1. Introduction
Diving is an activity that can have significant cardiovascular effects on the human body, including changes in heart rate (
), blood pressure and cardiac output, and alterations in pulmonary circulation [
1]. These changes can place significant stress on the cardiovascular system and increase the risk of worsening underlying cardiomyopathies during diving. Therefore, it is important for individuals with preexisting cardiac conditions to undergo a thorough medical evaluation before engaging in diving activities.
Elevated environmental pressure causes changes in cardiac function, including an increase in systolic volume and a decrease in
to maintain an adequate cardiac output and minimize the impact on the body. This adaptation is possible thanks to the autonomic nervous system (ANS) response [
2]. Assessing the ANS response to significant pressure changes is challenging and may vary significantly among individuals. Studies aimed at monitoring and controlling this response in extreme conditions, as well as identifying potential health risks for divers, are of great interest. Such studies are particularly important in the training of military personnel. Typically, the response of the ANS is characterized by both time and frequency analysis of the heart rate variability signal (
), particularly those related to temporal changes in
and those related to the power of the different spectral bands and their relationships. Previous studies have shown variations in these indices when the barometric pressure changes [
3,
4].
It is important to mention that there are serious health issues that can be derived from diving activities, particularly if the decompression protocol is not properly followed, that cannot be directly studied from the
signal. The clearest example is an arterial gas embolism, which can occur when air bubbles, usually caused by pulmonary barotrauma during a rapid ascent, enter the bloodstream and travel to the heart and other organs, leading to tissue damage and potentially life-threatening complications [
5]. In addition, diving can also increase the risk of long-term cardiovascular problems such as arterial disease, hypertension, and atherosclerosis. According to a study published in the Journal of the American College of Cardiology, diving-induced stress on the cardiovascular system can lead to endothelial dysfunction, oxidative stress, and chronic inflammation, which can contribute to the development of cardiovascular diseases [
6].
While increased pressure is a critical factor in the adaptive response of the ANS during diving, other variables can also significantly affect this response. The diving environment itself can influence the sympathovagal balance and the adaptation to humid conditions, known as the diving reflex. In this reflex, the slows down to reduce oxygen consumption, mediated by the parasympathetic nervous system. Cold water temperature leads to vasoconstriction, which is related to increased sympathetic activity. Additionally, the buoyancy and relaxation effects of water immersion promote parasympathetic activity.
Several other factors influence the sympathovagal balance during diving. Physical exertion and increased cardiovascular workload can trigger sympathetic activation. The respiratory pattern plays a role, with breathing through a regulator potentially inducing sympathetic activation, while controlled breathing techniques may promote vagal tone. Moreover, gas density is influenced by pressure and temperature, which can impact the ease and efficiency of breathing. Psychological factors, such as stress and anxiety, can also promote sympathetic activity [
7]. Moreover, individuals with previous expertise in diving tend to experience relaxation and subsequent parasympathetic dominance.
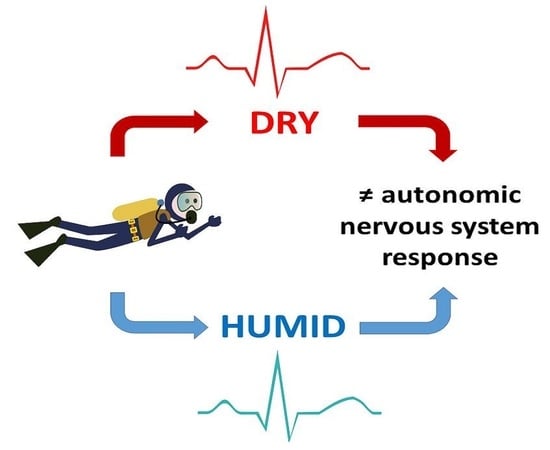
The present study aims to investigate the autonomic response during diving in both dry and humid conditions, taking into account that factors related to the environment may also have an impact, and to identify -derived indices that show significant discrepancies between the two conditions. For this purpose, electrocardiographic signals (ECG) were recorded from two groups of subjects. The first group performed a simulated immersion in a dry hyperbaric chamber, while the second group underwent the same immersion protocol in a humid hyperbaric chamber.
3. Results
Figure 3 illustrates that the computed indices showed similar trends in the referenced indices between the two groups of subjects. To avoid unnecessary repetitions, the referencing symbol
is not used in the rest of the text of the manuscript when specific indices are mentioned. The time indices in the dry dataset exhibited positive values in general for all stages, with slight increases over time, whereas the trend was also increasing for the indices with the humid dataset, except for a strong decrease in the stage “1A” for
,
, and
. Only the
exhibited significant differences between the two datasets in three out of the four stages analyzed. Regarding the frequency indices, the general trends over time were not so clear, with the four indices showing median values close to 0 in the dry dataset, and similarly with
and
in the humid dataset.
displayed the most significant differences, since, in the humid dataset, it took negative values and showed a decreasing trend over time. It is worth mentioning that
had a large variability in both datasets, whereas that of
was very reduced, particularly in the humid dataset.
