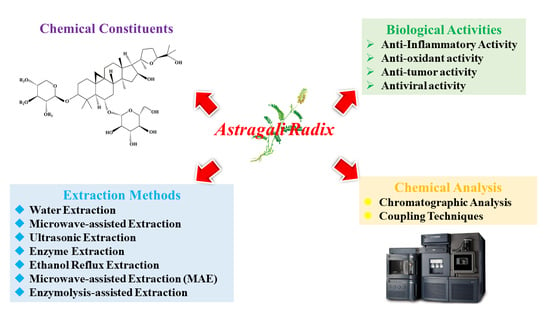
Advances in Chemical Composition, Extraction Techniques, Analytical Methods, and Biological Activity of Astragali Radix
Abstract
:1. Introduction
2. Chemical Composition
2.1. Polysaccharides
2.2. Saponins
2.3. Flavonoids
2.4. Others
3. Extraction Methods for AR Components
3.1. Extraction Methods for Astragalus Polysaccharides (AP)
3.1.1. Water Extraction
3.1.2. Microwave-Assisted Extraction
3.1.3. Ultrasonic Extraction
3.1.4. Enzyme Extraction
3.2. Extraction of Saponins and Flavonoids
3.2.1. Ethanol Reflux Extraction
3.2.2. Microwave-Assisted Extraction (MAE)
3.2.3. Enzymolysis-Assisted Extraction
3.3. Others
4. Analytical Methods
4.1. Spectral Analysis
4.2. Chromatographic Analysis
4.3. Coupling Techniques
5. Biological Activities of AR
5.1. Anti-Inflammatory Activity
5.2. Antioxidant Activity
5.3. Anti-Tumor Activity
5.4. Antiviral Activity
5.5. Cardiovascular Disease Prevention
5.6. Anti-Diabetic Activity
5.6.1. Prevention and Treatment of T1DM
5.6.2. Prevention and Treatment of T2DM
6. Standardization of AR
6.1. Efficacy Standards
6.2. Bioactivity Standards
6.3. Production Standards
7. Conclusions
Authors Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Fu, J.; Wang, Z.; Huang, L.; Zheng, S.; Wang, D.; Chen, S.; Zhang, H.; Yang, S. Review of the botanical characteristics, phytochemistry, and pharmacology of Astragalus membranaceus (huangqi). Phytother. Res. 2014, 28, 1275–1283. [Google Scholar] [CrossRef]
- Zhang, R.-P.; Zhang, X.-P.; Ruan, Y.-F.; Ye, S.-Y.; Zhao, H.-C.; Cheng, Q.-H.; Wu, D.-L. Protective effect of radix astragali injection on immune organs of rats with obstructive jaundice and its mechanism. World J. Gastroenterol. 2009, 15, 2862–2869. [Google Scholar] [CrossRef]
- Li, R.; Chen, W.-c.; Wang, W.-p.; Tian, W.-y.; Zhang, X.-g. Antioxidant activity of Astragalus polysaccharides and antitumour activity of the polysaccharides and sirna. Carbohydr. Polym. 2010, 82, 240–244. [Google Scholar] [CrossRef]
- Kafle, B.; Baak, J.P.A.; Brede, C. Major bioactive chemical compounds in astragali radix samples from different vendors vary greatly. PLoS ONE 2021, 16, 1–8. [Google Scholar] [CrossRef]
- Sun, X.-R.; Wei, G.-J.; Wang, H.-Y.; Zhao, W.-W.; Zhang, Z.; Zhang, T.; Wei, F.; Zhang, Y.-J. Evaluation of astragali radix quality grade based on appearance characteristics and internal ingredients. China J. Chin. Mater. Med. 2021, 46, 966–971. [Google Scholar]
- Zhang, Q.; Gao, W.-Y.; Man, S.-L. Chemical composition and pharmacological activities of astragali radix. China J. Chin. Mater. Med. 2012, 37, 3203–3207. [Google Scholar]
- Jin, M.; Zhao, K.; Huang, Q.; Shang, P. Structural features and biological activities of the polysaccharides from Astragalus membranaceus. Int. J. Biol. Macromol. 2014, 64, 257–266. [Google Scholar] [CrossRef]
- Yeh, T.-S.; Chuang, H.-L.; Huang, W.-C.; Chen, Y.-M.; Huang, C.-C.; Hsu, M.-C. Astragalus membranaceus improves exercise performance and ameliorates exercise-induced fatigue in trained mice. Molecules 2014, 19, 2793–2807. [Google Scholar] [CrossRef] [Green Version]
- Rios, J.L.; Waterman, P.G. A review of the pharmacology and toxicology of Astragalus. Phytother. Res. 1997, 11, 411–418. [Google Scholar] [CrossRef]
- Xu, D.-J.; Xia, Q.; Wang, J.-J.; Wang, P.-P. Molecular weight and monosaccharide composition of Astragalus polysaccharides. Molecules 2008, 13, 2408–2415. [Google Scholar] [CrossRef] [Green Version]
- Wang, D.Q.; Shen, W.M.; Tian, Y.P. Scavenging effects of active principles from Astragalus mongholicus bunge on oxygen free radicals studied by esr. Prog. Biochem. Biophys. 1996, 23, 260–262. [Google Scholar]
- Yan, H.; Xie, Y.; Sun, S.; Sun, X.; Ren, F.; Shi, Q.; Wang, S.; Zhang, W.; Li, X.; Zhang, J. Chemical analysis of Astragalus mongholicus polysaccharides and antioxidant activity of the polysaccharides. Carbohydr. Polym. 2010, 82, 636–640. [Google Scholar] [CrossRef]
