From Wet Mount to Nucleic Acid Amplification Techniques: Current Diagnostic Methods and Future Perspectives Based on Patenting of New Assays, Stains, and Diagnostic Images for Trichomonas vaginalis Detection
Abstract
:1. Introduction
2. Methods
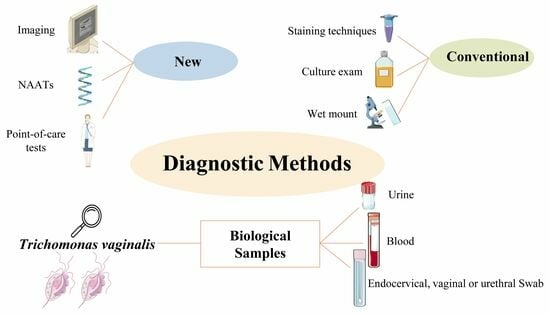
3. Consolidated Methods for Trichomoniasis Diagnosis
3.1. Wet Mount
3.2. Staining Techniques
3.3. Culture Exam
3.4. Point-of-Care Tests
3.5. Molecular Based Methods
4. Clinical Trials
5. Patents
5.1. Staining Technique
5.2. Culture Exam
5.3. Nucleic Acid Amplification Techniques—NAATs
5.4. Biomarker Tests
5.5. Novel Approaches
5.5.1. Devices of Images
5.5.2. Other Devices
| Database | Detects | Sample/Technique | Region of Deposit | Date of Deposit (Date Month Year) | Inventors | Publication Number |
|---|---|---|---|---|---|---|
| INPI CIPO UPSTO LATIPAT AUSPAT CPO | Candida albicans Trichomonas vaginalis Bacterial vaginosis | Urogenital secretion, urine/Multiplex nucleic acid-based detection in a sample | BR CA USA LA AU CN | 20.04.2016 15.01.2016 11.10.2018 27.04.2023 20.04.2016 08.07.2021 | [54,55,56] | BR1120170223791A2CA2982467 US20180291431A1 ES2939810 AU2016252551 US20217370923A |
| ESPACENET CPO | T. vaginalis | Blood/Staining | EU CN | 21.12.2017 | [51] | RU2639452C1 RU2017109830A |
| ESPACENET CPO | T. vaginalis | Urogenital secretion/Culture and staining | EU CN | 10.06.2015 | [52] | RU2552320C1 |
| ESPACENET CPO | T. vaginalis | New medium culture | EU CN | 21.04.2015 | [53] | UA103506U UAU201503787U |
| ESPACENET CPO | T. vaginalis | Samples of men/Polyclonal antibodies, TvMP50 * | EU CN | 13.05.2013 | [73,74] | MX2012000112W WO2013070056A1 |
| ESPACENET | T. vaginalis | Biological sample/LAMP amplification | EU | 09.08.2017 | [62] | CN107142327A |
| ESPACENET | T. vaginalis | Urine/Nested PCR | EU | 30.04.2014 | [61] | CN103757108A |
| ESPACENET | T. vaginalis | Biological samples/Diagnosis tests based on nucleotide sequences (TvCP39) | EU | 29.01.2013 | [75] | MX2011007531A |
| ESPACENET | T. vaginalis | Trichocystatin 2 protein * | EU | 29.02.2016 | [76] | MX2014010400A |
| ESPACENET | T. vaginalis | TvCP4 * | EU | 01.12.2014 | [77] | MX2013006126A |
| ESPACENET CPO | T. vaginalis | PFOR * | EU CN | 26.04.2013 27.10.2011 | [80] | MX2011011361A |
| CIPO USPTO | T. vaginalis | Endocervical, vaginal, and urethral swab sample/PCR Presence or absence of the TV 40S ribosomal protein (Tv40Srp) gene or RNA in the sample | CA USA | 19.12.201629.06.2017 | [63,64] | CA2953006 US20170183746A1 |
| CIPO USPTO | T. vaginalis | Biological or non-biological sample/Multiplex detection by PCR | CA USA | 30.11.201730.11.2017 | [59,60] | CA3025585 US20170342508A1 |
| CIPO USPTO | T. vaginalis | Biological sample/An amplification oligonucleotide for use in amplifying a target nucleic acid sequence | CA USA | 07.01.202129.09.2022 | [66,67] | CA3144452 US20220307093A1 |
| CIPO USPTO | T. vaginalis Chlamydia trachomatis Neisseria gonorrhoeae Mycoplasma | Biological sample/ Combinations of forward oligonucleotide primers, reverse oligonucleotide primers, and oligonucleotide probes | CA USA | 31.12.2018 | [57,58] | CA3088866 US20190211379A1 |
