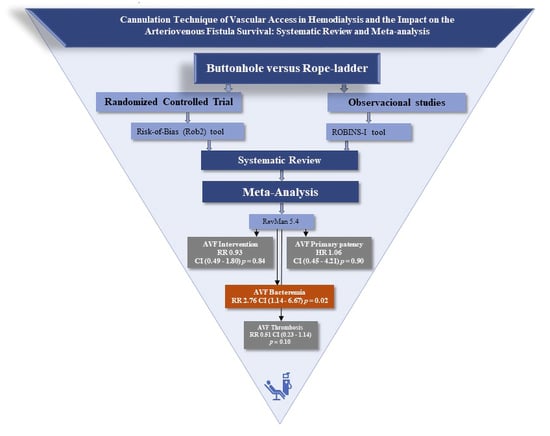
Cannulation Technique of Vascular Access in Hemodialysis and the Impact on the Arteriovenous Fistula Survival: Systematic Review and Meta-Analysis
Abstract
:1. Introduction
2. Materials and Methods
2.1. Search Strategy
2.2. Inclusion and Exclusion Criteria
2.3. Outcome Indicators
2.4. Data Extraction
2.5. Quality Assessment
2.6. Statistical Analysis
3. Results
3.1. Characteristics of the Included Studies
3.2. Risk-of-Bias Assessment for RCT Studies
3.3. Risk-of-Bias Assessment for Observational Studies
3.4. Primary Outcome—Unassisted Primary Patency
3.5. Number of Interventions in the Fistula
3.6. Arteriovenous Fistula Thrombosis
3.7. Bacteremia and/or Localized Signs of Infection Related to Vascular Access
3.8. Cannulation Pain
3.9. Hematoma Associated with Cannulation Techniques
3.10. Bleeding Time Post-Dialysis
3.11. Aneurysm Formation/Aneurysm Enlargement
3.12. Unsuccessful Cannulation
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Lee, T. Novel paradigms for dialysis vascular access: Downstream vascular biology-is there a final common pathway? Clin. J. Am. Soc. Nephrol. 2013, 8, 2194–2201. [Google Scholar] [CrossRef] [PubMed]
- Nath, K.A. Dialysis Vascular Access Intervention and the Search for Biomarkers. J. Am. Soc. Nephrol. 2016, 27, 970–972. [Google Scholar] [CrossRef] [PubMed]
- Ethier, J.; Mendelssohn, D.C.; Elder, S.J.; Hasegawa, T.; Akizawa, T.; Akiba, T.; Canaud, B.J.; Pisoni, R.L. Vascular access use and outcomes: An international perspective from the dialysis outcomes and practice patterns study. Nephrol. Dial. Transplant. 2008, 23, 3219–3226. [Google Scholar] [CrossRef] [PubMed]
- Feldman, H.I.; Held, P.J.; Hutchinson, J.T.; Stoiber, E.; Hartigan, M.F.; Berlin, J.A. Hemodialysis vascular access morbidity in the United States. Kidney Int. 1993, 43, 1091–1096. [Google Scholar] [CrossRef] [PubMed]
- Roy-Chaudhury, P.; Sukhatme Vikas, P.; Cheung, A.K. Hemodialysis Vascular Access Dysfunction: A Cellular and Molecular Viewpoint. J. Am. Soc. Nephrol. 2006, 17, 1112–1127. [Google Scholar] [CrossRef]
- Dhingra, R.K.; Young, E.W.; Hulbert-Shearon, T.E.; Leavey Sean, F.; Port, F.K. Type of vascular access and mortality in U.S. hemodialysis patients. Kidney Int. 2001, 60, 1443–1451. [Google Scholar] [CrossRef]
- McCann, M.; Einarsdottir, H.; Waeleghem, J.P.V.; Murphy, F.; Sedgwick, J. Vascular access management II: AVF/AVG cannulation techniques and complications. J. Ren. Care 2009, 35, 90–98. [Google Scholar] [CrossRef]
- Gallieni, M.; Hollenbeck, M.; Inston, N.; Kumwenda, M.; Powell, S.; Tordoir, J.; Al Shakarchi, J.; Berger, P.; Bolignano, D.; Cassidy, D.; et al. Clinical practice guideline on peri- and postoperative care of arteriovenous fistulas and grafts for haemodialysis in adults. Nephrol. Dial. Transplant. 2019, 34, II1–II42. [Google Scholar] [CrossRef]