- Huang, Q.S.; Lu, G.B.; Li, Y.C.; Guo, J.H.; Wang, R.X. Studies on the polysaccharides of “huang qi” (astrag alus mongholicus bunge (author’s transl). Acta Pharmaceutica Sinica 1982, 17, 200–206. [Google Scholar]
- Liu, M.; Wu, K.; Mao, X.; Wu, Y.; Ouyang, J. Astragalus polysaccharide improves insulin sensitivity in kkay mice: Regulation of pkb/glut4 signaling in skeletal muscle. J. Ethnopharmacol. 2010, 127, 32–37. [Google Scholar] [CrossRef]
- Xu, Q.; Ma, X.; Liang, X. Determination of astragalosides in the roots of Astragalus spp. Using liquid chromatography tandem atmospheric pressure chemical ionization mass spectrometry. Phytochem. Anal. 2007, 18, 419–427. [Google Scholar] [CrossRef]
- Du, H.-w.; Zhao, X.-l.; Zhang, A.-h.; Yao, L.; Zhang, Y.-y. Rapid separation, identification and analysis of Astragalus membranaceus fisch using liquid chromatography-tandem mass spectrometry. J. Chromatogr. Sci. 2014, 52, 226–231. [Google Scholar] [CrossRef] [Green Version]
- Hirotani, M.; Zhou, Y.; Lui, H.; Furuya, T. Astragalosides from hairy root cultures of Astragalus-membranaceus. 100. Studies on plant-tissue cultures. Phytochemistry 1994, 36, 665–670. [Google Scholar] [CrossRef]
- Zhou, Y.; Hirotani, M.; Rui, H.; Furuya, T. 2 triglycosidic triterpene astragalosides from hairy root cultures of Astragalus-membranaceus. Phytochemistry 1995, 38, 1407–1410. [Google Scholar] [CrossRef]
- He, Z.Q.; Findlay, J.A. Constituents of Astragalus-membranaceus. J. Nat. Prod. 1991, 54, 810–815. [Google Scholar] [CrossRef]
- Yu, Q.-T.; Qi, L.-W.; Li, P.; Yi, L.; Zhao, J.; Bi, Z. Determination of seventeen main flavonoids and saponins in the medicinal plant huang-qi (radix astragali) by hplc-dad-elsd. J. Sep. Sci. 2007, 30, 1292–1299. [Google Scholar] [CrossRef]
- Kitagawa, I. Chemical investigation of naturally-occurring drug materials—Elucidation of scientific basis for traditional medicines and exploitation of new naturally-occurring drugs. Yakugaku Zasshi-J. Pharm. Soc. Jpn. 1992, 112, 1–41. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Du, N.; Xu, Z.; Gao, M.; Liu, P.; Sun, B.; Cao, X. Combination of ginsenoside rg1 and astragaloside iv reduces oxidative stress and inhibits tgf-beta 1/smads signaling cascade on renal fibrosis in rats with diabetic nephropathy. Drug Des. Dev. Ther. 2018, 12, 3517–3524. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zhang, Z.Y.; Wu, B.; Tang, Y.H.; Li, Z.X.; Sun, Z.L.; Chen, L.Y.; Ji, Y.B.; Ma, C.H.; Huang, C.G. Characterization of major flavonoids, triterpenoid, dipeptide and their metabolites in rat urine after oral administration of radix astragali decoction. J. Anal. Chem. 2013, 68, 716–721. [Google Scholar] [CrossRef]
- Lin, L.Z.; He, X.G.; Lindenmaier, M.; Nolan, G.; Yang, J.; Cleary, M.; Qiu, S.X.; Cordell, G.A. Liquid chromatography-electrospray ionization mass spectrometry study of the flavonoids of the roots of Astragalus mongholicus and a-membranaceus. J. Chromatogr. A 2000, 876, 87–95. [Google Scholar] [CrossRef]
- Guo-hui, C.; Wen-feng, H. Progress in pharmacological effects of compositions of Astragalus membranaceus. Chin. J. New Drugs 2008, 17, 1482–1485. [Google Scholar]
- Chen, R.-Z.; Tan, L.; Jin, C.-G.; Lu, J.; Tian, L.; Chang, Q.-Q.; Wang, K. Extraction, isolation, characterization and antioxidant activity of polysaccharides from Astragalus membranaceus. Ind. Crops Prod. 2015, 77, 434–443. [Google Scholar] [CrossRef]
- Li, R.; Chen, W.-c.; Wang, W.-p.; Tian, W.-y.; Zhang, X.-g. Optimization of extraction technology of Astragalus polysaccharides by response surface methodology and its effect on cd40. Carbohydr. Polym. 2009, 78, 784–788. [Google Scholar]
- Wen, X.; Shao, J.; Wang, L.; Zhao, Z.; Guo, M. Optimization of extracting polysaccharides from Astragalus by orthogonal design and three colorimetric methods. China J. Tradit. Chin. Med. Pharm. 2018, 33, 1562–1566. [Google Scholar]