| KIPRIS | Agents causing vaginitis | Biological sample/Device with a PCR unit | ROK | 02.09.2017 | [65] | 1020150102826 |
| USPTO CPO | T. vaginalis | Urine/Urine specimen analyzer with a detector and an analysis unit | USA CN | 24.08.2023 30.08.2023 | [82] | US20230266298A1 JP2022024062A |
| USPTO | T. vaginalis M. genitalium | Biological samples/Multiplex detection of nucleic acids using mixed reporters | USA | 13.07.2023 | [68] | US20230220463A1 |
| USPTO | Visual indication of infection in vaginitis | A personal care product with an indicator strip that contains an amine-sensitive dye | USA | 27.03.2014 | [85] | US20140087417A1 |
| USPTO | STIs | Biological sample/Method that generates a diagnosis based on the detected set of microbiome targets | USA | 30.06.2016 | [69] | US20170002432A1 |
| USPTO | T. vaginalis Treponema spp. Neisseria spp. | Vaginal fluid or washing, or semen or prostatic fluid/Uses an SOE specific for highly immunogenic regions of proteins from pathogens | USA | 23.05.2019 | [86] | US20190154689A1 |
| USPTO | STIs HPV | Any sample/NGS | USA | 10.12.2020 | [70] | US20200385821A1 |
| USPTO | Motile objects | Fluid sample/Imaging platform | USA | 02.12.2021 | [83] | US20210374381A1 |
| USPTO | Motile pathogen | Fluid sample/Microfluidic imager | USA | 23.12.2021 | [84] | US20210398296A1 |
| USPTO | STIs | Urine/LAMP | USA | 25.05.2023 | [71] | US20230160021A1 |
| AUSPAT CPO | T. vaginalis | Biological sample/PCR AP65-1 gene * | AU CN | 29.06.2016 21.12.2011 | [81] | ES2575538 EP10701589A |
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Rowley, J.; Vander Hoorn, S.; Korenromp, E.; Low, N.; Unemo, M.; Abu-Raddad, L.J.; Chico, R.M.; Smolak, A.; Newman, L.; Gottlieb, S.; et al. Chlamydia, gonorrhoea, trichomoniasis and syphilis: Global prevalence and incidence estimates, 2016. Bull. World Health Organ. 2019, 97, 548–562. [Google Scholar] [CrossRef]
- Eleutério, J., Jr.; Campaner, A.B.; de Carvalho, N.S. Diagnosis and treatment of infectious vaginitis: Proposal for a new algorithm. Front. Med. 2023, 10, 1040072. [Google Scholar] [CrossRef] [PubMed]
- Yang, H.Y.; Su, R.Y.; Chung, C.H.; Huang, K.Y.; Lin, H.A.; Wang, J.Y.; Chen, C.-C.; Chien, W.-C.; Lin, H.-C. Association between trichomoniasis and prostate and bladder diseases: A population-based case-control study. Sci. Rep. 2022, 12, 15358. [Google Scholar] [CrossRef] [PubMed]
- Menezes, C.B.; Frasson, A.P.; Tasca, T. Trichomoniasis—Are we giving the deserved attention to the most common non-viral sexually transmitted disease worldwide? Microb. Cell 2016, 3, 404–419. [Google Scholar] [CrossRef] [PubMed]
- Masha, S.C.; Cools, P.; Sanders, E.J.; Vaneechoutte, M.; Crucitti, T. Trichomonas vaginalis and HIV infection acquisition: A systematic review and meta-analysis. Sex. Transm. Infect. 2019, 95, 36–42. [Google Scholar] [CrossRef] [PubMed]
- Mavedzenge, S.N.; Pol, B.V.; Cheng, H.; Montgomery, E.T.; Blanchard, K.; de Bruyn, G.; Ramjee, G.; Straten, A. Epidemiological synergy of Trichomonas vaginalis and HIV in Zimbabwean and South African women. Sex. Transm. Dis. 2010, 37, 460–466. [Google Scholar] [CrossRef] [PubMed]
