Cryptosporidiosis in Reptiles from Brazil: An Update for Veterinary Medicine
Abstract
:1. Introduction
2. Cryptosporidium spp.
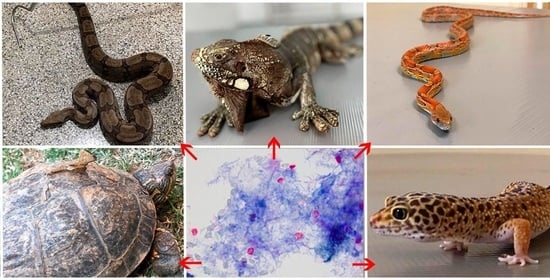
3. Cryptosporidium spp. in Reptiles
4. Cryptosporidium spp. in Reptiles from Brazil
5. Transmission
6. Diagnosis
7. Treatment and Control
8. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
References
- Uetz, P.; Freed, P.; Hošek, J. (Eds.) The Reptile Database. 2019. Available online: http://www.reptile-database.org/ (accessed on 1 April 2020).
- Costa and Bernils. Sociedade Brasileira De Herpetologia. Lista de Anfíbios e Répteis do Brasil. 2019. Available online: http://www.sbherpetologia.org.br/ (accessed on 15 July 2020).
- Barbosa, A.S.; Pinheiro, J.L.; dos Santos, C.R.; de Lima, C.S.C.C.; Dib, L.V.; Echarte, G.V.; Augusto, A.M.; Bastos, A.C.M.P.; Antunes Uchôa, C.M.; Bastos, O.M.P.; et al. Gastrointestinal Parasites in Captive Animals at the Rio de Janeiro Zoo. Acta Parasitol. 2020, 65, 237–249. [Google Scholar] [CrossRef] [PubMed]
- Reis, F.C.; Minuzzi-Souza, T.T.C.; Neiva, M.; Timbó, R.V.; Morais, I.O.B.; Lima, T.M.; Hecht, M.; Nitz, N.; Gurgel-Gonçalves, R. Trypanosomatid infections in captive wild mammals and potential vectors at the Brasilia Zoo, Federal District, Brazil. Vet. Med. Sci. 2019, 6, 248–256. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Brener, B.; Rique, A.A.; Diniz, A.L.; Millar, P.R. Parasitismo em serpentes. Med. Veterinária 2020, 14, 141–150. [Google Scholar] [CrossRef]
- Villar Echarte, G.; Da Silva Barbosa, A.; Pinheiro, J.L.; Segon, A.M.R.; Augusto, A.M.; Chenard, M.G.; Amendoeira, M.R.R. Toxoplasma gondii and other parasites studied in feline feces in zoos in Cuba and Brazil. Rev. De Patol. Trop./J. Trop. Pathol. 2020, 48, 211–221. [Google Scholar] [CrossRef]
- Ras-Norynska, M.; Sokól, R. Internal parasites of reptiles. Ann. Parasitol. 2015, 61, 115–117. [Google Scholar]
- Rataj, A.; Lindtner-Knific, R.; Vlahović, K.; Mavri, U.; Dovč, A. Parasites in pet reptiles. Acta Vet. Scand. 2011, 53, 33. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fonseca, É.; Solé, M.; Rödder, D.; de Marco, P. Pet snakes illegally marketed in Brazil: Climatic viability and establishment risk. PLoS ONE 2017, 12, e0183143. [Google Scholar] [CrossRef] [Green Version]
- Mani, I.; Maguire, J.H. Small animal zoonoses and immuncompromised pet owners. Top. Companion Anim. Med. 2009, 24, 164–174. [Google Scholar] [CrossRef]
- Chagas, C.R.F.; Gonzalez, I.H.L.; Salgado, P.A.B.; Rodrigues, B.; Ramos, P.L. Giardia spp.; ten years of parasitological data in the biggest zoo of Latin America. Ann. Parasitol. 2019, 65, 35–51. [Google Scholar] [PubMed]
- Graczyk, T.K.; Aguirre, A.A.; Ostfeld, R.S.; Tabor, G.M.; House, C.; Pearl, M.C. (Eds.) Zoonotic infections and conservation. In Conservation Medicine: Ecological Health in Practice; Oxford University Press: Oxford, UK, 2002; pp. 40–61. [Google Scholar]
- Grego, K.F.; Gardiner, C.H.; Catao-Dias, J.L. Comparative pathology of parasitic infections in free-ranging and captive pit vipers (Bothrops jararac). Vet. Rec. 2004, 154, 559–562. [Google Scholar] [CrossRef] [PubMed]