- Hao, J.Y.; Han, W.; Huang, S.D.; Xue, B.Y.; Deng, X. Microwave-assisted extraction of artemisinin from artemisia annua l. Sep. Purif. Technol. 2002, 28, 191–196. [Google Scholar] [CrossRef]
- Gong, S.; Yang, Z. Investigation into the microwave-assisted extraction technology for Astragalus polysaccharide. J. South China Univ. Technol. Nat. Sci. Ed. 2004, 32, 93–96. [Google Scholar]
- Lv, G.P.; Hu, D.J.; Cheong, K.L.; Li, Z.Y.; Qing, X.M.; Zhao, J.; Li, S.P. Decoding glycome of Astragalus membranaceus based on pressurized liquid extraction, microwave-assisted hydrolysis and chromatographic analysis. J. Chromatogr. A 2015, 1409, 19–29. [Google Scholar] [CrossRef]
- Cheng, J.-H.; Guo, Q.; Sun, D.-W.; Han, Z. Kinetic modeling of microwave extraction of polysaccharides from Astragalus membranaceus. J. Food Processing Preserv. 2019, 43, 1–9. [Google Scholar] [CrossRef]
- Chemat, F.; Zill e, H.; Khan, M.K. Applications of ultrasound in food technology: Processing, preservation and extraction. Ultrason. Sonochemistry 2011, 18, 813–835. [Google Scholar] [CrossRef] [PubMed]
- Li, J.X.; Xue, B.; Chai, Q.; Liu, Z.X.; Zhao, A.P.; Chen, L.B. Antihypertensive effect of total flavonoid fraction of Astragalus complanatus in hypertensive rats. Chin. J. Physiol. 2005, 48, 101–106. [Google Scholar] [PubMed]
- Puri, M.; Sharma, D.; Barrow, C.J. Enzyme-assisted extraction of bioactives from plants. Trends Biotechnol. 2012, 30, 37–44. [Google Scholar] [CrossRef] [PubMed]
- Chen, H.; Zhou, X.; Zhang, J. Optimization of enzyme assisted extraction of polysaccharides from Astragalus membranaceus. Carbohydr. Polym. 2014, 111, 567–575. [Google Scholar] [CrossRef]
- Lijun, D.; Bohang, S.U.N. Research reviews on astragaloside IV. J. Shenyang Pharm. Univ. 2011, 28, 410–416. [Google Scholar]
- Weihua, X.; Lujia, H.A.N. Study on extraction technology of flavonoids from Astragalus mongholicus by alcohol reflux. Sci. Technol. Food Ind. 2008, 29, 233–235. [Google Scholar]
- Yan, M.-M.; Liu, W.; Fu, Y.-J.; Zu, Y.-G.; Chen, C.-Y.; Luo, M. Optimisation of the microwave-assisted extraction process for four main astragalosides in radix astragali. Food Chem. 2010, 119, 1663–1670. [Google Scholar] [CrossRef]
- Yong-guang, B.I.; Tai-qiu, Q.I.U.; Kun-ping, L.I.; Ai-qun, S.U.N. Cellulase enzymatic extraction of total flavonoids of Astragalus technology. Lishizhen Med. Mater. Med. Res. 2009, 20, 2478–2480. [Google Scholar]
- Lan-Hua, X.; Bing, D.; Qiong-Juan, Y.; Jia-Yi, Z.; Tao, Y.; Gong-Ming, Y. Study on cellulase enzymolysis assisted ethanol extraction of total flavonoids from radix Astragalus. Packag. Food Mach. 2013, 31, 7–12. [Google Scholar]
- Pan, C.; Wang, H.; Shan, H.; Lu, H. Preparative isolation and purification of calycosin and formononetin from astragali radix using hydrolytic extraction combined with high speed countercurrent chromatography. J. Chromatogr. Sci. 2021, 59, 412–418. [Google Scholar] [CrossRef] [PubMed]
- Wang, W.; Zheng, B.; Wu, J.; Lv, W.; Lin, P.; Gong, X. Determination of the dissociation constants of 16 active ingredients in medicinal herbs using a liquid-liquid equilibrium method. Separations 2021, 8, 49. [Google Scholar] [CrossRef]
- Chu, C.; Qi, L.-W.; Liu, E.H.; Li, B.; Gao, W.; Li, P. Radix astragali (Astragalus): Latest advancements and trends in chemistry, analysis, pharmacology and pharmacokinetics. Curr. Org. Chem. 2010, 14, 1792–1807. [Google Scholar] [CrossRef]
- Lin, H.; Chen, Y.; Feng, S.; Chen, W.; Lin, D.; Huang, H.; Lin, J.; Chen, R.; Chen, G.; Yu, Y. Surface-enhanced raman on gold nanoparticles for the identification of the most common adulterant of astragali radix. Spectrosc. Lett. 2018, 51, 389–394. [Google Scholar] [CrossRef]
- Song, Y.; Li, P.; Wang, D.; Cheng, Y.-Y. Micellar electrokinetic chromatography for the quantitative analysis of flavonoids in the radix of Astragalus membranaceus var.Mongholicus. Planta Med. 2008, 74, 84–89. [Google Scholar] [CrossRef]