- Workowski, K.A.; Bachmann, L.H.; Chan, P.A.; Johnston, C.M.; Muzny, C.A.; Park, I.; Reno, H.; Zenilman, J.M.; Bolan, G.A. Sexually Transmitted Infections Treatment Guidelines, 2021. MMWR Recomm. Rep. 2021, 70, 1–187. [Google Scholar] [PubMed]
- Ghosh, A.P.; Aycock, C.; Schwebke, J.R. In Vitro Study of the Susceptibility of Clinical Isolates of Trichomonas vaginalis to Metronidazole and Secnidazole. Antimicrob. Agents Chemother. 2018, 62, e02329-17. [Google Scholar] [CrossRef] [PubMed]
- Alessio, C.; Nyirjesy, P. Management of Resistant Trichomoniasis. Curr. Infect. Dis. Rep. 2019, 21, 31. [Google Scholar] [CrossRef]
- Mtshali, A.; Ngcapu, S.; Govender, K.; Sturm, A.W.; Moodley, P.; Joubert, B.C. In Vitro Effect of 5-Nitroimidazole Drugs against Trichomonas vaginalis Clinical Isolates. Microbiol. Spectr. 2022, 10, e0091222. [Google Scholar] [CrossRef]
- Secor, W.E.; Meites, E.; Starr, M.C.; Workowski, K.A. Neglected parasitic infections in the United States: Trichomoniasis. Am. J. Trop. Med. Hyg. 2014, 90, 800–804. [Google Scholar] [CrossRef]
- Kumar, S.; Chesson, H.; Gift, T.L. Estimating the Direct Medical Outpatient Costs of Diagnosis and Treatment of Trichomoniasis Among Commercially Insured Patients in the United States, 2016 to 2018. Sex. Transm. Dis. 2021, 48, e45–e47. [Google Scholar] [CrossRef] [PubMed]
- Chesson, H.W.; Blandford, J.M.; Pinkerton, S.D. Estimates of the annual number and cost of new HIV infections among women attributable to trichomoniasis in the United States. Sex. Transm. Dis. 2004, 31, 547–551. [Google Scholar] [CrossRef] [PubMed]
- Nathan, B.; Appiah, J.; Saunders, P.; Heron, D.; Nichols, T.; Brum, R.; Alexander, S.; Baraitser, P.; Ison, C. Microscopy outperformed in a comparison of five methods for detecting Trichomonas vaginalis in symptomatic women. Int. J. STD AIDS 2015, 26, 251–256. [Google Scholar] [CrossRef] [PubMed]
- Diamond, L.S. The establishment of various trichomonads of animals and man in axenic cultures. J. Parasitol. 1957, 43, 488–490. [Google Scholar] [CrossRef]
- Menezes, C.B.; Mello, M.D.S.; Tasca, T. Comparison of permanent staining methods for the laboratory diagnosis of trichomoniasis. Rev. Inst. Med. Trop. Sao Paulo 2016, 58, 5. [Google Scholar] [CrossRef] [PubMed]
- Huppert, J.S.; Mortensen, J.E.; Reed, J.L.; Kahn, J.A.; Rich, K.D.; Miller, W.C.; Hobbs, M.M. Rapid antigen testing compares favorably with transcription-mediated amplification assay for the detection of Trichomonas vaginalis in young women. Clin. Infect. Dis. 2007, 45, 194–198. [Google Scholar] [CrossRef] [PubMed]
- Gaydos, C.A.; Klausner, J.D.; Pai, N.P.; Kelly, H.; Coltart, C.; Peeling, R.W. Rapid and point-of-care tests for the diagnosis of Trichomonas vaginalis in women and men. Sex. Transm. Infect. 2017, 93, S31–S35. [Google Scholar] [CrossRef]
- Butler, S.E.; Augostini, P.; Secor, W.E. Mycoplasma hominis infection of Trichomonas vaginalis is not associated with metronidazole-resistant trichomoniasis in clinical isolates from the United States. Parasitol. Res. 2010, 107, 1023–1027. [Google Scholar] [CrossRef]
