CMR Predictors of Favorable Outcome in Myocarditis: A Single-Center Experience
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Participants
2.2. CMR Protocol and Analysis
2.3. Statistical Analysis
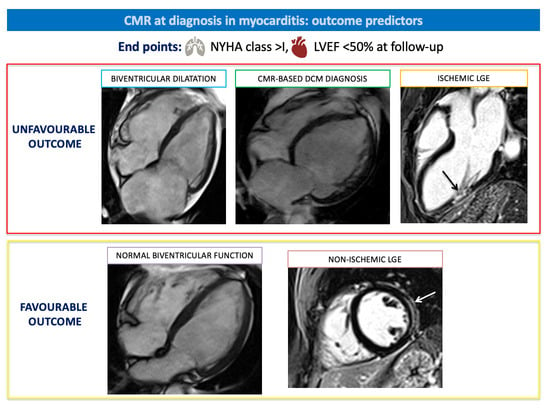
3. Results
3.1. Baseline Patient Characteristics
3.2. CMR Findings—Overall Cohort
3.3. CMR Findings—CS vs. EMB-Proven Cohort
3.4. Prognosis in the Overall Cohort
4. Discussion
4.1. Diagnostic Role of CMR in Suspected Myocarditis
4.2. CMR Features in EMB-Proven versus CS Myocarditis
4.3. Prognostic Role of CMR in Myocarditis
4.4. Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Caforio, A.L.; Pankuweit, S.; Arbustini, E.; Basso, C.; Gimeno-Blanes, J.; Felix, S.B.; Fu, M.; Heliö, T.; Heymans, S.; Jahns, R.; et al. Current state of knowledge on aetiology, diagnosis, management, and therapy of myocarditis: A position statement of the European Society of Cardiology Working Group on Myocardial and Pericardial Diseases. Eur. Heart J. 2013, 34, 2636–2648. [Google Scholar] [CrossRef]
- Tschöpe, C.; Ammirati, E.; Bozkurt, B.; Caforio, A.L.P.; Cooper, L.T.; Felix, S.B.; Hare, J.M.; Heidecker, B.; Heymans, S.; Hübner, N.; et al. Myocarditis and inflammatory cardiomyopathy: Current evidence and future directions. Nat. Rev. Cardiol. 2021, 18, 169–193. [Google Scholar] [CrossRef]
- Sinagra, G.; Anzini, M.; Pereira, N.L.; Bussani, R.; Finocchiaro, G.; Bartunek, J.; Merlo, M. Myocarditis in clinical practice. Mayo. Clin. Proc. 2016, 91, 1256–1266. [Google Scholar] [CrossRef]
- Cooper, L.T.; Baughman, K.L.; Feldman, A.M.; Frustaci, A.; Jessup, M.; Kuhl, U.; Levine, G.N.; Narula, J.; Starling, R.C.; Towbin, J.; et al. The role of endomyocardial biopsy in the management of cardiovascular disease: A scientific statement from American Heart Association, the American College of Cardiology, and the European Society of Cardiology. J. Am. Coll. Cardiol. 2007, 50, 1914–1931. [Google Scholar] [CrossRef]
- Seferović, P.M.; Tsutsui, H.; McNamara, D.M.; Ristić, A.D.; Basso, C.; Bozkurt, B.; Cooper, L.T., Jr.; Filippatos, G.; Ide, T.; Inomata, T.; et al. Heart Failure Association of the ESC, Heart Failure Society of America and Japanese Heart Failure Society Position statement on endomyocardial biopsy. Eur. J. Heart Fail. 2021, 23, 854–871. [Google Scholar] [CrossRef]
- McDonagh, T.A.; Metra, M.; Adamo, M.; Gardner, R.S.; Baumbach, A.; Böhm, M.; Burri, H.; Butler, J.; Čelutkienė, J.; Chioncel, O.; et al. 2021 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure. Eur. Heart J. 2021, 42, 3599–3726. [Google Scholar] [CrossRef]
- Friedrich, M.G.; Sechtem, U.; Schulz-Menger, J.; Holmvang, G.; Alakija, P.; Cooper, L.T.; White, J.A.; Abdel-Aty, H.; Gutberlet, M.; Prasad, S.; et al. Cardiovascular Magnetic Resonance in Myocarditis: A JACC White Paper. J. Am. Coll. Cardiol. 2009, 53, 1475–1487. [Google Scholar] [CrossRef]
