Trihalomethane Cancer Risk Assessment for Private and Shared Residences: Addressing the Differences in Inhalation Exposure
Abstract
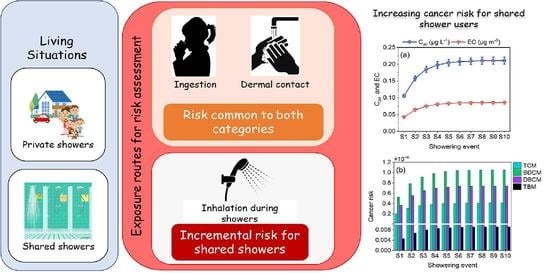
:1. Introduction
2. Materials and Methods
2.1. Study Area and Population
2.2. Water Quality Analysis
2.3. Trihalomethane Analysis
2.4. Exposure Routes and Risk Assessment Models
| Parameters | Distribution and Values | Reference |
|---|---|---|
| Cwi,/Chw—THM concentration (µg L−1/µg m3) | Table 2 | This study |
| IR—Ingestion rate (L day−1) | T a (1, 2, 3) | [25] |
| Pd—Permeability of THM through the skin (m min−1) | T (0.0000267, 0.00003, 0.000035) | [26] |
| t—Showering duration (minutes) | T (5, 10, 15) | [11] |
| Vs—Shower stall volume (L) | T (2000, 3500, 5000) | [27] |
| H—Henry’s constant | TCM: 0.25, BDCM: 0.124, DBCM: 0.0526, TBM: 0.0501. | [14] |
| Qw—Water flow (L min−1) | T (3, 4, 5) | [16] |
| Qg—Air flow/ventilation rate (L min−1) | T (40, 50, 60) | [1] |
| KoLA—Overall mass coefficient of each THM (L min−1) | TCM: 7.4, BDCM: 5.9, DBCM: 4.6, TBM: 3.7 | [28] |
| R—Breathing rate (m3 min−1) | T (0.012, 0.014, 0.016) | [14] |
| F—Showering frequency (events day−1) | T (0.72, 0.74, 0.76) | [11] |
| EF—Exposure frequency (days year−1) | T (330, 350, 365) drinking, T (300, 330, 365) dermal, T (300, 330, 360) inhalation | [1] |
| ED—Exposure duration (year) | Female: T (67, 72, 77) Male: T (65, 70, 75) | [29] |
| BW—Bodyweight (kg) | Female: T (50, 55, 60) Male: T (60, 65, 70) | [30] |
| AT—Averaging time (day) | Female: T (24,455, 26,280, 28,105) Male: T (23,725, 25,550, 27,375) | Calculated as per exposure duration |
| T—water temperature (°C) | Cold: T (10, 15, 20) Hot: T (35, 40, 45) | [16] |
| CSF—Cancer slope factor (mg kg−1 day−1) | [1] | |
| Trichloromethane | Oral and dermal: 0.0061 | |
| Bromodichloromethane | Oral and dermal: 0.062 | |
| Dibromochloromethane | Oral and dermal: 0.084 | |
| Tribromomethane | Oral and dermal: 0.0079 | |
| IUR—Inhalation unit risk (μg m−3)−1 | [4,13,14] | |
| Trichloromethane | 0.000023 | |
| Bromodichloromethane | 0.000037 | |
| Dibromochloromethane | 0.000024 | |
| Tribromomethane | 0.0000011 | |
| Parameter | Concentration Range (Min–Max) |
|---|---|
| pH | 6.8–7.5 |
| TOC (mg L−1) | 0.397–2.053 |
| Free chlorine residual (mg L−1) | 0–0.6 |
| Fluoride (mg L−1) | 0.014–0.49 |
| Bromide (mg L−1) | 0.95–1.35 |
| Chloride (mg L−1) | 2.48–18.97 |
| Nitrate (mg L−1) | 0.029–2.50 |
| Trihalomethanes (µg L−1) | |
| TCM | 1.7–15.24 |
| BDCM | 3.55–23.29 |
| DBCM | 4.84–25.52 |
| TBM | 1.6–6.57 |
2.4.1. Ingestion Route
2.4.2. Dermal Contact Route
2.4.3. Inhalation Route
2.5. Modified Inhalation Risk Model
2.6. Effect of Water Temperature on Trihalomethane Concentration
2.7. Adjustments in Population and Location-Based Parameters
3. Results and Discussion
3.1. Water Quality and Trihalomethane Concentration
3.2. Risk through Ingestion and Dermal Routes
3.3. Inhalation Route
3.3.1. Inhalation Risk from Private Shower Rooms
3.3.2. Inhalation Risk from Common Shower Rooms
3.4. Total Cancer Risk
3.5. Effect of Ventilation and Shower Duration on Cancer Risk
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Parveen, N.; Chowdhury, S.; Goel, S. Probabilistic Approach for Health Hazard Assessment of Trihalomethanes through Successive Showering Events. Environ. Sci. Pollut. Res. 2021, 30, 24793–24803. [Google Scholar] [CrossRef]