- Becker, D.L.; dos Santos, O.; Frasson, A.P.; de Vargas Rigo, G.; Macedo, A.J.; Tasca, T. High rates of double-stranded RNA viruses and Mycoplasma hominis in Trichomonas vaginalis clinical isolates in South Brazil. Infect. Genet. Evol. 2015, 34, 181–187. [Google Scholar] [CrossRef]
- Nye, M.B.; Schwebke, J.R.; Body, B.A. Comparison of APTIMA Trichomonas vaginalis transcription-mediated amplification to wet mount microscopy, culture, and polymerase chain reaction for diagnosis of trichomoniasis in men and women. Am. J. Obstet. Gynecol. 2009, 200, 188.e1–188.e7. [Google Scholar] [CrossRef]
- Van Der Pol, B.; Williams, J.A.; Taylor, S.N.; Cammarata, C.L.; Rivers, C.A.; Body, B.A.; Nye, M.; Fuller, D.; Schwebke, J.R.; Barnes, M.; et al. Detection of Trichomonas vaginalis DNA by use of self-obtained vaginal swabs with the BD ProbeTec Qx assay on the BD Viper system. J. Clin. Microbiol. 2014, 52, 885–889. [Google Scholar] [CrossRef]
- Kissinger, P. Trichomonas vaginalis: A review of epidemiologic, clinical and treatment issues. BMC Infect. Dis. 2015, 15, 307. [Google Scholar] [CrossRef]
- Van Der Pol, B. Clinical and Laboratory Testing for Trichomonas vaginalis Infection. J. Clin. Microbiol. 2016, 54, 7–12. [Google Scholar] [CrossRef]
- Nabweyambo, S.; Kakaire, O.; Sowinski, S.; Okeng, A.; Ojiambo, H.; Kimeze, J.; Najjingo, I.; Bwanga, F. Very low sensitivity of wet mount microscopy compared to PCR against culture in the diagnosis of vaginal trichomoniasis in Uganda: A cross sectional study. BMC Res. Notes 2017, 10, 259. [Google Scholar] [CrossRef]
- Ismail, K.A.; Hagag, H.M.; Alam-Eldin, Y.H.; Mahmoud, M.K.; Abdulaziz, A.M.; Khalifa, A.M.; Khalifa, O.M. Perinuclear halo indicate Trichomonas vaginalis in Pap smear. Arch. Biotechnol. Biomed. 2019, 3, 001–005. [Google Scholar]
- Centers for Disease Control and Prevention. Available online: https://www.cdc.gov/std/treatment-guidelines/trichomoniasis.htm (accessed on 15 September 2023).
- Hobbs, M.M.; Seña, A.C. Modern diagnosis of Trichomonas vaginalis infection. Sex. Transm. Infect. 2013, 89, 434–438. [Google Scholar] [CrossRef]
- Patil, M.J.; Nagamoti, J.M.; Metgud, S.C. Diagnosis of Trichomonas vaginalis from Vaginal Specimens by Wet Mount Microscopy, In Pouch TV Culture System, and PCR. J. Glob. Infect. Dis. 2012, 4, 22–25. [Google Scholar] [CrossRef] [PubMed]
- Campbell, L.; Woods, V.; Lloyd, T.; Elsayed, S.; Church, D.L. Evaluation of the OSOM Trichomonas rapid test versus wet preparation examination for detection of Trichomonas vaginalis vaginitis in specimens from women with a low prevalence of infection. J. Clin. Microbiol. 2008, 46, 3467–3469. [Google Scholar] [CrossRef] [PubMed]
- Hegazy, M.M.; El-Tantawy, N.L.; Soliman, M.M.; El-Sadeek, E.S.; El-Nagar, H.S. Performance of rapid immunochromatographic assay in the diagnosis of Trichomoniasis vaginalis. Diagn. Microbiol. Infect. Dis. 2012, 74, 49–53. [Google Scholar] [CrossRef] [PubMed]
- A Validation Study of Genzyme Diagnostics OSOM Trichomonas Rapid Test and BVBlue Test. Available online: https://clinicaltrials.gov/study/NCT00682851?cond=NCT00682851&rank=1 (accessed on 22 September 2023).
