1. Introduction
Freezing of gait (FOG) is one of the most disabling features of Parkinson’s disease (PD) [
1]. FOG motor disorder represents an intermittent failure to initiate or maintain locomotion [
2]. FOG was defined in 2010, as a “brief episodic absence or marked reduction in stride progression despite the intention to walk” [
3].
According to Bartels et al. [
4], the prevalence of freezers, which are people diagnosed with PD in whom the FOG symptom manifests, ranges from 7% in the early stages to 60% in the severe stages. Rawson et al. [
5] have stated that between 20% and 60% of people living with PD will eventually experience this symptom, and Saad et al. [
6] considered that over half of patients with PD could develop FOG in the course of the disease. Morris et al. [
7] have reported that progressively more people who experience FOG restrict their walking and reduce their level of physical activity to avoid triggering the motor disorder.
The relationship between akinesia and FOG remains unclear [
4] as FOG is not necessarily a completely frozen akinetic posture [
8]. Akinesia is the sudden inability to initiate any movement [
9], and there is a type of FOG related to this behavior. However, different disturbances may be seen during the gait of freezers [
8].
In 1995, Thompson and Marseden [
8,
10,
11,
12] defined three types of FOG, (I) freezing, when the feet seems like they are glued to the ground, as a complete or partial akinesia; (II) festination, when the normal gait rhythm changes to a shuffling gait, with faster and shorter steps; and (III) trembling in place, when the lower extremities may show signs of shaking while glued to the ground.
FOG episodes last more than one second and can be triggered by postural transitions [
1]. An FOG trigger can be a movement, e.g., a turn while walking (turning hesitation), the beginning of walking (starting hesitation), and just before reaching a destination (destination hesitation); an environmental constraint, e.g., doors, narrow passages, public transportation, and small or messy spaces; a dual task, either motor dual task or motor-cognitive dual task; or a negative emotion, such as anxiety, stress, anger, fear, or distress [
7,
13,
14,
15].
FOG is still a poorly understood phenomenon [
8] and its pathophysiology is still not clear enough [
4]. Clinical evaluation of FOG has been included in the Movement Disorder Society Unified Parkinson’s Disease Rating Scale (MDS-UPDRS), the most widely used clinical scale for assessing PD [
16]. In item 2.13 of Part II (MDS-UPDRS)—the motor experiences of daily living (M-EDL)—the evaluator asks the patient if, during a normal day in the past week, a sudden block or stop, as if his/her foot were glued to the floor, occurred while walking. The answer is a score from 0 (“No”) to 4 (“Due to FOG episodes, I need help to walk”). In item 3.11 of Part III (MDS-UPDRS), a motor examination—gait assessment—is performed while the patient walks away from and then towards the examiner, allowing both sides of the body to be observed simultaneously. The patient should walk at least 10 m (30 feet), then turn around and return to the evaluator. The evaluator looks for hesitations at the beginning and hesitation in movements, especially when turning around and reaching the end of the task. The evaluator scores the patient’s gait from 0 (no freezing) to 4 (the patient freezes several times while walking straight).
It is important to highlight that Part II of MDS-UPDRS has 13 items and Part III has 18 items in total, therefore, there are two specific items for FOG assessment out of 31. The MDS-UPDRS has the advantage of being available to most clinicians; however, it requires experience and may not reveal FOG even for cases confirmed by the individual’s medical history [
8]. The assessment of FOG in the MDS-UPDRS is not an accurate representation of daily life and, as a consequence, FOG is often difficult to observe during a clinical visit [
2].
A golden standard for the detection and assessment of the FOG phenomenon is currently unavailable [
3,
5,
6,
17]. The importance of this work is due to the crucial need for an accurate method of detecting FOG and rating its severity and impact for the determination of the appropriate treatment and follow up [
5,
6]. Furthermore, determining methods to assess physical mobility in PD could prevent falls, reduce or overcome FOG episodes, and increase the quality of life of freezers [
5,
6].
