The Impact of the COVID-19 Pandemic on the Practice of Forensic Medicine: An Overview
Abstract
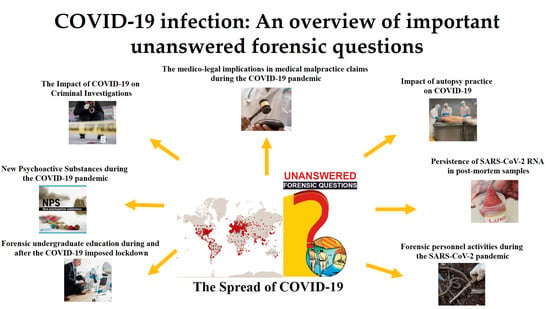
:1. Introduction
2. The sCOVID-19 Pandemic and Its Impact on Forensic Investigations
2.1. Influence of External Factors on Forensic Activities
2.2. Impact of Autopsy Practice on COVID-19 and Vice-Versa
2.3. Persistence of SARS-CoV-2 RNA in Post-Mortem Samples
2.4. Forensic Personnel Activities during the SARS-CoV-2 Pandemic
2.5. The Global Vaccination Program and Forensic Sciences
2.6. Forensic Undergraduate Education during and after the Imposed COVID-19 Lockdown
2.7. The Medico-Legal Implications in Medical Malpractice Claims during the COVID-19 Pandemic
3. Discussion
4. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Acknowledgments
Conflicts of Interest
References
- Ye, Z.-W.; Yuan, S.; Yuen, K.-S.; Fung, S.-Y.; Chan, C.-P.; Jin, D.-Y. Zoonotic origins of human coronaviruses. Int. J. Biol. Sci. 2020, 16, 1686–1697. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- World Health Organization (WHO). WHO Director-General’s Opening Remarks at the Media Briefing on COVID-19. 11 March 2020. Available online: https://www.who.int/director-general/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19---11-march-2020 (accessed on 17 November 2021).
- Haghani, M.; Bliemer, M.C.J. COVID-19 pandemic and the unprecedented mobilisation of scholarly efforts prompted by a health crisis: Scientometric comparisons across SARS, MERS and 2019-nCoV literature. Scientometrics 2020, 125, 2695–2726. [Google Scholar] [CrossRef] [PubMed]
- Valenzano, A.; Scarinci, A.; Monda, V.; Sessa, F.; Messina, A.; Monda, M.; Precenzano, F.; Mollica, M.P.; Carotenuto, M.; Messina, G.; et al. The Social Brain and Emotional Contagion: COVID-19 Effects. Medicina 2020, 56, 640. [Google Scholar] [CrossRef] [PubMed]
- Tangcharoensathien, V.; Calleja, N.; Nguyen, T.; Purnat, T.; D’Agostino, M.; Garcia-Saiso, S.; Landry, M.; Rashidian, A.; Hamilton, C.; AbdAllah, A.; et al. Framework for Managing the COVID-19 Infodemic: Methods and Results of an Online, Crowdsourced WHO Technical Consultation. J. Med. Internet Res. 2020, 22, e19659. [Google Scholar] [CrossRef]
- Nivette, A.E.; Zahnow, R.; Aguilar, R.; Ahven, A.; Amram, S.; Ariel, B.; Burbano, M.J.A.; Astolfi, R.; Baier, D.; Bark, H.-M.; et al. A global analysis of the impact of COVID-19 stay-at-home restrictions on crime. Nat. Hum. Behav. 2021, 5, 868–877. [Google Scholar] [CrossRef]
- Office for National Statistics Crime in England and Wales: Year Ending. March 2021. Available online: https://www.ons.gov.uk/peoplepopulationandcommunity/crimeandjustice/bulletins/crimeinenglandandwales/yearendingmarch2021 (accessed on 1 December 2021).