- Ibeas, J.; Roca-Tey, R.; Vallespín, J.; Moreno, T.; Moñux, G.; Martí-Monrós, A.; del Pozo, J.L.; Gruss, E.; de Arellano, M.R.; Fontseré, N.; et al. Spanish Clinical Guidelines on Vascular Access for Haemodialysis. Nefrologia 2017, 37 (Suppl. S1), 1–191. [Google Scholar] [CrossRef]
- Lok, C.E.; Huber, T.S.; Lee, T.; Shenoy, S.; Yevzlin, A.S.; Abreo, K.; Allon, M.; Asif, A.; Astor, B.C.; Glickman, M.H.; et al. KDOQI Clinical Practice Guideline for Vascular Access: 2019 Update. Am. J. Kidney Dis. 2020, 75, S1–S164. [Google Scholar] [CrossRef]
- Aitken, E.; McLellan, A.; Glen, J.; Serpell, M.; Mactier, R.; Clancy, M. Pain resulting from arteriovenous fistulae: Prevalence and impact. Clin. Nephrol. 2013, 80, 328–333. [Google Scholar] [CrossRef] [PubMed]
- da Silva, O.M.; Rigon, E.; Dalazen, J.; Bissoloti, A.; Rabelo-Silva, E.R. Pain during Arteriovenous Fistula Cannulation in Chronic Renal Patients on Hemodialysis. Open J. Nurs. 2016, 06, 1028–1037. [Google Scholar] [CrossRef]
- MacRae, J.M.; Ahmed, S.B.; Atkar, R.; Hemmelgarn, B.R. A randomized trial comparing buttonhole with rope ladder needling in conventional hemodialysis patients. Clin. J. Am. Soc. Nephrol. 2012, 7, 1632–1638. [Google Scholar] [CrossRef] [PubMed]
- Van Loon, M.M.; Goovaerts, T.; Kessels, A.G.H.; Van Der Sande, F.M.; Tordoir, J.H.M. Buttonhole needling of haemodialysis arteriovenous fistulae results in less complications and interventions compared to the rope-ladder technique. Nephrol. Dial. Transplant. 2010, 25, 225–230. [Google Scholar] [CrossRef]
- Parisotto, M.T.; Schoder, V.U.; Miriunis, C.; Grassmann, A.H.; Scatizzi, L.P.; Kaufmann, P.; Stopper, A.; Marcelli, D. Cannulation technique influences arteriovenous fistula and graft survival. Kidney Int. 2014, 86, 790–797. [Google Scholar] [CrossRef]
- MacRae, J.M.; Ahmed, S.B.; Hemmelgarn, B.R. Arteriovenous fistula survival and needling technique: Long-term results from a randomized buttonhole trial. Am. J. Kidney Dis. 2014, 63, 636–642. [Google Scholar] [CrossRef]
- Lyman, M.; Nguyen Duc, B.; Shugart, A.; Gruhler, H.; Lines, C.; Patel, P.R. Risk of Vascular Access Infection Associated With Buttonhole Cannulation of Fistulas: Data From the National Healthcare Safety Network. Am. J. Kidney Dis. 2020, 76, 82–89. [Google Scholar] [CrossRef]
- Collier, S.; Kandil, H.; Yewnetu, E.; Cross, J.; Caplin, B.; Davenport, A. Infection Rates Following Buttonhole Cannulation in Hemodialysis Patients. Ther. Apher. Dial. 2016, 20, 476–482. [Google Scholar] [CrossRef]
- Peralta, R.; Fazendeiro Matos, J.; Pinto, B.; Gonçalves, P.; Sousa, R.; Felix, C.; Carvalho, H.; Vinhas, J.; Ponce, P. Multiple single cannulation technique of arteriovenous fistula: A randomized controlled trial. Hemodial. Int. 2022, 26, 4–12. [Google Scholar] [CrossRef]