The need to assess physical mobility in clinical practice was raised by Podsiadlo and Richardson [
18] in 1991, when the Timed-Up and Go (TUG) test, using a time score in seconds, was proposed to assess the risk of fall in elderly populations. Similarly, our hypothesis is that it is possible to assess FOG episodes in freezers with a simple and short test, using limited space.
Laboratory testing of gait motor abilities on sway platforms or treadmills is impractical in most clinical settings, due to their length and complexity; furthermore, it is not profitable to use them with frail patients [
18]. The challenge to cause FOG in a controlled environment without the use of complex technologies and while respecting the fragility and limitation of the PD patient came about because of its convenience.
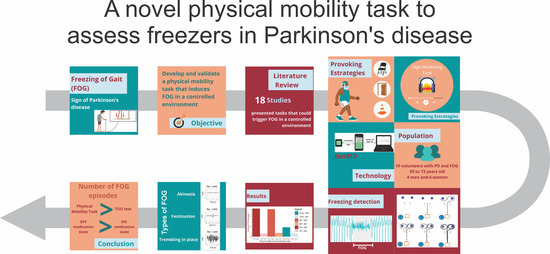
The objective of the current study is to develop a simple physical mobility task that induces FOG in a controlled environment using known triggers of FOG episodes as described in the literature in order to evaluate freezers in PD. Using Inertial Measurement Unit (IMU) with accelerometer and gyroscope and video recordings, the proposed method was validated.
3. Results
The results are presented to validate the proposed physical mobility tasks.
Table 3 shows the number of FOG episodes during the TUG test,
Table 4 shows the number of FOG episodes during the proposed physical mobility motor task (MT) and
Table 5 shows the number of FOG episodes during the dual task (DT). Three trials were conducted in each medication state (ON or OFF) to increase the number of observations, thereby contributing to a more reliable result. The answers of the volunteers for the DMT during the dual task are presented in
Supplementary Materials.
Table 6 shows the information about the NFOG-Q score and the total number of FOG episodes for each volunteer during OFF and ON medication states and while performing the proposed physical mobility tasks, the motor task, and the cognitive–motor dual task.
Table 6 displays the total duration time of FOG episodes and the TF (as employed in several studies [
9,
15,
23,
25,
27]). The latter represents the sum, in seconds, of the time difference between the beginning and end of each FOG episode. The results depict the number of FOG occurrences and total duration of FOG episodes for each participant during the OFF and ON medication states.
Table 7 compares the results of the present study with the results of the studies included in the literature review that could trigger and detect FOG episodes during data collection.
Table 7 shows the author and year of the paper (see also
Table 1), the sample size N, which is the number of participants who took part in the study, the number of freezers, which represents the number of participants who froze during the experiment, the number of FOG events, the recording time, and the number of trials.
Not all papers disclosed the duration of the trials, so recording time was not included in lines 1, 2, 3, and 5 of
Table 7. The authors conclude that, analogous to what happened in our work, not all trials have a specific time to be completed. As a result the authors chose to analyze the number of trials indicated in the method sections of the studies—except Handojoseno et al. [
20]—and compare this with the number of FOG events that occurred during the proposed physical mobility tasks—the motor task and dual task—during the OFF-medication state.
The three types of FOG according to the literature [
8,
10,
11,
12] are presented in
Figure 6,
Figure 7 and
Figure 8. The figures show data from accelerometer and gyroscope on x, y and z axes placed on the right iliac spine. The waveforms shown in
Figure 6,
Figure 7 and
Figure 8 are typical signals that occur during akinesia, shuffling and trembling in place.
Figure 6 shows one type of freezing—akinesia—of two volunteers, one for each row. This FOG type can manifest as a complete akinesia, in which the entire body is frozen, or partial akinesia, when only the lower body is frozen.
Figure 7 shows the second type of freezing—festination or shuffling—of two volunteers, one for each row. This FOG type is characterized by a change in the normal gait rhythm. Finally,
Figure 8 shows the third type of freezing—trembling in place—of two volunteers, one for each row. This FOG type happens when the lower extremities show signs of shaking while glued to the ground.