- Dessai, F.; Nyirenda, M.; Sebitloane, M.; Abbai, N. Diagnostic evaluation of the BD Affirm VPIII assay as a point-of-care test for the diagnosis of bacterial vaginosis, trichomoniasis and candidiasis. Int. J. STD AIDS 2020, 31, 303–311. [Google Scholar] [CrossRef]
- Adamson, P.C.; Loeffelholz, M.J.; Klausner, J.D. Point-of-Care Testing for Sexually Transmitted Infections: A Review of Recent Developments. Arch. Pathol. Lab. Med. 2020, 144, 1344–1351. [Google Scholar] [CrossRef]
- Abou Tayoun, A.N.; Burchard, P.R.; Caliendo, A.M.; Scherer, A.; Tsongalis, G.J. A multiplex PCR assay for the simultaneous detection of Chlamydia trachomatis, Neisseria gonorrhoeae, and Trichomonas vaginalis. Exp. Mol. Pathol. 2015, 98, 214–218. [Google Scholar] [CrossRef]
- Van Der Pol, B.; Torres-Chavolla, E.; Kodsi, S.; Cooper, C.K.; Davis, T.E.; Fife, K.H.; Taylor, S.N.; Augenbraun, M.H.; Gaydos, C.A. Clinical Performance of the BD CTGCTV2 Assay for the BD MAX System for Detection of Chlamydia trachomatis, Neisseria gonorrhoeae, and Trichomonas vaginalis Infections. Sex. Transm. Dis. 2021, 48, 134–140. [Google Scholar] [CrossRef]
- Schwebke, J.R.; Gaydos, C.A.; Nyirjesy, P.; Paradis, S.; Kodsi, S.; Cooper, C.K. Diagnostic Performance of a Molecular Test versus Clinician Assessment of Vaginitis. J. Clin. Microbiol. 2018, 56, e00252-18. [Google Scholar] [CrossRef]
- Vieira-Baptista, P.; Silva, A.R.; Costa, M.; Aguiar, T.; Saldanha, C.; Sousa, C. Clinical validation of a new molecular test (Seegene Allplex™ Vaginitis) for the diagnosis of vaginitis: A cross-sectional study. BJOG Int. J. Obstet. Gynaecol. 2021, 128, 1344–1352. [Google Scholar] [CrossRef]
- de Salazar, A.; Espadafor, B.; Fuentes-López, A.; Barrientos-Durán, A.; Salvador, L.; Álvarez, M.; García, F. Comparison between Aptima Assays (Hologic) and the Allplex STI Essential Assay (Seegene) for the diagnosis of Sexually transmitted infections. PLoS ONE 2019, 14, e0222439. [Google Scholar] [CrossRef]
- Chapin, K.; Andrea, S. APTIMA® Trichomonas vaginalis, a transcription-mediated amplification assay for detection of Trichomonas vaginalis in urogenital specimens. Expert. Rev. Mol. Diagn. 2011, 11, 679–688. [Google Scholar] [CrossRef] [PubMed]
- Schwebke, J.R.; Hobbs, M.M.; Taylor, S.N.; Sena, A.C.; Catania, M.G.; Weinbaum, B.S.; Gaydos, C.A. Molecular testing for Trichomonas vaginalis in women: Results from a prospective US clinical trial. J. Clin. Microbiol. 2011, 49, 4106–4111. [Google Scholar] [CrossRef] [PubMed]
- Caza, M.; Charles, M.; Locher, K.; Hoang, L.; Tucker, M.; Mandy, J.; Jewsbury, H.; Wilmer, A. Evaluation of the Aptima BV and CV/TV assays compared to conventional laboratory based testing methods for the diagnosis of vaginitis. Diagn. Microbiol. Infect. Dis. 2023, 106, 115953. [Google Scholar] [CrossRef] [PubMed]
- Schwebke, J.R.; Gaydos, C.A.; Davis, T.; Marrazzo, J.; Furgerson, D.; Taylor, S.N.; Smith, B.; Bachmann, L.H.; Ackerman, R.; Spurrell, T.; et al. Clinical Evaluation of the Cepheid Xpert TV Assay for Detection of Trichomonas vaginalis with Prospectively Collected Specimens from Men and Women. J. Clin. Microbiol. 2018, 56, e01091-17. [Google Scholar] [CrossRef] [PubMed]
- Notomi, T.; Okayama, H.; Masubuchi, H.; Yonekawa, T.; Watanabe, K.; Amino, N.; Hase, T. Loop-mediated isothermal amplification of DNA. Nucleic Acids Res. 2000, 28, E63. [Google Scholar] [CrossRef] [PubMed]
- Li, Y.; Wang, S.; Li, H.; Song, X.; Zhang, H.; Duan, Y.; Luo, C.; Wang, B.; Ji, S.; Xie, Q.; et al. Development of a convenient detection method for Trichomonas vaginalis based on loop-mediated isothermal amplification targeting adhesion protein 65. BMC Infect. Dis. 2020, 20, 319. [Google Scholar] [CrossRef] [PubMed]
- Clinical Study of a Single-Use, Point-of-Care Molecular Diagnostic Device for the Detection of Neisseria gonorrhoeae (NG), Trichomonas vaginalis (TV), and Chlamydia trachomatis (CT) Utilizing Vaginal Swabs. Available online: https://clinicaltrials.gov/study/NCT03596151?cond=NCT03596151&rank=1 (accessed on 22 September 2023).
- Solana™ Trichomonas Assay Field Study. Available online: https://clinicaltrials.gov/study/NCT02566447?cond=NCT02566447&rank=1 (accessed on 22 September 2023).
- Prospective Collection of Female Specimens for Testing with Gen-Probe APTIMA (Registered Trademark) Assays. Available online: https://clinicaltrials.gov/study/NCT01728103?cond=NCT01728103&rank=1 (accessed on 22 September 2023).