- Han, Q.B.; Song, J.Z.; Qiao, C.F.; Wong, L.; Xu, H.X. Preparative isolation of cyclolanostane-type saponins from Astragalus membranaceus bge. Var. Mongholicus (bge.) hsiao by tlc-ms/ms guided high-speed counter-current chromatography. J. Sep. Sci. 2007, 30, 135–140. [Google Scholar] [CrossRef]
- Liu, Y.; Liu, J.; Wu, K.-X.; Guo, X.-R.; Tang, Z.-H. A rapid method for sensitive profiling of bioactive triterpene and flavonoid from Astragalus mongholicus and Astragalus membranaceus by ultra-pressure liquid chromatography with tandem mass spectrometry. J. Chromatogr. B-Anal. Technol. Biomed. Life Sci. 2018, 1085, 110–118. [Google Scholar] [CrossRef]
- Liu, P.-P.; Shan, G.-S.; Zhang, F.; Shi, J.; Jia, T.-Z. Comparison of 12 constituents of astragali radix directionally processed with organic acid by uplc-ms. China J. Chin. Mater. Med. 2020, 45, 113–118. [Google Scholar]
- Liu, X.-h.; Zhao, L.-g.; Liang, J.; Guo, L.; Yang, Y.-l.; Hu, F.; Zhu, R.-j.; Feng, S.-l. Component analysis and structure identification of active substances for anti-gastric ulcer effects in radix astragali by liquid chromatography and tandem mass spectrometry. J. Chromatogr. B-Anal. Technol. Biomed. Life Sci. 2014, 960, 43–51. [Google Scholar] [CrossRef]
- Yin, G.; Cheng, X.; Tao, W.; Dong, Y.; Bian, Y.; Zang, W.; Tang, D. Comparative analysis of multiple representative components in the herb pair astragali radix-curcumae rhizoma and its single herbs by uplc-qqq-ms. J. Pharm. Biomed. Anal. 2018, 148, 224–229. [Google Scholar] [CrossRef] [PubMed]
- Li, X.; Qu, L.; Dong, Y.; Han, L.; Liu, E.; Fang, S.; Zhang, Y.; Wang, T. A review of recent research progress on the Astragalus genus. Molecules 2014, 19, 18850–18880. [Google Scholar] [CrossRef] [PubMed]
- Guo, Z.; Lou, Y.; Kong, M.; Luo, Q.; Liu, Z.; Wu, J. A systematic review of phytochemistry, pharmacology and pharmacokinetics on astragali radix: Implications for astragali radix as a personalized medicine. Int. J. Mol. Sci. 2019, 20, 1463. [Google Scholar] [CrossRef] [Green Version]
- Li, H.; Zhang, Y.; Min, J.; Gao, L.; Zhang, R.; Yang, Y. Astragaloside iv attenuates orbital inflammation in graves’ orbitopathy through suppression of autophagy. Inflamm. Res. 2018, 67, 117–127. [Google Scholar] [CrossRef] [PubMed]
- Zhu, Z.; Li, J.; Zhang, X. Astragaloside iv protects against oxidized low-density lipoprotein (ox-ldl)-induced endothelial cell injury by reducing oxidative stress and inflammation. Med. Sci. Monit. 2019, 25, 2132–2140. [Google Scholar] [CrossRef] [PubMed]
- Hoo, R.L.C.; Wong, J.Y.L.; Qiao, C.F.; Xu, A.; Xu, H.X.; Lam, K.S.L. The effective fraction isolated from radix astragali alleviates glucose intolerance, insulin resistance and hypertriglyceridemia in db/db diabetic mice through its anti-inflammatory activity. Nutr. Metab. 2010, 7, 1–9. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Noest, X.; Pferschy-Wenzig, E.-M.; Nikles, S.; He, X.; Fan, D.; Lu, A.; Yuk, J.; Yu, K.; Isaac, G.; Bauer, R. Identification of constituents affecting the secretion of pro-inflammatory cytokines in lps-induced u937 cells by uhplc-hrms-based metabolic profiling of the traditional chinese medicine formulation huangqi jianzhong tang. Molecules 2019, 24, 3116. [Google Scholar] [CrossRef] [Green Version]
- Hao, M.; Liu, Y.; Chen, P.; Jiang, H.; Kuang, H.-Y. Astragaloside iv protects rgc-5 cells against oxidative stress. Neural Regen. Res. 2018, 13, 1081–1086. [Google Scholar]
- Yang, P.; Zhou, Y.; Xia, Q.; Yao, L.; Chang, X. Astragaloside iv regulates the pi3k/akt/ho-1 signaling pathway and inhibits h9c2 cardiomyocyte injury induced by hypoxia-reoxygenation. Biol. Pharm. Bull. 2019, 42, 721–727. [Google Scholar] [CrossRef] [Green Version]
- Murata, I.; Abe, Y.; Yaginuma, Y.; Yodo, K.; Kamakari, Y.; Miyazaki, Y.; Baba, D.; Shinoda, Y.; Iwasaki, T.; Takahashi, K.; et al. Astragaloside-iv prevents acute kidney injury and inflammation by normalizing muscular mitochondrial function associated with a nitric oxide protective mechanism in crush syndrome rats. Ann. Intensive Care 2017, 7, 1–9. [Google Scholar] [CrossRef] [Green Version]
