Development of Hydroxyapatite Coatings for Orthopaedic Implants from Colloidal Solutions: Part 2—Detailed Characterisation of the Coatings and Their Growth Mechanism
Abstract
:1. Introduction
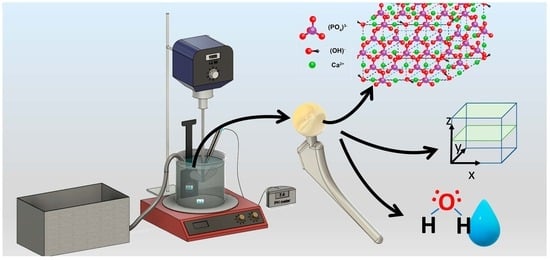
2. Materials and Methods
3. Results
3.1. Analysis of HA Generated from within This Process in Powder Form
 31PO43−. Crystalline HA material is correlated by the proton of the hydroxyl functional group with the P proton of a phosphate O1H
31PO43−. Crystalline HA material is correlated by the proton of the hydroxyl functional group with the P proton of a phosphate O1H 31PO43−. Two distinct areas could be seen on the HETCOR spectrum (τcp = 0.5 ms) through contour vectors at the location of the cross peaks (Figure 1c). The cross-correlated peak at 1H 0 ppm was due to apatitic OH− and can be assigned to a more well-formed crystalline HA. The broader cross peak between 1H 5 and 10 ppm was due to correlations between hydrogen phosphates, ACP and free and bound water, i.e., less well-formed HA. The NMR data indicated the existence of two distinct types of HA within the powder, one crystalline and one amorphous. The ACP peak also manifested the presence of water nuclei in and around all HA phases.
31PO43−. Two distinct areas could be seen on the HETCOR spectrum (τcp = 0.5 ms) through contour vectors at the location of the cross peaks (Figure 1c). The cross-correlated peak at 1H 0 ppm was due to apatitic OH− and can be assigned to a more well-formed crystalline HA. The broader cross peak between 1H 5 and 10 ppm was due to correlations between hydrogen phosphates, ACP and free and bound water, i.e., less well-formed HA. The NMR data indicated the existence of two distinct types of HA within the powder, one crystalline and one amorphous. The ACP peak also manifested the presence of water nuclei in and around all HA phases.3.2. The Growth Mechanism of HA Film on a Titanium Substrate
- OCP [002] is indicative of a calcium deficient plane [002] (26.2°);
- HA [210] (28.5°);
- HA Triple Peak containing the planes [211], [112] and [310] in varying degrees and could be masking the present of TCP which would be observed at a similar position.
4. Conclusions
Supplementary Materials
Author Contributions
Funding
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Murphy, B.; Morris, M.A.; Baez, J. Development of Hydroxyapatite Coatings for Orthopaedic Implants from Colloidal Solutions: Part 1—Effect of Solution Concentration and Deposition Kinetics. Nanomaterials 2023, 13, 2577. [Google Scholar] [CrossRef]
- Keyhani, S.; Movahedinia, M.; Vaziri, A.S.; Soleymanha, M.; Vosoughi, F.; Tahami, M.; LaPrade, R.F. Is Posterior Knee Arthroscopy Using Posterior Portals Necessary for Orthopedic Surgeons? The Latest Evidence on Applications and Techniques. EFORT Open Rev. 2023, 8, 189–198. [Google Scholar] [CrossRef] [PubMed]
- Josyula, A.; Parikh, K.S.; Pitha, I.; Ensign, L.M. Engineering Biomaterials to Prevent Post-Operative Infection and Fibrosis. Drug Deliv. Transl. Res. 2021, 11, 1675–1688. [Google Scholar] [CrossRef] [PubMed]