- Comparing NAAT Testing to Standard Methods for the Diagnosis of Vaginitis (VAST). Available online: https://clinicaltrials.gov/study/NCT02203942?cond=%20NCT02203942&rank=1 (accessed on 22 September 2023).
- Validity of Patient-Collected Wet Mounts. Available online: https://clinicaltrials.gov/study/NCT02641717?cond=NCT02641717&rank=1 (accessed on 22 September 2023).
- Diagnostic Technique for Urogenital Trichomoniais. Available online: https://worldwide.espacenet.com/patent/search/family/063857258/publication/RU2639452C1?q=RU2639452C1 (accessed on 22 September 2023).
- Diagnostic Technique for Urogenital Trichomoniais. Available online: https://worldwide.espacenet.com/patent/search/family/053294884/publication/RU2552320C1?q=RU2552320C1 (accessed on 22 September 2023).
- Liquid Medium for the Diagnosis of Trichomoniasis “SKM-1-U”. Available online: https://worldwide.espacenet.com/patent/search/family/055172028/publication/UA103506U?q=UA103506U (accessed on 22 September 2023).
- Detecção Multiplex da Candidíase Vulvovaginal, Tricomoníase e Vaginose Bacteriana. Available online: https://busca.inpi.gov.br/pePI/servlet/PatenteServletController?Action=detail&CodPedido=1433346&SearchParameter=1120170223791%20%20%20%20%20%20&Resumo=&Titulo= (accessed on 22 September 2023).
- Multiplex Detection of Vulvovaginal Candidiasis, Trichomoniasis and Bacterial Vaginosis. Available online: https://www.ic.gc.ca/opic-cipo/cpd/eng/patent/2982467/summary.html?type=number_search&tabs1Index=tabs1_1 (accessed on 22 September 2023).
- Multiplex Detection of Vulvovaginal Candidiasis, Trichomoniasis and Bacterial Vaginosis (20180291431). Available online: https://ppubs.uspto.gov/pubwebapp/static/pages/ppubsbasic.html (accessed on 22 September 2023).
- Assay for Detecting Chlamydia trachomatis, Neisseria gonorrhoeae, Trichomonas vaginalis, and Mycoplasma genitalium. Available online: https://www.ic.gc.ca/opic-cipo/cpd/eng/patent/3088866/summary.html?query=ASSAY+FOR+DETECTING+CHLAMYDIA+TRACHOMATIS%2C+NEISSERIA+GONORRHOEAE%2C+TRICHOMONAS+VAGINALIS%2C+AND+MYCOPLASMA+GENITALIUM&type=basic_search (accessed on 22 September 2023).
- Assay for Detecting Chlamydia trachomatis, Neisseria gonorrhoeae, Trichomonas vaginalis, and Mycoplasma genitalium (20190211379). Available online: https://ppubs.uspto.gov/pubwebapp/static/pages/ppubsbasic.html (accessed on 22 September 2023).
- Compositions and Methods for Detection of Trichomonas vaginalis. Available online: https://www.ic.gc.ca/opic-cipo/cpd/eng/patent/3025585/summary.html?query=COMPOSITIONS+AND+METHODS+FOR+DETECTION+OF+TRICHOMONAS+VAGINALIS&type=basic_search (accessed on 22 September 2023).
- Compositions and Methods for Detection of Trichomonas vaginalis (20170342508). Available online: https://ppubs.uspto.gov/pubwebapp/static/pages/ppubsbasic.html (accessed on 22 September 2023).
- Specific Trichomonas vaginalis Nested PCR (Polymerase Chain Reaction) Detection Kit. Available online: https://worldwide.espacenet.com/patent/search/family/050524423/publication/CN103757108A?q=CN103757108A (accessed on 22 September 2023).
- Primer Composition, Application Thereof, Trichomonas vaginalis Detection Kit. Available online: https://worldwide.espacenet.com/patent/search/family/059785450/publication/CN107142327A?q=CN107142327A (accessed on 22 September 2023).
- Methods of Detecting Trichomonas vaginalis. Available online: https://www.ic.gc.ca/opic-cipo/cpd/eng/patent/2953006/summary.html?query=METHODS+OF+DETECTING+TRICHOMONAS+VAGINALIS&type=basic_search (accessed on 22 September 2023).
- Methods of Detecting Trichomonas vaginalis (20170183746). Available online: https://ppubs.uspto.gov/pubwebapp/static/pages/ppubsbasic.html (accessed on 22 September 2023).
- Diagnostic Kit for Diagnosing Vaginitis (1020150102826). Available online: http://engpat.kipris.or.kr/engpat/biblioa.do?method=biblioFrame (accessed on 22 September 2023).
