discussion
4.1. Bacterial Isolates
4.2. AMR of the Clinical Isolates
4.3. MDR, HRMO Profiles, and ESBL-Producing
4.4. Study Limitations
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- World Health Organization. WHO Antimicrobial Resistance; WHO: Geneva, Switzerland, 2018; Available online: http://www.who.int/en/news-room/fact-heets/detail/antimicrobial-resistance (accessed on 12 July 2019).
- Ventola, C.L. The antibiotic resistance crisis Part 1: Causes and threats. Pharm. Ther. 2015, 40, 277–283. [Google Scholar]
- Blair, J.M.; Webber, M.A.; Baylay, A.J.; Ogbolu, D.O.; Piddock, L.J. Molecular mechanisms of antibiotic resistance. Nat. Rev. Microbiol. 2015, 13, 42–51. [Google Scholar] [CrossRef] [PubMed]
- Fair, R.J.; Tor, Y. Antibiotics and bacterial resistance in the 21st century. Perspect. Med. Chem. 2014, 28, 25–64. [Google Scholar] [CrossRef] [PubMed]
- De Kraker, M.E.A.; Stewardson, A.J.; Harbarth, S. Will 10 million people die a year due to antimicrobial resistance by 2050? PLoS Med. 2016, 13, e1002184. [Google Scholar] [CrossRef] [PubMed]
- Anderson, D.J.; Jenkins, T.C.; Evans, S.R.; Harris, A.D.; Weinstein, R.A.; Tamma, P.D.; Han, J.H.; Banerjee, R.; Patel, R.; Zaoutis, T.; et al. The role of stewardship in addressing antibacterial resistance: Stewardship and infection control committee of the antibacterial resistance leadership Group. Clin. Infect. Dis. 2017, 64, S36–S40. [Google Scholar] [CrossRef] [PubMed]
- Magiorakos, A.P.; Srinivasan, A.; Carey, R.B.; Carmeli, Y.; Falagas, M.E.; Giske, C.G.; Harbarth, S.; Hindler, J.F.; Kahlmeter, G.; Olsson-Liljequist, B.; et al. Multidrug-resistant, extensively drug-resistant and pandrug-resistant bacteria: An international expert proposal for interim standard definitions for acquired resistance. Clin. Microbiol. Infect. 2012, 18, 268–281. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. WHO Global Priority List of Antibiotic-Resistant Bacteria to Guide Research, Discovery, and Development of New Antibiotics; WHO: Geneva, Switzerland, 2017; Available online: https://www.who.int/medicines/publications/WHO-PPL-Short_Summary_25Feb-ET_NM_WHO.pdf (accessed on 12 July 2019).
- Santajit, S.; Indrawattana, N. Mechanisms of antimicrobial resistance in ESKAPE pathogens. Biomed. Res. Int. 2016, 2016, 1–8. [Google Scholar] [CrossRef]
- Parajuli, N.P.; Acharya, S.P.; Mishra, S.K.; Parajuli, K.; Rijal, B.P.; Pokhrel, B.M. High burden of antimicrobial resistance among Gram negative bacteria causing healthcare associated infections in a critical care unit of Nepal. Antimicrob. Resist. Infect. Control. 2017, 6, 1–9. [Google Scholar] [CrossRef]
- Moolchandani, K.; Sastry, A.S.; Deepashree, R.; Sistla, S.; Harish, B.N.; Mandal, J. Antimicrobial resistance surveillance among intensive care units of a tertiary care hospital in South India. J. Clin. Diagn. Res. 2017, 11, DC01–DC07. [Google Scholar] [CrossRef]