- Ferreira, V.M.; Schulz-Menger, J.; Holmvang, G.; Kramer, C.M.; Carbone, I.; Sechtem, U.; Kindermann, I.; Gutberlet, M.; Cooper, L.T.; Liu, P.; et al. Cardiovascular Magnetic Resonance in nonischemic myocardial inflammation: Expert Recommendations. J. Am. Coll. Cardiol. 2018, 72, 3158–3176. [Google Scholar] [CrossRef] [PubMed]
- Aquaro, G.D.; Perfetti, M.; Camastra, G.; Monti, L.; Dellegrottaglie, S.; Moro, C.; Pepe, A.; Todiere, G.; Lanzillo, C.; Scatteia, A.; et al. Cardiac MR with late gadolinium enhancement in acute myocarditis with preserved systolic function. ITAMY study. J. Am. Coll. Cardiol. 2017, 70, 1977–1987. [Google Scholar] [CrossRef] [PubMed]
- Schumm, J.; Greulich, S.; Wagner, A.; Grün, S.; Ong, P.; Bentz, K.; Klingel, K.; Kandolf, R.; Bruder, O.; Schneider, S.; et al. Cardiovascular magnetic resonance risk stratification in patients with clinically suspected myocarditis. J. Cardiovasc. Magn. Reson. 2014, 16, 14. [Google Scholar] [CrossRef] [PubMed]
- Anzini, M.; Merlo, M.; Sabbadini, G.; Barbati, G.; Finocchiaro, G.; Pinamonti, B.; Salvi, A.; Perkan, A.; Di Lenarda, A.; Bussani, R.; et al. Long-term evolution and prognostic stratification of biopsy-proven active myocarditis. Circulation 2013, 128, 2384–2394. [Google Scholar] [CrossRef]
- Gräni, C.; Eichhorn, C.; Bière, L.; Murthy, V.L.; Agarwal, V.; Kaneko, K.; Cuddy, S.; Aghayev, A.; Steigner, M.; Blankstein, R.; et al. Prognostic value of cardiac magnetic resonance tissue characterization in risk stratifying patients with suspected myocarditis. J. Am. Coll. Cardiol. 2017, 70, 1964–1976. [Google Scholar] [CrossRef]
- Chopra, H.; Arangalage, D.; Bouleti, C.; Zarka, S.; Fayard, F.; Chillon, S.; Laissy, J.-P.; Henry-Feugeas, M.-C.; Steg, P.-G.; Vahanian, A.; et al. Prognostic value of the infarct- and non-infarct like patterns and cardiovascular magnetic resonance parameters on long-term outcome of patients after acute myocarditis. Int. J. Cardiol. 2016, 212, 63–69. [Google Scholar] [CrossRef] [PubMed]
- Grün, S.; Schumm, J.; Greulich, S.; Wagner, A.; Schneider, S.; Bruder, O.; Kispert, E.-M.; Hill, S.; Ong, P.; Klingel, K.; et al. Long-term follow-up of biopsy-proven viral myocarditis. Predictors of mortality and incomplete recovery. J. Am. Coll. Cardiol. 2012, 59, 1604–1615. [Google Scholar] [CrossRef] [PubMed]
- Pommier, T.; Leclercq, T.; Guenancia, C.; Tisserand, S.; Lairet, C.; Carré, M.; Lalande, A.; Bichat, F.; Maza, M.; Zeller, M.; et al. More than 50% of persistent myocardial scarring at one year in “infarct-like” acute myocarditis evaluated by CMR. J. Clin. Med. 2021, 10, 4677. [Google Scholar] [CrossRef] [PubMed]
- Sanguineti, F.; Garot, P.; Mana, M.; O’h-Ici, D.; Hovasse, T.; Unterseeh, T.; Louvard, Y.; Troussier, X.; Morice, M.-C.; Garot, J. Cardiovascular magnetic resonance predictors of clinical outcome in patients with suspected acute myocarditis. J. Cardiovasc. Magn. Reson. 2015, 17, 78. [Google Scholar] [CrossRef] [PubMed]