- Oh, H.-A.; Choi, H.J.; Kim, N.J.; Kim, D.-H. Anti-stress effect of astragaloside iv in immobilized mice. J. Ethnopharmacol. 2014, 153, 928–932. [Google Scholar] [CrossRef] [PubMed]
- Gong, G.; Zheng, Y.; Yang, Y.; Sui, Y.; Wen, Z. Pharmaceutical values of calycosin: One type of flavonoid isolated from Astragalus. Evid.-Based Complement. Altern. Med. 2021, 2021, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Yang, B.; Yang, N.; Chen, Y.; Zhu, M.; Lian, Y.; Xiong, Z.; Wang, B.; Feng, L.; Jia, X. An integrated strategy for effective-component discovery of astragali radix in the treatment of lung cancer. Front. Pharmacol. 2021, 11, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Li, W.; Song, K.; Wang, S.; Zhang, C.; Zhuang, M.; Wang, Y.; Liu, T. Anti-tumor potential of Astragalus polysaccharides on breast cancer cell line mediated by macrophage activation. Mater. Sci. Eng. C-Mater. Biol. Appl. 2019, 98, 685–695. [Google Scholar] [CrossRef] [PubMed]
- Cho, W.C.S.; Leung, K.N. In vitro and in vivo anti-tumor effects of Astragalus membranaceus. Cancer Lett. 2007, 252, 43–54. [Google Scholar] [CrossRef] [PubMed]
- Li, J.; Bao, Y.; Lam, W.; Li, W.; Lu, F.; Zhu, X.; Liu, J.; Wang, H. Immunoregulatory and anti-tumor effects of polysaccharopeptide and Astragalus polysaccharides on tumor-bearing mice. Immunopharmacol. Immunotoxicol. 2008, 30, 771–782. [Google Scholar]
- Xu, C.; Wang, Y.; Feng, J.; Xu, R.; Dou, Y. Extracts from huangqi (radix astragali mongoliciplus) and ezhu (rhizoma curcumae phaeocaulis) inhibit lewis lung carcinoma cell growth in a xenograft mouse model by impairing mitogen-activated protein kinase signaling, vascular endothelial growth factor production, and angiogenesis. J. Tradit. Chin. Med. 2019, 39, 559–565. [Google Scholar]
- Wang, Z.; Cheng, Z.; Fang, X. Antiviral action of combined use of rhizoma polygoni cuspidati and radix astragali on hsv-1 strain. China J. Chin. Mater. Med. 1999, 24, 176–192. [Google Scholar]
- Tang, L.L.; Sheng, J.F.; Xu, C.H.; Liu, K.Z. Clinical and experimental effectiveness of astragali compound in the treatment of chronic viral hepatitis b. J. Int. Med. Res. 2009, 37, 662–667. [Google Scholar] [CrossRef] [Green Version]
- Kajimura, K.; Takagi, Y.; Ueba, N.; Yamasaki, K.; Sakagami, Y.; Yokoyama, H.; Yoneda, K. Protective effect of astragali radix by oral administration against Japanese encephalitis virus infection in mice. Biol. Pharm. Bull. 1996, 19, 1166–1169. [Google Scholar] [CrossRef] [Green Version]
- Wang, S.; Li, J.; Huang, H.; Gao, W.; Zhuang, C.; Li, B.; Zhou, P.; Kong, D. Anti-hepatitis b virus activities of astragaloside iv isolated from radix astragali. Biol. Pharm. Bull. 2009, 32, 132–135. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zheng, Q.; Zhu, J.-Z.; Bao, X.-Y.; Zhu, P.-C.; Tong, Q.; Huang, Y.-Y.; Zhang, Q.-H.; Zhang, K.-J.; Zheng, G.-Q.; Wang, Y. A preclinical systematic review and meta-analysis of astragaloside iv for myocardial ischemia/reperfusion injury. Front. Physiol. 2018, 9, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Liu, Z.-h.; Liu, H.-b.; Wang, J. Astragaloside iv protects against the pathological cardiac hypertrophy in mice. Biomed. Pharmacother. 2018, 97, 1468–1478. [Google Scholar] [CrossRef] [PubMed]
- Leng, B.; Tang, F.; Lu, M.; Zhang, Z.; Wang, H.; Zhang, Y. Astragaloside iv improves vascular endothelial dysfunction by inhibiting the tlr4/nf-kappa b signaling pathway. Life Sci. 2018, 209, 111–121. [Google Scholar] [CrossRef] [PubMed]
- Lin, X.-P.; Cui, H.-J.; Yang, A.L.; Luo, J.-K.; Tang, T. Astragaloside iv improves vasodilatation function by regulating the pi3k/akt/enos signaling pathway in rat aorta endothelial cells. J. Vasc. Res. 2018, 55, 169–176. [Google Scholar] [CrossRef] [PubMed]
- Jin, C.; Dai, R.H. Effect of Astragalus membranaceus on erythrocyte sodium content and sodium transport in the coronary heart disease. Chin. J. Integr. Med. 1991, 11, 651-3, 643. [Google Scholar]
