Radiological and Functional Pulmonary Evolution in Post-COVID-19 Patients: An Observational Study
Abstract
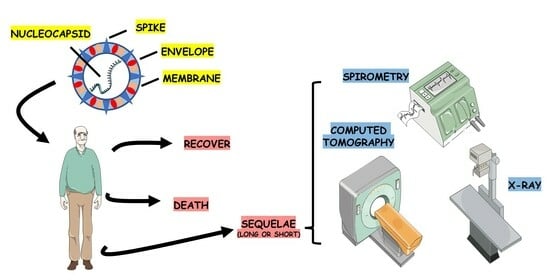
:1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Statistics
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Esakandari, H.; Nabi-Afjadi, M.; Fakkari-Afjadi, J.; Farahmandian, N.; Miresmaeili, S.-M.; Bahreini, E. A comprehensive review of COVID-19 characteristics. Biol. Proced. Online 2020, 22, 19. [Google Scholar] [CrossRef] [PubMed]
- Cox, L.; Alfredsson, E.; Psouni, E. Coparent exclusion, prenatal experiences, and mental health during COVID-19 in Sweden. J. Fam. Psychol. 2023. [Google Scholar] [CrossRef]
- Hu, B.; Guo, H.; Zhou, P.; Shi, Z.-L. Characteristics of SARS-CoV-2 and COVID-19. Nat. Rev. Microbiol. 2021, 19, 141–154. [Google Scholar] [CrossRef] [PubMed]
- Rosa, R.G.; Cavalcanti, A.B.; Azevedo, L.C.P.; Veiga, V.C.; de Souza, D.; da Rosa Minho dos Santos, R.; de Carli Schardosim, R.F.; Rech, G.S.; Trott, G.; Schneider, D.; et al. Association between acute disease severity and one-year quality of life among post-hospitalisation COVID-19 patients: Coalition VII prospective cohort study. Intensive Care Med. 2023, 49, 166–177. [Google Scholar] [CrossRef] [PubMed]
- Barbalho, S.M.; Minniti, G.; Miola, V.F.B.; Haber, J.F.D.S.; Bueno, P.C.D.S.; de Argollo Haber, L.S.; Girio, R.; Detregiachi, C.R.P.; Dall, C.T.; Rodrigues, V.D.; et al. Organokines in COVID-19: A Systematic Review. Cell 2023, 12, 1349. [Google Scholar] [CrossRef]
- Churruca, M.; Martínez-Besteiro, E.; Couñago, F.; Landete, P. COVID-19 pneumonia: A review of typical radiological characteristics. World J. Radiol. 2021, 13, 327. [Google Scholar] [CrossRef]
- Huang, C.; Wang, Y.; Li, X.; Ren, L.; Zhao, J.; Hu, Y.; Zhang, L.; Fan, G.; Xu, J.; Gu, X. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet 2020, 395, 497–506. [Google Scholar] [CrossRef]
- Kiener, M.; Roldan, N.; Machahua, C.; Sengupta, A.; Geiser, T.; Guenat, O.T.; Funke-Chambour, M.; Hobi, N.; Kruithof-de Julio, M. Human-based advanced in vitro approaches to investigate lung fibrosis and pulmonary effects of COVID-19. Front. Med. 2021, 8, 644678. [Google Scholar] [CrossRef]
- To, K.K.-W.; Sridhar, S.; Chiu, K.H.-Y.; Hung, D.L.-L.; Li, X.; Hung, I.F.-N.; Tam, A.R.; Chung, T.W.-H.; Chan, J.F.-W.; Zhang, A.J.-X.; et al. Lessons learned 1 year after SARS-CoV-2 emergence leading to COVID-19 pandemic. Emerg. Microbes Infect. 2021, 10, 507–535. [Google Scholar] [CrossRef]
- Guan, W.; Ni, Z.; Hu, Y.; Liang, W.; Ou, C.; He, J.; Liu, L.; Shan, H.; Lei, C.; Hui, D.S. Clinical characteristics of coronavirus disease 2019 in China. N. Engl. J. Med. 2020, 382, 1708–1720. [Google Scholar] [CrossRef]
- Su, W.L.; Lu, K.C.; Chan, C.Y.; Chao, Y.C. COVID-19 and the lungs: A review. J. Infect. Public Health 2021, 14, 1708–1714. [Google Scholar] [CrossRef]