- Uwingabiye, J.; Frikh, M.; Lemnouer, A.; Bssaibis, F.; Belefquih, B.; Maleb, A.; Dahraoui, S.; Belyamani, L.; Bait, A.; Haimeur, C.; et al. Acinetobacter infections prevalence and frequency of the antibiotics resistance: Comparative study of intensive care units versus other hospital units. Pan Afr. Med. J. 2016, 23, 1–10. [Google Scholar] [CrossRef]
- Tran, G.M.; Ho-Le, T.P.; Ha, D.T.; Tran-Nguyen, C.H.; Nguyen, T.S.M.; Pham, T.T.N.; Nguyen, T.A.; Nguyen, D.A.; Hoang, H.Q.; Tran, N.V.; et al. Patterns of antimicrobial resistance in intensive care unit patients: A study in Vietnam. BMC Infect. Dis. 2017, 17, 429. [Google Scholar] [CrossRef] [PubMed]
- Álvarez, C.; Cortés, J.; Arango, Á.; Correa, C.; Leal, A. Resistencia antimicrobiana en unidades de cuidado intensivo de Bogotá, Colombia, 2001–2003. Revista de Salud Pública 2006, 8, 86–101. [Google Scholar] [CrossRef] [PubMed]
- Hamishehkar, H.; Shadmehr, P.; Mahmoodpoor, A.; Mashayekhi, S.O.; Entezari-Maleki, T. Antimicrobial susceptibility patterns among bacteria isolated from intensive care units of the largest teaching hospital at the northwest of Iran. Braz. J. Pharm. Sci. 2016, 52, 403–412. [Google Scholar] [CrossRef] [Green Version]
- Esfahani, B.N.; Basiri, R.; Mirhosseini, S.M.M.; Moghim, S.; Dolatkhah, S. Nosocomial infections in intensive care unit: Pattern of antibiotic-resistance in Iranian community. Adv. Biomed. Res. 2017, 6, 1–5. [Google Scholar]
- Ruppé, É.; Woerther, P.L.; Barbier, F. Mechanisms of antimicrobial resistance in Gram-negative bacilli. Ann. Intens. Care 2015, 5, 1–15. [Google Scholar] [CrossRef] [Green Version]
- Aardema, H.; Arends, J.P.; de Smet, A.M.; Zijlstra, J.G. Burden of highly resistant microorganisms in a Dutch intensive care unit. Neth. J. Med. 2015, 73, 169–174. [Google Scholar] [PubMed]
- MacFaddin, J.F. Biochemical Tests for Identification of Medical Bacteria, 3rd ed.; Williams and Wilkins: Baltimore, MD, USA, 2000. [Google Scholar]
- Clinical and Laboratory Standards Institute. Performance Standards for Antimicrobial Susceptibility Testing 2013; Twenty third informational supplement M100-S23; Clinical and Laboratory Standards Institute: Wayne, PA, USA, 2013. [Google Scholar]
- Tilton, R.C.; Lieberman, L.; Gerlach, E.H. Microdilution antibiotic susceptibility test: Examination of certain variables. Appl. Microbiol. 1973, 26, 658–665. [Google Scholar]
- Gutiérrez-Muñoz, J.; Ramírez-Corona, A.; Martínez-Bustamante, M.E.; Coria-Lorenzo, J.J.; Armenta-Gallegos, L.; Ayala-Franco, J.R.; Bernal-Granillo, S.M.; Flores-Zaleta, F.J.; García-Pérez, F.E.; Monjardín-Rochín, J.A.; et al. Estudio multicéntrico de resistencias bacterianas nosocomiales en México. Rev. Latin. Infect. Pediatr. 2017, 30, 68–75. [Google Scholar]
- Charles, M.P.; Kali, A.; Easow, J.M.; Joseph, N.M.; Ravishankar, M.; Srinivasan, S.; Kumar, S.; Umadevi, S. Ventilator-associated pneumonia. Australas. Med. J. 2014, 7, 334–344. [Google Scholar] [CrossRef]