- Qin, H.; Liu, P.; Lin, S. Effects of astragaloside iv on the sdf-1/cxcr4 expression in atherosclerosis of apoe(−/−) mice induced by hyperlipaemia. Evid.-Based Complement. Altern. Med. 2015, 2015, 1–9. [Google Scholar] [CrossRef]
- Jia, G.; Leng, B.; Wang, H.; Dai, H. Inhibition of cardiotrophin-1 overexpression is involved in the anti-fibrotic effect of astrogaloside iv. Mol. Med. Rep. 2017, 16, 8365–8370. [Google Scholar] [CrossRef]
- Piao, Y.-l.; Liang, X.-c. Astragalus membranaceus injection combined with conventional treatment for viral myocarditis: A systematic review of randomized controlled trials. Chin. J. Integr. Med. 2014, 20, 787–791. [Google Scholar] [CrossRef]
- Su, D.; Li, H.-Y.; Yan, H.-R.; Liu, P.-F.; Zhang, L.; Cheng, J.-H. Astragalus improved cardiac function of adriamycin-injured rat hearts by upregulation of serca2a expression. Am. J. Chin. Med. 2009, 37, 519–529. [Google Scholar] [CrossRef]
- Iantorno, M.; Hays, A.G.; Schar, M.; Krishnaswamy, R.; Soleimanifard, S.; Steinberg, A.; Stuber, M.; Gerstenblith, G.; Weiss, R.G. Simultaneous noninvasive assessment of systemic and coronary endothelial function. Circ.-Cardiovasc. Imaging 2016, 9, 1–9. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Huang, Y.; Kwan, K.K.L.; Leung, K.W.; Wang, H.; Kong, X.P.; Dong, T.T.X.; Tsim, K.W.K. The extracts and major compounds derived from astragali radix alter mitochondrial bioenergetics in cultured cardiomyocytes: Comparison of various polar solvents and compounds. Int. J. Mol. Sci. 2018, 19, 1574. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Qiu, L.-H.; Zhang, B.-Q.; Lian, M.-J.; Xie, X.-J.; Chen, P. Vascular protective effects of Astragalus membranaceus and its main constituents in rats with chronic hyperhomocysteinemia. Exp. Ther. Med. 2017, 14, 2401–2407. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Roden, M.; Shulman, G.I. The integrative biology of type 2 diabetes. Nature 2019, 576, 51–60. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cho, J.; D’Antuono, M.; Glicksman, M.; Wang, J.; Jonklaas, J. A review of clinical trials: Mesenchymal stem cell transplant therapy in type 1 and type 2 diabetes mellitus. Am. J. Stem Cells 2018, 7, 82–93. [Google Scholar]
- Hull, C.M.; Peakman, M.; Tree, T.I.M. Regulatory t cell dysfunction in type 1 diabetes: What’s broken and how can we fix it? Diabetologia 2017, 60, 1839–1850. [Google Scholar] [CrossRef] [Green Version]
- Sang, Z.; Zhou, L.; Fan, X.; McCrimmon, R.J. Radix astragali (huangqi) as a treatment for defective hypoglycemia counterregulation in diabetes. Am. J. Chin. Med. 2010, 38, 1027–1038. [Google Scholar] [CrossRef]
- Li, R.-J.; Qiu, S.-D.; Chen, H.-X.; Tian, H.; Wang, H.-X. The immunotherapeutic effects of Astragalus polysaccharide in type 1 diabetic mice. Biol. Pharm. Bull. 2007, 30, 470–476. [Google Scholar] [CrossRef] [Green Version]
- Chen, W.; Li, Y.M.; Yu, M.H. Astragalus polysaccharides: An effective treatment for diabetes prevention in nod mice. Exp. Clin. Endocrinol. Diabetes 2008, 116, 468–474. [Google Scholar] [CrossRef]
- Zhou, X.; Xu, Y.; Yang, G.; Li, F. Increased galectin-1 expression in muscle of Astragalus polysaccharide-treated type 1 diabetic mice. J. Nat. Med. 2011, 65, 500–507. [Google Scholar] [CrossRef]
- Zhang, R.; Qin, X.; Zhang, T.; Li, Q.; Zhang, J.; Zhao, J. Astragalus polysaccharide improves insulin sensitivity via ampk activation in 3t3-l1 adipocytes. Molecules 2018, 23, 2711. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chen, X.; Wang, H.; Jiang, M.; Zhao, J.; Fan, C.; Wang, Y.; Peng, W. Huangqi (Astragalus) decoction ameliorates diabetic nephropathy via irs1-pi3k-glut signaling pathway. Am. J. Transl. Res. 2018, 10, 2491–2501. [Google Scholar] [PubMed]
- Chen, W.; Xia, Y.; Zhao, X.; Wang, H.; Chen, W.; Yu, M.; Li, Y.; Ye, H.; Zhang, Y. The critical role of Astragalus polysaccharides for the improvement of ppra alpha-mediated lipotoxicity in diabetic cardiomyopathy. PLoS ONE 2012, 7, e45541. [Google Scholar]
