Biomechanical Analysis of the FlatFoot with Different 3D-Printed Insoles on the Lower Extremities
Abstract
:1. Background
2. Methods
2.1. 3D-Printed Insole Fabrication
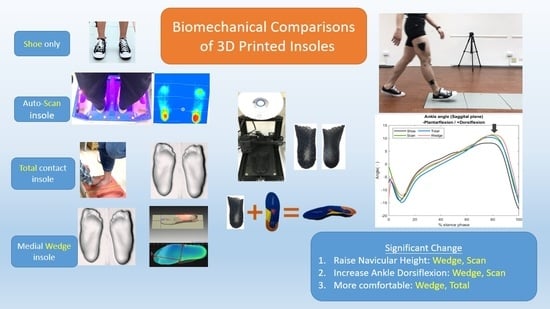
- Auto-scan insoles: the participants were asked to stand on a pressure sensor with body weight equally distributed across both feet using an auto-scan system (Joy Sunrise Research Inc., Taipei, Taiwan) (Figure 1). Subsequently, the software automatically determined the module of the insole based on the distribution of pressure.
- Total contact insoles: the geometric shape of the foot was obtained by scanning a foam box stepped in by the participants via a 3D scanner (iSense 3D, 3D system Inc., Washington, DC, USA) (Figure 2).
- Medial wedge insoles: 5-mm wedges were added through the medial side of the foot to the abovementioned scanning results using foot model editing software (InsoleModuleDesign, Joy Sunrise Research Inc., Taipei, Taiwan) (Figure 3).
2.2. Experimental Procedures
2.3. Statistical Analyses
3. Results
3.1. Navicular Height
3.2. Ankle Joint Peak Eversion Angle and Frontal Plane Motion
3.3. Ankle Joint Peak Dorsiflexion Angle and Sagittal Plane Motion
3.4. Ankle Joint Frontal Plane Moment
3.5. Knee Joint Frontal Plane Moment
3.6. Comfort Scale
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Harris, R.I.; Beath, T. Hypermobile flat-foot with short tendon achillis. J. Bone Joint Surg. Am. 1948, 30, 116–140. [Google Scholar] [CrossRef] [PubMed]
- Bordin, D.; De Giorgi, G.; Mazzocco, G.; Rigon, F. Flat and cavus foot, indexes of obesity and overweight in a population of primary-school children. Minerva Pediatr. 2001, 53, 7–13. [Google Scholar] [PubMed]
- Harris, R.; Beath, T. An Investigation of Foot Ailments in Canadian Soldiers; Report fi NRC; National Research Council of Canada: Ottawa, ON, Canada, 1947; Volume 1. [Google Scholar]
- Tareco, J.M.; Miller, N.H.; MacWilliams, B.A.; Michelson, J.D. Defining flatfoot. Foot Ankle Int. 1999, 20, 456–460. [Google Scholar] [CrossRef] [PubMed]
- Saraswat, P.; MacWilliams, B.A.; Davis, R.B.; D’Astous, J.L. Kinematics and kinetics of normal and planovalgus feet during walking. Gait Posture 2014, 39, 339–345. [Google Scholar] [CrossRef]
- Tong, J.W.; Kong, P.W. Association between foot type and lower extremity injuries: Systematic literature review with meta-analysis. J. Orthop. Sports Phys. Ther. 2013, 43, 700–714. [Google Scholar] [CrossRef] [Green Version]
- Huang, Y.C.; Wang, L.Y.; Wang, H.C.; Chang, K.L.; Leong, C.P. The relationship between the flexible flatfoot and plantar fasciitis: Ultrasonographic evaluation. Chang Gung Med. J. 2004, 27, 443–448. [Google Scholar]
- Peng, Y.; Wong, D.W.; Wang, Y.; Chen, T.L.; Tan, Q.; Chen, Z.; Jin, Z.; Zhang, M. Immediate effects of medially posted insoles on lower limb joint contact forces in adult acquired flatfoot: A pilot study. Int. J. Environ. Res. Public Health 2020, 17, 2226. [Google Scholar] [CrossRef] [Green Version]