Table 8, based on the work of Podsiadlo and Richardson [
18], illustrates how the proposed physical mobility motor task can be used to record changes in the duration and number of FOG events over time. A pair of specific improvements for freezers—a reduction of the time in seconds of FOG and the number of FOG episodes—is of particular interest.
4. Discussion
The results of this study support our hypothesis that it is possible to cause FOG in a controlled environment with a short and simple physical mobility motor task, using limited space, without the use of complex technologies as force platforms and treadmills, and respecting the fragility and limitation of a Parkinson’s disease patient. Besides that, the findings show that it is possible to detect FOG and to distinguish FOG types, i.e., freezing, shuffling, and trembling in place, by means of inertial sensors placed on the hips and calf. In our population of Parkinson’s disease patients, the proposed physical mobility tasks to assess FOG, both motor task and dual task, were practical and reliable.
Time in seconds to complete TUG provides a score that is an objective mean of the consequent functional changes of an individual over time [
18]. The TUG score for each volunteer who participated in this study is shown in
Table 2. In the same sense, the proposed physical mobility motor task to assess FOG can be used either as a screening test or a descriptive tool, as shown in
Table 8.
The New FOG-Q is reliable [
32] and has been used in several experiments [
1,
2,
5,
27]. Therefore, it is considered an important measurement for the elucidation of FOG severity during the assessment of freezers in Parkinson’s disease.
Table 2 shows that the highest score of TUG and of the New FOG-Q belongs to volunteer 9, a subject that experienced several FOG episodes during OFF and ON medication states. Volunteer 8 has the second highest score for New FOG-Q, with 14 FOG events, and nine minutes and three seconds spent in FOG condition during data collection (See
Table 6). Volunteer 5 has the third highest score of New FOG-Q and froze during OFF and ON medication states. Only volunteers 5 and 9 froze under both medication conditions. Volunteer 2 had a significantly higher New FOG-Q score; however, the subject froze only three times.
Volunteers 3 and 4 have the highest number of FOG events, both have a New FOG-Q score greater than 19. For the volunteers with New FOG-Q scores lower than 14 (volunteers 1 and 10), the number of FOG events was 1 or 0 and the time spent frozen was less than 2 s. Only one volunteer did not freeze during the experiment.
It is not possible to state with certainty the reasons why volunteers 3 and 4 had the highest number of FOG, since this symptom is still a poorly understood phenomenon, and its pathophysiology, according to the literature, is still unclear according. Both volunteers do not stand out from the others in relation to age, time of PD diagnosis, the TUG score, nor the total MDS-UPDRS score, however when considering the New FOG-Q, both have a score greater than 19. Even so, the highest scores for the New FOG-Q belong to volunteers 9, 8, 5 and 2.
Motor performance among PD patients generally shows large variability. This was also the case among the group of patients who participated in this study. For example, during nonfreezing episodes, some patients maintained a regular gait that could hardly be distinguished from that of healthy elderly people, while others had slow and unstable gait [
37].
Bachlin [
37] stated that a limitation in FOG studies is that the controlled environment and the presence of a physiotherapist may reduce the likelihood of FOG in patients that do not experience any FOG events during data collection and where researchers are not able to explain why two volunteers did not have any FOG during their study.
The video recordings of our data collection show that volunteer 1, the one who did not freeze during our data collection, used strategies for overcoming FOG episodes, such as adapting a faster-than-normal rhythm and lifting the leg higher than usual to walk [
5].
Table 6 shows that the time spent frozen is not directly correlated with the number of FOG events. For example, volunteer 3 had 39 FOG events during their OFF-medication state while performing the motor task and the dual task, but the time they spent frozen was less than 3 min, while volunteer 8 had 14 FOG events performing the same tasks, but they spent more than 9 min in a FOG condition while performing the proposed tasks. The same happens with volunteer 4, who had 21 FOG events and spent more than 11 min in a FOG condition. One can conclude that volunteer 3 has a high number of FOG events, but is able to de-FOG fast, which means that they are able to get out of the FOG condition in less time than volunteers 4 and 8, for example. It can be concluded that, due to the variability of the signs in Parkinson’s disease and the different progressions of the disease in each individual, volunteers 3 and 4 were more sensitive to the triggers used in the proposed tasks.