- Huang, S.H.S.; MacRae, J.; Ross, D.; Imtiaz, R.; Hollingsworth, B.; Nesrallah, G.E.; Copland, M.A.; McFarlane, P.A.; Chan, C.T.; Zimmerman, D. Buttonhole versus stepladder cannulation for home hemodialysis: A multicenter, randomized, pilot trial. Clin. J. Am. Soc. Nephrol. 2019, 14, 403–410. [Google Scholar] [CrossRef]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef]
- Lee, T.; Mokrzycki, M.; Moist, L.; Maya, I.; Vazquez, M.; Lok, C.E. Standardized Definitions for Hemodialysis Vascular Access. Semin. Dial. 2011, 24, 515–524. [Google Scholar] [CrossRef]
- Peralta, R.; Sousa, L.; Cristóvão, A.F. Cannulation technique of vascular access in haemodialysis and the impact on the arteriovenous fistula survival: Protocol of systematic review. Int. J. Environ. Res. Public Health 2022, 18, 12554. [Google Scholar] [CrossRef]
- Sterne, J.A.C.; Savović, J.; Page, M.J.; Elbers, R.G.; Blencowe, N.S.; Boutron, I.; Cates, C.J.; Cheng, H.-Y.; Corbett, M.S.; Eldridge, S.M.; et al. Revised Cochrane Risk-of-Bias Tool for Randomized Trials (RoB 2); Cochrane: London, UK, 2019; pp. 1–24. Available online: https://methods.cochrane.org/risk-bias-2 (accessed on 1 March 2021).
- Sterne, J.A.C.; Hernán, M.A.; Reeves, B.C.; Savović, J.; Berkman, N.D.; Viswanathan, M.; Henry, D.; Altman, D.G.; Ansari, M.T.; Boutron, I.; et al. ROBINS-I: A tool for assessing risk of bias in non-randomized studies of interventions. BMJ 2016, 355, i4919. Available online: http://www.riskofbias.info (accessed on 1 March 2021). [CrossRef] [PubMed]
- Struthers, J.; Allan, A.; Peel, R.K.; Lambie, S.H. Buttonhole needling of ateriovenous fistulae: A randomized controlled trial. ASAIO J. 2010, 56, 319–322. [Google Scholar] [CrossRef] [PubMed]
- Vaux, E.; King, J.; Lloyd, S.; Moore, J.; Bailey, L.; Reading, I.; Naik, R. Effect of buttonhole cannulation with a polycarbonate peg on in-center hemodialysis fistula outcomes: A randomized controlled trial. Am. J. Kidney Dis. 2013, 62, 81–88. [Google Scholar] [CrossRef] [PubMed]
- Chan, M.R.; Shobande, O.; Vats, H.; Wakeen, M.; Meyer, X.; Bellingham, J.; Astor, B.C.; Yevzlin, A.S. The effect of buttonhole cannulation vs. rope-ladder technique on hemodialysis access patency. Semin. Dial. 2014, 27, 210–216. [Google Scholar] [CrossRef]
- Pergolotti, A.; Rich, E.; Lock, K. The effect of the buttonhole method vs. the traditional method of AV fistula cannulation on hemostasis, needle stick pain, pre-needle stick anxiety, and presence of aneurysms in ambulatory patients on hemodialysis. Nephrol. Nurs. J. 2011, 38, 333–336. [Google Scholar]
- Smyth, W.; Hartig, V.; Manickam, V. Outcomes of buttonhole and rope-ladder cannulation techniques in a tropical renal service. J. Ren. Care 2013, 39, 157–165. [Google Scholar] [CrossRef]