- Weinstein, R.A. Controlling antimicrobial resistance in hospitals: Infection control and use of antibiotics. Emerg. Infect. Dis. 2001, 7, 188–192. [Google Scholar] [CrossRef]
- Durdu, B.; Meric-Koc, M.; Hakyemez, I.N.; Akkoyunlu, Y.; Daskaya, H.; Sumbul-Gultepe, B.; Aslan, T. Risk Factors affecting patterns of antibiotic resistance and treatment efficacy in extreme drug resistance in intensive care unit-acquired Klebsiella pneumoniae infections: A 5-year analysis. Med. Sci. Monit. 2019, 7, 174–183. [Google Scholar] [CrossRef] [PubMed]
- Ibrahim, M.E. High antimicrobial resistant rates among Gram-negative pathogens in intensive care units. A retrospective study at a tertiary care hospital in Southwest Saudi Arabia. Saudi Med. J. 2018, 39, 1035–1043. [Google Scholar] [CrossRef] [PubMed]
- Luna, C.M.; Rodríguez-Noriega, E.; Bavestrello, L.; Guzmán-Blanco, M. Gram-negative infections in adult intensive care units of Latin America and the Caribbean. Crit. Care Res. Pract. 2014, 2014, 1–12. [Google Scholar] [CrossRef] [PubMed]
- Hancock, R.E. Resistance mechanisms in Pseudomonas aeruginosa and other nonfermentative Gram-Negative bacteria. Clin. Infect. Dis. 1998, 1, S93–S99. [Google Scholar] [CrossRef] [PubMed]
- Ameen, N.; Memon, Z.; Shaheen, S.; Fatima, G.; Ahmed, F. Imipenem resistant Pseudomonas aeruginosa: The fall of the final quarterback. Pak. J. Med. Sci. 2015, 31, 561–565. [Google Scholar] [PubMed]
- Meletis, G. Carbapenem resistance: Overview of the problem and future perspectives. Ther. Adv. Infect. Dis. 2016, 3, 15–21. [Google Scholar] [CrossRef]
- López-García, A.; Rocha-Gracia, C.; Bello-López, E.; Juárez-Zelocualtecalt, C.; Sáenz, Y.; Castañeda-Lucio, M.; López-Pliego, L.; González-Vázquez, M.C.; Torres, C.; Ayala-Núñez, T.; et al. Characterization of antimicrobial resistance mechanisms in carbapenem-resistant Pseudomonas aeruginosa carrying IMP variants recovered from a Mexican hospital. Inf. Drug Resist. 2018, 11, 1523–1536. [Google Scholar] [CrossRef]
- Garza-Ramos, U.; Barrios, H.; Reyna-Flores, F.; Tamayo-Legorreta, E.; Catalán-Nájera, J.C.; Morfín-Otero, R.; Rodríguez-Noriega, E.; Volkow, P.; Cornejo-Juárez, P.; González, A.; et al. Widespread of ESBL- and carbapenemase GES-type genes on carbapenem-resistant Pseudomonas aeruginosa clinical isolates: A multicenter study in Mexican hospitals. Diagn. Microbiol. Infect. Dis. 2015, 81, 135–137. [Google Scholar] [CrossRef]
- Garza-González, E.; Llaca-Díaz, J.M.; Bosques-Padilla, F.J.; González, G.M. Prevalence of multidrug-resistant bacteria at a tertiary-care teaching hospital in Mexico: Special focus on Acinetobacter baumannii. Chemotherapy 2010, 56, 275–279. [Google Scholar] [CrossRef]
- US Centers for Disease Control and Prevention. Antibiotic Resistance Threats in the United States. 2013. Available online: https://www.cdc.gov/drugresistance/pdf/ar-threats-2013-508.pdf (accessed on 12 July 2018).