- Caforio, A.L.; Calabrese, F.; Angelini, A.; Tona, F.; Vinci, A.; Bottaro, S.; Ramondo, A.; Carturan, E.; Iliceto, S.; Thiene, G.; et al. A prospective study of biopsy-proven myocarditis: Prognostic relevance of clinical and aetiopathogenetic features at diagnosis. Eur. Heart J. 2007, 28, 1326–1333. [Google Scholar] [CrossRef] [PubMed]
- Merlo, M.; Ammirati, E.; Gentile, P.; Artico, J.; Cannatà, A.; Finocchiaro, G.; Barbati, G.; Sormani, P.; Varrenti, M.; Perkan, A.; et al. Persistent left ventricular dysfunction after acute lymphocytitc myocarditis: Frequency and predictors. PLoS ONE 2019, 14, e0214616. [Google Scholar] [CrossRef] [PubMed]
- Gräni, C.; Eichhorn, C.; Bière, L.; Kaneko, K.; Murthy, V.L.; Agarwal, V.; Aghayev, A.; Steigner, M.; Blankstein, R.; Jerosch-Herold, M.; et al. Comparison of myocardial fibrosis quantification methods by cardiovascular magnetic resonance imaging for risk stratification of patients with suspected myocarditis. J. Cardiovasc. Magn. Reson. 2019, 21, 14. [Google Scholar] [CrossRef]
- Schulz-Menger, J.; Bluemke, D.A.; Bremerich, J.; Flamm, S.D.; Fogel, M.A.; Friedrich, M.G.; Kim, R.J.; von Knobelsdorff-Brenkenhoff, F.; Kramer, C.M.; Pennell, D.J.; et al. Standardized image interpretation and post-processing in cardiovascular magnetic resonance–2020 update. J. Cardiovasc. Magn. Reson. 2020, 22, 19. [Google Scholar] [CrossRef]
- R Development Core Team 3.0.1. A Language and Environment for Statistical Computing [Internet]; R Foundation for Statistical Computing: Vienna, Austria, 2019; Volume 2, Available online: https://www.R-project.org (accessed on 1 December 2020).
- Harrell, F.E., Jr. rms: Regression Modeling Strategies. 2019, pp. 1–246. Available online: https://cran.r-project.org/web/packages/rms/rms.pdf (accessed on 1 December 2020).
- Therneau, T.M.; Grambsch, P.M. Modeling Survival Data: Extending the Cox Model; Springer: Berlin/Heidelberg, Germany, 2000; 350p. [Google Scholar]
- Alboukadel, K.; Marcin, K.; Przemyslaw, B.; Scheipl, F. Drawing Survival Curves Using ‘ggplot2’; R Package Survminer Version 0.4.3; R Foundation for Statistical Computing: Vienna, Austria, 2018. [Google Scholar]
- Francone, M.; Chimenti, C.; Galea, N.; Scopelliti, F.; Verardo, R.; Galea, R.; Carbone, I.; Catalano, C.; Fedele, F.; Frustaci, A. CMR sensitivity varies with clinical presentation and extent of cell necrosis in ciopsy-proven acute myocarditis. J. Am. Coll. Cardiol. 2014, 7, 254–263. [Google Scholar] [CrossRef]
- Cundari, G.; Galea, N.; De Rubeis, G.; Frustaci, A.; Cilia, F.; Mancuso, G.; Marchitelli, L.; Catapano, F.; Carbone, I.; Catalano, C.; et al. Use of the new Lake Louise Criteria improves CMR detection of atypical forms of acute myocarditis. Int. J. Cardiovasc. Imaging 2021, 37, 1395–1404. [Google Scholar] [CrossRef]