Velik et al. [
27] and Alvarez et al. [
33] recorded daily life motion to detect specific motor patterns of the limbs, since it is often difficult to observe these during clinical visits [
2]. However, to achieve this feat, expensive technology, large available space, and a previously trained staff are required to operate the cameras and sensors. Additionally, there is a need for storage capacity so that all recordings are saved and can be later watched by experienced evaluators for the detection of FOG. Meanwhile, the present work raises the possibility that FOG assessment can be carried out, supported by health professionals, in a limited space by performing a physical mobility task designed to trigger FOG events. Furthermore, the detection of FOG events for posterior analysis can be executed with the use of inertial sensors and video recordings from a cell phone camera.
The proposed method to assess FOG, when combined with a mobile phone and three smartwatches equipped with inertial sensors, allows one to trigger and to detect FOG episodes in a controlled environment using a physical mobility task. We were able to create an accurate representation of daily life situations to cause FOG by developing a task that includes all the movements highlighted in the literature as potential triggers to FOG episodes, for instance, to initiating gait, walking through a narrow doorway, making left and right 360-degree turns, and reaching a destination.
It was possible to detect FOG using inertial sensors placed on the hips and calf of the subjects while they performed the proposed physical mobility tasks (MT and DT).
Table 6 shows the number of FOG episodes and the total time in seconds of FOG duration.
Table 4 and
Table 5 show the total number of FOG episodes for each trial of the motor task and the dual task per volunteer. This number is considered high when compared with the work of Popovic et al. [
8], Beck et al. [
15] and Cando et al. [
23] presented in
Table 7, and when compared with the number of FOG events caused by the TUG test, displayed in
Table 3.
Dopaminergic medication has a significant effect on the occurrence of FOG [
4,
12]. Clinical experience suggests that most patients who experience FOG improve with the dopaminergic medication, however FOG persists in a milder form [
4]. The results of Schaafsma [
12] suggest the medication increases the threshold of FOG occurrence but does not cure the symptoms.
Table 3,
Table 4,
Table 5 and
Table 6 show the difference in number of FOG comparing OFF and ON medication states while performing the proposed motor tasks. They show that 125 FOG episodes occurred during the OFF state and 19 FOG episodes occurred during the ON state. Therefore, the proposed method is able to detect the reduction in FOG events when patients are using dopamine.
The comparison between volunteers young and older than 60 showed that, for volunteers younger 60 years old, the total number of FOG was 64, distributed in 32 FOG events for the motor task and 32 for the dual task. TUG did not trigger any FOG episode during OFF medication state for this subgroup. During the ON medication state, there were no FOG episodes either.
For volunteers older than 60, the total number of FOG was 80, distributed in such a way that there were 18 for TUG, 21 for the motor task and 22 for the dual task during the OFF medication state. During the ON medication state, there were six FOG episodes in TUG, seven FOG episodes in the motor task and six FOG episodes in the dual task.
An important aspect to note of
Table 4 and
Table 5 is the number of FOG events triggered by the motor task (MT) and the dual task (DT). The simple motor task caused 53 FOG episodes while the dual task caused 54 during the OFF medication state. The TUG test, which is widely used in the clinical evaluation of PD patients, triggered 18 FOG episodes during the OFF medication state. During the ON medication state, there were seven FOG episodes for MT, six for DT and six for the TUG test. The close results between the proposed tasks may indicate that the dual task is not crucial to trigger FOG, as at one point both the simple motor task and the dual task caused 60 FOG episodes each. Furthermore, the results show how effective novel physical mobility tasks are in triggering FOG to assess freezers in Parkinson’s disease, as they were able to cause three times more FOG episodes during the OFF medication state than the TUG test.