- Lallo, M.A.; Pereira, A.; Araújo, R.; Favorito, S.E.; Bertolla, P.; Bondan, E.F. Ocorrência de Giardia, Cryptosporidium e microsporídios em animais silvestres em área de desmatamento no Estado de São Paulo, Brasil. Ciência Rural. 2009, 39, 1465–1470. [Google Scholar] [CrossRef] [Green Version]
- Marenzoni, M.; Zicavo, A.; Veronesi, F. Microbiological and parasitological investigation on chelonians reared in Italian facilities. Vet. Ital. 2015, 51, 173–178. [Google Scholar] [CrossRef] [PubMed]
- Papini, R.; Manetti, C.; Mancianti, F. Coprological survey in pet reptiles in Italy. Vet. Rec. 2011, 169, 207. [Google Scholar] [CrossRef]
- Rinaldi, L.; Capasso, M.; Mihalca, A.D.; Cirillo, R.; Cringoli, G.; Cacciò, S. Prevalence and molecular identification of Cryptosporidium isolates from pet lizards and snakes in Italy. Parasite 2012, 19, 437–440. [Google Scholar] [CrossRef] [Green Version]
- Ryan, U. Cryptosporidium in birds, fish and amphibians. Exp. Parasitol. 2010, 124, 113–120. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ryan, U.; Xiao, L. Taxonomy and Molecular Taxonomy. In Cryptosporidium: Parasite and Disease; Cacciò, S.M., Widmer, G., Eds.; Springer: Vienna, Austria, 2014; pp. 3–41. [Google Scholar] [CrossRef]
- Santín, M. Clinical and subclinical infections with Cryptosporidium in animals. N. Z. Vet. J. 2013, 61, 1–10. [Google Scholar] [CrossRef]
- Cavalier-Smith, T. Gregarine site-heterogeneous 18S rDNA trees, revision of gregarine higher classification, and the evolutionary diversification of Sporozoa. Eur. J. Protistol. 2014, 50, 472–495. [Google Scholar] [CrossRef]
- Ryan, U.; Paparini, A.; Monis, P.; Hijjawi, N. It’s official—Cryptosporidium is a gregarine: What are the implications for the water industry? Water Res. 2016, 105, 305–313. [Google Scholar] [CrossRef] [Green Version]
- Bones, A.J.; Jossé, L.; More, C.; Miller, C.N.; Michaelis, M.; Tsaousis, A.D. Past and future trends of Cryptosporidium in vitro research. Exp. Parasitol. 2019, 196, 28–37. [Google Scholar] [CrossRef] [PubMed]
- Bogan, J.E. Gastric Cryptosporidiosis in Snakes, a Review. J. Herpetol. Med. Surg. 2019, 29, 71. [Google Scholar] [CrossRef]
- Feng, Y.; Xiao, L. Zoonotic Potential and Molecular Epidemiology of Giardia Species and Giardiasis. Clin. Microbiol. Rev. 2011, 24, 110–140. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Thompson, R.C.A.; Ash, A. Molecular epidemiology of Giardia and Cryptosporidium infections—What’s new? Infect. Genet. Evol. 2019, 75, 103951. [Google Scholar] [CrossRef]
- Xiao, L.; Ryan, U.M.; Graczyk, T.K.; Limor, J.; Li, L.; Kombert, M.; Junge, R.; Sulaiman, I.M.; Zhou, L.; Arrowood, M.J.; et al. Genetic Diversity of Cryptosporidium spp. in Captive Reptiles. Appl. Environ. Microbiol. 2004, 70, 891–899. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Šlapeta, J. DNA barcoding of Cryptosporidium. Parasitology 2018, 145, 574–584. [Google Scholar] [CrossRef]
- Karasawa, A.S.M.; da Silva, R.J.; Mascarini, L.M.; Barrella, T.H.; de Magalhães Lopes, C.A. Occurrence of Cryptosporidium (Apicomplexa, Cryptosporidiidae) in Crotalus durissus terrificus (Serpentes, Viperidae) in Brazil. Memórias Inst. Oswaldo Cruz 2002, 97, 779–781. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zahedi, A.; Paparini, A.; Jian, F.; Robertson, I.; Ryan, U. Public health significance of zoonotic Cryptosporidium species in wildlife: Critical insights into better drinking water management. Int. J. Parasitol. Parasites Wildl. 2016, 5, 88–109. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zahedi, A.; Ryan, U. Cryptosporidium–an update with an emphasis on foodborne and waterborne transmission. Res. Vet. Sci. 2020, 132, 500–512. [Google Scholar] [CrossRef]
