Immediate vs. Delayed Placement of Immediately Provisionalized Self-Tapping Implants: A Non-Randomized Controlled Clinical Trial with 1 Year of Follow-Up
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design
Inclusion/Exclusion Criteria
2.2. Surgical Protocol
2.3. Prosthetic Protocol
2.4. Follow-Up and Outcome Variables
2.5. Statistics
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Lemos, C.A.A.; Verri, F.R.; Bonfante, E.A.; Júnior, J.F.S.; Pellizzer, E.P. Comparison of external and internal implant-abutment connections for implant supported prostheses. A systematic review and meta-analysis. J. Dent. 2018, 70, 14–22. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Prato, G.P.P.; Gianfilippo, R.D.; Wang, H.-L. Success in periodontology: An evolutive concept. J. Clin. Periodontol. 2019, 46, 840–845. [Google Scholar] [CrossRef] [PubMed]
- Buser, D.; Sennerby, L.; Bruyn, H.D. Modern implant dentistry based on osseointegration: 50 years of progress, current trends and open questions. Periodontol. 2000 2017, 73, 7–21. [Google Scholar] [CrossRef]
- Carosi, P.; Ferrigno, N.; Arcuri, C.; Laureti, M. Computer-Aided Surgery and Immediate Loading to Rehabilitate Complete Arch with Four Dental Implants and Fixed Screw-Retained Prosthesis Up to 4 Years in Function: A Retrospective Study. Int. J. Oral Maxillofac. Implant. 2021, 36, 1180–1187. [Google Scholar] [CrossRef] [PubMed]
- Chen, S.T.; Buser, D. Clinical and esthetic outcomes of implants placed in postextraction sites. Int. J. Oral Maxillofac. Implant. 2009, 24, 186–217. [Google Scholar]
- Carosi, P.; Lorenzi, C.; Lio, F.; Cardelli, P.; Pinto, A.; Laureti, A.; Pozzi, A. Accuracy of Computer-Assisted Flapless Implant Placement by Means of Mucosa-Supported Templates in Complete-Arch Restorations: A Systematic Review. Materials 2022, 15, 1462. [Google Scholar] [CrossRef]
- Pozzi, A.; Arcuri, L.; Carosi, P.; Nardi, A.; Kan, J. Clinical and radiological outcomes of novel digital workflow and dynamic navigation for single-implant immediate loading in aesthetic zone: 1-year prospective case series. Clin. Oral Implant. Res. 2021, 32, 1397–1410. [Google Scholar] [CrossRef]
- Gianfilippo, R.D.; Chambrone, L.; Prato, G.; Nevins, M.; Franceschi, D. Paradigm Shifts in the Evolution of Implant Therapy. Int. J. Periodontics Restor. Dent. 2022, 42, 605–612. [Google Scholar] [CrossRef]
- Gallucci, G.O.; Hamilton, A.; Zhou, W.; Buser, D.; Chen, S. Implant placement and loading protocols in partially edentulous patients: A systematic review. Clin. Oral Implant. Res. 2018, 29 (Suppl. S16), 106–134. [Google Scholar] [CrossRef] [Green Version]
- Carosi, F.; Ottria, L.; Lio, F.; Laureti, A.; Papi, P. The health of soft tissues around four dental implants loaded immediately supporting a 4-year-old fixed screw-retained prosthesis. J. Biol. Regul. Homeost. Agents 2021, 35, 57–66. [Google Scholar]
- Hämmerle, C.H.F.; Chen, S.T.; Wilson, T.G. Consensus statements and recommended clinical procedures regarding the placement of implants in extraction sockets. Int. J. Oral Maxillofac. Implant. 2004, 19, 26–28. [Google Scholar]
- Chen, S.T.; Darby, I. The relationship between facial bone wall defects and dimensional alterations of the ridge following flapless tooth extraction in the anterior maxilla. Clin. Oral Implant. Res. 2016, 28, 931–937. [Google Scholar] [CrossRef]
- Gallucci, G.O.; Benic, G.I.; Eckert, S.E.; Papaspyridakos, P.; Schimmel, M.; Schrott, A.; Weber, H.P. Consensus statements and clinical recommendations for implant loading protocols. Int. J. Oral Maxillofac. Implant. 2014, 29, 287–290. [Google Scholar] [CrossRef]