- Souza, T.R.; Pinto, R.Z.; Trede, R.G.; Kirkwood, R.N.; Fonseca, S.T. Temporal couplings between rearfoot-shank complex and hip joint during walking. Clin. Biomech. 2010, 25, 745–748. [Google Scholar] [CrossRef]
- Neal, B.S.; Griffiths, I.B.; Dowling, G.J.; Murley, G.S.; Munteanu, S.E.; Franettovich Smith, M.M.; Collins, N.J.; Barton, C.J. Foot posture as a risk factor for lower limb overuse injury: A systematic review and meta-analysis. J. Foot Ankle Res. 2014, 7, 55. [Google Scholar] [CrossRef] [Green Version]
- Van der Worp, H.; van Ark, M.; Roerink, S.; Pepping, G.J.; van den Akker-Scheek, I.; Zwerver, J. Risk factors for patellar tendinopathy: A systematic review of the literature. Br. J. Sports Med. 2011, 45, 446–452. [Google Scholar] [CrossRef] [Green Version]
- Andriacchi, T.P. Valgus alignment and lateral compartment knee osteoarthritis: A biomechanical paradox or new insight into knee osteoarthritis? Arthritis Rheum. 2013, 65, 310–313. [Google Scholar] [CrossRef]
- Shriram, D.; Parween, R.; Lee, Y.H.D.; Subburaj, K. Effects of counteracting external valgus moment on lateral tibial cartilage contact conditions and tibial rotation. Annu. Int. Conf. IEEE Eng. Med. Biol. Soc. 2017, 2017, 1625–1628. [Google Scholar]
- Sharma, L.; Song, J.; Dunlop, D.; Felson, D.; Lewis, C.E.; Segal, N.; Torner, J.; Cooke, T.D.; Hietpas, J.; Lynch, J.; et al. Varus and valgus alignment and incident and progressive knee osteoarthritis. Ann. Rheum. Dis. 2010, 69, 1940–1945. [Google Scholar] [CrossRef]
- Chen, Y.C.; Lou, S.Z.; Huang, C.Y.; Su, F.C. Effects of foot orthoses on gait patterns of flat feet patients. Clin. Biomech. 2010, 25, 265–270. [Google Scholar] [CrossRef]
- Bonifacio, D.; Richards, J.; Selfe, J.; Curran, S.; Trede, R. Influence and benefits of foot orthoses on kinematics, kinetics and muscle activation during step descent task. Gait Posture 2018, 65, 106–111. [Google Scholar] [CrossRef]
- Costa, B.L.; Magalhaes, F.A.; Araujo, V.L.; Richards, J.; Vieira, F.M.; Souza, T.R.; Trede, R. Is there a dose-response of medial wedge insoles on lower limb biomechanics in people with pronated feet during walking and running? Gait Posture 2021, 90, 190–196. [Google Scholar] [CrossRef]
- Dombroski, C.E.; Balsdon, M.E.; Froats, A. The use of a low cost 3D scanning and printing tool in the manufacture of custom-made foot orthoses: A preliminary study. BMC Res. Notes 2014, 7, 443. [Google Scholar] [CrossRef] [Green Version]
- Tack, P.; Victor, J.; Gemmel, P.; Annemans, L. 3D-printing techniques in a medical setting: A systematic literature review. Biomed. Eng. Online 2016, 15, 115. [Google Scholar] [CrossRef] [Green Version]
- Lee, J.S.; Kim, K.B.; Jeong, J.O.; Kwon, N.Y.; Jeong, S.M. Correlation of foot posture index with plantar pressure and radiographic measurements in pediatric flatfoot. Ann. Rehabil. Med. 2015, 39, 10–17. [Google Scholar] [CrossRef] [Green Version]
- Lu, T.W.; Chen, H.L.; Chen, S.C. Comparisons of the lower limb kinematics between young and older adults when crossing obstacles of different heights. Gait Posture 2006, 23, 471–479. [Google Scholar] [CrossRef]