- Yang, M.; Chen, Z.; Zhou, M.; Liang, X.; Bai, Z. The Impact of COVID-19 on Crime: A Spatial Temporal Analysis in Chicago. ISPRS Int. J. Geo-Inf. 2021, 10, 152. [Google Scholar] [CrossRef]
- Perez-Vincent, S.M.; Schargrodsky, E.; García Mejía, M. Crime under lockdown: The impact of COVID-19 on citizen security in the city of Buenos Aires. Criminol. Public Policy 2021, 20, 463–492. [Google Scholar] [CrossRef]
- Boserup, B.; McKenney, M.; Elkbuli, A. Alarming trends in US domestic violence during the COVID-19 pandemic. Am. J. Emerg. Med. 2020, 38, 2753–2755. [Google Scholar] [CrossRef]
- Vignali, G.; Franceschetti, L.; Merzagora, I. A retrospective study on femicides assessed at the Institute of Legal Medicine of Milan. Are older women at risk? Forensic Sci. Int. 2021, 325, 110890. [Google Scholar] [CrossRef]
- Aolymat, I. A cross-sectional study of the impact of COVID-19 on domestic violence, menstruation, genital tract health, and contraception use among women in Jordan. Am. J. Trop. Med. Hyg. 2021, 104, 519–525. [Google Scholar] [CrossRef]
- Rhodes, H.X.; Petersen, K.; Lunsford, L.; Biswas, S. COVID-19 Resilience for Survival: Occurrence of Domestic Violence During Lockdown at a Rural American College of Surgeons Verified Level One Trauma Center. Cureus 2020, 12, e10059. [Google Scholar] [CrossRef]
- Sediri, S.; Zgueb, Y.; Ouanes, S.; Ouali, U.; Bourgou, S.; Jomli, R.; Nacef, F. Women’s mental health: Acute impact of COVID-19 pandemic on domestic violence. Arch. Women’s Ment. Health 2020, 23, 749–756. [Google Scholar] [CrossRef]
- Hsu, L.C.; Henke, A. COVID-19, staying at home, and domestic violence. Rev. Econ. Househ. 2021, 19, 145–155. [Google Scholar] [CrossRef]
- Yari, A.; Zahednezhad, H.; Gheshlagh, R.G.; Kurdi, A. Frequency and determinants of domestic violence against Iranian women during the COVID-19 pandemic: A national cross-sectional survey. BMC Public Health 2021, 21, 1727. [Google Scholar] [CrossRef]
- Makaroun, L.K.; Bachrach, R.L.; Rosland, A.-M. Elder Abuse in the Time of COVID-19—Increased Risks for Older Adults and Their Caregivers. Am. J. Geriatr. Psychiatry 2020, 28, 876–880. [Google Scholar] [CrossRef]
- Lawson, M.; Piel, M.H.; Simon, M. Child Maltreatment during the COVID-19 Pandemic: Consequences of Parental Job Loss on Psychological and Physical Abuse Towards Children. Child Abuse Negl. 2020, 110, 104709. [Google Scholar] [CrossRef]
- Caron, F.; Plancq, M.-C.; Tourneux, P.; Gouron, R.; Klein, C. Was child abuse underdetected during the COVID-19 lockdown? Arch. Pédiatrie 2020, 27, 399–400. [Google Scholar] [CrossRef]
- Martinkevich, P.; Larsen, L.L.; Græsholt-Knudsen, T.; Hesthaven, G.; Hellfritzsch, M.B.; Petersen, K.K.; Møller-Madsen, B.; Rölfing, J.D. Physical child abuse demands increased awareness during health and socioeconomic crises like COVID-19: A review and education material. Acta Orthop. 2020, 91, 527–533. [Google Scholar] [CrossRef]
- Bouillon-Minois, J.-B.; Clinchamps, M.; Dutheil, F. Coronavirus and Quarantine: Catalysts of Domestic Violence. Violence Against Women 2020, 107780122093519. [Google Scholar] [CrossRef]
- Roesch, E.; Amin, A.; Gupta, J.; García-Moreno, C. Violence against women during COVID-19 pandemic restrictions. BMJ 2020, 369, 2–3. [Google Scholar] [CrossRef]
- Ertan, D.; El-Hage, W.; Thierrée, S.; Javelot, H.; Hingray, C. COVID-19: Urgency for distancing from domestic violence. Eur. J. Psychotraumatol. 2020, 11, 1800245. [Google Scholar] [CrossRef] [PubMed]
- Sharma, A.; Borah, S.B. COVID-19 and Domestic Violence: An Indirect Path to Social and Economic Crisis. J. Fam. Violence 2020, 2667, 1–7. [Google Scholar] [CrossRef]
- Ortega Pacheco, Y.J.; Martínez Rudas, M. Domestic violence and COVID-19 in Colombia. Psychiatry Res. 2021, 300, 113925. [Google Scholar] [CrossRef] [PubMed]
- Campbell, A.M. Improving prevention of family violence during (and after) disaster: Lessons learned from the COVID-19 pandemic. Forensic Sci. Int. Rep. 2021, 3, 100179. [Google Scholar] [CrossRef]
- Sacco, M.A.; Caputo, F.; Ricci, P.; Sicilia, F.; De Aloe, L.; Bonetta, C.F.; Cordasco, F.; Scalise, C.; Cacciatore, G.; Zibetti, A.; et al. The impact of the COVID-19 pandemic on domestic violence: The dark side of home isolation during quarantine. Med. Leg. J. 2020, 88, 71–73. [Google Scholar] [CrossRef] [PubMed]
- Buil-Gil, D.; Zeng, Y.; Kemp, S. Offline crime bounces back to pre-COVID levels, cyber stays high: Interrupted time-series analysis in Northern Ireland. Crime Sci. 2021, 10, 26. [Google Scholar] [CrossRef] [PubMed]
- Kemp, S.; Buil-Gil, D.; Moneva, A.; Miró-Llinares, F.; Díaz-Castaño, N. Empty Streets, Busy Internet: A Time-Series Analysis of Cybercrime and Fraud Trends During COVID-19. J. Contemp. Crim. Justice 2021, 37, 480–501. [Google Scholar] [CrossRef]
- Griffith, A.K. Parental Burnout and Child Maltreatment During the COVID-19 Pandemic. J. Fam. Violence 2020, 1–7. [Google Scholar] [CrossRef]
- Bradbury-Jones, C.; Isham, L. The pandemic paradox: The consequences of COVID-19 on domestic violence. J. Clin. Nurs. 2020, 29, 2047–2049. [Google Scholar] [CrossRef] [Green Version]
