Cardiovascular Care of Turner Syndrome Women in Germany: Where Do We Stand?—Results from an Online Patient Survey
Abstract
:1. Introduction
2. Materials and Methods
2.1. Ethical Approval
2.2. Study Design
2.3. Assessment of Patient Characteristics and Cardiovascular Morbidity
2.4. Assessment of Cardiovascular Care
2.5. Statistical Analysis
3. Results
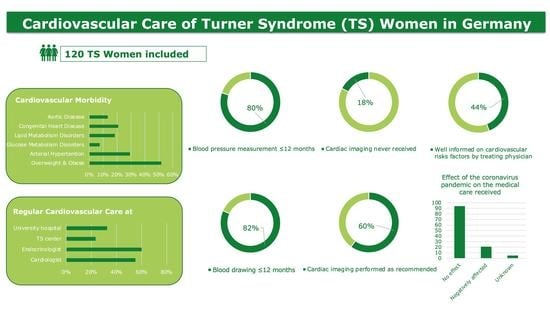
3.1. Patient Characteristics and Cardiovascular Morbidity
3.2. Cardiovascular Care
3.2.1. General Cardiovascular Care of TS Women in Germany
3.2.2. Cardiovascular Care of TS Women with Arterial Hypertension and/or Congenital Heart Disease in Germany
3.2.3. Cardiovascular Care of TS Women without Arterial Hypertension and/or Congenital Heart Disease in Germany
3.2.4. Cardiovascular Care of TS Women at Cardiometabolic Risk in Germany
4. Discussion
4.1. Cardiovascular Care of Women with TS in Germany: Where Do We Stand?
4.1.1. Importance of Specialized Multidisciplinary Clinics in the Cardiovascular Care of TS
4.1.2. Potential Influence of the Coronavirus Pandemic
4.2. Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Sybert, V.P.; McCauley, E. Turner’s Syndrome. N. Engl. J. Med. 2004, 351, 1227–1238. [Google Scholar] [CrossRef] [PubMed]
- Gravholt, C.H.; Andersen, N.H.; Conway, G.S.; Dekkers, O.M.; Geffner, M.E.; Klein, K.O.; Lin, A.E.; Mauras, N.; Quigley, C.A.; Rubin, K.; et al. Clinical practice guidelines for the care of girls and women with Turner Syndrome: Proceedings from the 2016 Cincinnati International Turner Syndrome Meeting. Eur. J. Endocrinol. 2017, 177, G1–G70. [Google Scholar] [CrossRef] [PubMed]
- Li, P.; Bačová, M.; Dalla-Pozza, R.; Haas, N.A.; Oberhoffer, F.S. Prevalence of Bicuspid Aortic Valve in Turner Syndrome Patients Receiving Cardiac MRI and CT: A Meta-Analysis. Congenit. Heart Dis. 2021, 17, 129–141. [Google Scholar] [CrossRef]
- Mavinkurve, M.; O’Gorman, C.S. Cardiometabolic and vascular risks in young and adolescent girls with Turner Syndrome. BBA Clin. 2015, 3, 304–309. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Oberhoffer, F.S.; Abdul-Khaliq, H.; Jung, A.-M.; Rohrer, T.R.; El Rahman, M.A. Two-dimensional speckle tracking of the abdominal aorta: A Novel Approach to Evaluate Arterial Stiffness in Patients with Turner Syndrome. Cardiovasc. Diagn. Ther. 2019, 9, S228–S237. [Google Scholar] [CrossRef]
- An, H.S.; Baek, J.S.; Song, M.K.; Kwon, B.S.; Bae, E.J.; Kim, G.B.; Lee, Y.A.; Noh, C.I. Impaired Vascular Function of the Aorta in Adolescents with Turner Syndrome. Pediatr. Cardiol. 2017, 38, 20–26. [Google Scholar] [CrossRef] [PubMed]
- Uçar, A.; Öz, F.; Baş, F.; Oflaz, H.; Nisli, K.; Tuğrul, M.; Yetim, A.; Darendeliler, F.; Saka, N.; Poyrazoğlu, Ş.; et al. Increased arterial stiffness in young normotensive patients with Turner Syndrome: Associations with Vascular Biomarkers. Clin. Endocrinol. 2015, 82, 719–727. [Google Scholar] [CrossRef] [PubMed]
- Bondy, C.A. Aortic dissection in Turner Syndrome. Curr. Opin. Cardiol. 2008, 23, 519–526. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Schoemaker, M.J.; Swerdlow, A.J.; Higgins, C.D.; Wright, A.F.; Jacobs, P.A. Mortality in Women with Turner Syndrome in Great Britain: A National Cohort Study. J. Clin. Endocrinol. Metab. 2008, 93, 4735–4742. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Arnold, L.; Bacova, M.; Dalla-Pozza, R.; Haas, N.A.; Oberhoffer, F.S. Physical Activity and Diet Quality: Effects on Cardiovascular Morbidity in Women with Turner Syndrome—Results from an Online Patient Survey. J. Clin. Med. 2022, 11, 167. [Google Scholar] [CrossRef] [PubMed]
- Hjerrild, B.E.; Mortensen, K.H.; Sørensen, K.E.; Pedersen, E.M.; Andersen, N.H.; Lundorf, E.; Hansen, K.W.; Hørlyck, A.; Hager, A.; Christiansen, J.S.; et al. Thoracic aortopathy in Turner Syndrome and the influence of bicuspid aortic valves and blood pressure: A CMR Study. J. Cardiovasc. Magn. Reson. 2010, 12, 12. [Google Scholar] [CrossRef] [PubMed] [Green Version]

| Patient Characteristics | |
