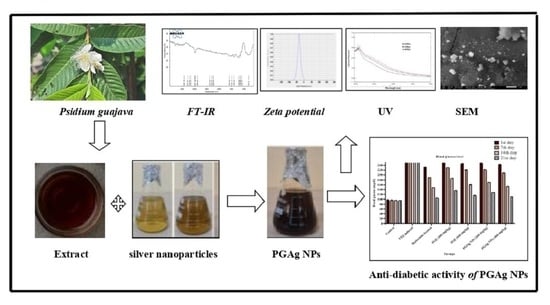
Green Synthesis and Characterization of Silver Nanoparticles of Psidium guajava Leaf Extract and Evaluation for Its Antidiabetic Activity
Abstract
:1. Introduction
2. Results and Discussion
2.1. Phytochemical Constituents Present in the Extracts of P. guajava Leaves
2.2. Characterization of Psidium Guajava Silver Nanoparticles
2.2.1. UV-Visible Spectroscopy Analysis
2.2.2. Fourier Transform Infrared Spectroscopy (FTIR)
2.2.3. Scanning Electron Microscopy (SEM)
2.2.4. Zeta Potential
2.3. Evaluation of Antidiabetic Activity
2.3.1. Blood Glucose Level
2.3.2. Body Weight
2.3.3. Biochemical Parameters
2.3.4. Histopathological Examination
Liver Cells
Pancreatic Cells
3. Materials and Methods
3.1. Collection of Plant Materials
3.2. Preparation of Plant Extract
3.3. Preliminary Phytochemical Screening
3.4. Synthesis of Silver Nanoparticles from P. guajava Extract
3.5. Characterization
3.5.1. UV-Visible Spectroscopic Analysis
3.5.2. Fourier Transform Infrared Spectroscopy (FTIR)
3.5.3. Scanning Electron Microscopy (SEM) Analysis
3.5.4. Zeta Potential
3.6. In-Vivo Antidiabetic Activity
3.6.1. Experimental Animals
3.6.2. Induction of Diabetes
3.6.3. Experimental Design
3.6.4. Blood Glucose Level
3.6.5. Assessment of Body Weight
3.6.6. Biochemical and Histopathological Analysis
3.7. Statistical Analysis
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Sample Availability
References
- Parameswaran, G.; Ray, D.W. Sleep, circadian rhythms, and type 2 diabetes mellitus. Clin. Endocrinol. News 2022, 96, 12–20. [Google Scholar] [CrossRef]
- DeFronzo, R.A.; Ferrannini, E.; Groop, L.; Henry, R.R.; Herman, W.H.; Holst, J.J.; Hu, F.B.; Kahn, C.R.; Raz, I.; Shulman, G.I.; et al. Type 2 diabetes mellitus. Nat. Rev. Dis. Primers 2015, 1, 15019. [Google Scholar] [CrossRef]
- Saeedi, P.; Petersohn, I.; Salpea, P.; Malanda, B.; Karuranga, S.; Unwin, N.; Colagiuri, S.; Guariguata, L.; Motala, A.A.; Ogurtsova, K.; et al. Global and regional diabetes prevalence estimates for 2019 and projections for 2030 and 2045: Results from the International Diabetes Federation Diabetes Atlas. Diabetes Res. Clin. Pract. 2019, 157, 107843. [Google Scholar] [CrossRef] [Green Version]
- Turin, A.; Radobuljac, M.D. Psychosocial factors affecting the etiology and management of type 1 diabetes mellitus: A narrative review. World J. Diabetes 2021, 12, 1518. [Google Scholar] [CrossRef]
- Oguntibeju, O.O. Type 2 diabetes mellitus, oxidative stress and inflammation: Examining the links. Int. J. Physiol. Pathophysiol. Pharmacol. 2019, 11, 45–63. [Google Scholar]
- SreeHarsha, N.; Shariff, A.; Shendkar, Y.A.; Al-Dhubiab, B.E.; Meravanige, G. Development and Evaluation of a (SEDDS) Self—Emulsifying Drug Delivery System for Darifenacin Hydrobromide. Indian J. Pharm. Educ. Res. 2019, 53, 204–212. [Google Scholar] [CrossRef] [Green Version]