- Jemberie, W.B.; Stewart Williams, J.; Eriksson, M.; Grönlund, A.-S.; Ng, N.; Blom Nilsson, M.; Padyab, M.; Priest, K.C.; Sandlund, M.; Snellman, F.; et al. Substance Use Disorders and COVID-19: Multi-Faceted Problems Which Require Multi-Pronged Solutions. Front. Psychiatry 2020, 11, 714. [Google Scholar] [CrossRef]
- Estévez-Soto, P.R. Crime and COVID-19: Effect of changes in routine activities in Mexico City. Crime Sci. 2021, 10, 15. [Google Scholar] [CrossRef]
- Lapeyre-Mestre, M.; Boucher, A.; Daveluy, A.; Gibaja, V.; Jouanjus, E.; Mallaret, M.; Peyrière, H.; Micallef, J.; Bouquet, E.; Chaouachi, L.; et al. Addictovigilance contribution during COVID-19 epidemic and lockdown in France. Therapies 2020, 75, 343–354. [Google Scholar] [CrossRef]
- Panagiotidis, P.; Rantis, K.; Holeva, V.; Parlapani, E.; Diakogiannis, I. Changes in alcohol use habits in the general population, during the COVID-19 lockdown in greece. Alcohol Alcohol. 2020, 55, 702–704. [Google Scholar] [CrossRef]
- Banducci, A.N.; Weiss, N.H. Caring for patients with posttraumatic stress and substance use disorders during the COVID-19 pandemic. Psychol. Trauma Theory Res. Pract. Policy 2020, 12, S113–S114. [Google Scholar] [CrossRef]
- Ornell, F.; Moura, H.F.; Scherer, J.N.; Pechansky, F.; Kessler, F.H.P.; von Diemen, L. The COVID-19 pandemic and its impact on substance use: Implications for prevention and treatment. Psychiatry Res. 2020, 289, 113096. [Google Scholar] [CrossRef]
- Baillargeon, J.; Polychronopoulou, E.; Kuo, Y.F.; Raji, M.A. The impact of substance use disorder on COVID-19 outcomes. Psychiatr. Serv. 2021, 72, 578–581. [Google Scholar] [CrossRef]
- Wen, H.; Barnett, M.L.; Saloner, B. Clinical Risk Factors for COVID-19 Among People with Substance Use Disorders. Psychiatr. Serv. 2020, 71, 1308. [Google Scholar] [CrossRef]
- Zaami, S.; Marinelli, E.; Varì, M.R. New Trends of Substance Abuse During COVID-19 Pandemic: An International Perspective. Front. Psychiatry 2020, 11, 700. [Google Scholar] [CrossRef]
- Killgore, W.D.S.; Cloonan, S.A.; Taylor, E.C.; Lucas, D.A.; Dailey, N.S. Alcohol dependence during COVID-19 lockdowns. Psychiatry Res. 2021, 296, 113676. [Google Scholar] [CrossRef]
- López-Pelayo, H.; Aubin, H.-J.; Drummond, C.; Dom, G.; Pascual, F.; Rehm, J.; Saitz, R.; Scafato, E.; Gual, A. “The post-COVID era”: Challenges in the treatment of substance use disorder (SUD) after the pandemic. BMC Med. 2020, 18, 241. [Google Scholar] [CrossRef]
- Di Trana, A.; Carlier, J.; Berretta, P.; Zaami, S.; Ricci, G. Consequences of COVID-19 Lockdown on the Misuse and Marketing of Addictive Substances and New Psychoactive Substances. Front. Psychiatry 2020, 11, 1130. [Google Scholar] [CrossRef] [PubMed]
- White, M.D.; Fradella, H.F. Policing a Pandemic: Stay-at-Home Orders and What they Mean for the Police. Am. J. Crim. Justice 2020, 45, 702–717. [Google Scholar] [CrossRef] [PubMed]
- European Parliament the Role of Armed Forces in the Fight against Coronavirus. Available online: https://www.europarl.europa.eu/RegData/etudes/BRIE/2020/649401/EPRS_BRI(2020)649401_EN.pdf (accessed on 1 December 2021).
- Hansen, J.A.; Lory, G.L. Rural Victimization and Policing during the COVID-19 Pandemic. Am. J. Crim. Justice 2020, 45, 731–742. [Google Scholar] [CrossRef] [PubMed]
- Campbell, A.M. An increasing risk of family violence during the COVID-19 pandemic: Strengthening community collaborations to save lives. Forensic Sci. Int. Rep. 2020, 2, 100089. [Google Scholar] [CrossRef]
- Salerno, M.; Sessa, F.; Piscopo, A.; Montana, A.; Torrisi, M.; Patanè, F.; Murabito, P.; Volti, G.L.; Pomara, C. No Autopsies on COVID-19 Deaths: A Missed Opportunity and the Lockdown of Science. J. Clin. Med. 2020, 9, 1472. [Google Scholar] [CrossRef]
- Barranco, R.; Ventura, F. The role of forensic pathologists in coronavirus disease 2019 infection: The importance of an interdisciplinary research. Med. Sci. Law 2020, 60, 237–238. [Google Scholar] [CrossRef]
- Sessa, F.; Salerno, M.; Pomara, C. Autopsy Tool in Unknown Diseases: The Experience with Coronaviruses (SARS-CoV, MERS-CoV, SARS-CoV-2). Medicina 2021, 57, 309. [Google Scholar] [CrossRef]
- Pomara, C.; Li Volti, G.; Cappello, F. COVID-19 Deaths: Are We Sure It Is Pneumonia? Please, Autopsy, Autopsy, Autopsy! J. Clin. Med. 2020, 9, 1259. [Google Scholar] [CrossRef]
- Baj, J.; Ciesielka, M.; Buszewicz, G.; Maciejewski, R.; Budzyńska, B.; Listos, P.; Teresiński, G. COVID-19 in the autopsy room-requirements, safety, recommendations and pathological findings. Forensic Sci. Med. Pathol. 2021, 17, 101–113. [Google Scholar] [CrossRef]
- Teresiński, G.; Jurek, T. Recommendations of the Polish Society of Forensic Medicine and Criminology and National Consultant for forensic medicine with regard to performing forensic post-mortem examinations in case of confirmed COVID-19 disease and suspected SARS CoV-2 infections. Arch. Med. Sadowej Kryminol. 2019, 69, 147–157. [Google Scholar]
- Centers for Disease Control and Prevention Collection and Submission of Postmortem Specimens from Deceased Persons with Known or Suspected COVID-19. Available online: https://eaaf.org/wp-content/uploads/covid19-PDFs/EEUU/CDC-guidance-postmortem-specimens.pdf (accessed on 18 August 2020).