- Fugazzaro, S.; Contri, A.; Esseroukh, O.; Kaleci, S.; Croci, S.; Massari, M.; Facciolongo, N.C.; Besutti, G.; Iori, M.; Salvarani, C.; et al. Rehabilitation interventions for post-acute COVID-19 syndrome: A systematic review. Int. J. Environ. Res. Public Health 2022, 19, 5185. [Google Scholar] [CrossRef]
- Mogami, R.; Araújo Filho, R.C.; Chantong, C.; Gianella, C.; Santos de Almeida, F.C.; Baptista Koifman, A.C.; Jauregui, G.F.; Mafort, T.T.; da Silva Bessa da Costa, H.; Peres dos Santos, G.A.; et al. The Importance of Radiological Patterns and Small Airway Disease in Long-Term Follow-Up of Postacute COVID-19: A Preliminary Study. Radiol. Res. Pract. 2022, 2022, 7919033. [Google Scholar] [CrossRef]
- Sanli, D.E.T.; Yildirim, D.; Sanli, A.N.; Turkmen, S.; Erozan, N.; Husmen, G.; Altundag, A.; Tuzuner, F. A practical approach to imaging characteristics and standardized reporting of COVID-19: A radiologic review. Mil. Med. Res. 2021, 8, 7. [Google Scholar] [CrossRef]
- Awulachew, E.; Diriba, K.; Anja, A.; Getu, E.; Belayneh, F. Computed tomography (CT) imaging features of patients with COVID-19: Systematic review and meta-analysis. Radiol. Res. Pract. 2020, 2020, 1023506. [Google Scholar] [CrossRef]
- Islam, N.; Ebrahimzadeh, S.; Salameh, J.-P.; Kazi, S.; Fabiano, N.; Treanor, L.; Absi, M.; Hallgrimson, Z.; Leeflang, M.M.; Hooft, L. Thoracic imaging tests for the diagnosis of COVID-19. Cochrane Database Syst. Rev. 2021. [Google Scholar]
- Sharif, P.M.; Nematizadeh, M.; Saghazadeh, M.; Saghazadeh, A.; Rezaei, N.J. Computed tomography scan in COVID-19: A systematic review and meta-analysis. Pol. J. Radiol. 2022, 87, e1–e23. [Google Scholar] [CrossRef]
- Kotzé, P.B.; Manthey, R.; Griffith-Richards, S.; Ackermann, C.; Klusmann, K. Computed tomography chest findings in post-acute COVID-19 lung disease at a South African regional hospital—A descriptive study. Pan Afr. Med. J. 2023, 44, 175. [Google Scholar] [CrossRef]
- Lehmann, A.; Gysan, M.; Bernitzky, D.; Bal, C.; Prosch, H.; Zehetmayer, S.; Milos, R.-I.; Vonbank, K.; Pohl, W.; Idzko, M. Comparison of pulmonary function test, diffusion capacity, blood gas analysis and CT scan in patients with and without persistent respiratory symptoms following COVID-19. BMC Pulm. Med. 2022, 22, 196. [Google Scholar] [CrossRef]
- Niyatiwatchanchai, N.; Deesomchok, A.; Chaiwong, W.; Duangjit, P.; Pothirat, C.; Liwsrisakun, C.; Bumroongkit, C.; Theerakittikul, T.; Limsukon, A.; Tajarernmuang, P. Comparative study of early impacts of post-COVID-19 pneumonia on clinical manifestations, pulmonary function, and chest radiographs. Medicina 2022, 58, 216. [Google Scholar] [CrossRef]