- Pachava, S.; Puttachari, S.; Shariff, A.; Thakur, R.S. Formulation and Evaluation of Solid Selfmicroemulsifying Drug Delivery System of A Selective Second Generation Cephalosporin Antibiotic. Int. J. Pharm. Sci. Rev. Res. 2014, 24, 176–181. [Google Scholar]
- Keat, C.L.; Aziz, A.; Eid, A.M.; Elmarzugi, N.A. Biosynthesis of nanoparticles and silver nanoparticles. Bioresour. Bioprocess. 2015, 2, 47. [Google Scholar] [CrossRef] [Green Version]
- Khan, I.; Saeed, K.; Khan, I. Nanoparticles: Properties, applications and toxicities. Arab. J. Chem. 2019, 12, 908–931. [Google Scholar] [CrossRef]
- Liu, Y.; Zeng, S.; Liu, Y.; Wu, W.; Shen, Y.; Zhang, L.; Li, C.; Chen, H.; Liu, A.; Shen, L.; et al. Synthesis and antidiabetic activity of selenium nanoparticles in the presence of polysaccharides from Catathelasma ventricosum. Int. J. Biol. Macromol. 2018, 114, 632–639. [Google Scholar] [CrossRef]
- Javed, B.; Mashwani, Z.U.; Sarwer, A.; Raja, N.I.; Nadhman, A. Synergistic response of physicochemical reaction parameters on biogenesis of silver nanoparticles and their action against colon cancer and leishmanial cells. Artif. Cells Nanomed. Biotechnol. 2020, 48, 1340–1353. [Google Scholar] [CrossRef]
- Malapermal, V.; Botha, I.; Krishna, S.B.; Mbatha, J.N. Enhancing antidiabetic and antimicrobial performance of Ocimumbasilicum, and Ocimum sanctum (L.) using silver nanoparticles. Saudi J. Biol. Sci. 2017, 24, 1294–1305. [Google Scholar] [CrossRef]
- Ahmed, S.S.; Prakash, K.C.; Tabassum, S.; Salma, N.; Devi, K.A. Antidiarrhoeal Potential of various Solvent Extracts of Achyranthes aspera against three diverse diarrhoeal animal models. Res. J. Pharm. Technol. 2021, 14, 4173–4177. [Google Scholar] [CrossRef]
- Anand, U.; Jacobo-Herrera, N.; Altemimi, A.; Lakhssassi, N. A comprehensive review on medicinal plants as antimicrobial therapeutics: Potential avenues of biocompatible drug discovery. Metabolites 2019, 9, 258. [Google Scholar] [CrossRef] [Green Version]
- Anand, U.; Tudu, C.K.; Nandy, S.; Sunita, K.; Tripathi, V.; Loake, G.J.; Dey, A.; Proćków, J. Ethnodermatological use of medicinal plants in India: From ayurvedic formulations to clinical perspectives—A review. J. Ethnopharmacol. 2022, 284, 114744. [Google Scholar] [CrossRef]
- Kumar, M.; Tomar, M.; Amarowicz, R.; Saurabh, V.; Nair, M.S.; Maheshwari, C.; Sasi, M.; Prajapati, U.; Hasan, M.; Singh, S.; et al. Guava (Psidium guajava L.) leaves: Nutritional composition, phytochemical profile, and health-promoting bioactivities. Foods 2021, 10, 752. [Google Scholar] [CrossRef]
- Hamida, R.S.; Abdelmeguid, N.E.; Ali, M.A.; Bin-Meferij, M.M.; Khalil, M.I. Synthesis of silver nanoparticles using a novel cyanobacteria Desertifilum sp. extract: Their antibacterial and cytotoxicity effects. Int. J. Nanomed. 2020, 15, 49–63. [Google Scholar] [CrossRef] [Green Version]