- Sdougkou, A.; Kapsalaki, K.; Kozari, A.; Pantelaki, I.; Voutsa, D. Occurrence of Disinfection By-Products in Swimming Pools in the Area of Thessaloniki, Northern Greece. Assessment of Multi-Pathway Exposure and Risk. Molecules 2021, 26, 7639. [Google Scholar] [CrossRef] [PubMed]
- Colas, A.; Baudet, A.; Le Cann, P.; Blanchard, O.; Gangneux, J.P.; Baurès, E.; Florentin, A. Quantitative Health Risk Assessment of the Chronic Inhalation of Chemical Compounds in Healthcare and Elderly Care Facilities. Toxics 2022, 10, 141. [Google Scholar] [CrossRef] [PubMed]
- IRIS Integrated Risk Information System. Available online: https://www.epa.gov/iris (accessed on 21 May 2022).
- US EPA National Primary Drinking Water Regulations. Available online: https://www.epa.gov/ground-water-and-drinking-water/national-primary-drinking-water-regulations (accessed on 21 May 2022).
- Health Canada. Guidelines for Canadian Drinking Water Quality: Guideline Technical Document; Trihalomethanes; Federal-Provincial-Territorial Committee on Drinking Water of the Federal-Provincial-Territorial Committee on Health and the Environment: Ottawa, ON, Canada, 2006. [Google Scholar]
- Indian Standard 10500; Drinking Water—Specifications (Second Revision). Bureau of India Standards: New Delhi, India, 2012; p. 16.
- Lee, S.C.; Guo, H.; Lam, S.M.J.; Lau, S.L.A. Multipathway Risk Assessment on Disinfection By-Products of Drinking Water in Hong Kong. Environ. Res. 2004, 94, 47–56. [Google Scholar] [CrossRef]
- Wang, Y.; Zhu, G.; Engel, B. Health Risk Assessment of Trihalomethanes in Water Treatment Plants in Jiangsu Province, China. Ecotoxicol. Environ. Saf. 2019, 170, 346–354. [Google Scholar] [CrossRef] [PubMed]
- Furst, K.E.; Coyte, R.M.; Wood, M.; Vengosh, A.; Mitch, W.A. Disinfection Byproducts in Rajasthan, India: Are Trihalomethanes a Sufficient Indicator of Disinfection Byproduct Exposure in Low-Income Countries? Environ. Sci. Technol. 2019, 53, 12007–12017. [Google Scholar] [CrossRef]
- Chowdhury, S. Exposure Assessment for Trihalomethanes in Municipal Drinking Water and Risk Reduction Strategy. Sci. Total Environ. 2013, 463, 922–930. [Google Scholar] [CrossRef]
- Zhang, D.; Dong, S.; Chen, L.; Xiao, R.; Chu, W. Disinfection Byproducts in Indoor Swimming Pool Water: Detection and Human Lifetime Health Risk Assessment. J. Environ. Sci. 2023, 126, 378–386. [Google Scholar] [CrossRef]
- USEPA. Exposures and Internal Doses of Trihalomethanes in Humans: Multi-Route Contributions from Drinking Water (Final); National Center for Environmental Assessment Office of Research and Development U.S. Environmental Protection Agency Cincinnati: Cincinnati, OH, USA, 2006. [Google Scholar]
- Tovar, S.S.T.; Susa, M.R. Cancer Risk Assessment from Exposure to Trihalomethanes in Showers by Inhalation. Environ. Res. 2020, 196, 110401. [Google Scholar] [CrossRef]
- Ahmed, F.; Khan, T.A.; Fakhruddin, A.N.M.; Rahman, M.M.; Mazumdar, R.M.; Ahmed, S.; Imam, M.T.; Kabir, M.; Abdullah, A.T.M. Estimation and Exposure Concentration of Trihalomethanes (THMs) and Its Human Carcinogenic Risk in Supplied Pipeline Water of Dhaka City, Bangladesh. Environ. Sci. Pollut. Res. 2019, 26, 16316–16330. [Google Scholar] [CrossRef]