- Glerup, R.; Svensson, M.; Jensen, J.D.; Christensen, J.H. Staphylococcus aureus Bacteremia Risk in Hemodialysis Patients Using the Buttonhole Cannulation Technique: A Prospective Multicenter Study. Kidney Med. 2019, 1, 263–270. [Google Scholar] [CrossRef]
- Sukthinthai, N.; Sittipraneet, A.; Tummanittayangkoon, B.; Vasuvattakul, S.; Chanchairujira, T. Buttonhole technique better than area puncture technique on hemostasis and pain associated with needle cannulation. J. Med. Assoc. Thai. 2012, 95 (Suppl. S2), S208–S212. [Google Scholar] [PubMed]
- Kim, M.K.; Kim, H.S. Clinical effects of buttonhole cannulation method on hemodialysis patients. Hemodial. Int. 2013, 17, 294–299. [Google Scholar] [CrossRef] [PubMed]
- Peralta, R.; Matos, J.F.; Carvalho, H. Safe Needling of Arteriovenous Fistulae in Patients on Hemodialysis: Literature Review and a New Approach. Nephrol. Nurs. J. 2021, 48, 169–177. [Google Scholar] [CrossRef]
- Peralta, R.; Sousa, R.; Pinto, B.; Gonçalves, P.; Felix, C.; Fazendeiro Matos, J. Commentary on: “Multiple single cannulation technique of arteriovenous fistula: A randomized controlled trial”. Arch. Nephrol. Ren. Stud. 2021, 1, 28–33. [Google Scholar]
- Sidawy, A.N.; Gray, R.; Besarab, A.; Henry, M.; Ascher, E.; Silva, M., Jr.; Miller, A.; Scher, L.; Trerotola, S.; Gregory, R.T.; et al. Recommended standards for reports dealing with arteriovenous hemodialysis accesses. J. Vasc. Surg. 2002, 35, 603–610. [Google Scholar] [CrossRef] [PubMed]
- Viecelli, A.K.; O’Lone, E.; Sautenet, B.; Craig, J.C.; Tong, A.; Chemla, E.; Hooi, L.S.; Lee, T.; Lok, C.; Polkinghorne, K.R.; et al. Vascular Access Outcomes Reported in Maintenance Hemodialysis Trials: A Systematic Review. Am. J. Kidney Dis. 2018, 71, 382–391. [Google Scholar] [CrossRef] [PubMed]
- Ren, C.; Han, X.; Huang, B.; Yuan, L.; Cao, Y.; Yang, X. Efficacy of buttonhole cannulation (BH) in hemodialysis patients with arteriovenous fistula: A meta-analysis. Int. J. Clin. Exp. Med. 2016, 9, 15363–15370. [Google Scholar]
- Wang, L.-P.; Tsai, L.-H.; Huang, H.-Y.; Okoli, C.; Guo, S.-E. Effect of buttonhole cannulation versus rope- ladder cannulation in hemodialysis patients with vascular access: A systematic review and meta -analysis of randomized/clinical controlled trials. Medicine 2022, 101, e29597. [Google Scholar] [CrossRef]
- Muir, C.A.; Kotwal, S.S.; Hawley, C.M.; Polkinghorne, K.; Gallagher, M.P.; Snelling, P.; Jardine, M.J. Buttonhole cannulation and clinical outcomes in a home hemodialysis cohort and systematic review. Clin. J. Am. Soc. Nephrol. 2014, 9, 110–119. [Google Scholar] [CrossRef]
- Kang, H. Trial sequential analysis: Novel approach for meta-analysis. Anesth. Pain Med. 2021, 16, 138–150. [Google Scholar] [CrossRef]
- Sanfilippo, F.; La Via, L.; Tigano, S.; Morgana, A.; La Rosa, V.; Astuto, M. Trial sequential analysis: The evaluation of the robustness of meta-analyses findings and the need for further research. Euromediterranean Biomed. J. 2021, 16, 104–107. [Google Scholar] [CrossRef]