- Kesharwani, J.; Yoon, K.Y.; Hwang, J.; Rai, M. Phytofabrication of silver nanoparticles by leaf extract of Datura metel: Hypothetical mechanism involved in synthesis. J. Bionanosci. 2009, 3, 39–44. [Google Scholar] [CrossRef]
- Khan, S.A.; Shahid, S.; Lee, C.S. Green synthesis of gold and silver nanoparticles using leaf extract of clerodendruminerme; characterization, antimicrobial, and antioxidant activities. Biomolecules 2020, 10, 835. [Google Scholar] [CrossRef]
- Anandalakshmi, K.; Venugobal, J.; Ramasamy, V. Characterization of silver nanoparticles by green synthesis method using Pedalium murex leaf extract and their antibacterial activity. Appl. Nanosci. 2016, 6, 399–408. [Google Scholar] [CrossRef] [Green Version]
- Kokate, C.K. Practical Pharmacognosy, 4th ed.; Vallabh Prakashan: Delhi, India, 1994; p. 107. [Google Scholar]
- Devanesan, S.; AlSalhi, M.S. Green synthesis of silver nanoparticles using the flower extract of Abelmoschus esculentus for cytotoxicity and antimicrobial studies. Int. J. Nanomed. 2021, 16, 3343. [Google Scholar] [CrossRef] [PubMed]
- Yassin, M.A.; Elgorban, A.M.; El-Samawaty, A.E.; Almunqedhi, B.M. Biosynthesis of silver nanoparticles using Penicillium verrucosum and analysis of their antifungal activity. Saudi J. Biol. Sci. 2021, 28, 2123–2127. [Google Scholar] [CrossRef] [PubMed]
- Shafaghat, A. Synthesis and characterization of silver nanoparticles by phytosynthesis method and their biological activity. Inorg. Nano-Met. Chem. 2015, 45, 381–387. [Google Scholar] [CrossRef]
- Bairagi, U.; Mittal, P.; Singh, J.; Mishra, B. Preparation, characterization, and in vivo evaluation of nano formulations of ferulic acid in diabetic wound healing. Drug Dev. Ind. Pharm. 2018, 44, 1783–1796. [Google Scholar] [CrossRef] [PubMed]
- Sharma, A.; Kaur, R.; Kaur, J.; Garg, S.; Bhatti, R.; Kaur, A. An endophytic Schizophyllum commune Fr. exhibits in-vitro and in-vivo antidiabetic activity in streptozotocin induced diabetic rats. AMB Express 2021, 11, 58. [Google Scholar] [CrossRef]
- Manekeng, H.T.; Mbaveng, A.T.; Ntyam Mendo, S.A.; Agokeng, A.J.; Kuete, V. Evaluation of acute and subacute toxicities of Psidium guajava methanolic bark extract: A botanical with in vitro antiproliferative potential. Evid.-Based Complement. Altern. Med. 2019. [Google Scholar] [CrossRef] [Green Version]








| Group | Blood Glucose Levels (mg/dL) (Mean ± SEM) | |||
|---|---|---|---|---|
| 1st Day | 7th Day | 14th Day | 21st Day | |
| GP I | 97 ± 0.577 | 96.5 ± 1.87 | 95.3 ± 0.88 | 94.50 ± 0.76 |
| GP II | 281.16 ± 1.13 | 289.5 ± 0.76 | 289.7 ± 0.88 | 293.3 ± 0.55 |
| GP III | 231.5 ± 1.25 c f | 189.8 ± 0.94 c f | 147.5 ± 0.76 c f | 104.5 ± 0.76 c f |
| GP IV | 251.83 ± 1.3 c f | 229.5 ± 0.76 c f | 186.5 ± 0.76 c f | 135.8 ± 0.6 c f |