Interestingly, the stages that showed significant differences in the highest number of indices were the stage with the highest pressure, stage “5” (for
,
,
and
), and the last stage of the immersion, stage “1A” (for
,
,
,
), which suggests that the differences between datasets were more prominent at high pressure and after spending a long time in hyperbaric conditions (see
Figure 3).
3.1. Safety Ranges
Figure 4 shows the evolution of both the IQR and 5–95 percentile ranges in dry hyperbaric conditions (in red) together with the individual values of the five subjects of the humid dataset (symbols in blue) during the simulated immersions. It is worth mentioning that the index variations between consecutive stages were considered linear for the representation of the patches. As can be derived from the analysis of the statistical ranges,
and
showed, in general, less prominent variations than the rest of the indices with respect to the baseline in all of the stages of immersion (i.e., the values were closer to 0). Interestingly, the ranges tended to be enlarged in the last stage of the immersion for all of the time indices, when the pressure was the same as in the baseline conditions before the immersion started, probably indicating that ANS recovery may be highly variable between subjects with different previous diving expertise and/or physical condition, whereas the widths of the ranges of the frequency indices were more stable in the four stages of immersion.
In the analysis of the humid indices with the dry chamber ranges, there was an overlap between the two groups for all of the stages and indices, except for and in the “1A” stage. This was due to the narrow ranges of these two indices, indicating small relative variations between the subjects in both datasets. The differences in the two other time indices were subtle: the trends were similar in both datasets, while showed larger positive ranges in the dry chamber subjects than in the humid chamber subjects in the early stages of immersion. This resulted in an increasing overlap between the two groups as the immersion progressed.
Regarding the frequency indices, the large variability of the
was reflected in both the wide ranges observed in
Figure 4 and the indices of the humid subjects. The ranges of
overlapped; however, in this case, the overlap was due to the thin width of the ranges computed with the humid dataset. Regarding the ranges of
and
, the main differences were observed in the second, with indices showing more negative values in the humid dataset than the dry dataset ranges, suggesting a reduction in the index during the immersion with respect to the baseline.
3.2. Subject Classification
As explained in the Methods section, the determination of whether a subject’s ANS response was classified as “abnormal” relied on the identification of indices that fell outside the previously calculated ranges. This classification process was conducted using all of the indices of individual subjects in both datasets (28 dry + 5 humid) with the ranges derived from the 28 subjects of the dry dataset. The results of the classification are shown in
Table 1.
As expected, since the ranges were based on the dry dataset values, out of the 28 subjects of the dry chamber, none of them exhibited significantly abnormal behavior (i.e., with more than 8 indices outside of the 5–95 percentile dry ranges), and only 3 subjects showed more than 20 indices outside of the IQR (one female and two males). In the classification of the subjects in the humid chamber dataset, of the five subjects, two showed more than 8 indices outside of the 5–95 percentile range, one of them with more than 20 indices outside of the IQR.
3.3. Stage and Index Classification
In order to identify the stages and indices in which differences in the ANS behavior between both databases were more prominent, an additional classification of the humid subjects with the dry ranges was performed.
Figure 5 shows the indices of the humid subjects, separated by stages, outside of the 5–95 percentile range of the dry database. On the one hand, the stage with the largest number of indices classified as out of range was “1A” (over 50% of a total number of indices of 40 (8 indices × 1 stage × 5 subjects)). On the other hand, the indices that led to classifying the largest number of stages as out of range were:
and
(over 50% of a total number of stages of 20 (1 index × 4 stages × 5 subjects)).
4. Discussion
The present study aimed to investigate the ANS responses of healthy individuals during simulated dives in hyperbaric chambers and to explore the effects of humidity and the factors associated with the protocols in both chambers (temperature, body position…) on these responses. Our analysis of -derived indices and their statistical ranges revealed important insights into the ANS responses of the subjects at stages at different depths during the immersions.
The results showed that the
index was notably reduced in all stages of the humid dataset compared to the dry dataset, indicating a reduction in parasympathetic activity not associated with respiration in humid conditions. This finding is consistent with previous studies [
18] and suggests that the longer the time spent within the hyperbaric chamber, the more prominent the sympathetic dominance becomes. Additionally, the
index was found to be the most different between datasets, with a reduction in the humid dataset compared to the dry dataset [
4]. This points to activation of sympathetic activity triggered by factors such as cold water temperature and psychological stress or anxiety associated with diving. There are, however, studies pointing to an increase in parasympathetic activity when the skin makes contact with water [
19] or when subjects breathed through a mouthpiece compared to spontaneous breathing [
16]. This effect may also be present in the baseline state, thereby negating its effect when referencing the rest of the measurements to this state. In the case of hyperbaric conditions, there is an additional factor to consider. As the pressure increases, more effort is required to extract air from the regulator, and, over time, this respiratory effort can become tiring, triggering the dominance of the parasympathetic response [
16]. All of this may suggest that the impact of the pressure of the environment dominates over other effects. Overall, the impact of the differentiating factors between the dry and humid chambers is mitigated by referencing the indices’ values to those obtained at the baseline stage. For instance, the changes associated with the diving reflex, which typically lead to an increase in parasympathetic activity, as mentioned earlier, already occur during the baseline stage (1D). Consequently, the ANS response stemming from the diving reflex is present throughout all stages. Similarly, the increased vagal tone resulting from breathing through a respiration mask persists throughout the entire immersion period, and referencing the baseline values helps minimize this factor. Furthermore, the decision to keep the divers in a horizontal position in the humid chamber was made to ensure that the entire body experiences the same pressure when immersed in water. If the divers were seated or in a vertical position, there would be variations in the pressure sensed by the head and feet.