- Osborn, M.; Lucas, S.B.; Stewart, R.; Swift, B.; Youd, E. Autopsy Practice Relating to Possible Cases of COVID-19 (2019-nCov, Novel Coronavirus from China 2019/2020). Available online: https://www.rcpath.org/uploads/assets/d5e28baf-5789-4b0f-acecfe370eee6223/447e37d0-29dd-4994-a11fe27b93de0905/Briefing-on-COVID-19-autopsy-Feb-2020.pdf (accessed on 18 August 2020).
- Wichmann, D.; Sperhake, J.-P.; Lütgehetmann, M.; Steurer, S.; Edler, C.; Heinemann, A.; Heinrich, F.; Mushumba, H.; Kniep, I.; Schröder, A.S.; et al. Autopsy Findings and Venous Thromboembolism in Patients with COVID-19. Ann. Intern. Med. 2020, 173, 268–277. [Google Scholar] [CrossRef] [PubMed]
- Wang, C.; Xie, J.; Zhao, L.; Fei, X.; Zhang, H.; Tan, Y.; Nie, X.; Zhou, L.; Liu, Z.; Ren, Y.; et al. Alveolar macrophage dysfunction and cytokine storm in the pathogenesis of two severe COVID-19 patients. EBioMedicine 2020, 57, 102833. [Google Scholar] [CrossRef]
- Nienhold, R.; Ciani, Y.; Koelzer, V.H.; Tzankov, A.; Haslbauer, J.D.; Menter, T.; Schwab, N.; Henkel, M.; Frank, A.; Zsikla, V.; et al. Two distinct immunopathological profiles in autopsy lungs of COVID-19. Nat. Commun. 2020, 11, 5086. [Google Scholar] [CrossRef]
- Borczuk, A.C.; Salvatore, S.P.; Seshan, S.V.; Patel, S.S.; Bussel, J.B.; Mostyka, M.; Elsoukkary, S.; He, B.; Del Vecchio, C.; Fortarezza, F.; et al. COVID-19 pulmonary pathology: A multi-institutional autopsy cohort from Italy and New York City. Mod. Pathol. 2020, 33, 2156–2168. [Google Scholar] [CrossRef]
- Fox, S.E.; Akmatbekov, A.; Harbert, J.L.; Li, G.; Quincy Brown, J.; Vander Heide, R.S. Pulmonary and cardiac pathology in African American patients with COVID-19: An autopsy series from New Orleans. Lancet Respir. Med. 2020, 8, 681–686. [Google Scholar] [CrossRef]
- Ackermann, M.; Verleden, S.E.; Kuehnel, M.; Haverich, A.; Welte, T.; Laenger, F.; Vanstapel, A.; Werlein, C.; Stark, H.; Tzankov, A.; et al. Pulmonary Vascular Endothelialitis, Thrombosis, and Angiogenesis in COVID-19. N. Engl. J. Med. 2020, 383, 120–128. [Google Scholar] [CrossRef]
- Varga, Z.; Flammer, A.J.; Steiger, P.; Haberecker, M.; Andermatt, R.; Zinkernagel, A.S.; Mehra, M.R.; Schuepbach, R.A.; Ruschitzka, F.; Moch, H. Endothelial cell infection and endotheliitis in COVID-19. Lancet 2020, 395, 1417–1418. [Google Scholar] [CrossRef]
- Cipolloni, L.; Sessa, F.; Bertozzi, G.; Baldari, B.; Cantatore, S.; Testi, R.; D’Errico, S.; Di Mizio, G.; Asmundo, A.; Castorina, S.; et al. Preliminary post-mortem COVID-19 evidence of endothelial injury and factor VIII hyperexpression. Diagnostics 2020, 10, 575. [Google Scholar] [CrossRef]
- Barone, R.; Marino Gammazza, A.; Paladino, L.; Pitruzzella, A.; Spinoso, G.; Salerno, M.; Sessa, F.; Pomara, C.; Cappello, F.; Rappa, F. Morphological Alterations and Stress Protein Variations in Lung Biopsies Obtained from Autopsies of COVID-19 Subjects. Cells 2021, 10, 3136. [Google Scholar] [CrossRef]
- Mukerji, S.S.; Solomon, I.H. What can we learn from brain autopsies in COVID-19? Neurosci. Lett. 2021, 742, 135528. [Google Scholar] [CrossRef]
- Matschke, J.; Lütgehetmann, M.; Hagel, C.; Sperhake, J.P.; Schröder, A.S.; Edler, C.; Mushumba, H.; Fitzek, A.; Allweiss, L.; Dandri, M.; et al. Neuropathology of patients with COVID-19 in Germany: A post-mortem case series. Lancet Neurol. 2020, 19, 919–929. [Google Scholar] [CrossRef]
- Reichard, R.R.; Kashani, K.B.; Boire, N.A.; Constantopoulos, E.; Guo, Y.; Lucchinetti, C.F. Neuropathology of COVID-19: A spectrum of vascular and acute disseminated encephalomyelitis (ADEM)-like pathology. Acta Neuropathol. 2020, 140, 1–6. [Google Scholar] [CrossRef] [PubMed]