| GP V | 246.3 ± 1.35 c f | 219.7 ± 2.48 c f | 161.2 ± 1.07 c f | 115.8 ± 1.24 c f |
| GP VI | 248.5 ± 1.23 c f | 221 ± 1.3 c f | 169.8 ± 0.94 c f | 126.8 ± 0.79 c f |
| GP VII | 243 ± 1.6 c f | 207.3 ± 1.52 c f | 153 ± 0.81 c f | 109.7 ± 0.88 c f |
| Groups | Mean Body Weight (g) (Mean ± SEM) | |||
|---|---|---|---|---|
| 1st Day | 7th Day | 14th Day | 21st Day | |
| GP I | 189.8 ± 2.89 | 198.2 ± 3 | 200.8 ± 2.7 | 205 ± 2.05 |
| GP II | 198.2 ± 1.64 | 180.3 ± 1.66 | 168 ± 1.5 | 160 ± 2.0 |
| GP III | 196 ± 2.7 ns | 199.5 ± 2.4 c f | 203.2 ± 2.4 c f | 206.7 ± 1.92 c f |
| GP IV | 191.7 ± 3.45 ns | 186.3 ± 3.33 ns | 177 ± 3.4 a d | 172.1 ± 2.8 b e |
| GP V | 194.2 ± 2.38 ns | 193.2 ± 2.38 b e | 200.8 ± 2.2 c f | 206.8 ± 1.77 c f |
| GP VI | 197 ± 2.74 ns | 191.2 ± 2.3 a d | 180 ± 2.1 b e | 179.2 ± 1.6 c f |
| GP VII | 196.7 ± 3.8 ns | 201.5 ± 3.8 c f | 205.3 ± 2.72 c f | 209 ± 2.38 c f |
| Group | Biochemical Parameters(mg/dL) | ||||
|---|---|---|---|---|---|
| TG | TC | HDL | LDL | VLDL | |
| GP I | 85.5 ± 0.76 | 132.5 ± 0.76 | 53.5 ± 1.17 | 34.5 ± 0.76 | 18.5 ± 0.76 |
| GP II | 143.3 ± 0.88 | 265.3 ± 0.91 | 31.33 ± 0.66 | 65 ± 1.06 | 41.83 ± 0.79 |
| GP III | 89.5 ± 0.99 c f | 147.7 ± 0.61 c f | 45.17 ± 0.94 c f | 39.50 ± 0.76 c f | 22.5 ± 0.76 c f |
| GP IV | 133.8 ± 0.60 c f | 252.5 ± 0.76 c f | 39.83 ± 0.60 c f | 46.17 ± 1.01 c f | 35.33 ± 0.88 c f |
| GP V | 101 ± 0.856 c f | 172.8 ± 0.70 c f | 40.17 ± 0.60 c f | 43 ± 0.577 c f | 26.5 ± 0.76 c f |
| GP VI | 134.7 ± 0.76 c f | 255.3 ± 0.76 c f | 35.5 ± 0.86 b e | 55.33 ± 0.88 c f | 34.5 ± 0.78 c f |
| GP VII | 96.33 ± 0.6 c f | 166.2 ± 1.04 c f | 42.33 ± 0.61 c f | 40.67 ± 0.77 c f | 26 ± 0.577 c f |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Nagaraja, S.; Ahmed, S.S.; D. R., B.; Goudanavar, P.; M., R.K.; Fattepur, S.; Meravanige, G.; Shariff, A.; Shiroorkar, P.N.; Habeebuddin, M.; et al. Green Synthesis and Characterization of Silver Nanoparticles of Psidium guajava Leaf Extract and Evaluation for Its Antidiabetic Activity. Molecules 2022, 27, 4336. https://doi.org/10.3390/molecules27144336
Nagaraja S, Ahmed SS, D. R. B, Goudanavar P, M. RK, Fattepur S, Meravanige G, Shariff A, Shiroorkar PN, Habeebuddin M, et al. Green Synthesis and Characterization of Silver Nanoparticles of Psidium guajava Leaf Extract and Evaluation for Its Antidiabetic Activity. Molecules. 2022; 27(14):4336. https://doi.org/10.3390/molecules27144336
Chicago/Turabian StyleNagaraja, Sreeharsha, Syed Sagheer Ahmed, Bharathi D. R., Prakash Goudanavar, Rupesh Kumar M., Santosh Fattepur, Girish Meravanige, Arshia Shariff, Predeepkumar Narayanappa Shiroorkar, Mohammed Habeebuddin, and et al. 2022. "Green Synthesis and Characterization of Silver Nanoparticles of Psidium guajava Leaf Extract and Evaluation for Its Antidiabetic Activity" Molecules 27, no. 14: 4336. https://doi.org/10.3390/molecules27144336