- Pozzi, A.; Hansson, L.; Carosi, P.; Arcuri, L. Dynamic navigation guided surgery and prosthetics for immediate loading of complete-arch restoration. J. Esthet. Restor. Dent. 2021, 33, 224–236. [Google Scholar] [CrossRef]
- Pozzi, A.; Tallarico, M.; Moy, P.K. Immediate loading with a novel implant featured by variable-threaded geometry, internal conical connection and platform shifting: Three-year results from a prospective cohort study. Eur. J. Oral Implantol. 2015, 8, 51–63. [Google Scholar]
- Albertini, M.; Herrero-Climent, F.; Díaz-Castro, C.M.; Nart, J.; Fernández-Palacín, A.; Ríos-Santos, J.V.; Herrero-Climent, M. A Radiographic and Clinical Comparison of Immediate vs. Early Loading (4 Weeks) of Implants with a New Thermo-Chemically Treated Surface: A Randomized Clinical Trial. Int. J. Environ Res. Public Health 2021, 18, 1223. [Google Scholar] [CrossRef]
- Al-Tarawneh, S.K.; Thalji, G.; Cooper, L.F. Macrogeometric Differentiation of Dental Implant Primary Stability: An In Vitro Study. Int. J. Oral Maxillofac. Implants 2022, 37, 1110–1118. [Google Scholar] [CrossRef]
- Sartoretto, S.C.; Calasans-Maia, J.; Resende, R.; Câmara, E.; Ghiraldini, B.; Barbosa Bezerra, F.J.; Granjeiro, J.M.; Calasans-Maia, M.D. The Influence of Nanostructured Hydroxyapatite Surface in the Early Stages of Osseointegration: A Multiparameter Animal Study in Low-Density Bone. Int. J. Nanomed. 2020, 15, 8803–8817. [Google Scholar] [CrossRef]
- Duyck, J.; Corpas, L.; Vermeiren, S.; Ogawa, T.; Quirynen, M.; Vandamme, K.; Jacobs, R.; Naert, I. Histological, histomorphometrical, and radiological evaluation of an experimental implant design with a high insertion torque: Evaluation of experimental implant design with high insertion torque. Clin. Oral Implant. Res. 2010, 21, 877–884. [Google Scholar] [CrossRef]
- Von Elm, E.; Altman, D.G.; Egger, M.; Pocock, S.J.; Gøtzsche, P.C.; Vandenbroucke, J.P.; STROBE Initiative. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) Statement: Guidelines for reporting observational studies. Int. J. Surg. 2014, 12, 1495–1499. [Google Scholar] [CrossRef] [Green Version]
- Apfelbaum, J.L.; Connis, R.T. The American Society of Anesthesiologists Practice Parameter Methodology. Anesthesiology 2019, 130, 367–384. [Google Scholar] [CrossRef] [PubMed]
- Pan, H.Y.; Yang, H.; Zhang, R.; Yang, Y.M.; Wang, H.; Hu, T.; Dummer, P. Use of cone-beam computed tomography to evaluate the prevalence of root fenestration in a Chinese subpopulation. Int. Endod. J. 2013, 47, 10–19. [Google Scholar] [CrossRef]
- Yang, Y.; Yang, H.; Pan, H.; Xu, J.; Hu, T. Evaluation and New Classification of Alveolar Bone Dehiscences Using Cone-beam Computed Tomography in vivo. Int. J. Morphol. 2015, 33, 361–368. [Google Scholar] [CrossRef]
- Carosi, P.; Ferrigno, N.; Renzi, G.D.; Laureti, M. Digital Workflow to Merge an Intraoral Scan and CBCT of Edentulous Maxilla: A Technical Report. J. Prosthodont. 2020, 29, 730–732. [Google Scholar] [CrossRef] [PubMed]
- Steigmann, L.; Steigmann, M.; Di Gianfilippo, R.; Wang, I.-C.; Wang, H.-L.; Chan, H.-L. Comparative Assessment of Flap-Advancing Techniques in an Ex Vivo Cadaverous Porcine Model. Int. J. Oral Maxillofac. Implant. 2022, 37, 823–829. [Google Scholar] [CrossRef]
- Morton, D.; Gallucci, G.; Lin, W.; Pjetursson, B.; Polido, W.; Roehling, S.; Sailer, I.; Aghaloo, T.; Albera, H.; Bohner, L.; et al. Group 2 ITI Consensus Report: Prosthodontics and implant dentistry. Clin. Oral Implant. Res. 2018, 29 (Suppl. S16), 215–223. [Google Scholar] [CrossRef]