- Rhodes, R.H.; Love, G.L.; Lameira, F.D.S.; Sadough, M.S.; Fox, S.E.; Vander Heide, R. Acute Endotheliitis (Type 3 Hypersensitivity Vasculitis) in Ten COVID-19 Autopsy Brains. medRxiv 2021. [Google Scholar] [CrossRef]
- Lindner, D.; Fitzek, A.; Bräuninger, H.; Aleshcheva, G.; Edler, C.; Meissner, K.; Scherschel, K.; Kirchhof, P.; Escher, F.; Schultheiss, H.P.; et al. Association of Cardiac Infection with SARS-CoV-2 in Confirmed COVID-19 Autopsy Cases. JAMA Cardiol. 2020, 5, 1281–1285. [Google Scholar] [CrossRef]
- Schaller, T.; Hirschbühl, K.; Burkhardt, K.; Braun, G.; Trepel, M.; Märkl, B.; Claus, R. Postmortem Examination of Patients With COVID-19. JAMA 2020, 323, 2518–2520. [Google Scholar] [CrossRef]
- Unudurthi, S.D.; Luthra, P.; Bose, R.J.C.; McCarthy, J.; Kontaridis, M.I. Cardiac inflammation in COVID-19: Lessons from heart failure. Life Sci. 2020, 260, 118482. [Google Scholar] [CrossRef]
- Roshdy, A.; Zaher, S.; Fayed, H.; Coghlan, J.G. COVID-19 and the Heart: A Systematic Review of Cardiac Autopsies. Front. Cardiovasc. Med. 2021, 7, 400. [Google Scholar] [CrossRef]
- Fassan, M.; Mescoli, C.; Sbaraglia, M.; Guzzardo, V.; Russo, F.P.; Fabris, R.; Trevenzoli, M.; Pelizzaro, F.; Cattelan, A.M.; Basso, C.; et al. Liver histopathology in COVID-19 patients: A mono-Institutional series of liver biopsies and autopsy specimens. Pathol. Res. Pract. 2021, 221, 153451. [Google Scholar] [CrossRef]
- Schmit, G.; Lelotte, J.; Vanhaebost, J.; Horsmans, Y.; Van Bockstal, M.; Baldin, P. The Liver in COVID-19-Related Death: Protagonist or Innocent Bystander? Pathobiology 2020, 88, 88–94. [Google Scholar] [CrossRef]
- Batlle, D.; Soler, M.J.; Sparks, M.A.; Hiremath, S.; South, A.M.; Welling, P.A.; Swaminathan, S. Acute Kidney Injury in COVID-19: Emerging Evidence of a Distinct Pathophysiology. J. Am. Soc. Nephrol. 2020, 31, 1380–1383. [Google Scholar] [CrossRef]
- Mondello, C.; Roccuzzo, S.; Malfa, O.; Sapienza, D.; Gualniera, P.; Ventura Spagnolo, E.; Di Nunno, N.; Salerno, M.; Pomara, C.; Asmundo, A. Pathological Findings in COVID-19 as a Tool to Define SARS-CoV-2 Pathogenesis. A Systematic Review. Front. Pharmacol. 2021, 12, 614586. [Google Scholar] [CrossRef] [PubMed]
- Bogdanović, M.; Atanasijević, T.; Popović, V.; Mihailović, Z.; Radnić, B.; Durmić, T. Is the role of forensic medicine in the COVID-19 pandemic underestimated? Forensic Sci. Med. Pathol. 2020, 17, 136–138. [Google Scholar] [CrossRef] [PubMed]
- Sessa, F.; Bertozzi, G.; Cipolloni, L.; Baldari, B.; Cantatore, S.; D’Errico, S.; Di Mizio, G.; Asmundo, A.; Castorina, S.; Salerno, M.; et al. Clinical-Forensic Autopsy Findings to Defeat COVID-19 Disease: A Literature Review. J. Clin. Med. 2020, 9, 2026. [Google Scholar] [CrossRef] [PubMed]
- Kevadiya, B.D.; Machhi, J.; Herskovitz, J.; Oleynikov, M.D.; Blomberg, W.R.; Bajwa, N.; Soni, D.; Das, S.; Hasan, M.; Patel, M.; et al. Diagnostics for SARS-CoV-2 infections. Nat. Mater. 2021, 20, 593–605. [Google Scholar] [CrossRef]
- Kampf, G. Potential role of inanimate surfaces for the spread of coronaviruses and their inactivation with disinfectant agents. Infect. Prev. Pract. 2020, 2, 100044. [Google Scholar] [CrossRef]
- Marquès, M.; Domingo, J.L. Contamination of inert surfaces by SARS-CoV-2: Persistence, stability and infectivity. A review. Environ. Res. 2021, 193, 110559. [Google Scholar] [CrossRef]
- WHO Interm Guidance Infection Prevention and Control for the safe management of a dead body in the context of COVID-19. J. Hosp. Infect. 2020, 104, 246–251.