Studies that have investigated dual task [
13,
15,
21,
22,
29], have demonstrated that cognitive load has a negative effect on the gait of patients with PD, however, when it comes to FOG-provoking strategies, the dual task is non-essential according to our findings. Considering the equipment and resources needed to complete the dual task, e.g., a device to play the audio track with the numbers for the Digital Monitoring Task, a speaker, a number draw, and the complexity of the dual task itself—not only for the person who is performing the dual task but also to the researcher group—one can conclude that, when the physical mobility motor task is specially designed to cause FOG episodes using triggers of movement and environmental constraints, that the dual task is not fundamental.
Figure 6,
Figure 7 and
Figure 8 show, respectively, the distinct FOG types, freezing, festination, and trembling in place, defined by Thompson and Marseden [
8]. In the work of Schaafsma [
12], three different observers characterized the type, duration, and clinical manifestations of FOG, and quantified it by analyzing their videotapes. In the study of Bartels et al. [
4], three observers independently watched videotapes of the tasks and elucidated the number of FOG episodes. A FOG episode was considered to take place if a patient hesitated for one second or more [
4]. The researchers clarified that by exclusively using the video rating method, they might have missed very brief FOG episodes [
4]. The analysis of FOG episodes using only video recordings represents a subjective assessment of the patient, because it depends on the observer’s experience and expertise, the shooting angle, and the quality of the video. It has been proven by several studies [
8,
20,
27] that the use of sensors optimizes data collection.
The literature review showed that 11 studies were able to trigger FOG in a controlled environment.
Table 7 shows the papers over time that disclose the number of FOG episodes during the experiment.
Table 7 displays the total number of volunteers included in the research; the column titled ‘Number of Freezers’ shows the actual number of volunteers who froze during data collection [
15,
23,
27]. The difficulty of accessing the FOG and causing it in a controlled environment is also disclosed in the studies of Saad et al. [
6] and Jovanov et al. [
6,
9] in which, to test a new equipment, the researchers had to simulate FOG episodes themselves.
Table 8 is an example of how the proposed physical mobility motor task can be used to record changes in the duration and number of FOG events over time and, per
Figure 2, in a setting where freezers perform regular tasks, thus allowing the examiner to assess the FOG symptom during a clinical visit.
An intervention designed by Rawson [
5] to reduce FOG in PD was tested in seven patients. The participants completed what the authors called a ‘FOG boot Camp’, a six-week program with one and a half hour classes each week designed and taught by two specialists in neurological and geriatric physiotherapy, respectively [
5]. The classes had education and group discussions on strategies for overcoming a FOG episode. This was followed by practicing these strategies in environments designed to trigger FOG, such as sharp turns, narrow pathways, doorways, and turns to sit in a chair [
5].
The applied strategies were based on existing literature and included sensorial cues (auditory, visual, and vibratory) and self-initiated strategies that required executive functioning and attentional processes and included activities such as lifting one leg higher than usual, walking sideways, moving one foot backward before walking, making wider turns, shifting leg weight, and imagining a clock on the ground to help with turning [
3,
5]. The main objective of Rawson et al. [
5] was to determine the feasibility, safety, and acceptability of a once-weekly community-based group intervention. Participants had favorable feedback and showed reduced FOG.
External rhythmic cues have been found to be effective in overcoming FOG [
19,
23,
42]. However, the continuous presence of an auditory, visual, or vibratory cue may reduce effectiveness and disturb normal social activity [
27]. Therefore, taking the dopaminergic medication correctly and learning self-initiated strategies to reduce or overcome FOG episodes is the best current alternative for freezers.
The proposed physical mobility motor task could be used as a tool to measure functional changes, to record changes in the duration and number of FOG events over time, to assess the impact on gait of a medication dosage change, and to test the acknowledgement and effectiveness of learned self-strategies to overcome FOG. The improvement of gait mobility and the decrease frequency of FOG events are the goals when assessing gait in freezers [
5].
Further work, with an increased number of volunteers, is required to understand the influence of age, the time of diagnosis and the New FOG-Q score on results and to improve the analysis. Additionally, the next stage of the research should be a feature extraction from the inertial signals, to better understand the signal dynamics and how the accelerometer and gyroscope signals from the three sensors placed in the volunteer’s body behave during an FOG event.