- Guillem-Marti, J.; Cinca, N.; Punset, M.; Cano, I.G.; Gil, F.J.; Guilemany, J.M.; Dosta, S. Porous Titanium-Hydroxyapatite Composite Coating Obtained on Titanium by Cold Gas Spray with High Bond Strength for Biomedical Applications. Colloids Surf. B Biointerfaces 2019, 180, 245–253. [Google Scholar] [CrossRef] [PubMed]
- Ibrahim, A.-R.; Benoit, R.; Suo, X.; Li, X.; Huang, Y.; Ma, G.; Li, J. Ultra-Fast Route to Synthesizing Biogenic Carbonate Hydroxyapatite: Consequence of a High-Pressure Solid-Solid Preparation Technique. Chem. Eng. Process. Process Intensif. 2019, 142, 107549. [Google Scholar] [CrossRef]
- Hussain, M.A.; Ul Haq, E.; Munawar, I.; Maqbool, A.; Saleem, M.; Rafiq, M.A.; Inam, A.; Hakeem, A.S. Influence of Spark Plasma Sintering Temperature and Hydroxyapatite Nanoparticles on Properties of HA Based Functionally Graded Materials for Bone Prosthesis. Ceram. Int. 2022, 48, 14481–14490. [Google Scholar] [CrossRef]
- Varadavenkatesan, T.; Vinayagam, R.; Pai, S.; Kathirvel, B.; Pugazhendhi, A.; Selvaraj, R. Synthesis, Biological and Environmental Applications of Hydroxyapatite and Its Composites with Organic and Inorganic Coatings. Prog. Org. Coat. 2021, 151, 106056. [Google Scholar] [CrossRef]
- Kumar, R.; Mohanty, S. Hydroxyapatite: A Versatile Bioceramic for Tissue Engineering Application. J. Inorg. Organomet. Polym. 2022, 32, 4461–4477. [Google Scholar] [CrossRef]
- Murphy, B.; Baez, J.; Morris, M.A. Characterising Hydroxyapatite Deposited from Solution onto Novel Substrates: Growth Mechanism and Physical Properties. Nanomaterials 2023, 13, 2483. [Google Scholar] [CrossRef]
- Murphy, B.; Baez, J.; Morris, M.A. Characterizing Hydroxyapatite Deposited from Solution onto Novel Substrates in Terms of Growth Mechanism and Physical Chemical Properties. Mater. Proc. 2023, 14, 34. [Google Scholar] [CrossRef]
- Rajkumar, P.; Sarma, B.K. Substrate Dependent Structural Variations of Biomimetic Carbonated Hydroxyapatite Deposited on Glass, Ti and Sputtered ZnO Thin Films. Mater. Charact. 2022, 191, 112120. [Google Scholar] [CrossRef]
- Hua, L.C.; Wang, W.Y.; Swain, M.V.; Zhu, C.L.; Huang, H.B.; Du, J.K.; Zhou, Z.R. The Dehydration Effect on Mechanical Properties of Tooth Enamel. J. Mech. Behav. Biomed. Mater. 2019, 95, 210–214. [Google Scholar] [CrossRef]
- Heimann, R.B. Structural Changes of Hydroxylapatite during Plasma Spraying: Raman and NMR Spectroscopy Results. Coatings 2021, 11, 987. [Google Scholar] [CrossRef]
- Prakasam, M.; Locs, J.; Salma-Ancane, K.; Loca, D.; Largeteau, A.; Berzina-Cimdina, L. Fabrication, Properties and Applications of Dense Hydroxyapatite: A Review. J. Funct. Biomater. 2015, 6, 1099–1140. [Google Scholar] [CrossRef]
- Schröter, L.; Kaiser, F.; Stein, S.; Gbureck, U.; Ignatius, A. Biological and Mechanical Performance and Degradation Characteristics of Calcium Phosphate Cements in Large Animals and Humans. Acta Biomater. 2020, 117, 1–20. [Google Scholar] [CrossRef] [PubMed]
- Zhou, H.; Yang, L.; Gbureck, U.; Bhaduri, S.B.; Sikder, P. Monetite, an Important Calcium Phosphate Compound–Its Synthesis, Properties and Applications in Orthopedics. Acta Biomater. 2021, 127, 41–55. [Google Scholar] [CrossRef] [PubMed]