- Bozkurt, B.; Colvin, M.; Cook, J.; Cooper, L.T.; Deswal, A.; Fonarow, G.C.; Francis, G.S.; Lenihan, D.; Lewis, E.F.; McNamara, D.M.; et al. Current Diagnostic and Treatment Strategies for Specific Dilated Cardiomyopathies: A Scientific Statement From the American Heart Association. Circulation 2016, 134, e579–e646. [Google Scholar] [CrossRef] [PubMed]
- Aquaro, G.D.; Negri, F.; De Luca, A.; Todiere, G.; Bianco, F.; Barison, A.; Camastra, G.; Monti, L.; Dellegrottaglie, S.; Moro, C.; et al. Role of right ventricular involvement in acute myocarditis, assessed by cardiac magnetic resonance. Int. J. Cardiol. 2018, 271, 359–365. [Google Scholar] [CrossRef] [PubMed]
- Corrado, D.; Basso, C.; Leoni, L.; Tokajuk, B.; Turrini, P.; Bauce, B.; Migliore, F.; Pavei, A.; Tarantini, G.; Napodano, M.; et al. Three-dimensional electroanatomic voltage mapping and histologic evaluation of myocardial substrate in right ventricular outflow tract tachycardia. J. Am. Coll. Cardiol. 2008, 51, 731–739. [Google Scholar] [CrossRef]
- Basso, C. Arrhythmogenic right ventricular cardiomyopathy. Lancet 2009, 373, 1289–1300. [Google Scholar] [CrossRef] [PubMed]
- Ammirati, E.; Cipriani, M.; Lilliu, M.; Sormani, P.; Varrenti, M.; Raineri, C.; Petrella, D.; Garascia, A.; Pedrotti, P.; Roghi, A.; et al. Survival and Left Ventricular Function Changes in Fulminant Versus Nonfulminant Acute Myocarditis. Circulation 2017, 136, 529–545. [Google Scholar] [CrossRef] [PubMed]
- Ammirati, E.; Cipriani, M.; Moro, C.; Raineri, C.; Pini, D.; Sormani, P.; Mantovani, R.; Varrenti, M.; Pedrotti, P.; Conca, C.; et al. Clinical Presentation and Outcome in a Contemporary Cohort of Patients With Acute Myocarditis: Multicenter Lombardy Registry. Circulation 2018, 138, 1088–1099. [Google Scholar] [CrossRef] [PubMed]
- Ammirati, E.; Veronese, G.; Brambatti, M.; Merlo, M.; Cipriani, M.; Potena, L.; Sormani, P.; Aoki, T.; Sugimura, K.; Sawamura, A.; et al. Fulminant Versus Acute Nonfulminant Myocarditis in Patients With Left Ventricular Systolic Dysfunction. J. Am. Coll. Cardiol. 2019, 74, 299–311. [Google Scholar] [CrossRef]
- Verdonschot, J.A.; Merlo, M.; Dominguez, F.; Wang, P.; Henkens, M.T.; Adriaens, M.E.; Hazebroek, M.R.; Mase, M.; Escobar, L.E.; Cobas-Paz, R.; et al. Phenotypic clustering of dilated cardiomyopathy patients highlights important pathophysiological differences. Eur. Heart J. 2021, 42, 162–174. [Google Scholar] [CrossRef]
- Baritussio, A.; Schiavo, A.; Basso, C.; Giordani, A.S.; Cheng, C.; Pontara, E.; Cattini, M.G.; Bison, E.; Gallo, N.; De Gaspari, M.; et al. Predictors of relapse, death or heart transplantation in myocarditis before the introduction of immunosuppression: Negative prognostic impact of female gender, fulminant onset, lower ejection fraction and serum autoantibodies. Eur. J. Heart Fail. 2022, 24, 1033–1044. [Google Scholar] [CrossRef]