- Sahin, M.E.; Gökçek, A.; Satar, S.; Ergün, P. Relation of impulse oscillometry and spirometry with quantitative thorax computed tomography after COVID-19 pneumonia. Rev. Da Assoc. Med. Bras. 2023, 69, e20221427. [Google Scholar] [CrossRef]
- Jutant, E.-M.; Meyrignac, O.; Beurnier, A.; Jaïs, X.; Pham, T.; Morin, L.; Boucly, A.; Bulifon, S.; Figueiredo, S.; Harrois, A. Respiratory symptoms and radiological findings in post-acute COVID-19 syndrome. ERJ Open Res. 2022, 8. [Google Scholar] [CrossRef]
- Munker, D.; Veit, T.; Barton, J.; Mertsch, P.; Mümmler, C.; Osterman, A.; Khatamzas, E.; Barnikel, M.; Hellmuth, J.C.; Münchhoff, M. Pulmonary function impairment of asymptomatic and persistently symptomatic patients 4 months after COVID-19 according to disease severity. Infection 2021, 50, 157–168. [Google Scholar] [CrossRef]
- Stavrou, V.T.; Vavougios, G.D.; Kalogiannis, P.; Tachoulas, K.; Touloudi, E.; Astara, K.; Mysiris, D.S.; Tsirimona, G.; Papayianni, E.; Boutlas, S. Breathlessness and exercise with virtual reality system in long-post-coronavirus disease 2019 patients. Front. Public Health 2023, 11, 1115393. [Google Scholar] [CrossRef]
- Péterfi, A.; Mészáros, Á.; Szarvas, Z.; Pénzes, M.; Fekete, M.; Fehér, Á.; Lehoczki, A.; Csípő, T.; Fazekas-Pongor, V. Comorbidities and increased mortality of COVID-19 among the elderly: A systematic review. Physiol. Int. 2022, 109, 163–176. [Google Scholar] [CrossRef]
- Üçsular, F.D.; Karadeniz, G.; Polat, G.; Ayrancı, A.; Yalnız, E.; Kazankaya, F.; Güldaval, F.; Büyükşirin, M.; Anar, C. Clinical Differences Between Elderly and Non-elderly Patients with COVID-19. Turk. Thorac. J. 2022, 23, 238. [Google Scholar] [CrossRef]
- Watanabe, J.H.; Kwon, J.; Mehta, S.R. Association of Age and Hospitalization Amongst Those with Underlying High-risk Conditions at COVID-19 Diagnosis in a Large, State-wide Health System. J. Gen. Intern. Med. 2021, 36, 2906–2908. [Google Scholar] [CrossRef]
- Navarro, A.O.; Cervantes-Bojalil, J.; de Jesús Cobos Quevedo, O.; Martínez, A.A.; Hernández-Jiménez, C.A.; Álvarez, E.P.; Gil, A.G.; Amaro, A.L.P.; Vera-Lastra, O.; Luis, B.A.L. Decreased quality of life and spirometric alterations even after mild-moderate COVID-19. Respir. Med. 2021, 181, 106391. [Google Scholar] [CrossRef]
- Nalbandian, A.; Desai, A.D.; Wan, E.Y. Post-COVID-19 condition. Annu. Rev. Med. 2023, 74, 55–64. [Google Scholar] [CrossRef]
- Lam, I.C.H.; Wong, C.K.H.; Zhang, R.; Chui, C.S.L.; Lai, F.T.T.; Li, X.; Chan, E.W.Y.; Luo, H.; Zhang, Q.; Man, K.K.C. Long-term post-acute sequelae of COVID-19 infection: A retrospective, multi-database cohort study in Hong Kong and the UK. EClinicalMedicine 2023, 60, 102000. [Google Scholar] [CrossRef]
- Salamanna, F.; Veronesi, F.; Martini, L.; Landini, M.P.; Fini, M. Post-COVID-19 syndrome: The persistent symptoms at the post-viral stage of the disease. A systematic review of the current data. Front. Med. 2021, 8, 392. [Google Scholar] [CrossRef] [PubMed]