- CDC Collection and Submission of Postmortem Specimens from Deceased Persons with Confirmed or Suspected COVID-19. Available online: https://www.cdc.gov/coronavirus/2019-ncov/hcp/guidance-postmortem-specimens.html (accessed on 11 December 2020).
- Skok, K.; Stelzl, E.; Trauner, M.; Kessler, H.H.; Lax, S.F. Post-mortem viral dynamics and tropism in COVID-19 patients in correlation with organ damage. Virchows Arch. 2020, 478, 343–353. [Google Scholar] [CrossRef]
- Musso, N.; Falzone, L.; Stracquadanio, S.; Bongiorno, D.; Salerno, M.; Esposito, M.; Sessa, F.; Libra, M.; Stefani, S.; Pomara, C. Post-Mortem Detection of SARS-CoV-2 RNA in Long-Buried Lung Samples. Diagnostics 2021, 11, 1158. [Google Scholar] [CrossRef]
- Beltempo, P.; Curti, S.M.; Maserati, R.; Gherardi, M.; Castelli, M. Persistence of SARS-CoV-2 RNA in post-mortem swab 35 days after death: A case report. Forensic Sci. Int. 2021, 319, 110653. [Google Scholar] [CrossRef]
- Ventura, F.; Barranco, R. Cadaveric Nasopharyngeal Swab in Coronavirus Disease 2019 Infections: Can it be Useful for Medico-Legal Purposes? Am. J. Forensic Med. Pathol. 2020, 41, 238–239. [Google Scholar] [CrossRef]
- Plenzig, S.; Holz, F.; Bojkova, D.; Kettner, M.; Cinatl, J.; Verhoff, M.A.; Birngruber, C.G.; Ciesek, S.; Rabenau, H.F. Detection and infectivity of SARS-CoV-2 in exhumated corpses. Int. J. Legal Med. 2021, 135, 2531–2536. [Google Scholar] [CrossRef]
- Pomara, C.; Salerno, M.; Sessa, F.; Esposito, M.; Barchitta, M.; Ledda, C.; Grassi, P.; Liberto, A.; Mattaliano, A.R.; Rapisarda, V.; et al. Safe Management Strategies in Clinical Forensic Autopsies of Confirmed COVID-19 Cases. Diagnostics 2021, 11, 457. [Google Scholar] [CrossRef]
- Pomara, C.; Sessa, F.; Galante, D.; Pace, L.; Fasanella, A.; Di Nunno, N.; Esposito, M.; Salerno, M. Do We Really Need Hazard Prevention at the Expense of Safeguarding Death Dignity in COVID-19? Diagnostics 2021, 11, 1913. [Google Scholar] [CrossRef]
- Plenzig, S.; Bojkova, D.; Held, H.; Berger, A.; Holz, F.; Cinatl, J.; Gradhand, E.; Kettner, M.; Pfeiffer, A.; Verhoff, M.A.; et al. Infectivity of deceased COVID-19 patients. Int. J. Legal Med. 2021, 135, 2055–2060. [Google Scholar] [CrossRef]
- Prajapati, S.; Kaur, S. Safety Recommendations for Forensic Laboratory Staff During COVID-19 Pandemic. Acad. Forensic Pathol. 2021, 11, 94–102. [Google Scholar] [CrossRef]
- Centers for Disease Control and Prevention (CDC) What Law Enforcement Personnel Need to Know about Coronavirus Disease 2019 (COVID-19). Available online: https://www.cdc.gov/coronavirus/2019-ncov/community/guidance-law-enforcement.html (accessed on 1 December 2021).
- OSHA Updated Interim Enforcement Response Plan for Coronavirus Disease 2019 (COVID-19). Available online: https://www.osha.gov/laws-regs/standardinterpretations/2021-07-07 (accessed on 1 December 2021).