- Chowdhury, I.R.; Chowdhury, S.; Al-Suwaiyan, M.S. Human Exposure and Risk of Trihalomethanes during Continuous Showering Events. Sci. Total Environ. 2020, 701, 134521. [Google Scholar] [CrossRef]
- USEPA. EPA Method 501.1, The Analysis of Trihalomethanes in Drinking Water by He Purge and Trap Method; EPA-500 Series; Genium Publishing Corporation 1996: Schenectady, NY, USA; Washington, DC, USA, 1979; p. 16. [Google Scholar]
- Mosaferi, M.; Asadi, M.; Aslani, H.; Mohammadi, A.; Abedi, S.; Nemati Mansour, S.; Maleki, S. Temporospatial Variation and Health Risk Assessment of Trihalomethanes (THMs) in Drinking Water (Northwest Iran). Environ. Sci. Pollut. Res. 2021, 28, 8168–8180. [Google Scholar] [CrossRef] [PubMed]
- USEPA. Guidelines for Human Exposure Assessment Risk Assessment; Risk Assessment Forum U.S. Environmental Protection Agency: Washington, DC, USA, 2019; p. 223. [Google Scholar]
- Zhang, Y.; Liang, C.; Zhao, L.; Guan, Y.; Jiang, S.; Zhan, C.; Du, P. Risk Analysis of Natural Water Resources Scarcity Based on a Stochastic Simulation Model in the Hilly Area of Southwest China. Stoch Environ. Res. Risk. Assess. 2022, 36, 33–49. [Google Scholar] [CrossRef]
- Senoro, D.B.; de Jesus, K.L.M.; Nolos, R.C.; Lamac, M.R.L.; Deseo, K.M.; Tabelin, C.B. In Situ Measurements of Domestic Water Quality and Health Risks by Elevated Concentration of Heavy Metals and Metalloids Using Monte Carlo and MLGI Methods. Toxics 2022, 10, 342. [Google Scholar] [CrossRef] [PubMed]
- Jiménez-Oyola, S.; Escobar Segovia, K.; García-Martínez, M.J.; Ortega, M.; Bolonio, D.; García-Garizabal, I.; Salgado, B. Human Health Risk Assessment for Exposure to Potentially Toxic Elements in Polluted Rivers in the Ecuadorian Amazon. Water 2021, 13, 613. [Google Scholar] [CrossRef]
- Qin, N.; Tuerxunbieke, A.; Wang, Q.; Chen, X.; Hou, R.; Xu, X.; Liu, Y.; Xu, D.; Tao, S.; Duan, X. Key Factors for Improving the Carcinogenic Risk Assessment of PAH Inhalation Exposure by Monte Carlo Simulation. Int. J. Environ. Res. Public Health 2021, 18, 11106. [Google Scholar] [CrossRef]
- Quality Companion 3 by Minitab; [Computer software]; Minitab, Inc.: State College, PA, USA, 2009; Available online: www.minitab.com (accessed on 12 October 2020).
- Parveen, N.; Ranjan, V.P.; Chowdhury, S.; Goel, S. Occurrence and Potential Health Risks Due to Trihalomethanes and Microplastics in Bottled Water. Environ. Eng. Sci. 2022, 39, 523–534. [Google Scholar] [CrossRef]
- Chowdhury, S.; Champagne, P. Risk from Exposure to Trihalomethanes during Shower: Probabilistic Assessment and Control. Sci. Total Environ. 2009, 407, 1570–1578. [Google Scholar] [CrossRef]
- BIS. National Building Code of India-Volume 1; Bureau of Indian Standards: New Delhi, India, 2016; p. 1226. [Google Scholar]
- Kujlu, R.; Mahdavianpour, M.; Ghanbari, F. Multi-Route Human Health Risk Assessment from Trihalomethanes in Drinking and Non-Drinking Water in Abadan, Iran. Environ. Sci. Pollut. Res. 2020, 27, 42621–42630. [Google Scholar] [CrossRef]
- Census Commissioner of India. Sample Registration System Based Abridged Life Tables 2014–2018; Ministry of Home Affairs, Government of India: New Delhi, India, 2018. [Google Scholar]
- ICMR ICMR-National Institute of Nutrition, India. Available online: https://www.nin.res.in/ (accessed on 12 October 2020).