- Nalbandian, A.; Sehgal, K.; Gupta, A.; Madhavan, M.V.; McGroder, C.; Stevens, J.S.; Cook, J.R.; Nordvig, A.S.; Shalev, D.; Sehrawat, T.S. Post-acute COVID-19 syndrome. Nat. Med. 2021, 27, 601–615. [Google Scholar] [CrossRef]
- Peghin, M.; Palese, A.; Venturini, M.; De Martino, M.; Gerussi, V.; Graziano, E.; Bontempo, G.; Marrella, F.; Tommasini, A.; Fabris, M.; et al. Post-COVID-19 symptoms 6 months after acute infection among hospitalized and non-hospitalized patients. Clin. Microbiol. Infect. 2021, 27, 1507–1513. [Google Scholar] [CrossRef] [PubMed]
- Santos, R.; Barros, D.; Moraes, T.; Hayashi, C.; Ralio, R.; Minenelli, F.; van Zon, K.; Ripardo, J. Clinical characteristics and outcomes of hospitalized COVID-19 patients in a Brazilian Hospital-A retrospective study comprising first and second waves. IJID Reg. 2022, 3, 189–195. [Google Scholar] [CrossRef] [PubMed]
- Parashar, R.; Joshi, A.; Raghuwanshi, P.; Joshi, R.; Hulke, S.; Sharma, J.P.; Joshi, A. Patterns and Trajectories of Pulmonary Function in Coronavirus Disease 2019 Survivors: An Exploratory Study Conducted in Central India. Cureus 2022, 14. [Google Scholar] [CrossRef]
- Zuo, H. Contribution of CT Features in the Diagnosis of COVID-19. Can. Respir. J. 2020, 2020, 1237418. [Google Scholar] [CrossRef]
- Pan, F.; Yang, L.; Liang, B.; Ye, T.; Li, L.; Li, L.; Liu, D.; Wang, J.; Hesketh, R.L.; Zheng, C. Chest CT Patterns from Diagnosis to 1 Year of Follow-up in Patients with COVID-19. Radiology 2022, 302, 709–719. [Google Scholar] [CrossRef]
- Corsi, A.; Caroli, A.; Bonaffini, P.A.; Conti, C.; Arrigoni, A.; Mercanzin, E.; Imeri, G.; Anelli, M.; Balbi, M.; Pace, M. Structural and functional pulmonary assessment in severe COVID-19 survivors at 12 months after discharge. Tomography 2022, 8, 2588–2603. [Google Scholar] [CrossRef]
- Watanabe, A.; So, M.; Iwagami, M.; Fukunaga, K.; Takagi, H.; Kabata, H.; Kuno, T. One-year follow-up CT findings in COVID-19 patients: A systematic review and meta-analysis. Respirology 2022, 27, 605–616. [Google Scholar] [CrossRef]
- Lerum, T.V.; Meltzer, C.; Rodriguez, J.R.; Aaløkken, T.M.; Brønstad, E.; Aarli, B.B.; Aarberg-Lund, K.M.; Durheim, M.T.; Ashraf, H.; Einvik, G.; et al. A prospective study of pulmonary outcomes and chest computed tomography in the first year after COVID-19. ERJ Open Res. 2023, 9, 00575. [Google Scholar] [CrossRef]
- Bongiovanni, M.; Barilaro, G.; Bini, F. Twelve-month clinical, functional, and radiological outcomes in patients hospitalized for SARS-CoV-2 pneumonia. J. Med. Virol. 2023, 95, e28524. [Google Scholar] [CrossRef] [PubMed]


| Variable | Category | Year of Collection | ||||||
|---|---|---|---|---|---|---|---|---|