- Kluytmans-Vandenbergh, M.F.; Kluytmans, J.A.; Voss, A. Dutch guideline for preventing nosocomial transmission of Highly Resistant Microorganisms (HRMO). Infection 2005, 33, 309–313. [Google Scholar] [CrossRef]
- Souverein, D.; Euser, S.M.; Herpers, B.L.; Kluytmans, J.; Rossen, J.W.A.; Den-Boer, J.W. Association between rectal colonization with Highly Resistant Gram-negative Rods (HR-GNRs) and subsequent infection with HR-GNRs in clinical patients: A one-year historical cohort study. PLoS ONE 2017, 14, e0211016. [Google Scholar] [CrossRef] [PubMed]
- Andrew, B.; Kagirita, A.; Bazira, J. Prevalence of Extended-Spectrum Beta-Lactamases-Producing microorganisms in patients admitted at KRRH, southwestern Uganda. Int. J. Microb. 2017, 2017, 1–5. [Google Scholar] [CrossRef] [PubMed]
- Arora, A.; Jain, C.; Saxena, S.; Kaur, R. Profile of drug resistant Gram negative bacteria from ICU at a tertiary care center of India. Asian J. Med. Health 2017, 3, 1–7. [Google Scholar] [CrossRef]
- Sader, H.; Farrell, D.; Flamm, R.; Jones, R. Antimicrobial susceptibility of Gram-negative organisms isolated from patients hospitalized in intensive care units in United States and European hospitals (2009–2011). Diagn. Microbiol. Infect. Dis. 2014, 78, 443–448. [Google Scholar] [CrossRef] [PubMed]
- Guzmán-Blanco, M.; Labarca, J.A.; Villegas, M.V.; Gotuzzo, E. Extended spectrum β-lactamase producers among nosocomial Enterobacteriaceae in Latin America. Braz. J. Infect. Dis. 2014, 18, 421–433. [Google Scholar] [CrossRef] [PubMed]
- Garza-González, E.; Ibarra, S.I.M.; Llaca-Díaz, J.M.; González, G.M. Molecular characterization and antimicrobial susceptibility of extended-spectrum β-lactamase-producing Enterobacteriaceae isolates at a tertiary-care centre in Monterrey, Mexico. J. Med. Microbiol. 2011, 60, 84–90. [Google Scholar] [CrossRef] [PubMed]
- Morfín-Otero, R.; Mendoza-Olazarán, S.; Silva-Sánchez, J.; Rodríguez-Noriega, E.; Laca-Díaz, J.; Tinoco-Carrillo, P.; Petersen, L.; López, P.; Reyna-Flores, F.; Alcántar-Curiel, D.; et al. Characterization of Enterobacteriaceae isolates obtained from a tertiary care hospital in Mexico, which produces extended-spectrum beta-lactamase. Microb. Drug Resist. 2013, 19, 378–383. [Google Scholar] [CrossRef]
- Aquino-Andrade, A.; Mérida-Vieyra, J.; Arias de la Garza, E.; Arzate-Barbosa, P.; De Colsa-Ranero, A.E. Carbapenemase-producing Enterobacteriaceae in Mexico: Report of seven non-clonal cases in a pediatric hospital. BMC Microbiol. 2018, 18, 38. [Google Scholar] [CrossRef]