- USEPA. Risk Assessment Guidance for Superfund Volume I: Human Health Evaluation Manual (Part F, Supplemental Guidance for Inhalation Risk Assessment); US Environmental Protection Agency: Washington, DC, USA, 2009; pp. 7–82. [Google Scholar]
- Little, J.C. Applying the Two-Resistance Theory to Contaminant Volatilization in Showers. Environ. Sci. Technol. 1992, 26, 1341–1349. [Google Scholar] [CrossRef] [Green Version]
- Xu, X.; Weisel, C.P. Human Respiratory Uptake of Chloroform and Haloketones during Showering. J. Expo. Sci. Environ. Epidemiol. 2005, 15, 6–16. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- USEPA. Supplemental Guidance for Assessing Susceptibility from Early-Life Exposure to Carcinogens; Risk Assessment Forum U.S. Environmental Protection Agency: Washington, DC, USA, 2005; pp. 1–126. [Google Scholar]
- Basu, M.; Gupta, S.K.; Singh, G.; Mukhopadhyay, U. Multi-Route Risk Assessment from Trihalomethanes in Drinking Water Supplies. Environ. Monit. Assess. 2011, 178, 121–134. [Google Scholar] [CrossRef] [PubMed]
- Kumari, M.; Gupta, S.K. Age Dependent Adjustment Factor (ADAF) for the Estimation of Cancer Risk through Trihalomethanes (THMs) for Different Age Groups A Innovative Approach. Ecotoxicol. Environ. Saf. 2018, 148, 960–968. [Google Scholar] [CrossRef]
- Siddique, A.; Saied, S.; Mumtaz, M.; Hussain, M.M.; Khwaja, H.A. Multipathways Human Health Risk Assessment of Trihalomethane Exposure through Drinking Water. Ecotoxicol. Environ. Saf. 2015, 116, 129–136. [Google Scholar] [CrossRef]
- Mishaqa, E.S.I.; Radwan, E.K.; Ibrahim, M.B.M.; Hegazy, T.A.; Ibrahim, M.S. Multi-Exposure Human Health Risks Assessment of Trihalomethanes in Drinking Water of Egypt. Environ. Res. 2022, 207, 112643. [Google Scholar] [CrossRef]
- Zaccarin, M.; Zanni, S.; Gallè, F.; Protano, C.; Valeriani, F.; Liguori, G.; Romano Spica, V.; Vitali, M. Studying Respiratory Symptoms Related to Swimming Pools Attendance in Young Athletes: The SPHeRA Study. Toxics 2022, 10, 759. [Google Scholar] [CrossRef]
- Ashley, D.L.; Smith, M.M.; Silva, L.K.; Yoo, Y.M.; De Jesús, V.R.; Blount, B.C. Factors Associated with Exposure to Trihalomethanes, NHANES 2001–2012. Environ. Sci. Technol. 2020, 54, 1066–1074. [Google Scholar] [CrossRef]
- Dock, A.; Linders, J.; David, M.; Gollasch, S.; David, J.; Ziegler, G. Are Workers on Board Vessels Involved with Chemicals from Treated Ballast Water Sufficiently Protected? A Decadal Perspective and Risk Assessment. Chemosphere 2020, 247, 125824. [Google Scholar] [CrossRef]
- Gängler, S.; Makris, K.C.; Bouhamra, W.; Dockery, D.W. Coupling External with Internal Exposure Metrics of Trihalomethanes in Young Females from Kuwait and Cyprus. J. Expo. Sci. Environ. Epidemiol. 2018, 28, 140–146. [Google Scholar] [CrossRef]







| THM Species | Cancer Risk (Minimum, Mean, Maximum) × 10−6 | Total Cancer Risk (Mean) × 10−6 | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Inhalation | Ingestion | Dermal Contact | S1 a | S3 | S5 | S7 | S10 | |||||
| S1 b | S3 | S5 | S7 | S10 | ||||||||
| TCM | 0.03 | 0.05 | 0.06 | 0.06 | 0.06 | 0.34 | 0.06 | 1.33 | 1.49 | 1.53 | 1.54 | 1.54 |