- Oligonucleotides for Use in Determining the Presence of Trichomonas vaginalis in a Sample. Available online: https://www.ic.gc.ca/opic-cipo/cpd/eng/patent/3144452/summary.html?query=OLIGONUCLEOTIDES+FOR+USE+IN+DETERMINING+THE+PRESENCE+OF+TRICHOMONAS+VAGINALIS+IN+A+SAMPLE&type=basic_search (accessed on 22 September 2023).
- Oligonucleotides for Use in Determining the Presence of Trichomonas vaginalis in a Sample (20220307093). Available online: https://ppubs.uspto.gov/pubwebapp/static/pages/ppubsbasic.html (accessed on 22 September 2023).
- Multiplex Detection of Nucleic Acids Using Mixed Reporters (20230220463). Available online: https://ppubs.uspto.gov/pubwebapp/static/pages/ppubsbasic.html (accessed on 22 September 2023).
- Method and System for Diagnostic Testing (20170002432). Available online: https://ppubs.uspto.gov/pubwebapp/static/pages/ppubsbasic.html (accessed on 22 September 2023).
- Methods and Compositions for Human Papillomaviruses and Sexually Transmitted Infections Detection, Identification and Quantification (20200385821). Available online: https://ppubs.uspto.gov/pubwebapp/static/pages/ppubsbasic.html (accessed on 22 September 2023).
- Method for Detection of a Sexually Transmitted Infectious Pathogen (20230160021). Available online: https://ppubs.uspto.gov/pubwebapp/static/pages/ppubsbasic.html (accessed on 22 September 2023).
- Arroyo, R.; Cárdenas-Guerra, R.E.; Figueroa-Angulo, E.E.; Puente-Rivera, J.; Zamudio-Prieto, O.; Ortega-López, J. Trichomonas vaginalis Cysteine Proteinases: Iron Response in Gene Expression and Proteolytic Activity. BioMed Res. Int. 2015, 2015, 946787. [Google Scholar] [CrossRef]
- Production of Anti TvMP50r Polyclonal Antibodies That Can Be Used in the Diagnosis of Trichomonas vaginalis in Men. Available online: https://worldwide.espacenet.com/patent/search/family/048290344/publication/WO2013070055A1?q=MX2012000112W (accessed on 22 September 2023).
- Production of a Low-Molecular-Weight Recombinant Metalloproteinase (50kDA) of Trichomonas vaginalis and Identification of the Gene That Codes for Said Low-Molecular-Weight Metalloproteinase (50kDA) That Is Expressed Differentially in the Presence of Zn+2. Available online: https://worldwide.espacenet.com/patent/search/family/048290345/publication/WO2013070056A1?q=WO2013070056A1 (accessed on 22 September 2023).
- Diagnosis and Therapeutic Methods for Treating Trichomonas vaginalis Infection by Protein TVCP29. Available online: https://worldwide.espacenet.com/patent/search/family/048195103/publication/MX2011007531A?q=MX2011007531A (accessed on 22 September 2023).
- Trichosystatin-2 (TC-2) a Cysteine Proteinase Inhibitor TVCP39 of Trichomonas vaginalis. Available online: https://worldwide.espacenet.com/patent/search/family/055959529/publication/MX2014010400A?q=MX2014010400A (accessed on 22 September 2023).
- Cysteine Proteinase TvCP4 as Therapeutic and Diagnosis Target of Virulence in Infection by Trichomonas vaginalis. Available online: https://worldwide.espacenet.com/patent/search/family/052824735/publication/MX2013006126A?q=MX2013006126A (accessed on 22 September 2023).
- Diagnosis of Trichomonosis and Determination of Isolated Virulence of the Trichomonas vaginalis Parasite through the Quantitative Analysis of the Proteinase Cysteine 2, TvCP2. Available online: https://worldwide.espacenet.com/patent/search/family/066823418/publication/MX2017013824A?q=MX2017013824A (accessed on 22 September 2023).
- Graves, K.J.; Novak, J.; Secor, W.E.; Kissinger, P.J.; Schwebke, J.R.; Muzny, C.A. A systematic review of the literature on mechanisms of 5-nitroimidazole resistance in Trichomonas vaginalis. Parasitology 2020, 147, 1383–1391. [Google Scholar] [CrossRef]
- Pyruvate-Ferredoxin Oxidoreductase (PFO) Adhesine Protein as a Target for Inhibiting the Adherence of Trichomonas vaginalis and as a Diagnosis and Vaccinal Target for Trichomoniasis. Available online: https://worldwide.espacenet.com/patent/search/family/048741720/publication/MX2011011361A?q=MX2011011361A (accessed on 22 September 2023).