- Barrios, H.; Garza-Ramos, U.; Mejía-Miranda, I.; Reyna-Flores, F.; Sánchez-Pérez, A.; Mosqueda-García, D.; Silva-Sánchez, J. ESBL-producing Escherichia coli and Klebsiella pneumoniae: The most prevalent clinical isolates obtained between 2005 and 2012 in Mexico. J. Glob. Antimicrob. Resist. 2017, 10, 243–246. [Google Scholar] [CrossRef]
- Alcántar-Curiel, M.D.; Alpuche-Aranda, C.M.; Varona-Bobadilla, H.J.; Gayosso-Vázquez, C.; Jarillo-Quijada, M.D.; Frías-Mendívil, M.; Sanjuan-Padrón, L.; Santos-Preciado, J.I. Risk factors for extended-spectrum β-lactamases-producing Escherichia coli urinary tract infections in a tertiary hospital. Salud Pública de México 2015, 57, 412–418. [Google Scholar] [CrossRef]
- Mérida-Vieyra, J.; De Colsa, A.; Calderón-Castañeda, Y.; Arzate-Barbosa, P.; Aquino-Andrade, A. First report of group CTX-M-9 Extended spectrum beta- lactamases in Escherichia coli isolates from pediatric patients in Mexico. PLoS ONE 2016, 11, e0168608. [Google Scholar] [CrossRef] [PubMed]



| Sample | Total Number of Isolates | PA | KP | EC | AB | SM | ECl | OGNB |
|---|---|---|---|---|---|---|---|---|
| Bronchial secretions | 245 | 65 | 40 | 35 | 38 | 40 | 14 | 13 |
| Urine | 91 | 21 | 30 | 25 | 0 | 0 | 9 | 6 |
| Blood | 76 | 19 | 21 | 10 | 3 | 7 | 2 | 14 |
| Catheter | 37 | 13 | 7 | 3 | 6 | 0 | 3 | 5 |
| Wound | 34 | 10 | 6 | 8 | 4 | 2 | 4 | 0 |
| Cerebrospinal fluids | 28 | 25 | 0 | 0 | 2 | 0 | 0 | 1 |
| Pleural fluids | 5 | 2 | 0 | 2 | 0 | 0 | 0 | 1 |
| Ear-sample | 1 | 1 | 0 | 0 | 0 | 0 | 0 | 0 |
| Total (%) | 517 | 156 (30.17) | 104 (20.12) | 83 (16.05) | 53 (10.25) | 49 (9.48) | 32 (6.19) | 40 (7.74) |
| Antimicrobial Drugs | PA | KN | EC | AB | SM | ECl | OGNB | Overall Isolates |
|---|---|---|---|---|---|---|---|---|
| Ampicillin | 101/104 (97.12) | 78/83 (93.98) | 30/32 (93.75) | 22/22 (100) | 231/241 (95.85) | |||
| Ampicillin/ Sulbactam | 71/104 (68.27) | 64/83 (77.11) | 28/53 (52.83) | 24/32 (75.00) | 13/29 (44.83) | 200/301 (66.67) | ||
| Piperacillin | 12/17 (70.59) | 30/30 (100) | 20/25 (80.00) | 6/8 (75.00) | 0/2 (0.00) | 68/82 (82.93) | ||
| Piperacillin/ Tazobactam | 71/155 (45.80) | 28/103 (27.18) | 28/81 (34.57) | 8/32 (25.00) | 4/22 (18.18) | 139/393 (35.36) | ||
| Ticarcillin/ Clavulanic acid | 26/40 (65.00) | 11/28 (39.29) | 16/29 (55.17) | 16/28 (57.14) | 10/28 (35.71) | 4/7 (57.14) | 2/14 (14.29) | 85/174 (48.85) |
| Cefazolin | 25/41 (60.97) | 34/411 (82.93) | 8/8 (100) | 8/10 (80.00) | 75/100 (75.00) | |||
| Cefotetan | 7/62 (11.29) | 1/57 (1.75) | 6/16 (37.50) | 2/11 (18.18) | 16/146 (10.96) | |||
| Cefuroxime | 84/103 (81.55) | 73/83 (87.95) | 27/32 (84.98) | 18/22 (81.82) | 202/240 (84.17) | |||
| Cefotaxime | 84/104 (80.76) | 72/83 (86.75) | 40/53 (75.47) | 22/32 (68.75) | 17/29 (58.62) | 235/301 (78.07) | ||