- Merken, J.; Hazebroek, M.; Van Paassen, P.; Verdonschot, J.; Van Empel, V.; Knackstedt, C.; Hamid, M.A.; Seiler, M.; Kolb, J.; Hoermann, P.; et al. Immunosuppressive Therapy Improves Both Short- and Long-Term Prognosis in Patients With Virus-Negative Nonfulminant Inflammatory Cardiomyopathy. Circ. Heart Fail. 2018, 11, e004228. [Google Scholar] [CrossRef]
- Frustaci, A.; Russo, M.A.; Chimenti, C. Randomized study on the efficacy of immunosuppressive therapy in patients with virus-negative inflammatory cardiomyopathy: The TIMIC study. Eur. Heart J. 2009, 30, 1995–2002. [Google Scholar] [CrossRef]
- Chimenti, C.; Russo, M.A.; Fristaci, A. Immunosuppressive therapy in virus-negative inflammatory cardiomyopathy: 20-year follow-up of the TIMIC trial. Eur. Heart J. 2022, 43, 3463–3473. [Google Scholar] [CrossRef] [PubMed]
- Peretto, G.; Sala, S.; De Luca, G.; Marcolongo, R.; Campochiaro, C.; Sartorelli, S.; Tresoldi, M.; Foppoli, L.; Palmisano, A.; Esposito, A.; et al. Immunosuppressive therapy and risk stratification of patients with myocarditis presenting with ventricular arrhythmias. JACC Clin. Electrophysiol. 2020, 6, 1221–1234. [Google Scholar] [CrossRef] [PubMed]
- Aquaro, G.D.; Habtemicael, Y.G.; Camastra, G.; Monti, L.; Dellegrottaglie, S.; Moro, C.; Lanzillo, C.; Scatteia, A.; Di Roma, M.; Pontone, G.; et al. Prognostic value of repeating cardiac magnetic resonance in patients with acute myocarditis. J. Am. Coll. Cardiol. 2019, 74, 2339–2348. [Google Scholar] [CrossRef] [PubMed]
- Georgiopoulos, G.; Figliozzi, S.; Sanguineti, F.; Aquaro, G.D.; di Bella, G.; Stamatelopoulos, K.; Chiribiri, A.; Garot, J.; Masci, P.G.; Ismail, T.F. Prognostic impact of late gadolinium enhancement by cardiovascular magnetic resonance in myocarditis. A systematic review and meta-analysis. Circ. Cardiovasc. Imaging 2021, 14, e011492. [Google Scholar] [CrossRef]
- Blissett, S.; Chocron, Y.; Kovacina, B.; Afilalo, J. Diagnostic and prognostic value of cardiac magnetic resonance in acute myocarditis: A systematic review and meta-analysis. Int. J. Cardiovasc. Imaging 2019, 35, 2221–2229. [Google Scholar] [CrossRef]
- Lota, A.S.; Tsao, A.; Owen, R.; Halliday, B.P.; Auger, D.; Vassiliou, V.S.; Tayal, U.; Almogheer, B.; Vilches, S.; Al-Balah, A.; et al. Prognostic Significance of Nonischemic Myocardial Fibrosis in Patients With Normal LV Volumes and Ejection-Fraction. J. Am. Coll. Cardiol. Imaging 2021, 14, 2353–2365. [Google Scholar] [CrossRef]
- Fischer, K.; Obrist, S.J.; Erne, S.A.; Stark, A.W.; Marggraf, M.; Kaneko, K.; Guensch, D.P.; Huber, A.T.; Greulich, S.; Aghayev, A.; et al. Feature tracking myocardial strain incrementally improves prognostication in myocarditis beyond traditional CMR imaging features. J. Am. Coll. Cardiol. Imaging 2020, 13, 1891–1901. [Google Scholar] [CrossRef]