|---|---|
| Total number | 120 |
| Age (years) | 36.79 ± 11.90 |
| Height (cm) | 153.94 ± 6.88 |
| Body weight (kg) | 63.08 ± 15.98 |
| BMI (kg/m2) | 26.56 ± 6.32 |
| Underweight (%) | 7 (5.83) |
| Normal weight (%) | 51 (42.50) |
| Overweight (%) | 35 (29.17) |
| Obese (%) | 27 (22.50) |
| Arterial hypertension (%) | 35 (29.17) |
| Anti-hypertensive therapy (%) | 28 (80.00) |
| Glucose metabolism disorders (%) | 9 (7.5) |
| Glucose metabolism therapy (%) | 9 (100.00) |
| Lipid metabolism disorders (%) | 22 (18.33) |
| Lipid metabolism therapy (%) | 3 (13.64) |
| Smoker (%) | 5 (4.17) |
| Congenital heart disease (%) | 25 (20.83) |
| Aortic disease (%) | 16 (13.33) |
| Aortic surgery (%) | 8 (50) |
| Cardiac surgery (%) | 17 (14.17) |
| Stroke (%) | 3 (2.5) |
| Cardiovascular Care | n (%) |
|---|---|
| Total number | 120 |
| Regular care at | |
| Cardiologist a | 66 (55) |
| Endocrinologist a | 72 (60) |
| TS center | 28 (23.33) |
| University hospital | 39 (32.5) |
| Member of TS Association | 44 (36.67) |
| Blood drawing ≤ 12 months a | 98 (81.67) |
| BP measurement ≤ 12 months a | 96 (80) |
| Cardiac imaging a,b | |
| Never received | 21 (17.5) |
| Performed as recommended | 72 (60) |
| Cardiovascular Care | University Hospital/TS Center (n = 18) | Others (n = 22) | p-Value |
|---|---|---|---|
| Arterial hypertension (%) | 13 (72.22) | 15 (68.18) | 1 |
| BP measurement ≤ 12 months a (%) | 12 (92.31) | 14 (93.33) | 1 |
| Anti-hypertensive therapy (%) | 12 (92.31) | 11 (73.33) | 0.33 |
| 24h blood pressure monitoring (%) | 12 (92.31) | 11 (73.33) | 0.33 |
| Congenital heart disease (%) | 9 (50) | 11 (50) | 1 |
| Cardiac surgery (%) | 5 (55.56) | 6 (54.55) | 1 |
| Cardiac imaging a,b | |||
| Never received (%) | 2 (11.11) | 3 (14.29) | 1 |
| Performed as recommended (%) | 12 (66.67) | 14 (70) | 1 |
| Well informed on cardiovascular risks factors (%) | 9 (52.94) | 10 (45.45) | 0.75 |
| Cardiovascular Care | University Hospital/TS Center (n = 26) | Others (n = 29) | p-Value |
|---|---|---|---|
| Blood drawing ≤ 12 months a (%) | 23 (88.46) | 23 (79.31) | 0.48 |
| BP measurement ≤ 12 months a (%) | 21 (80.77) | 20 (74.07) | 0.74 |
| Cardiac imaging a,b | |||
| Never received (%) | 2 (7.69) | 10 (34.48) | 0.022 * |
| Performed as recommended (%) | 19 (79.17) | 16 (55.17) | 0.085 |
| Well informed on cardiovascular risks factors (%) | 17 (65.38) | 9 (33.33) | 0.028 * |
| Cardiovascular Care | University Hospital/TS Center (n = 24) | Others (n = 33) | p-Value |
|---|---|---|---|
| Overweight/Obese (%) | 17 (70.83) | 28 (84.85) | 0.32 |
| BP measurement ≤ 12 months a (%) | 12 (70.59) | 22 (81.48) | 0.47 |
| Glucose metabolism disorders (%) | 5 (20.83) | 3 (9.1) | 0.26 |
| Glucose metabolism therapy (%) | 5 (100) | 3 (100) | |
| Blood drawing ≤ 12 months a (%) | 4 (80) | 3 (100) | 1 |
| Lipid metabolism disorders (%) | 8 (33.33) | 13 (39.39) | 0.78 |
| Lipid metabolism therapy (%) | 1 (12.5) | 2 (15.38) | 1 |
| Blood drawing ≤ 12 months a (%) | 7 (87.5) | 12 (92.31) | 1 |
| Well informed on cardiovascular risks factors (%) | 14 (58.33) | 12 (38.71) | 0.18 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bačová, M.; Li, P.; Arnold, L.; Dalla-Pozza, R.; Haas, N.A.; Oberhoffer, F.S. Cardiovascular Care of Turner Syndrome Women in Germany: Where Do We Stand?—Results from an Online Patient Survey. Healthcare 2022, 10, 504. https://doi.org/10.3390/healthcare10030504
Bačová M, Li P, Arnold L, Dalla-Pozza R, Haas NA, Oberhoffer FS. Cardiovascular Care of Turner Syndrome Women in Germany: Where Do We Stand?—Results from an Online Patient Survey. Healthcare. 2022; 10(3):504. https://doi.org/10.3390/healthcare10030504
Chicago/Turabian StyleBačová, Martina, Pengzhu Li, Leonie Arnold, Robert Dalla-Pozza, Nikolaus Alexander Haas, and Felix Sebastian Oberhoffer. 2022. "Cardiovascular Care of Turner Syndrome Women in Germany: Where Do We Stand?—Results from an Online Patient Survey" Healthcare 10, no. 3: 504. https://doi.org/10.3390/healthcare10030504