| 2020 (n = 41) | 2021 (n = 146) | 2022 (n = 115) | p-Value | |||||
| f | % | f | % | f | % | |||
| Sex | Female | 24 | 58.5 | 85 | 58.2 | 75 | 65.2 | 0.303 |
| Male | 17 | 41.5 | 61 | 41.8 | 40 | 34.8 | ||
| Age range | <40 years | 10 | 24.4 | 45 | 30.8 | 31 | 27.0 | 0.634 |
| 40–59 years | 13 | 31.7 | 74 | 50.7 | 40 | 34.8 | ||
| >59 years | 18 | 43.9 | 27 | 18.5 | 44 | 38.3 | ||
| Priority treatment | Domiciliary | 28 | 68.3 | 96 | 65.8 | 110 | 95.7 | <0.001 * |
| Hospital | 13 | 31.7 | 50 | 34.2 | 5 | 4.3 | ||
| Intensive Care Unit | No | 30 | 73.2 | 129 | 88.4 | 114 | 99.1 | <0.001 * |
| Yes | 11 | 26.8 | 17 | 11.6 | 1 | 0.9 | ||
| Orotracheal intubation | No | 35 | 85.4 | 133 | 91.1 | 115 | 100.0 | <0.001 * |
| Yes | 6 | 14.6 | 13 | 8.9 | 0 | 0.0 | ||
| Asthma | No | 33 | 80.5 | 122 | 83.6 | 76 | 66.1 | 0.006 * |
| Yes | 8 | 19.5 | 24 | 16.4 | 39 | 33.9 | ||
| COPD | No | 38 | 92.7 | 144 | 98.6 | 100 | 87.0 | 0.015 * |
| Yes | 3 | 7.3 | 2 | 1.4 | 15 | 13.0 | ||
| Hypertension | No | 30 | 73.2 | 122 | 83.6 | 86 | 74.8 | 0.630 |
| Yes | 11 | 26.8 | 24 | 16.4 | 29 | 25.2 | ||
| Diabetes | No | 38 | 92.7 | 135 | 92.5 | 109 | 94.8 | 0.516 |
| Yes | 3 | 7.3 | 11 | 7.5 | 6 | 5.2 | ||
| Smoke | No | 32 | 78.0 | 128 | 87.7 | 95 | 82.6 | 0.904 |
| Yes | 9 | 22.0 | 18 | 12.3 | 20 | 17.4 | ||
| Category | f | % | p-Value | |
|---|---|---|---|---|
| Normalization of chest tomography | Initial | 8 | 4.2 | <0.001 * |
| <6 months | 96 | 50.3 | ||
| 6–12 months | 44 | 23.0 | ||
| >12 months | 10 | 5.2 | ||
| No normalization | 33 | 17.3 | ||
| Total | 191 | 100.0 | ||
| Normalization of spirometry | <6 months | 35 | 61.4 | <0.001 * |
| 6–12 months | 7 | 12.3 | ||
| >12 months | 4 | 7.0 | ||
| No normalization | 11 | 19.3 | ||
| Total | 57 | 100.0 |
| Variable | Category | Normalization CT (n = 191) | p-Value | |||||
|---|---|---|---|---|---|---|---|---|
| Initial | <6 Months | 6–12 Months | >12 Months | Not Normalized | ||||
| Priority treatment | Home | f (%) | 8 (100.0) | 82 (85.4) | 21 (47.7) | 4 (40.0) | 12 (36.4) | <0.001 * |
| Hospital | f (%) | 0 (0.0) | 14 (14.6) | 23 (52.3) | 6 (60.0) | 21 (63.6) | ||
| Intensive Care Unit | No | f (%) | 8 (100.0) | 94 (97.9) | 36 (81.8) | 9 (90.0) | 18 (54.5) | <0.001 * |
| Yes | f (%) | 0 (0.0) | 2 (2.1) | 8 (18.2) | 1 (10.0) | 15 (45.5) | ||
| Orotracheal intubation | No | f (%) | 8 (100.0) | 95 (99.0) | 39 (88.6) | 9 (90.0) | 22 (66.7) | <0.001 * |
| Yes | f (%) | 0 (0.0) | 1 (1.0) | 5 (11.4) | 1 (10.0) | 11 (33.3) | ||
| Post-COVID-19 treatment | No | f (%) | 2 (25.0) | 3 (3.1) | 1 (2.3) | 0 (0.0) | 3 (9.1) | <0.001 * |
| Inhaled Medication | f (%) | 4 (50.0) | 60 (62.5) | 25 (56.8) | 6 (60.0) | 7 (21.2) | ||
| Physiotherapy | f (%) | 2 (25.0) | 19 (19.8) | 6 (13.6) | 1 (10.0) | 3 (9.1) | ||