- Spieker, M.; Haberkorn, S.; Gastl, M.; Behm, P.; Katsianos, S.; Horn, P.; Jacoby, C.; Schnackenburg, B.; Reinecke, P.; Kelm, M.; et al. Abnormal T2 mapping cardiovascular magnetic resonance correlates with adverse clinical outcome in patients with suspected acute myocarditis. J. Cardiovasc. Magn. Reson. 2017, 19, 38. [Google Scholar] [CrossRef] [PubMed]
- Bohnen, S.; Radunski, U.; Lund, G.; Ojeda, F.; Looft, Y.; Senel, M.; Radziwolek, L.; Avanesov, M.; Tahir, E.; Stehning, C.; et al. Tissue characterization by T1 and T2 mapping cardiovascular magnetic resonance imaging to monitor myocardial inflammation and healing. Eur. Heart J.-Cardiovasc. Imaging 2017, 18, 744–751. [Google Scholar] [CrossRef] [PubMed]
- Gräni, C.; Bière, L.; Eichhorn, C.; Kaneko, K.; Agarwal, V.; Aghayev, A.; Steigner, M.; Blankstein, R.; Jerosch-Herold, M.; Kwong, R.Y. Incremental value of extracellular volume assessment by cardiovascular magnetica resonance imaging in risk stratifying patients with suspected myocarditis. Int. J. Cardiovasc. Imaging 2019, 35, 1067–1078. [Google Scholar] [CrossRef] [PubMed]

| All n = 207 | EMB-Proven Myocarditis n = 51 | Clinically Suspected Myocarditis n = 156 | p-Value | |
|---|---|---|---|---|
| Age, years | 36 (24–47) | 41 ± 15 | 35 ± 14 | 0.01 |
| Female | 54 (26%) | 20 (39%) | 34 (22%) | 0.014 |
| FHx ID * | 23 (11%) | 7 (14%) | 16 (10%) | 0.52 |
| FHx CAD † | 42 (21%) | 12 (25%) | 30 (20%) | 0.45 |
| Previous viral infection * | 91 (45%) | 12 (24%) | 79 (52%) | <0.001 |
| ID | 25 (12%) | 11 (22%) | 14 (9%) | 0.017 |
| Arrhythmic presentation | 16 (8%) | 8 (16%) | 8 (5%) | 0.014 |
| HF presentation | 41 (20%) | 32 (63%) | 9 (6%) | <0.001 |
| Infarct-like presentation | 144 (70%) | 9 (18%) | 135 (87%) | <0.001 |
| Symptom duration before diagnosis (mo) | 1.00 (0.17–6.00) | 2.00 (1.00–11.25) | 0.15 (0.03–1.25) | <0.001 |
| NYHA class at diagnosis ‡, I | 167 (81%) | 18 (36%) | 149 (96%) | <0.001 |
| II–IV | 39 (19%) | 32 (64%) | 7 (4%) | |
| Left HF | 37 (18%) | 31 (61%) | 6 (4%) | <0.001 |
| Right HF | 14 (7%) | 12 (24%) | 2 (1%) | <0.001 |
| Sinus rhythm * | 198 (97%) | 47 (92%) | 151 (99%) | 0.057 |
| Atrial fibrillation * | 3 (1%) | 2 (4%) | 1 (1%) | |
| Left bundle branch block § | 9 (4%) | 8 (16%) | 1 (1%) | <0.001 |
| Right bundle branch block § | 13 (6%) | 6 (12%) | 7 (5%) | <0.001 |
| Troponin I peak, ng/L ? | 3350 (276–10,575) | 210 (0–7930) | 4963 (1100–11,100) | <0.001 |
| CRP peak, mg/dL # | 19.2 (4.9–50.0) | 6.8 (3.1–21.8) | 25.5 (7.0–51.5) | 0.004 |
| LV diastolic diameter, mm ** | 51 ± 7 | 56.2 ± 9.8 | 49.6 ± 4.9 | <0.001 |
| Left atrial volume mL/m2 ‡‡ | 33 ± 13 | 43 ± 18 | 30 ± 10 | <0.001 |
| LVEDVi, mL/m2 ? | 71 ± 25 | 92 ± 39 | 64 ± 12 | <0.001 |
| LVEF, % §§ | 52 ± 14 | 36.9 ± 16.2 | 57.0 ± 7.3 | <0.001 |
| RVEDA, cm2 ?? | 21.3 ± 5.2 | 23.0 ± 7.3 | 20.8 ± 4.1 | 0.21 |
| RVFAC, % ## | 42 ± 10 | 33.6 ± 10.2 | 45.4 ± 7.1 | <0.001 |
| All n = 207 | EMB-Proven Myocarditis n = 51 | Clinically Suspected Myocarditis n = 156 | p-Value | |