- Assay for Trichomonas vaginalis by Amplification and Detection of Trichomonas vaginalis AP65-1 Gene. Available online: https://pss-system.cponline.cnipa.gov.cn/documents/detail?prevPageTit=changgui (accessed on 22 February 2024).
- Urine Specimen Analysis Method and Urine Specimen Analyzer (20230266298). Available online: https://ppubs.uspto.gov/pubwebapp/static/pages/ppubsbasic.html (accessed on 22 September 2023).
- Device and Method for Motility-Based Label-Free Detection of Motile Objects in a Fluid Sample (20210374381). Available online: https://ppubs.uspto.gov/pubwebapp/static/pages/ppubsbasic.html (accessed on 22 September 2023).
- Motion Based Pathogen Detection Using a Fluidic Imager (20210398296). Available online: https://ppubs.uspto.gov/pubwebapp/static/pages/ppubsbasic.html (accessed on 22 September 2023).
- Personal Care Products with Visual Indicator of Vaginitis (20140087417). Available online: https://ppubs.uspto.gov/pubwebapp/static/pages/ppubsbasic.html (accessed on 22 September 2023).
- Strings of Epitopes Useful in Diagnosing and Eliciting Immune Responses to Sexually Transmitted Infection (20190154689). Available online: https://ppubs.uspto.gov/pubwebapp/static/pages/ppubsbasic.html (accessed on 22 September 2023).

| Assay | Equipment Requirements | Sample Type | Cost 1 | Relative Sensitivity 2 |
|---|---|---|---|---|
| Wet mount | Microscope | vaginal and endocervical swabs, urine sediment | $ | + |
| Staining method | Microscope | vaginal and endocervical swabs, urine sediment | $ | ++ |
| Culture | Incubator, microscope | vaginal and endocervical swabs, urine sediment | $$ | ++ |
| Sorology (antigen)—OSOM® | None | vaginal and endocervical swabs | $$ | +++ |
| Nucleic acid test (NAAT)—Affirm VPIII® | Affirm VPIII instrument | vaginal and endocervical swabs | $$ | ++ |
| Nucleic acid test (NAAT)—Hologic Aptima TV® 3 | Tigris or Panther automated system | endocervical swabs, vaginal swabs, endocervical specimens collected in PreservCyt(®) (Thin Prep, Hologic Incorporated, MA, USA) solution and female urine specimens | $$$ | +++ |
| Nucleic acid test—Solana Trichomonas Assay® (Quidel) 4 | Solana’s platform | vaginal swabs and urine specimens | $$ | +++ |
| Nucleic acid test (PCR) Max CTGCTV2 assay® (Becton Dickinson) 5 | Benchtop instrument, BD CTGCTV2 | vaginal swab specimens and male or female urine specimens | $$$ | +++ |
| Nucleic acid test (PCR)—Cepheid® 6 | GeneXpert Instrument | Vaginal and endocervical swabs, female or male urine sediment | $$$ | +++ |
| Nucleic acid test (PCR real time multiplex) The Allplex™ STI Essential assay | Seegene® 7 | vaginal and endocervical swabs, urine sediment | $$$ | +++ |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cardoso, F.G.; Freitas, M.D.; Tasca, T.; Rigo, G.V. From Wet Mount to Nucleic Acid Amplification Techniques: Current Diagnostic Methods and Future Perspectives Based on Patenting of New Assays, Stains, and Diagnostic Images for Trichomonas vaginalis Detection. Venereology 2024, 3, 35-50. https://doi.org/10.3390/venereology3010004
Cardoso FG, Freitas MD, Tasca T, Rigo GV. From Wet Mount to Nucleic Acid Amplification Techniques: Current Diagnostic Methods and Future Perspectives Based on Patenting of New Assays, Stains, and Diagnostic Images for Trichomonas vaginalis Detection. Venereology. 2024; 3(1):35-50. https://doi.org/10.3390/venereology3010004
Chicago/Turabian StyleCardoso, Fernanda Gomes, Mariana Dicki Freitas, Tiana Tasca, and Graziela Vargas Rigo. 2024. "From Wet Mount to Nucleic Acid Amplification Techniques: Current Diagnostic Methods and Future Perspectives Based on Patenting of New Assays, Stains, and Diagnostic Images for Trichomonas vaginalis Detection" Venereology 3, no. 1: 35-50. https://doi.org/10.3390/venereology3010004