- Li, M.; Wang, W.; Xue, J.; Gu, Y.; Lin, S. Meta-analysis of the clinical value of Astragalus membranaceus in diabetic nephropathy. J. Ethnopharmacol. 2011, 133, 412–419. [Google Scholar] [CrossRef]
- Koh, A.; Backhed, F. From association to causality: The role of the gut microbiota and its functional products on host metabolism. Mol. Cell 2020, 78, 584–596. [Google Scholar] [CrossRef]
- Wang, X.-M.; Li, X.-B.; Peng, Y. Impact of qi-invigorating traditional chinese medicines on intestinal flora: A basis for rational choice of prebiotics. Chin. J. Nat. Med. 2017, 15, 241–254. [Google Scholar] [CrossRef]
- Yao, Y.; Zhang, H.; Li, J.; Zhang, J.; Sun, X. Effect of Modified Huangqi Biejiatang Combined with Auricular Acupressure on Diabetic Peripheral Neuropathy of Qi-Yin Deficiency Syndrome and Serum MyD88/IκB Signaling Pathway. Chin. J. Exp. Formul. 2021, 27, 98–105. (In Chinese) [Google Scholar]
- Ul Uza, N.; Dastagir, G. Microscopic and pharmacognostic standardization of Astragalus scorpiurus bunge. Microsc. Res. Tech. 2022, 85, 324–338. [Google Scholar] [CrossRef]








| No. | Name | Molecular Weight (Da) | Identification Method | Classification | Structure | Source | Refs. |
|---|---|---|---|---|---|---|---|
| 1 | AG-1 | - | 400 M NMR | Glucan | - | A. membranaceus | [13] |
| 2 | AG-2 | - | 400 M NMR | Glucan | - | A. membranaceus | [13] |
| 3 | AH-1 | - | 400 M NMR | Heteropolysaccharide | - | A. membranaceus | [13] |
| 4 | AH-2 | - | 400 M NMR | Heteropolysaccharide | - | A. membranaceus | [13] |
| 5 | APS-I | 1.7 × 106 | HPLC (C18), TLC | Heteropolysaccharide | - | A. membranaceus | [7] |
| 6 | APS-II | 1.2 × 106 | HPLC (C18), TLC | D-Glucan | Dextran bonded mainly with-(1 → 4)-d-glycosidic linkage | A. membranaceus | [7] |
| 7 | APS-III | 3.5 × 104 | 400 M NMR | D-Glucan | Dextran bonded mainly with -(1 → 4)-d-glycosidic linkage | A. membranaceus | [14] |
| No. | Compound Name | Molecular Formula | Molecular Weight | ESI–MS | APCI–MS | Source | Refs. | ||
|---|---|---|---|---|---|---|---|---|---|
| Parent Ion (m/z) | Fragment Ion (m/z) | Parent Ion (m/z) | Fragment Ion (m/z) | ||||||
| 1 | Astragaloside I | C45H72O16 | 869.04 | - | - | 867.7 [M − H]− | 807.5 [M − H-Ac]− | A. membranaceus | [15] |
| 2 | Isoastragaloside I | C45H72O16 | 869.04 | - | - | - | - | A. membranaceus | [21] |
| 3 | Acetylastragaloside I | C47H74O17 | 911.08 | - | - | - | - | A. membranaceus | [21] |
| 4 | Astragaloside II | C43H70O15 | 827.00 | - | - | 825.7 [M − H]− | 765.5 [M − H-Ac]− | A. membranaceus | [15] |
| 5 | Isoastragaloside II | C43H70O15 | 827.00 | - | - | - | - | A. membranaceus | [21] |
| 6 | Astragaloside IV | C41H68O14 | 784.97 | - | - | 783.7 [M − H]− | 651.4 [M − H−(Xyl-H2O)]− | A. membranaceus | [15] |
| 7 | Astragaloside IV isomer/III | C41H68O14 | 784.97 | - | - | 783.7 [M − H]− | 651.7 [M − H-(Xyl-H2O)]− | A. membranaceus | [15] |
| 8,9,10 | Astragaloside V/VI/VII | C47H78O19 | 947.11 | - | - | 945.6 [M − H]− | 783.6 [M − H-(Glu-H2O)]− | A. membranaceus | [15] |
| 11 | Soyasaponin II | C47H76O17 | 913.10 | 914 [M + H]+ | 457.4 | - | - | A. membranaceus | [22] |
| 12 | Soyasaponin I | C48H78O18 | 943.12 | 944 [M + H]+ | 617.4 | - | - | A. membranaceus | [22] |
| 13 | Agroastragaloside III | C51H82O21 | 1031.18 | - | - | - | - | A. membranaceus | [20] |
| 14 | Agroastragaloside IV | C49H80O20 | 989.14 | - | - | - | - | A. membranaceus | [20] |
| 15 | Agroastragaloside I | C45H74O16 | 871.06 | - | - | - | - | A. membranaceus | [17] |
| 16 | Alexandroside | C36H62O10 | 654.87 | - | - | - | - | A. membranaceus A. membranaceus | [20] |
| No. | Compounds Name | Molecular Formula | Molecular Weight | ESI–MS | APCI–MS | Source | Refs. | ||
|---|---|---|---|---|---|---|---|---|---|
| Parent Ion (m/z) [M + H]+/[M + Na]+ | Fragment Ion (m/z) | Parent Ion (m/z) [M + H]+ | Fragment Ion (m/z) | ||||||