- Benedetti, M.G.; Berti, L.; Straudi, S.; Ceccarelli, F.; Giannini, S. Clinicoradiographic assessment of flexible flatfoot in children. J. Am. Podiatr. Med. Assoc. 2010, 100, 463–471. [Google Scholar]
- Hunt, A.E.; Smith, R.M. Mechanics and control of the flat versus normal foot during the stance phase of walking. Clin. Biomech. 2004, 19, 391–397. [Google Scholar] [CrossRef]
- Leung, A.; Mak, A.; Evans, J. Biomechanical gait evaluation of the immediate effect of orthotic treatment for flexible flat foot. Prosthet. Orthot. Int. 1998, 22, 25–34. [Google Scholar] [CrossRef]
- Kitaoka, H.B.; Luo, Z.P.; Kura, H.; An, K.N. Effect of foot orthoses on 3-dimensional kinematics of flatfoot: A cadaveric study. Arch. Phys. Med. Rehabil. 2002, 83, 876–879. [Google Scholar] [CrossRef]
- Kido, M.; Ikoma, K.; Hara, Y.; Imai, K.; Maki, M.; Ikeda, T.; Fujiwara, H.; Tokunaga, D.; Inoue, N.; Kubo, T. Effect of therapeutic insoles on the medial longitudinal arch in patients with flatfoot deformity: A three-dimensional loading computed tomography study. Clin. Biomech. 2014, 29, 1095–1098. [Google Scholar] [CrossRef] [Green Version]
- Moriguchi, C.; Sato, T.; Gil Coury, H. Ankle movements during normal gait evaluated by flexible electrogoniometer. Braz. J. Phys. Ther. 2007, 11, 205–211. [Google Scholar] [CrossRef] [Green Version]
- Brockett, C.L.; Chapman, G.J. Biomechanics of the ankle. Orthop. Trauma 2016, 30, 232–238. [Google Scholar] [CrossRef]










| Shoe | Scan | Total | Wedge | |
|---|---|---|---|---|
| Lowest navicular height in static standing (mm) | 20.1 (11.6) | 29.4 (13.0) * | 30.4 (11.3) * | 32.2 (12.4) * |
| Lowest navicular height in dynamic walking (mm) | 19.8 (12.0) | 27.9 (12.0) * | 30.3 (11.7) * | 31.6 (11.6) * |
| Ankle eversion angle peak value (°) | 4.7 (6.0) | 4.0 (7.4) | 4.2 (6.4) | 6.2 (6.5) |
| Ankle eversion moment peak value (Nm/kg) | 0.67 (0.44) | 0.65 (0.39) | 0.63 (0.44) | 0.70 (0.27) |
| Ankle dorsiflexion angle peak value (°) | 9.6 (3.4) | 11.6 (3.2) * | 11.0 (3.0) | 12.5 (4.3) * |
| Knee adduction peak value (Nm/kg) | 0.77 (0.38) | 0.72 (0.36) | 0.81 (0.43) | 0.79 (0.24) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hsu, C.-Y.; Wang, C.-S.; Lin, K.-W.; Chien, M.-J.; Wei, S.-H.; Chen, C.-S. Biomechanical Analysis of the FlatFoot with Different 3D-Printed Insoles on the Lower Extremities. Bioengineering 2022, 9, 563. https://doi.org/10.3390/bioengineering9100563
Hsu C-Y, Wang C-S, Lin K-W, Chien M-J, Wei S-H, Chen C-S. Biomechanical Analysis of the FlatFoot with Different 3D-Printed Insoles on the Lower Extremities. Bioengineering. 2022; 9(10):563. https://doi.org/10.3390/bioengineering9100563
Chicago/Turabian StyleHsu, Chia-Yi, Chien-Shun Wang, Kuang-Wei Lin, Mu-Jung Chien, Shun-Hwa Wei, and Chen-Sheng Chen. 2022. "Biomechanical Analysis of the FlatFoot with Different 3D-Printed Insoles on the Lower Extremities" Bioengineering 9, no. 10: 563. https://doi.org/10.3390/bioengineering9100563