- Cubas, Z.S.; Silva, J.C.R.; Catão Dias, J.L. Tratado de Animais Selvagens: Medicina Veterinária; Roca: Sao Paulo, Brazil, 2014; p. 207. [Google Scholar]
- Graczyk, T.K.; Cranfield, M.R.; Fayer, R. A comparative assessment of direct fluorescence antibody, modified acid-fast stain, and sucrose flotation techniques for detection of Cryptosporidium serpentis oocysts in snake fecal specimens. J. Zoo Wildl. Med. 1995, 26, 396–402. [Google Scholar]
- Gałęcki, R.; Sokół, R. Treatment of cryptosporidiosis in captive green iguanas (Iguana iguana). Vet. Parasitol. 2018, 252, 17–21. [Google Scholar] [CrossRef] [PubMed]
- Greiner, E.C.; Mader, D.R. Parasitology. In Reptile Medicine and Surgery, 2nd ed.; Mader, D.R., Ed.; Elsevier: St. Louis, MO, USA, 2006; p. 343364. [Google Scholar]
- Kik, M.J.; van Asten, A.J.; Lenstra, J.A.; Kirpensteijn, J. Cloaca prolapse and cystitis in green iguana (Iguana iguana) caused by a novel Cryptosporidium species. Vet. Parasitol. 2011, 175, 165–167. [Google Scholar] [CrossRef] [PubMed]
- Meireles, M.V. Cryptosporidium infection in Brazil: Implications for veterinary medicine and public health. Rev. Bras. Parasitol. Veterinária 2010, 19, 197–204. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- da Paixão Sevá, A.; Sercundes, M.K.; Martins, J.; de Souza, S.O.; da Cruz, J.B.; Lisboa, C.S.; Correa, S.H.R.; Soares, R.M. Occurrence and Molecular Diagnosis of Cryptosporidium serpentis in Captive Snakes in São Paulo, Brazil. J. Zoo Wildl. Med. 2011, 42, 326–329. [Google Scholar] [CrossRef] [PubMed]
- Ruggiero, P.C.; Zacariotti, R.L.; Bondan, E.F.; Lallo, M.A. Prevalence of Cryptosporidium serpentis in captive snakes. Ciência Rural. 2011, 41, 1975–1978. [Google Scholar] [CrossRef] [Green Version]
- Paiva, P.R.S.O.; Grego, K.F.; Lima, V.M.F.; Nakamura, A.A.; da Silva, D.C.; Meireles, M.V. Clinical, serological, and parasitological analysis of snakes naturally infected with Cryptosporidium serpentis. Vet. Parasitol. 2013, 198, 54–61. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- de Souza, J.L.; da Silva Barbosa, A.; Vazon, A.P.; Uchôa, C.M.A.; Nunes, B.C.; Cortez, M.B.V.; da Silva, V.L.; Más, L.B.; Melgarejo, A.R.; Bastos, O.M.P. Parasitological and immunological diagnoses from feces of captive-bred snakes at Vital Brazil Institute. Rev. Bras. Parasitol. Veterinária 2014, 23, 123–128. [Google Scholar] [CrossRef]
- da Silva, D.C.; Paiva, P.R.S.O.; Nakamura, A.A.; Homem, C.G.; de Souza, M.S.; Grego, K.F.; Meireles, M.V. The detection of Cryptosporidium serpentis in snake fecal samples by real-time PCR. Vet. Parasitol. 2014, 204, 134–138. [Google Scholar] [CrossRef]
- Graczyk, T.K.; Cranfield, M.R. Detection of Cryptosporidium-specific serum immunoglobulins in captive snakes by a polyclonal antibody in the indirect ELISA. Vet. Res. 1997, 28, 131–142. [Google Scholar]
- Fall, A.; Thompson, R.C.A.; Hobbs, R.P.; Morgan-Ryan, U. Morphology is not a reliable tool for delineating species within Cryptosporidium. J. Parasitol. 2003, 89, 399–402. [Google Scholar] [CrossRef]