- Bohner, M.; Santoni, B.L.G.; Döbelin, N. β-Tricalcium Phosphate for Bone Substitution: Synthesis and Properties. Acta Biomater. 2020, 113, 23–41. [Google Scholar] [CrossRef] [PubMed]
- Liu, D.; Cui, C.; Chen, W.; Shi, J.; Li, B.; Chen, S. Biodegradable Cements for Bone Regeneration. J. Funct. Biomater. 2023, 14, 134. [Google Scholar] [CrossRef]
- Suzuki, O.; Hamai, R.; Sakai, S. The Material Design of Octacalcium Phosphate Bone Substitute: Increased Dissolution and Osteogenecity. Acta Biomater. 2023, 158, 4742–4753. [Google Scholar] [CrossRef]
- Bhat, S.; Uthappa, U.T.; Altalhi, T.; Jung, H.-Y.; Kurkuri, M.D. Functionalized Porous Hydroxyapatite Scaffolds for Tissue Engineering Applications: A Focused Review. ACS Biomater. Sci. Eng. 2022, 8, 4039–4076. [Google Scholar] [CrossRef]
- Awasthi, S.; Pandey, S.K.; Arunan, E.; Srivastava, C. A Review on Hydroxyapatite Coatings for the Biomedical Applications: Experimental and Theoretical Perspectives. J. Mater. Chem. B 2021, 9, 228–249. [Google Scholar] [CrossRef] [PubMed]
- Xiao, D.; Zhang, J.; Zhang, C.; Barbieri, D.; Yuan, H.; Moroni, L.; Feng, G. The Role of Calcium Phosphate Surface Structure in Osteogenesis and the Mechanisms Involved. Acta Biomater. 2020, 106, 22–33. [Google Scholar] [CrossRef] [PubMed]
- Du, M.; Chen, J.; Liu, K.; Xing, H.; Song, C. Recent Advances in Biomedical Engineering of Nano-Hydroxyapatite Including Dentistry, Cancer Treatment and Bone Repair. Compos. Part B Eng. 2021, 215, 108790. [Google Scholar] [CrossRef]
- Kang, S.; Haider, A.; Gupta, K.C.; Kim, H.; Kang, I. Chemical Bonding of Biomolecules to the Surface of Nano-Hydroxyapatite to Enhance Its Bioactivity. Coatings 2022, 12, 999. [Google Scholar] [CrossRef]
- Safavi, M.S.; Walsh, F.C.; Surmeneva, M.A.; Surmenev, R.A.; Khalil-Allafi, J. Electrodeposited Hydroxyapatite-Based Biocoatings: Recent Progress and Future Challenges. Coatings 2021, 11, 110. [Google Scholar] [CrossRef]
- McCabe, A.; Pickford, M.; Shawcross, J. The History, Technical Specifications and Efficacy of Plasma Spray Coatings Applied to Joint Replacement Prostheses. Reconstr. Rev. 2016, 6, 19–26. [Google Scholar] [CrossRef]
- Safavi, M.S.; Etminanfar, M. A Review on the Prevalent Fabrication Methods, Microstructural, Mechanical Properties, and Corrosion Resistance of Nanostructured Hydroxyapatite Containing Bilayer and Multilayer Coatings Used in Biomedical Applications. J. Ultrafine Grained Nanostruct. Mater. 2019, 52, 1–17. [Google Scholar] [CrossRef]
- Guner, A.T.; Meran, C. A Review on Plasma Sprayed Titanium and Hydroxyapatite Coatings on Polyetheretherketone Implants. Int. J. Surf. Sci. Eng. 2019, 13, 237–262. [Google Scholar] [CrossRef]
- Singh, H.; Kumar, R.; Prakash, C.; Singh, S. HA-Based Coating by Plasma Spray Techniques on Titanium Alloy for Orthopedic Applications. Mater. Today Proc. 2022, 50, 612–628. [Google Scholar] [CrossRef]
- Ranjan Dev, P.; Parambil Anand, C.; Samuvel Michael, D.; Wilson, P. Hydroxyapatite Coatings: A Critical Review on Electrodeposition Parametric Variations Influencing Crystal Facet Orientation towards Enhanced Electrochemical Sensing. Mater. Adv. 2022, 3, 7773–7809. [Google Scholar] [CrossRef]