|---|---|---|---|---|
| LVEDVi mL/m2 | 90 (79–106) | 110 (92–156) | 86 (78–98) | <0.001 |
| LVESVi mL/m2 | 38 (31–48) | 69 (41–118) | 36 (30–42) | <0.001 |
| LVSV mL | 93 (76–106) | 67 (53–86) | 96 (83–111) | <0.001 |
| LVEF % | 57 (51–62) | 33 (23–51) | 59 (55–62) | <0.001 |
| LV mass, g/m2 | 61 (52–74) | 76 (58–85) | 59 (51–69) | <0.001 |
| LV regional WMA | 61 (29%) | 21 (41%) | 40 (26%) | 0.035 |
| LV diffuse WMA | 33 (16%) | 28 (55%) | 5 (3%) | <0.001 |
| RVEDVi mL/m2 | 83 (74–96) | 84 (70–100) | 83 (74–94) | 0.86 |
| RVESVi mL/m2 | 35 (28–44) | 45 (31–57) | 34 (27–40) | <0.001 |
| RVSV mL | 90 (72–106) | 68 (56–86) | 96 (81–109) | <0.001 |
| RVEF % | 58 (53–63) | 47 (36–56) | 59 (56–60) | <0.001 |
| Edema | 129 (62%) | 19 (37%) | 110 (70%) | <0.001 |
| LV segments with edema | 3 (2–5) | 2 (2–6) | 3 (2–4) | 0.53 |
| Transmural edema | 48 (38%) | 7 (37%) | 41 (38%) | 0.9 |
| EGE | 83 (40%) | 13 (25%) | 70 (45%) | 0.015 |
| LGE | 193 (93%) | 45 (88%) | 147 (94%) | 0.15 |
| LV segments with LGE | 3 (2–5) | 2 (2–4) | 3 (2–5) | 0.24 |
| Transmural LGE | 41 (21%) | 14 (30%) | 27 (18%) | 0.081 |
| LGE mass, g | 3.5 (1.7–7.5) | 3.3 (1.6–7.6) | 3.5 (1.7–7.5) | 0.88 |
| LGE mass, % of LV | 3.0 (1.5–6.1) | 2.5 (1.0–6.2) | 3.2 (1.6–5.9) | 0.29 |
| All n = 201 | EMB-Proven Myocarditis n = 49 | Clinically Suspected Myocarditis n = 152 | p-Value | |
|---|---|---|---|---|
| Duration of the follow-up (months) | 32 (14–61) | 42 (17–64) | 30 (14–57) | 0.16 |
| Dead or transplanted | 1 (0%) | 1 (2%) | 0 (0%) | 0.074 |
| NYHA class, I | 188 (94%) | 40 (85%) | 148 (97%) | 0.001 |
| II–IV | 11 (6%) | 7 (15%) | 4 (3%) | |
| Sinus rhythm | 187 (96%) | 40 (87%) | 147 (99%) | <0.001 |
| Atrial fibrillation | 4 (2%) | 4 (9%) | 0 (0%) | |
| Beta-blockers | 63 (31%) | 33 (67%) | 30 (20%) | 0.002 |
| Ivabradine | 6 (3%) | 4 (8%) | 2 (1%) | 0.014 |
| ACE inhibitors * | 59 (32%) | 20 (44%) | 39 (27%) | 0.033 |
| ARB † | 10 (9%) | 8 (22%) | 2 (3%) | <0.001 |
| Amiodarone | 2 (1%) | 2 (4%) | 0 (0%) | 0.012 |
| Anticoagulants * | 7 (4%) | 7 (16%) | 0 (0%) | <0.001 |
| LV end-diastolic diameter, mm ‡ | 49.4 ± 6.3 | 52.1 ± 8.8 | 48.6 ± 5.1 | 0.005 |
| Left atrial volume, mL/mq § | 23.3 ± 10.1 | 26.0 ± 13.5 | 22.0 ± 7.6 | 0.32 |
| LVEDVi, mL/mq ? | 59 ± 17 | 69 ± 28 | 56 ± 11 | <0.001 |
| LVEF, % # | 62.4 ± 8.1 | 57.4 ± 11.3 | 64.0 ± 6.0 | <0.001 |
| RVEDA, cm ‡ | 18.5 ± 4.6 | 18.8 ± 6.5 | 18.5 ± 3.9 | 0.50 |
| RVFAC, % ** | 48.9 ± 8.0 | 48.3 ± 10.1 | 49.2 ± 7.2 | 0.68 |
| 0–6 Months | 6–12 Months | 12–24 Months | >24 Months | Any Time Point | |
|---|---|---|---|---|---|
| Number of Events | 10 | 9 | 9 | 3 | 17 |
| LVEDVi mL/m2 | HR 1.01 (95% CI 1.01–1.02, p < 0.001) | HR 1.02 (95% CI 1.01–1.03, p < 0.001) | HR 1.02 (95% CI 1.01–1.03, p < 0.001) | HR 1.05 (95% CI 1.01–1.08, p = 0.006) | HR 1.02 (95% CI 1.02–1.03, p < 0.001) |