| 1 | Formononetin | C16H12O4 | 268.27 | 269 | 254 | - | - | both | [20,24] |
| 2 | Ononin | C22H22O9 | 430.40 | 431 | 269 | - | - | both | [20,24] |
| 3 | Calycosin | C16H12O5 | 284.26 | 285 | 275 | - | - | both | [20,24] |
| 4 | formononetin-7-O-β-d-glucoside-6”-O-acetate (4), (8), | C24H24O10 | 472.44 | - | - | 473 | 269 | both | [23] |
| 5 | Formononetin-7-O-β-d-glucoside-6”-O-malonate | C25H24O12 | 516.45 | 517 | 269 | - | - | A. membranaceus | [24] |
| 6 | Calycosin-7-O-β-d-glycoside | C22H22O10 | 446.40 | 447 | 285 | - | - | both | [24] |
| 7 | Calycosin-7-O-β-d-glucoside-6”-O-malonate | C25H24O13 | 532.45 | 533 | 285 | - | - | A. membranaceus | [24] |
| 8 | Calycosin-7-O-β-d-glucoside-6”-O-acetate | C24H24O11 | 488.44 | - | - | 489 | 285 | both | [23] |
| 9 | Pratensein | C16H12O6 | 300.26 | - | - | 301 | 269 | both | [23] |
| 10 | Pratensein-7-O-β-d-glycoside | C22H22O11 | 462.40 | - | - | 463 | 301 | both | [23] |
| 11 | Biochanin-A | C16H12O5 | 284.30 | - | - | 285 | - | A. membranaceus | [23] |
| 12 | (3R)-7,2′-Dihydroxy-3′,4′-dimethoxyisoflavan | C17H18O5 | 302.32 | - | - | 303 | 167 | both | [23,24] |
| 13 | (6a,llaR)-3-Hydroxy-9,10-Dimethoxypterocarpan | C17H16O5 | 300.31 | 301 | 152 | - | - | A. membranaceus | [23,24] |
| 14 | (6a,llaR)-3-Hydroxy-9,10-Dimethoxypterocarpan-3-O-β-d-glycoside | C23H26O10 | 462.15 | 463 | 301 | - | - | A. membranaceus | [24] |
| 15 | Astraisoflavanglucoside-6”-O-malonate | C26H30O13 | 550 | 551 | 303 | - | - | A. membranaceus | [24] |
| 16 | Wogonin | C16H12O5 | 284.27 | 285.1 | 270.2 | - | - | A. membranaceus | [22] |
| 17 | 3-Hydroxyflavanone | C15H12O3 | 240.25 | 241 | - | - | - | A. membranaceus | [22] |
| 18 | Medicarpin | C16H14O4 | 270.28 | 271 | - | - | - | A. membranaceus | [22] |
| 19 | Isorhamnetin | C16H12O7 | 316.26 | 317 | - | - | - | A. membranaceus | [22] |
| 20 | Mangiferin | C19H18O11 | 422.34 | 423 | - | - | - | A. membranaceus | [22] |
| 21 | Naringin | C27H32O14 | 580.53 | 603 | - | - | - | A. membranaceus | [22] |
| Advantages | Disadvantages | |
|---|---|---|
| Water extraction | Simple operation and low production costs (maximal extraction rate of AP was 16.32%) | Large energy consumption and low extraction rate |
| Ethanol Reflux extraction | Wide range of applications, simple equipment, good extraction effect | Long extraction time, solvent residue |
| Microwave-assisted Extraction | Penetrating heating, time saving, high efficiency, energy saving (maximal extraction rate of AP was 32%, 49% improvement compared to conventional water extraction) | Volatile components gradually dissipate as the extraction time increases. |
| Ultrasonic extraction | Simple operation, high efficiency, time saving and energy saving (maximal extraction rate of AP was 30.28%, 46.23% improvement compared to conventional water extraction) | Sound pollution |
| Enzyme extraction | High specificity and efficiency (maximal extraction rate of AP was 29.96%, 45.52% improvement compared to conventional water extraction) | High production costs |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chang, X.; Chen, X.; Guo, Y.; Gong, P.; Pei, S.; Wang, D.; Wang, P.; Wang, M.; Chen, F. Advances in Chemical Composition, Extraction Techniques, Analytical Methods, and Biological Activity of Astragali Radix. Molecules 2022, 27, 1058. https://doi.org/10.3390/molecules27031058
Chang X, Chen X, Guo Y, Gong P, Pei S, Wang D, Wang P, Wang M, Chen F. Advances in Chemical Composition, Extraction Techniques, Analytical Methods, and Biological Activity of Astragali Radix. Molecules. 2022; 27(3):1058. https://doi.org/10.3390/molecules27031058
Chicago/Turabian StyleChang, Xiangna, Xuefeng Chen, Yuxi Guo, Pin Gong, Shuya Pei, Danni Wang, Peipei Wang, Mengrao Wang, and Fuxin Chen. 2022. "Advances in Chemical Composition, Extraction Techniques, Analytical Methods, and Biological Activity of Astragali Radix" Molecules 27, no. 3: 1058. https://doi.org/10.3390/molecules27031058