- Lissandrello, F.; Magagnin, L. Pulsed Electrochemical Deposition of Calcium Phosphate Coatings for Biomedical Applications. Trans. IMF 2023, 101, 173–178. [Google Scholar] [CrossRef]
- Jaafar, A.; Hecker, C.; Árki, P.; Joseph, Y. Sol-Gel Derived Hydroxyapatite Coatings for Titanium Implants: A Review. Bioengineering 2020, 7, 127. [Google Scholar] [CrossRef] [PubMed]
- Ansari, Z.; Kalantar, M.; Kharaziha, M.; Ambrosio, L.; Raucci, M.G. Polycaprolactone/Fluoride Substituted-Hydroxyapatite (PCL/FHA) Nanocomposite Coatings Prepared by in-Situ Sol-Gel Process for Dental Implant Applications. Prog. Org. Coat. 2020, 147, 105873. [Google Scholar] [CrossRef]
- Chen, H.; Wang, R.; Qian, L.; Liu, H.; Wang, J.; Zhu, M. Surface Modification of Urchin-like Serried Hydroxyapatite with Sol-Gel Method and Its Application in Dental Composites. Compos. Part B Eng. 2020, 182, 107621. [Google Scholar] [CrossRef]
- Sebastin, A.X.S.; Uthirapathy, V. In Vitro Electrochemical Behavior of Sol-Gel Derived Hydroxyapatite/Graphene Oxide Composite Coatings on 316L SS for Biomedical Applications. ChemistrySelect 2020, 5, 12140–12147. [Google Scholar] [CrossRef]
- Tan, B.; Zhao, N.; Guo, W.; Huang, F.; Hu, H.; Chen, Y.; Li, J.; Ling, Z.; Zou, Z.; Hu, R.; et al. Biomimetic Hydroxyapatite Coating on the 3D-Printed Bioactive Porous Composite Ceramic Scaffolds Promoted Osteogenic Differentiation via PI3K/AKT/mTOR Signaling Pathways and Facilitated Bone Regeneration In Vivo. J. Mater. Sci. Technol. 2023, 136, 54–64. [Google Scholar] [CrossRef]
- Jiang, J.; Liu, W.; Xiong, Z.; Hu, Y.; Xiao, J. Effects of Biomimetic Hydroxyapatite Coatings on Osteoimmunomodulation. Biomater. Adv. 2022, 134, 112640. [Google Scholar] [CrossRef]
- Koju, N.; Sikder, P.; Ren, Y.; Zhou, H.; Bhaduri, S.B. Biomimetic Coating Technology for Orthopedic Implants. Curr. Opin. Chem. Eng. 2017, 15, 49–55. [Google Scholar] [CrossRef]
- Baino, F.; Yamaguchi, S. The Use of Simulated Body Fluid (SBF) for Assessing Materials Bioactivity in the Context of Tissue Engineering: Review and Challenges. Biomimetics 2020, 5, 57. [Google Scholar] [CrossRef]
- Suchý, T.; Bartoš, M.; Sedláček, R.; Šupová, M.; Žaloudková, M.; Martynková, G.S.; Foltán, R. Various Simulated Body Fluids Lead to Significant Differences in Collagen Tissue Engineering Scaffolds. Materials 2021, 14, 4388. [Google Scholar] [CrossRef]
- Ghorbani, F.; Zamanian, A.; Behnamghader, A.; Daliri-Joupari, M. Bone-like Hydroxyapatite Mineralization on the Bio-Inspired PDA Nanoparticles Using Microwave Irradiation. Surf. Interfaces 2019, 15, 38–42. [Google Scholar] [CrossRef]
- Wei, G.; Gong, C.; Hu, K.; Wang, Y.; Zhang, Y. Biomimetic Hydroxyapatite on Graphene Supports for Biomedical Applications: A Review. Nanomaterials 2019, 9, 1435. [Google Scholar] [CrossRef]
- Beig, B.; Liaqat, U.; Niazi, M.F.K.; Douna, I.; Zahoor, M.; Niazi, M.B.K. Current Challenges and Innovative Developments in Hydroxyapatite-Based Coatings on Metallic Materials for Bone Implantation: A Review. Coatings 2020, 10, 1249. [Google Scholar] [CrossRef]
- Domínguez-Trujillo, C.; Peón, E.; Chicardi, E.; Pérez, H.; Rodríguez-Ortiz, J.A.; Pavón, J.J.; García-Couce, J.; Galván, J.C.; García-Moreno, F.; Torres, Y. Sol-Gel Deposition of Hydroxyapatite Coatings on Porous Titanium for Biomedical Applications. Surf. Coat. Technol. 2018, 333, 158–162. [Google Scholar] [CrossRef]