- Di Luise, E.; Magni, P.A. Interim recommendations for the management of forensic investigation during the COVID-19 pandemic: An Italian perspective. Sci. Justice 2021, 61, 735–742. [Google Scholar] [CrossRef]
- De Ungria, M.C.A. Forensic DNA testing during the SARS-CoV-2 pandemic. Forensic Sci. Int. Genet. 2020, 48, 102346. [Google Scholar] [CrossRef] [PubMed]
- Roberts, C.h.; Brindle, H.; Rogers, N.T.; Eggo, R.M.; Enria, L.; Lees, S. Vaccine Confidence and Hesitancy at the Start of COVID-19 Vaccine Deployment in the UK: An Embedded Mixed-Methods Study. Front. Public Health 2021, 9, 745630. [Google Scholar] [CrossRef] [PubMed]
- Griva, K.; Tan, K.Y.K.; Chan, F.H.F.; Periakaruppan, R.; Ong, B.W.L.; Soh, A.S.E.; Chen, M.I. Evaluating Rates and Determinants of COVID-19 Vaccine Hesitancy for Adults and Children in the Singapore Population: Strengthening Our Community’s Resilience against Threats from Emerging Infections (SOCRATEs) Cohort. Vaccines 2021, 9, 1415. [Google Scholar] [CrossRef] [PubMed]
- Barranco, R.; Rocca, G.; Molinelli, A.; Ventura, F. Controversies and Challenges of Mass Vaccination against SARS-CoV-2 in Italy: Medico-Legal Perspectives and Considerations. Healthcare 2021, 9, 1163. [Google Scholar] [CrossRef]
- Sessa, F.; Salerno, M.; Esposito, M.; Di Nunno, N.; Zamboni, P.; Pomara, C. Autopsy Findings and Causality Relationship between Death and COVID-19 Vaccination: A Systematic Review. J. Clin. Med. 2021, 10, 5876. [Google Scholar] [CrossRef]
- Zamboni, P.; Scerrati, A.; Sessa, F.; Pomara, C.; Mannucci, P.M. Vaccine-induced immune thrombotic thrombocytopenia with atypical vein thrombosis: Implications for clinical practice. Phlebology 2022, 02683555211068948. [Google Scholar] [CrossRef]
- Schneider, J.; Sottmann, L.; Greinacher, A.; Hagen, M.; Kasper, H.-U.; Kuhnen, C.; Schlepper, S.; Schmidt, S.; Schulz, R.; Thiele, T.; et al. Postmortem investigation of fatalities following vaccination with COVID-19 vaccines. Int. J. Legal Med. 2021, 135, 2335–2345. [Google Scholar] [CrossRef]
- Pomara, C.; Sessa, F.; Ciaccio, M.; Dieli, F.; Esposito, M.; Garozzo, S.F.; Giarratano, A.; Prati, D.; Rappa, F.; Salerno, M.; et al. Post-mortem findings in vaccine-induced thrombotic thombocytopenia. Haematologica 2021, 106, 2291. [Google Scholar] [CrossRef]
- Pomara, C.; Sessa, F.; Ciaccio, M.; Dieli, F.; Esposito, M.; Giammanco, G.M.; Garozzo, S.F.; Giarratano, A.; Prati, D.; Rappa, F.; et al. COVID-19 Vaccine and Death: Causality Algorithm According to the WHO Eligibility Diagnosis. Diagnostics 2021, 11, 955. [Google Scholar] [CrossRef]
- Rosen, B.; Waitzberg, R.; Israeli, A.; Hartal, M.; Davidovitch, N. Addressing vaccine hesitancy and access barriers to achieve persistent progress in Israel’s COVID-19 vaccination program. Isr. J. Health Policy Res. 2021, 10, 43. [Google Scholar] [CrossRef]
- Mathieu, E.; Ritchie, H.; Ortiz-Ospina, E.; Roser, M.; Hasell, J.; Appel, C.; Giattino, C.; Rodés-Guirao, L. A global database of COVID-19 vaccinations. Nat. Hum. Behav. 2021, 5, 947–953. [Google Scholar] [CrossRef]
- Pokhrel, S.; Chhetri, R. A Literature Review on Impact of COVID-19 Pandemic on Teaching and Learning. High. Educ. Futur. 2021, 8, 133–141. [Google Scholar] [CrossRef]
- Tóth, D.; Petrus, K.; Heckmann, V.; Simon, G.; Poór, V.S. Application of photogrammetry in forensic pathology education of medical students in response to COVID-19. J. Forensic Sci. 2021, 66, 1533–1537. [Google Scholar] [CrossRef]
- Thompson, T.J.U.; Collings, A.J.; Earwaker, H.; Horsman, G.; Nakhaeizadeh, S.; Parekh, U. Forensic undergraduate education during and after the COVID-19 imposed lockdown: Strategies and reflections from India and the UK. Forensic Sci. Int. 2020, 316, 110500. [Google Scholar] [CrossRef] [PubMed]
- Jones, R.M. Online teaching of forensic medicine and pathology during the COVID-19 pandemic: A course evaluation. J. Forensic Leg. Med. 2021, 83, 102229. [Google Scholar] [CrossRef] [PubMed]
- Duignan, K.; Bradbury, C. COVID-19 and medical negligence litigation: Immunity for healthcare professionals? Med. Leg. J. 2020, 88, 31–34. [Google Scholar] [CrossRef] [PubMed]
- Martin-Fumadó, C.; Gómez-Durán, E.L.; Benet-Travé, J.; Barbería-Marcalain, E.; Arimany-Manso, J. Liability claims in Spain post-COVID-19: A predictable scenario. Leg. Med. 2020, 47, 101745. [Google Scholar] [CrossRef]