| LVESVi mL/m2 | HR 1.01 (95%CI 1.01–1.02, p < 0.001) | HR 1.01 (95% CI 1.01–1.02, p < 0.001) | HR 1.02 (95% CI 1.01–1.03, p < 0.001) | HR 1.06 (95% CI 1.01–1.12, p = 0.013) | HR 1.02 (95% CI 1.02–1.03, p < 0.001) |
| LVEF % | HR 0.93 (95% CI 0.89–0.97, p < 0.001) | HR 0.92 (95% CI 0.88–0.96, p < 0.001) | HR 0.91 (95% CI 0.86–0.97, p = 0.002) | HR 0.90 (95% CI 0.82–0.98, p = 0.013) | HR 0.89 (95% CI 0.88–0.94, p < 0.001) |
| LV mass, g/m2 | NS | HR 1.02 (95% CI 1.00–1.04, p = 0.027) | HR 1.03 (95% CI 1.01–1.04, p = 0.005) | NS | HR 1.04 (95% CI 1.02–1.05, p < 0.001) |
| LV regional WMA | NS | NS | NS | NS | NS |
| LV diffuse WMA | HR 10.8 (95% CI 2.26–51.3, p = 0.003) | HR 7.62 (95% CI 1.87–30.7, p = 0.004) | HR 6.79 (95% CI 1.12–41.3, p = 0.037) | NS | HR 22.4 (95% CI 6.41–78, p < 0.001) |
| RVEDVi mL/m2 | HR 1.03 (95% CI 1.01–1.06, p = 0.002) | HR 1.04 (95% CI 1.02–1.07, p < 0.001) | HR 1.06 (95% CI 1.03–1.08, p < 0.001) | HR 1.07 (95% CI 1.00–1.14, p = 0.038) | HR 1.04 (95% CI 1.02–1.06, p < 0.001) |
| RVESVi mL/m2 | HR 1.04 (95% CI 1.02–1.06, p < 0.001) | HR 1.03 (95% CI 1.03–1.07, p < 0.001) | HR 1.05 (95% CI 1.03–1.07, p < 0.001) | HR 1.10 (95% CI 1.02–1.19, p = 0.015) | HR 1.04 (95% CI 1.03–1.06, p < 0.001) |
| RVEF % | HR 0.9 (95%CI 0.86–0.95, p < 0.001) | HR 0.90 (95% CI 0.86–0.94, p < 0.001) | HR 0.90 (95% CI 0.85–0.95, p < 0.001) | HR 0.88 (95% CI 0.80–0.98, p = 0.014) | HR 0.91 (95% CI 0.88–0.94, p < 0.001) |
| Edema | NS | NS | NS | NS | NS |
| Transmural edema | NS | NS | NS | NS | NS |
| EGE | NS | NS | NS | NS | NS |
| LGE | NS | NS | NS | NS | NS |
| LGE > 1 wall | NS | HR 0.21 (95% CI 0.05–0.86, p = 0.029) | NS | NS | HR 0.03 (95% CI 0.01–0.13, p < 0.001) |
| Transmural LGE | NS | HR 7.26 (95% CI 1.84–28.7, p = 0.005) | NS | NS | NS |
| LGE mass, g | NS | NS | NS | NS | NS |
| LGE mass, % of LV | NS | NS | NS | NS | HR 0.73 (95% CI 0.55–0.97, p = 0.033) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Baritussio, A.; Cheng, C.-Y.; Simeti, G.; Ocagli, H.; Lorenzoni, G.; Giordani, A.S.; Basso, C.; Rizzo, S.; De Gaspari, M.; Motta, R.; et al. CMR Predictors of Favorable Outcome in Myocarditis: A Single-Center Experience. J. Clin. Med. 2024, 13, 1229. https://doi.org/10.3390/jcm13051229
Baritussio A, Cheng C-Y, Simeti G, Ocagli H, Lorenzoni G, Giordani AS, Basso C, Rizzo S, De Gaspari M, Motta R, et al. CMR Predictors of Favorable Outcome in Myocarditis: A Single-Center Experience. Journal of Clinical Medicine. 2024; 13(5):1229. https://doi.org/10.3390/jcm13051229
Chicago/Turabian StyleBaritussio, Anna, Chun-Yan Cheng, Giuseppe Simeti, Honoria Ocagli, Giulia Lorenzoni, Andrea Silvio Giordani, Cristina Basso, Stefania Rizzo, Monica De Gaspari, Raffaella Motta, and et al. 2024. "CMR Predictors of Favorable Outcome in Myocarditis: A Single-Center Experience" Journal of Clinical Medicine 13, no. 5: 1229. https://doi.org/10.3390/jcm13051229