- Andrusova, N.N.; Zhavoronok, E.S.; Legon’kova, O.A.; Goncharova, A.S.; Kedik, S.A. Polymer–Mineral Compounds for Cementless Hip Replacement. Polym. Sci. Ser. D 2020, 13, 68–72. [Google Scholar] [CrossRef]
- Sánchez-Bodón, J.; Andrade del Olmo, J.; Alonso, J.M.; Moreno-Benítez, I.; Vilas-Vilela, J.L.; Pérez-Álvarez, L. Bioactive Coatings on Titanium: A Review on Hydroxylation, Self-Assembled Monolayers (SAMs) and Surface Modification Strategies. Polymers 2022, 14, 165. [Google Scholar] [CrossRef]
- Durga, R.; Jimenez, N.; Ramanathan, S.; Suraneni, P.; Pestle, W.J. Use of Thermogravimetric Analysis to Estimate Collagen and Hydroxyapatite Contents in Archaeological Bone. J. Archaeol. Sci. 2022, 145, 105644. [Google Scholar] [CrossRef]
- Ebadipour, N.; Paul, S.; Katryniok, B.; Dumeignil, F. Calcium Hydroxyapatite: A Highly Stable and Selective Solid Catalyst for Glycerol Polymerization. Catalysts 2021, 11, 1247. [Google Scholar] [CrossRef]
- Roque-Ruiz, J.H.; Garibay-Alvarado, J.A.; Medellín-Castillo, N.A.; Reyes-López, S.Y. Preparation of Electrospun Hydroxyapatite-Glass Fibers for Removal of Cadmium (Cd+2) and Lead (Pb+2) from Aqueous Media. Water Air Soil Pollut. 2020, 231, 497. [Google Scholar] [CrossRef]
- Greiner, M.; Rodríguez-Navarro, A.; Schmahl, W.; Kocsis, B.; Grupe, G.; Mayer, K. The Bone Mineral Is Carbonato-Hydro-Apatite and It Transforms into Hydroxyapatite by Heating (Cremation) beyond 700 °C. Acta Crystallogr. Sect. A Found. Adv. 2019, 75, e199. [Google Scholar] [CrossRef]
- Malla, K.P.; Regmi, S.; Nepal, A.; Bhattarai, S.; Yadav, R.J.; Sakurai, S.; Adhikari, R. Extraction and Characterization of Novel Natural Hydroxyapatite Bioceramic by Thermal Decomposition of Waste Ostrich Bone. Int. J. Biomater. 2020, 2020, e1690178. [Google Scholar] [CrossRef]
- Jiang, Y.; Ren, C.; Guo, H.; Guo, M.; Li, W. Speciation Transformation of Phosphorus in Poultry Litter during Pyrolysis: Insights from X-ray Diffraction, Fourier Transform Infrared, and Solid-State NMR Spectroscopy. Environ. Sci. Technol. 2019, 53, 13841–13849. [Google Scholar] [CrossRef]
- Wang, J.; Ren, C.; Li, Z.; Li, W. Two-Dimensional Solid-State NMR Spectroscopy Investigations of Surface Precipitation of Phosphate onto Calcite. Sci. Total Environ. 2023, 890, 164444. [Google Scholar] [CrossRef] [PubMed]
- Klimavicius, V.; Maršalka, A.; Kizalaite, A.; Zarkov, A.; Kareiva, A.; Aidas, K.; Hirschinger, J.; Balevicius, V. Step-by-Step from Amorphous Phosphate to Nano-Structured Calcium Hydroxyapatite: Monitoring by Solid-State 1 H and 31 P NMR and Spin Dynamics. Phys. Chem. Chem. Phys. 2022, 24, 18952–18965. [Google Scholar] [CrossRef]
- Hamza, H.M.; Deen, K.M.; Haider, W. Microstructural Examination and Corrosion Behavior of Selective Laser Melted and Conventionally Manufactured Ti6Al4V for Dental Applications. Mater. Sci. Eng. C 2020, 113, 110980. [Google Scholar] [CrossRef] [PubMed]