| Both | f (%) | 0 (0.0) | 14 (14.6) | 12 (27.3) | 3 (30.0) | 20 (60.6) | ||
| Variable | Category | Normalization of Spirometry (n = 57) | p-Value | ||||
|---|---|---|---|---|---|---|---|
| <6 Months | 6–12 Months | >12 Months | No Normalization | ||||
| Priority treatment | Home | f (%) | 20 (57.1) | 3 (42.9) | 1 (25.0) | 7 (63.6) | 0.561 |
| Hospital | f (%) | 15 (42.9) | 4 (57.1) | 3 (75.0) | 4 (36.4) | ||
| Intensive Care Unit | No | f (%) | 31 (88.6) | 5 (71.4) | 1 (25.0) | 9 (81.8) | 0.025 * |
| Yes | f (%) | 4 (11.4) | 2 (28.6) | 3 (75.0) | 2 (18.2) | ||
| Orotracheal intubation | No | f (%) | 32 (91.4) | 5 (71.4) | 2 (50.0) | 10 (90.9) | 0.065 |
| Yes | f (%) | 3 (8.6) | 2 (28.6) | 2 (50.0) | 1 (9.1) | ||
| Post-COVID-19 treatment | No | f (%) | 2 (5.7) | 0 (0.0) | 0 (0.0) | 1 (9.1) | 0.718 |
| Inhaled Medication | f (%) | 16 (45.7) | 4 (57.1) | 3 (75.0) | 6 (54.6) | ||
| Physiotherapy | f (%) | 5 (14.3) | 0 (0.0) | 1 (25.0) | 0 (0.0) | ||
| Both | f (%) | 12 (34.3) | 3 (42.9) | 0 (0.0) | 4 (36.4) | ||
| Variable | B | Wald | Odds | IC95% (Odds) | Model | |||
|---|---|---|---|---|---|---|---|---|
| Dependent | Independent | p-Value | LL | UL | p-Value | R2 Cox | ||
| CT normalization | Age (years) | −0.043 | 0.004 * | 0.958 | 0.93 | 0.986 | <0.001 ** | 0.170 |
| ICU | −2.413 | <0.001 * | 0.09 | 0.034 | 0.234 | |||
| Constant | 4.37 | <0.001 * | 79.015 | |||||
| Spirometry normalization | COPD | −2.48 | 0.004 * | 0.084 | 0.016 | 0.443 | 0.003 ** | 0.145 |
| Constant | 1.969 | <0.001 * | 7.167 | |||||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cavallari Strozze Catharin, V.M.; Zutin, T.L.M.; Guiguer, E.L.; Cressoni Araújo, A.; Fornari Laurindo, L.; Chagas, E.F.B.; Gasparotti Zorzetto, C.F.; Bueno, P.C.d.S.; dos Santos Bueno, M.; Cervelim Nunes, Y.; et al. Radiological and Functional Pulmonary Evolution in Post-COVID-19 Patients: An Observational Study. Diseases 2023, 11, 113. https://doi.org/10.3390/diseases11030113
Cavallari Strozze Catharin VM, Zutin TLM, Guiguer EL, Cressoni Araújo A, Fornari Laurindo L, Chagas EFB, Gasparotti Zorzetto CF, Bueno PCdS, dos Santos Bueno M, Cervelim Nunes Y, et al. Radiological and Functional Pulmonary Evolution in Post-COVID-19 Patients: An Observational Study. Diseases. 2023; 11(3):113. https://doi.org/10.3390/diseases11030113
Chicago/Turabian StyleCavallari Strozze Catharin, Virgínia Maria, Tereza Laís Menegucci Zutin, Elen Landgraf Guiguer, Adriano Cressoni Araújo, Lucas Fornari Laurindo, Eduardo F. Baisi Chagas, Cássia Fernanda Gasparotti Zorzetto, Patrícia C. dos Santos Bueno, Manoela dos Santos Bueno, Yandra Cervelim Nunes, and et al. 2023. "Radiological and Functional Pulmonary Evolution in Post-COVID-19 Patients: An Observational Study" Diseases 11, no. 3: 113. https://doi.org/10.3390/diseases11030113