| Ceftazidime | 100/154 (64.93) | 84/104 (80.76) | 73/83 (87.95) | 43/53 (81.13) | 28/49 (57.14) | 22/32 (68.75) | 24/36 (66.67) | 374/511 (73.19) |
| Ceftriaxone | 84/104 (80.76) | 73/83 (87.95) | 36/53 (67.92) | 23/32 (71.88) | 17/29 (58.62) | 233/301 (77.41) | ||
| Cefepime | 83/155 (55.13) | 83/104 (79.80) | 71/83 (85.54) | 40/53 (75.47) | 19/32 (59.37) | 17/29 (58.62) | 313/456 (68.64) | |
| Aztreonam | 24/57 (42.11) | 65/74 (87.84) | 56/63 (88.89) | 14/16 (87.50) | 8/12 (66.67) | 167/222 (75.23) | ||
| Imipenem | 108/155 (69.68) | 10/104 (9.62) | 3/83 (3.61) | 7/32 (21.88) | 2/15 (13.33) | 130/389 (33.41) | ||
| Meropenem | 84/155 (54.19) | 7/104 (6.73) | 2/83 (2.41) | 30/53 (56.60) | 1/32 (3.13) | 3/36 (8.33) | 127/463 (27.42) | |
| Ciprofloxacin | 65/155 (41.93) | 32/104 (30.77) | 65/83 (78.31) | 42/53 (79.25) | 16/32 (50.00) | 8/29 (27.59) | 228/456 (49.34) | |
| Levofloxacin | 61/155 (39.35) | 16/104 (15.38) | 63/83 (75.90) | 32/53 (60.38) | 3/49 (6.12) | 4/32 (12.50) | 7/36 (19.44) | 186/512 (36.32) |
| Moxifloxacin | 5/28 (17.86) | 21/30 (70.00) | 1/8 (12.50) | 1/9 (11.11) | 28/75 (37.33) | |||
| Amikacin | 90/155 (58.06) | 14/104 (13.46) | 8/83 (9.64) | 31/53 (58.49) | 5/32 (15.63) | 10/29 (34.48) | 158/456 (34.65) | |
| Gentamicin | 80/155 (51.61) | 48/104 (46.15) | 52/83 (62.65) | 45/53 (84.91) | 9/32 (28.13) | 8/29 (27.59) | 242/456 (53.07) | |
| Tobramycin | 66/155 (42.58) | 63/102 (61.76) | 64/81 (79.01) | 34/53 (64.15) | 15/31 (48.39) | 18/29 (62.07) | 260/451 (57.65) | |
| Trimethoprim/ Sulfamethoxazole | 66/102 (64.71) | 52/82 (63.41) | 41/53 (77.36) | 4/49 (8.16) | 15/31 (48.39) | 15/35 (42.86) | 193/352 (54.83) |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Uc-Cachón, A.H.; Gracida-Osorno, C.; Luna-Chi, I.G.; Jiménez-Guillermo, J.G.; Molina-Salinas, G.M. High Prevalence of Antimicrobial Resistance Among Gram-Negative Isolated Bacilli in Intensive Care Units at a Tertiary-Care Hospital in Yucatán Mexico. Medicina 2019, 55, 588. https://doi.org/10.3390/medicina55090588
Uc-Cachón AH, Gracida-Osorno C, Luna-Chi IG, Jiménez-Guillermo JG, Molina-Salinas GM. High Prevalence of Antimicrobial Resistance Among Gram-Negative Isolated Bacilli in Intensive Care Units at a Tertiary-Care Hospital in Yucatán Mexico. Medicina. 2019; 55(9):588. https://doi.org/10.3390/medicina55090588
Chicago/Turabian StyleUc-Cachón, Andrés H., Carlos Gracida-Osorno, Iván G. Luna-Chi, Jonathan G. Jiménez-Guillermo, and Gloria M. Molina-Salinas. 2019. "High Prevalence of Antimicrobial Resistance Among Gram-Negative Isolated Bacilli in Intensive Care Units at a Tertiary-Care Hospital in Yucatán Mexico" Medicina 55, no. 9: 588. https://doi.org/10.3390/medicina55090588