- Bolcato, M.; Aurilio, M.T.; Aprile, A.; Di Mizio, G.; Della Pietra, B.; Feola, A. Take-Home Messages from the COVID-19 Pandemic: Strengths and Pitfalls of the Italian National Health Service from a Medico-Legal Point of View. Healthcare 2020, 9, 17. [Google Scholar] [CrossRef]
- Maiese, A.; Russa, R. La; Santoro, P.; Matteis, A. De; Paolo, M. Di Future litigation after COVID-19 pandemic in Italy. Med. Leg. J. 2021, 89, 148–149. [Google Scholar] [CrossRef]
- Cioffi, A.; Rinaldi, R. COVID-19 and medical liability: A delicate balance. Med. Leg. J. 2020, 88, 187–188. [Google Scholar] [CrossRef]
- Mehta, A.R.; Szakmany, T.; Sorbie, A. The medicolegal landscape through the lens of COVID-19: Time for reform. J. R. Soc. Med. 2021, 114, 55–59. [Google Scholar] [CrossRef]
- Barranco, R.; Messina, C.; Bonsignore, A.; Cattrini, C.; Ventura, F. Medical Liability in Cancer Care During COVID-19 Pandemic: Heroes or Guilty? Front. Public Health 2020, 8, 896. [Google Scholar] [CrossRef]
- Nioi, M.; Napoli, P.E.; Finco, G.; Demontis, R.; Fossarello, M.; D’aloja, E. Fear of the COVID-19 and medical liability. Insights from a series of 130 consecutives medico-legal claims evaluated in a single institution during SARS-CoV-2-related pandemic. Signa Vitae 2021, 17, 79–85. [Google Scholar]
- Barranco, R.; Vallega Bernucci Du Tremoul, L.; Ventura, F. Hospital-Acquired SARS-Cov-2 Infections in Patients: Inevitable Conditions or Medical Malpractice? Int. J. Environ. Res. Public Health 2021, 18, 489. [Google Scholar] [CrossRef]
- Close, E.; Willmott, L.; Cockburn, T.; Young, S.; Cairns, W.; White, B.P. Transparent triage policies during the COVID-19 pandemic: A critical part of medico-legal risk management for clinicians. Med. J. Aust. 2021, 215, 71. [Google Scholar] [CrossRef]
- Perrone, G.; Zerbo, S.; Bilotta, C.; Malta, G.; Argo, A. Telemedicine during COVID-19 pandemic: Advantage or critical issue? Med. Leg. J. 2020, 88, 76–77. [Google Scholar] [CrossRef]
- Pomara, C.; Li Volti, G.; Cappello, F. The post-lockdown era: What is next in Italy? Front. Pharmacol. 2020, 11, 1074. [Google Scholar] [CrossRef]
- Barranco, R.; Errico, S.; Ventura, F. Letter to the Editor: Risk of Suicide in People Whose Family Members Have Died from COVID-19: The Importance of an Empathetic Relationship in Medical Care and Psychological Help. Popul. Health Manag. 2021, 24, 525. [Google Scholar] [CrossRef]
- FDA Fraudulent Coronavirus Disease 2019 (COVID-19) Products. Available online: https://www.fda.gov/consumers/health-fraud-scams/fraudulent-coronavirus-disease-2019-covid-19-products (accessed on 14 December 2021).
- Turillazzi, E.; Riezzo, I.; Neri, M.; Pomara, C.; Cecchi, R.; Fineschi, V. The diagnosis of fatal pulmonary fat embolism using quantitative morphometry and confocal laser scanning microscopy. Pathol. Res. Pract. 2008, 204, 259–266. [Google Scholar] [CrossRef]
- Melo, D.N.; Mara Coelho, T.; Rolim Pinheiro Lima, G.; Gomes Fernandes, C.; Cavalcante Fales de Brito Alves, B.; Montenegro de Carvalho Araújo, F.; Aparecida de Almeida Monteiro, R.; Ordi, J.; Hilário do Nascimento Saldiva, P.; Pamplona de Góes Cavalcanti, L. Use of minimally invasive autopsy during the COVID-19 pandemic and its possibilities in the context of developing countries. PLoS Negl. Trop. Dis. 2021, 15, e0009629. [Google Scholar] [CrossRef]
- Nioi, M.; Napoli, P.E.; Fossarello, M.; d’Aloja, E. Autopsies and Asymptomatic Patients During the COVID-19 Pandemic: Balancing Risk and Reward. Front. Public Health 2020, 8, 739. [Google Scholar] [CrossRef]
- Bilotta, C.; Zerbo, S.; Perrone, G.; Malta, G.; Argo, A. The medico-legal implications in medical malpractice claims during COVID-19 pandemic: Increase or trend reversal? Med. Leg. J. 2020, 88, 35–37. [Google Scholar] [CrossRef]

Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Esposito, M.; Salerno, M.; Scoto, E.; Di Nunno, N.; Sessa, F. The Impact of the COVID-19 Pandemic on the Practice of Forensic Medicine: An Overview. Healthcare 2022, 10, 319. https://doi.org/10.3390/healthcare10020319
Esposito M, Salerno M, Scoto E, Di Nunno N, Sessa F. The Impact of the COVID-19 Pandemic on the Practice of Forensic Medicine: An Overview. Healthcare. 2022; 10(2):319. https://doi.org/10.3390/healthcare10020319
Chicago/Turabian StyleEsposito, Massimiliano, Monica Salerno, Edmondo Scoto, Nunzio Di Nunno, and Francesco Sessa. 2022. "The Impact of the COVID-19 Pandemic on the Practice of Forensic Medicine: An Overview" Healthcare 10, no. 2: 319. https://doi.org/10.3390/healthcare10020319