- Retzepi, M.; Donos, N. Guided Bone Regeneration: Biological principle and therapeutic applications. Clin. Oral Implant. Res. 2010, 21, 567–576. [Google Scholar] [CrossRef]
- Askar, H.; Di Gianfilippo, R.; Ravida, A.; Tattan, M.; Majzoub, J.; Wang, H. Incidence and severity of postoperative complications following oral, periodontal and implant surgeries: A retrospective study. J. Periodontol. 2019, 90, 1270–1278. [Google Scholar] [CrossRef]
- Berglundh, T.; Armitage, G.; Araujo, M.G.; Avila-Ortiz, G.; Blanco, J.; Camargo, P.M.; Chen, S.; Cochran, D.; Derks, J.; Figuero, E.; et al. Peri-implant diseases and conditions: Consensus report of workgroup 4 of the 2017 World Workshop on the Classification of Periodontal and Peri-Implant Diseases and Conditions. J. Periodontol. 2018, 89, S313–S318. [Google Scholar] [CrossRef]
- Belser, U.C.; Grütter, L.; Vailati, F.; Bornstein, M.M.; Weber, H.-P.; Buser, D. Outcome evaluation of early placed maxillary anterior single-tooth implants using objective esthetic criteria: A cross-sectional, retrospective study in 45 patients with a 2- to 4-year follow-up using pink and white esthetic scores. J. Periodontol. 2009, 80, 140–151. [Google Scholar] [CrossRef]
- Mombelli, A.; Lang, N.P. The diagnosis and treatment of peri-implantitis. Periodontol. 2000 1998, 17, 63–76. [Google Scholar] [CrossRef]
- Cheng, Q.; Su, Y.-Y.; Wang, X.; Chen, S. Clinical Outcomes Following Immediate Loading of Single-Tooth Implants in the Esthetic Zone: A Systematic Review and Meta-Analysis. Int. J. Oral Maxillofac. Implant. 2020, 35, 167–177. [Google Scholar] [CrossRef]
- Francisco, H.; Finelle, G.; Bornert, F.; Sandgren, R.; Herber, V.; Warfving, N.; Pippenger, B.E. Peri-implant bone preservation of a novel, self-cutting, and fully tapered implant in the healed crestal ridge of minipigs: Submerged vs. transgingival healing. Clin. Oral Investig. 2021, 25, 6821–6832. [Google Scholar] [CrossRef]
- Limmeechokchai, S.; Kan, J.; Rungcharassaeng, K.; Goodacre, C.J.; Lozada, J.; Oyoyo, U. Heat and Sound Generation During Implant Osteotomy When Using Different Types of Drills in Artificial and Bovine Bone Blocks. J. Oral Implant. 2021, 48, 187–193. [Google Scholar] [CrossRef]
- Cha, J.Y.; Pereira, M.; Smith, A.; Houschyar, K.; Yin, X.; Mouraret, S.; Brunski, J.; Helms, J. Multiscale analyses of the bone-implant interface. J. Dent. Res. 2015, 94, 482–490. [Google Scholar] [CrossRef] [Green Version]
- Gianfilippo, R.D.; Valente, N.A.; Toti, P.; Wang, H.-L.; Barone, A. Influence of implant mucosal thickness on early bone loss: A systematic review with meta-analysis. J. Periodontal Implant. Sci. 2020, 50, 209. [Google Scholar] [CrossRef]
- Lin, G.-H.; Chan, H.-L.; Bashutski, J.D.; Oh, T.-J.; Wang, H.-L. The effect of flapless surgery on implant survival and marginal bone level: A systematic review and meta-analysis. J. Periodontol. 2013, 85, e91–e103. [Google Scholar] [CrossRef]
- Kim, J.-I.; Choi, B.-H.; Li, J.; Xuan, F.; Jeong, S.-M. Blood vessels of the peri-implant mucosa: A comparison between flap and flapless procedures. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endodontology 2009, 107, 508–512. [Google Scholar] [CrossRef]
- Raico Gallardo, Y.N.; Da Silva-Olivio, I.R.T.; Mukai, E.; Morimoto, S.; Sesma, N.; Cordaro, L. Accuracy comparison of guided surgery for dental implants according to the tissue of support: A systematic review and meta-analysis. Clin. Oral Implant. Res. 2016, 28, 602–612. [Google Scholar] [CrossRef]