- Appelbee, A.J.; Thompson, R.A.; Olson, M.E. Giardia and Cryptosporidium in mammalian wildlife—Current status and future needs. Trends Parasitol. 2005, 21, 370–376. [Google Scholar] [CrossRef]
- Gracenea, M.; Gomez, M.S.; Torres, J.; Carne, E.; Fernández-Morán, J. Transmission dynamics of Cryptosporidium in primates and herbivores at the Barcelona zoo: A long-term study. Vet. Parasitol. 2002, 104, 19–26. [Google Scholar] [CrossRef]
- Santos, H.L.C.; Rebello, K.M.; Bomfim, T.C.B. State of the Art and Future Directions of Cryptosporidium spp. In Parasitology and Microbiology Research; IntechOpen: London, UK, 2019. [Google Scholar]
- O’Leary, J.K.; Sleator, R.D.; Lucey, B. Cryptosporidium spp. diagnosis and research in the 21st century. Food Waterborne Parasitol. 2021, 24, e00131. [Google Scholar] [CrossRef] [PubMed]
- Pavlasek, I.; Ryan, U. Cryptosporidium varanii takes precedence over C. saurophilum. Exp. Parasitol. 2008, 118, 434–437. [Google Scholar] [CrossRef]
- Pedraza-Díaz, S.; Ortega-Mora, L.M.; Carrión, B.A.; Navarro, V.; Gómez-Bautista, M. Molecular characterisation of Cryptosporidium isolates from pet reptiles. Vet. Parasitol. 2009, 160, 204–210. [Google Scholar] [CrossRef] [PubMed]
- Feng, Y.; Ryan, U.M.; Xiao, L. Genetic Diversity and Population Structure of Cryptosporidium. Trends Parasitol. 2018, 34, 997–1011. [Google Scholar] [CrossRef] [PubMed]
- Xiao, L.; Fayer, R. Molecular characterisation of species and genotypes of Cryptosporidium and Giardia and assessment of zoonotic transmission. Int. J. Parasitol. 2008, 38, 1239–1255. [Google Scholar] [CrossRef]
- Samuel, W.M.; Pybus, M.J.; Kocan, A.A. Parasitic Diseases of Wild Mammals, 2nd ed.; Iowa State University Press: Ames, IA, USA, 2001. [Google Scholar]
- Plutzer, J.; Karanis, P. Molecular identification of a Cryptosporidium saurophilum from corn snake (Elaphe guttata guttata). Parasitol. Res. 2007, 101, 1141–1145. [Google Scholar] [CrossRef] [PubMed]
| Host | Locality | Diagnostic Technique | Species | Gene Target | Reference |
|---|---|---|---|---|---|
| Snakes | São Paulo | ME | Cryptosporidium spp. | NE | Karasawa et al. [29] |
| Snakes | São Paulo | ME, PCR | C. serpentis | 18S | Da Paixão Sevá et al. [38] |
| Snakes | São Paulo | ME, PCR | C. serpentis | 18S | Ruggiero et. al. [39] |
| Snakes | São Paulo | ME, PCR | C. serpentis | 18S | Paiva et. al. [40] |
| Snakes | Rio de Janeiro | ME, ELISA | Cryptosporidium spp. | NE | Souza et. al. [41] |
| Snakes | São Paulo | PCR, Real-time PCR | C. serpentis | 18S, HSP70 | da Silva et. al. [42] |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Brener, B.; Burgarelli, E.; Suarez, M.; Keidel, L. Cryptosporidiosis in Reptiles from Brazil: An Update for Veterinary Medicine. Parasitologia 2022, 2, 228-236. https://doi.org/10.3390/parasitologia2030019
Brener B, Burgarelli E, Suarez M, Keidel L. Cryptosporidiosis in Reptiles from Brazil: An Update for Veterinary Medicine. Parasitologia. 2022; 2(3):228-236. https://doi.org/10.3390/parasitologia2030019
Chicago/Turabian StyleBrener, Beatriz, Eduardo Burgarelli, Marianne Suarez, and Lucas Keidel. 2022. "Cryptosporidiosis in Reptiles from Brazil: An Update for Veterinary Medicine" Parasitologia 2, no. 3: 228-236. https://doi.org/10.3390/parasitologia2030019