- Kaschel, F.R.; Vijayaraghavan, R.K.; Shmeliov, A.; McCarthy, E.K.; Canavan, M.; McNally, P.J.; Dowling, D.P.; Nicolosi, V.; Celikin, M. Mechanism of Stress Relaxation and Phase Transformation in Additively Manufactured Ti-6Al-4V via in Situ High Temperature XRD and TEM Analyses. Acta Mater. 2020, 188, 720–732. [Google Scholar] [CrossRef]
- Gross, K.A.; Petzold, C.; Pluduma-LaFarge, L.; Kumermanis, M.; Haugen, H.J. Structural and Chemical Hierarchy in Hydroxyapatite Coatings. Materials 2020, 13, 4447. [Google Scholar] [CrossRef]
- Li, T.-T.; Ling, L.; Lin, M.-C.; Jiang, Q.; Lin, Q.; Lin, J.-H.; Lou, C.-W. Properties and Mechanism of Hydroxyapatite Coating Prepared by Electrodeposition on a Braid for Biodegradable Bone Scaffolds. Nanomaterials 2019, 9, 679. [Google Scholar] [CrossRef]
- Londoño-Restrepo, S.M.; Millán-Malo, B.M.; del Real-López, A.; Rodriguez-García, M.E. In Situ Study of Hydroxyapatite from Cattle during a Controlled Calcination Process Using HT-XRD. Mater. Sci. Eng. C 2019, 105, 110020. [Google Scholar] [CrossRef] [PubMed]
- Pham, D.Q.; Gangadoo, S.; Berndt, C.C.; Chapman, J.; Zhai, J.; Vasilev, K.; Truong, V.K.; Ang, A.S.M. Antibacterial Longevity of a Novel Gallium Liquid Metal/Hydroxyapatite Composite Coating Fabricated by Plasma Spray. ACS Appl. Mater. Interfaces 2022, 14, 18974–18988. [Google Scholar] [CrossRef]
- Londoño-Restrepo, S.M.; Herrera-Lara, M.; Bernal-Alvarez, L.R.; Rivera-Muñoz, E.M.; Rodriguez-García, M.E. In-Situ XRD Study of the Crystal Size Transition of Hydroxyapatite from Swine Bone. Ceram. Int. 2020, 46, 24454–24461. [Google Scholar] [CrossRef]
- Khan, A.S.; Awais, M. Low-Cost Deposition of Antibacterial Ion-Substituted Hydroxyapatite Coatings onto 316L Stainless Steel for Biomedical and Dental Applications. Coatings 2020, 10, 880. [Google Scholar] [CrossRef]
- Grigoraviciute-Puroniene, I.; Tanaka, Y.; Vegelyte, V.; Nishimoto, Y.; Ishikawa, K.; Kareiva, A. A Novel Synthetic Approach to Low-Crystallinity Calcium Deficient Hydroxyapatite. Ceram. Int. 2019, 45, 15620–15623. [Google Scholar] [CrossRef]
- Vilardell, A.M.; Cinca, N.; Garcia-Giralt, N.; Dosta, S.; Cano, I.G.; Nogués, X.; Guilemany, J.M. In-Vitro Comparison of Hydroxyapatite Coatings Obtained by Cold Spray and Conventional Thermal Spray Technologies. Mater. Sci. Eng. C 2020, 107, 110306. [Google Scholar] [CrossRef] [PubMed]
- Lu, M.; Chen, H.; Yuan, B.; Zhou, Y.; Min, L.; Xiao, Z.; Yang, X.; Zhu, X.; Tu, C.; Zhang, X. The Morphological Effect of Nanostructured Hydroxyapatite Coatings on the Osteoinduction and Osteogenic Capacity of Porous Titanium. Nanoscale 2020, 12, 24085–24099. [Google Scholar] [CrossRef] [PubMed]
- Sun, Y.; Zhang, X.; Luo, M.; Hu, W.; Zheng, L.; Huang, R.; Greven, J.; Hildebrand, F.; Yuan, F. Plasma Spray vs. Electrochemical Deposition: Toward a Better Osteogenic Effect of Hydroxyapatite Coatings on 3D-Printed Titanium Scaffolds. Front. Bioeng. Biotechnol. 2021, 9, 705774. [Google Scholar] [CrossRef] [PubMed]
- Yokoi, T.; Shimabukuro, M.; Kawashita, M. Octacalcium Phosphate with Incorporated Carboxylate Ions: A Review. Sci. Technol. Adv. Mater. 2022, 23, 434–445. [Google Scholar] [CrossRef]