- Testori, T.; Weinstein, T.; Scutellà, F.; Wang, H.-L.; Zucchelli, G. Implant placement in the esthetic area: Criteria for positioning single and multiple implants. Periodontol. 2000 2018, 77, 176–196. [Google Scholar] [CrossRef]
- Pigozzo, M.N.; Da Costa, T.R.; Sesma, N.; Laganá, D.C. Immediate versus early loading of single dental implants: A systematic review and meta-analysis. J. Prosthet. Dent. 2018, 120, 25–34. [Google Scholar] [CrossRef] [PubMed]
- Velasco-Ortega, E.; Jiménez-Guerra, A.; Ortiz-Garcia, I.; Moreno-Muñoz, J.; Núñez-Márquez, E.; Cabanillas-Balsera, D.; López-López, J.; Monsalve-Guil, L. Immediate Loading of Implants Placed by Guided Surgery in Geriatric Edentulous Mandible Patients. Int. J. Environ Res. Public Health 2021, 18, 4125. [Google Scholar] [CrossRef] [PubMed]
- Kan, J.Y.K.; Rungcharassaeng, K.; Deflorian, M.; Weinstein, T.; Wang, H.L.; Testori, T. Immediate implant placement and provisionalization of maxillary anterior single implants. Periodontol. 2000 2018, 77, 197–212. [Google Scholar] [CrossRef] [PubMed]
- Del Fabbro, M.; Testori, T.; Kekovic, V.; Goker, F.; Tumedei, M.; Wang, H.L. A Systematic Review of Survival Rates of Osseointegrated Implants in Fully and Partially Edentulous Patients Following Immediate Loading. J. Clin. Med. 2019, 8, 2142. [Google Scholar] [CrossRef]
- Yan, Q.; Xiao, L.-Q.; Su, M.; Mei, Y.; Shi, B. Soft and Hard Tissue Changes Following Immediate Placement or Immediate Restoration of Single-Tooth Implants in the Esthetic Zone: A Systematic Review and Meta-Analysis. Int. J. Oral Maxillofac. Implant. 2016, 31, 1327–1340. [Google Scholar] [CrossRef]
- Ammarullah, M.I.; Santoso, G.; Sugiharto, S.; Supriyono, T.; Wibowo, D.B.; Kurdi, O.; Tauviqirrahman, M.; Jamari, J. Minimizing Risk of Failure from Ceramic-on-Ceramic Total Hip Prosthesis by Selecting Ceramic Materials Based on Tresca Stress. Sustainability 2022, 14, 13413. [Google Scholar] [CrossRef]











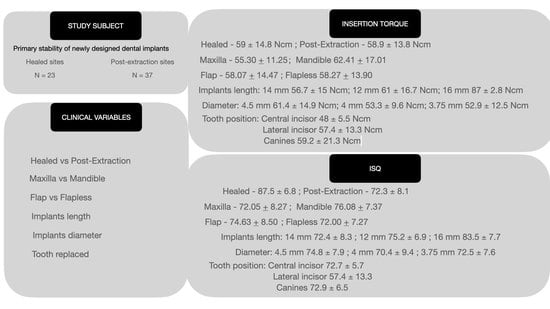
| Implant Stability Quotien (ISQ) (Mean ± SD) | Torque (Mean ± SD, Ncm) | 1-Year Radiographic Marginal Bone Loss (Mean ± SD, mm) | |
|---|---|---|---|
| All implants | 73.6 ± 8.1 | 58.1 ± 14.1 | 0.62 ± 0.1 |
| Immediate implants | 72.3 ± 8.1 | 58.9 ± 13.8 | 0.63 ± 0.4 |
| Delayed implants | 87.5 ± 6.8 | 59 ± 14.8 | 0.61 ± 0.2 |
| p-value | 0.875 | 0.716 | 0.385 |
| Maxilla | 72.05 ± 8.27 | 55.30 ± 11.25 | 0.64 ± 0.6 |
| Mandible | 76.08 ± 7.37 | 62.41 ± 17.01 | 0.60 ± 0.3 |
| p-value | 0.058 | 0.057 | 0.284 |
| Flap | 74.63 ± 8.50 | 58.07 ± 14.47 | 0.63 ± 0.2 |
| Flapless | 72.00 ± 7.27 | 58.27 ± 13.90 | 0.61 ± 0.4 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Carosi, P.; Lorenzi, C.; Di Gianfilippo, R.; Papi, P.; Laureti, A.; Wang, H.-L.; Arcuri, C. Immediate vs. Delayed Placement of Immediately Provisionalized Self-Tapping Implants: A Non-Randomized Controlled Clinical Trial with 1 Year of Follow-Up. J. Clin. Med. 2023, 12, 489. https://doi.org/10.3390/jcm12020489
Carosi P, Lorenzi C, Di Gianfilippo R, Papi P, Laureti A, Wang H-L, Arcuri C. Immediate vs. Delayed Placement of Immediately Provisionalized Self-Tapping Implants: A Non-Randomized Controlled Clinical Trial with 1 Year of Follow-Up. Journal of Clinical Medicine. 2023; 12(2):489. https://doi.org/10.3390/jcm12020489
Chicago/Turabian StyleCarosi, Paolo, Claudia Lorenzi, Riccardo Di Gianfilippo, Piero Papi, Andrea Laureti, Hom-Lay Wang, and Claudio Arcuri. 2023. "Immediate vs. Delayed Placement of Immediately Provisionalized Self-Tapping Implants: A Non-Randomized Controlled Clinical Trial with 1 Year of Follow-Up" Journal of Clinical Medicine 12, no. 2: 489. https://doi.org/10.3390/jcm12020489