One of the key contributions of our study was the classification of subjects into “normal” and “abnormal” categories based on the statistical range between the 5 and 95 percentiles and the IQR for each index and stage. These ranges could be used to generate warnings when monitoring the activity of divers and serve as a reference for avoiding future immersions if many indices are out of the normal ranges. Importantly, all subjects were apparently healthy, and most had significant previous expertise in diving, indicating that these ranges could be used as a baseline for any diver (professional or amateur). Among the few subjects classified as “abnormal” in the dry dataset, the ratio between females and males was much higher than that of the complete dataset (one out of three classified out of IQR). This could indicate that it may be necessary to adapt the warning ranges based on gender differences.
Our analysis also revealed that the humidity of the surrounding environment, together with its associated immersion protocol and body position, plays a crucial role in the ANS response of the subjects and their classification as “abnormal”. The stage with the largest number of indices out of range was “1A”, indicating that the recovery of ANS activity at sea level notably diverges between subjects within the two datasets. The indices with the highest number of stages classified as abnormal with the alternate dataset ranges were different between datasets, with
and
being the most affected in the humid dataset, as well as
and, to a lesser extent,
and
in the dry dataset. These results suggest that
, reflected in these time indices, is a crucial factor in determining whether a subject should be warned in a dry immersion, while
is key in the classification of abnormality in humid conditions [
18].
Finally, we checked whether using mathematical methods to overcome the limitations of the relatively low number of subjects in both hyperbaric chambers by increasing the variability presented by default datasets, such as the bootstrap aggregating method [
20], would affect the results of the classification and observed that it had a slight impact on the number of subjects classified as abnormal.
As stated in the Introduction section, the ANS response in variable hyperbaric environments can be influenced by numerous factors, both directly and indirectly. These factors contribute to the complex dynamics of the sympathovagal balance during diving, and gaining a comprehensive understanding of their interplay is crucial. While this study has shed light on some of these factors, there is still a need for further research to delve more deeply into their specific contributions and implications for divers’ physiological responses. One aspect requiring further investigation is the role of some environmental factors, such as water temperature, which may also vary with pressure and humidity. These factors can significantly impact the ANS response and have implications for divers’ cardiovascular and respiratory systems. Examining how changes in these environmental conditions affect the sympathovagal balance will provide valuable insights into the adaptive mechanisms of the ANS during diving.
Additionally, individual factors, including divers’ physical fitness, previous diving experience, and psychological state, can influence the ANS response. Investigating how these individual characteristics interact with environmental factors will enhance our understanding of the personalized nature of the sympathovagal balance in divers. Furthermore, the potential influence of different breathing patterns, respiratory control techniques, and gas mixtures on the ANS response warrants further exploration.
By conducting comprehensive studies that incorporate these various factors, researchers can unravel the intricate web of interactions shaping the sympathovagal balance during diving. This knowledge will not only contribute to our fundamental understanding of human physiology but also have practical implications for diving safety and performance. Ultimately, continued research in this field will provide valuable insights for optimizing dive protocols, training strategies, and medical guidelines tailored to individual divers, enhancing their overall well-being and performance in hyperbaric environments. Overall, our findings provide important insights into ANS responses during simulated dives in hyperbaric chambers and could be used as a reference for divers in the future.
Limitations
Obtaining an extensive database of signals recorded under realistic diving conditions at such great depths is very challenging for several reasons: specific equipment that is not accessible to the general population is needed (hyperbaric chambers), there are significant health risks for subjects if descent and ascent protocols are not properly followed, and subjects must have prior diving experience. Taking all this into consideration, the number of subjects registered in this study was limited, especially in the dataset from the humid hyperbaric chamber, which could affect the statistical significance of the differences between datasets. Nevertheless, the database was still large enough to derive qualitative conclusions about the impact of humidity on the ANS response during dives.
On the other hand, our study only utilized data from stationary stages with stable barometric pressure lasting several minutes within the immersion. Thus, extrapolating the evolution of index values and their respective ranges during intervals of pressure change should be approached with caution. To further analyze the raw signals and ensure accuracy, non-stationary methods should be considered in future studies.