- Hamai, R.; Sakai, S.; Shiwaku, Y.; Anada, T.; Tsuchiya, K.; Ishimoto, T.; Nakano, T.; Suzuki, O. Octacalcium Phosphate Crystals Including a Higher Density Dislocation Improve Its Materials Osteogenecity. Appl. Mater. Today 2022, 26, 101279. [Google Scholar] [CrossRef]
- Nosrati, H.; Sarraf-Mamoory, R.; Ahmadi, A.H.; Canillas, M. Synthesis of Graphene Nanoribbons-Hydroxyapatite Nanocomposite Applicable in Biomedicine and Theranostics. J. Nanotheranostics 2020, 1, 2. [Google Scholar] [CrossRef]
- In, Y.; Amornkitbamrung, U.; Hong, M.-H.; Shin, H. On the Crystallization of Hydroxyapatite under Hydrothermal Conditions: Role of Sebacic Acid as an Additive. ACS Omega 2020, 5, 27204–27210. [Google Scholar] [CrossRef]
- Reyes-Gasga, J.; Martínez-Piñeiro, E.L.; Brès, É.F. Crystallographic Structure of Human Tooth Enamel by Electron Microscopy and X-ray Diffraction: Hexagonal or Monoclinic? J. Microsc. 2012, 248, 102–109. [Google Scholar] [CrossRef] [PubMed]
- Bystrom, J.L.; Pujari-Palmer, M. Phosphoserine Functionalized Cements Preserve Metastable Phases, and Reprecipitate Octacalcium Phosphate, Hydroxyapatite, Dicalcium Phosphate, and Amorphous Calcium Phosphate, during Degradation, In Vitro. J. Funct. Biomater. 2019, 10, 54. [Google Scholar] [CrossRef] [PubMed]
- Lukina, Y.; Bionyshev-Abramov, L.; Kotov, S.; Serejnikova, N.; Smolentsev, D.; Sivkov, S. Carbonate-Hydroxyapatite Cement: The Effect of Composition on Solubility In Vitro and Resorption In Vivo. Ceramics 2023, 6, 1397–1414. [Google Scholar] [CrossRef]
- Mahmud, S.; Rahman, M.; Kamruzzaman, M.; Khatun, H.; Ali, M.O.; Haque, M.M. Recent Developments in Hydroxyapatite Coating on Magnesium Alloys for Clinical Applications. Results Eng. 2023, 17, 101002. [Google Scholar] [CrossRef]
- Zhang, A.-M.; Lenin, P.; Zeng, R.-C.; Kannan, M.B. Advances in Hydroxyapatite Coatings on Biodegradable Magnesium and Its Alloys. J. Magnes. Alloys 2022, 10, 1154–1170. [Google Scholar] [CrossRef]



| Peak Assignment | ||||
|---|---|---|---|---|
| Sample | OCP [002] (26.2°) | HA [210] (28.5°) | HA Triple Peak (32–33°) | Titanium (35.8°) |
| Dried process solute | Medium | Weak | Strong | Absent |
| 7× runs HA film on Ti | Strong | Weak | Medium | Weak |
| 4× runs HA film on Ti | Strong | Weak | Medium | Medium |
| 2× runs HA film on Ti | Weak | Absent | Strong | Strong |
| Blank Ti substrate | Absent | Absent | Absent | Strong |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Murphy, B.; Morris, M.A.; Baez, J. Development of Hydroxyapatite Coatings for Orthopaedic Implants from Colloidal Solutions: Part 2—Detailed Characterisation of the Coatings and Their Growth Mechanism. Nanomaterials 2023, 13, 2606. https://doi.org/10.3390/nano13182606
Murphy B, Morris MA, Baez J. Development of Hydroxyapatite Coatings for Orthopaedic Implants from Colloidal Solutions: Part 2—Detailed Characterisation of the Coatings and Their Growth Mechanism. Nanomaterials. 2023; 13(18):2606. https://doi.org/10.3390/nano13182606
Chicago/Turabian StyleMurphy, Bríd, Mick A. Morris, and Jhonattan Baez. 2023. "Development of Hydroxyapatite Coatings for Orthopaedic Implants from Colloidal Solutions: Part 2—Detailed Characterisation of the Coatings and Their Growth Mechanism" Nanomaterials 13, no. 18: 2606. https://doi.org/10.3390/nano13182606