| 0.21 | 0.36 | 0.40 | 0.41 | 0.41 | 0.96 | 0.17 | ||||||
| 0.45 | 0.79 | 0.87 | 0.89 | 0.90 | 1.69 | 0.30 | ||||||
| BDCM | 0.08 | 0.14 | 0.15 | 0.16 | 0.16 | 6.83 | 1.23 | 20.71 | 21.11 | 21.20 | 21.23 | 21.24 |
| 0.53 | 0.92 | 1.02 | 1.04 | 1.05 | 17.13 | 3.05 | ||||||
| 1.07 | 1.88 | 2.08 | 2.13 | 2.14 | 27.83 | 4.96 | ||||||
| DBCM | 0.08 | 0.14 | 0.15 | 0.16 | 0.16 | 13.69 | 2.45 | 35.49 | 35.77 | 35.84 | 35.85 | 35.86 |
| 0.37 | 0.65 | 0.72 | 0.74 | 0.74 | 29.80 | 5.32 | ||||||
| 0.74 | 1.30 | 1.43 | 1.47 | 1.48 | 46.59 | 8.30 | ||||||
| TBM | 0.001 | 0.002 | 0.002 | 0.002 | 0.002 | 0.431 | 0.075 | 0.999 | 1.003 | 1.003 | 1.004 | 1.004 |
| 0.005 | 0.008 | 0.009 | 0.009 | 0.009 | 0.846 | 0.149 | ||||||
| 0.009 | 0.015 | 0.017 | 0.018 | 0.018 | 1.283 | 0.228 | ||||||
| Total | 1.11 | 1.94 | 2.15 | 2.20 | 2.21 | 48.73 | 8.69 | 58.53 | 59.36 | 59.57 | 59.62 | 59.64 |
| Reference | Location | Trihalomethane Concentration (µg L−1) a | Cancer Risk | |||||
|---|---|---|---|---|---|---|---|---|
| TCM | BDCM | DBCM | TBM | Ingestion | Dermal | Inhalation | ||
| [35] | Jharkhand and West Bengal, India | 3.92–532.64 | 0.0–315.2 | 0.0–187.07 | 9.78–1854 | 3.93 × 10−5–3.19 × 10−3 | <10−8 | 6.02 × 10−5–3.36 × 10−3 |
| [36] | Eastern India | 223–461 | 2–13 | 2–13 | 231–484 | 2.37 × 10−4 | 5.76 × 10−9 | negligible |
| [37] | Karachi, Pakistan | 8.4–167.3 | 0.19–3.3 | 0.22–1.9 | 0 | 1.10 × 10−5 | 4.42 × 10−5 | 6.68 × 10−5 |
| [15] | Dhaka, Bangladesh | Total THM = 20.2–439.2 including TCM = 6.25–134.06. | 4.08 × 10−5 | 5.45 × 10−12 | 9.57 × 10−10 | |||
| [11] | Toronto, Canada | 1.4–10.7 | 1.0–5.8 | 0.8–3.6 | 0–0.5 | 9.0 × 10−6 | 3.0 × 10−6 | 3.0 × 10−6 |
| Dhahran, Saudi Arabia | 1.2–6.1 | 0.5–3.4 | 0.0–1.2 | 0–0.7 | 3.0 × 10−6 | 1.0 × 10−6 | 1.0 × 10−6 | |
| [9] | Jiangsu Province, China | 4.8–20.4 | 1.7–12.7 | 4.2–12.0 | 0.2–7.2 | 5.81 × 10−6–1.67 × 10−5 | 2.82 × 10−6–7.98 × 10−6 | 2.24 × 10−6–1.54 × 10−5 |
| [18] | Tabriz, Iran | 0.0–101 | 0.0–601 | 0.0–118 | 0.0–79 | 2 × 10−4 | 2.35 × 10−5 | 3.43 × 10−5 |
| [14] | Bogotá, Colombia | 31.25 | 0.0 | 4.01 | 4.09 | _ b | _ | 18 × 10−6–48 × 10−6 |
| [38] | All over Egypt | Total THM = 29.07–86.01 | Total Cancer risk = 1.0 × 10−6–42.2 × 10−6 | |||||
| Current study c | West Bengal, India | 1.7–15.24 | 3.55–23.2 | 4.84–25.5 | 1.6–6.57 | 48.73 × 10−6 | 8.69 × 10−6 | 1.11 × 10−6 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Parveen, N.; Goel, S. Trihalomethane Cancer Risk Assessment for Private and Shared Residences: Addressing the Differences in Inhalation Exposure. Toxics 2023, 11, 295. https://doi.org/10.3390/toxics11040295
Parveen N, Goel S. Trihalomethane Cancer Risk Assessment for Private and Shared Residences: Addressing the Differences in Inhalation Exposure. Toxics. 2023; 11(4):295. https://doi.org/10.3390/toxics11040295
Chicago/Turabian StyleParveen, Naseeba, and Sudha Goel. 2023. "Trihalomethane Cancer Risk Assessment for Private and Shared Residences: Addressing the Differences in Inhalation Exposure" Toxics 11, no. 4: 295. https://doi.org/10.3390/toxics11040295