- Nesrallah, G.E. Pro: Buttonhole cannulation of arteriovenous fistulae. Nephrol. Dial. Transplant. 2016, 31, 520–523. [Google Scholar] [CrossRef] [PubMed]
- Pinto, R.; Duarte, F.; Mata, F.; Sousa, C.; Salgueiro, A.; Fernandes, I. Construção e validação de um modelo de decisão para a canulação da fístula arteriovenosa em hemodiálise. Rev. Enferm. Ref. 2023, VI, 1–8. [Google Scholar] [CrossRef]
- Pinto, R.; Sousa, C.; Salgueiro, A.; Fernandes, I. Arteriovenous fistula cannulation in hemodialysis: A vascular access clinical practice guidelines narrative review. J. Vasc. Access. 2022, 23, 825–831. [Google Scholar] [CrossRef]
- Sousa, C.N.; Apóstolo, J.L.A.; Figueiredo, M.H.J.S.; Dias, V.F.F.; Teles, P.; Martins, M.M. Construction and validation of a scale of assessment of self-care behaviors with arteriovenous fistula in hemodialysis. Hemodial. Int. 2015, 19, 306–313. [Google Scholar] [CrossRef] [PubMed]







| First Author | Publication Year | Origin | Study Design | Context | Sample Size | Interventions | Protocol | Follow-Up (Months) | Outcomes | ||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Experimental Group | Control Group | Experimental Group | Control Group | ||||||||
| MacRae J. et al. [13] | 2012 | Canada | RCT | Center | 140 | BH | Standard needling | Specified | Not specified | 12 | ➀ ➁ ➂ ➄ |
| MacRae J. et al. [16] | 2014 | Canada | RCT | Center | 139 | BH | Standard needling | Specified | Not specified | 19.2 vs. 17.2 | ➄ ➇ ➈ ➉ |
| Peralta R. et al. [19] | 2022 | Portugal | RCT | Multicentric | 172 | MuST | BH and RL | Specified | Specified | 12 | ➃ ➄ ➈ ➉ |
| Struthers J. et al. [26] | 2010 | United Kingdom | RCT | Center | 56 | BH | Traditional RL | Specified | Not specified | 6 | ➀ ➁ ➂ ➃ ➄ ➇ |
| Vaux E. et al. [27] | 2013 | United Kingdom | RCT | Center | 127 | BH | Usual practice | Specified | Not specified | 12 | ➀ ➁ ➂ ➃ ➄ ➈ ➉ |
| Chan M. et al. [28] | 2014 | USA | CCT | Center | 83 | BH | RL | Specified | Not specified | 12 | ➄ ➈ |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Peralta, R.; Sousa, L.; Cristovão, A.F. Cannulation Technique of Vascular Access in Hemodialysis and the Impact on the Arteriovenous Fistula Survival: Systematic Review and Meta-Analysis. J. Clin. Med. 2023, 12, 5946. https://doi.org/10.3390/jcm12185946
Peralta R, Sousa L, Cristovão AF. Cannulation Technique of Vascular Access in Hemodialysis and the Impact on the Arteriovenous Fistula Survival: Systematic Review and Meta-Analysis. Journal of Clinical Medicine. 2023; 12(18):5946. https://doi.org/10.3390/jcm12185946
Chicago/Turabian StylePeralta, Ricardo, Luís Sousa, and António Filipe Cristovão. 2023. "Cannulation Technique of Vascular Access in Hemodialysis and the Impact on the Arteriovenous Fistula Survival: Systematic Review and Meta-Analysis" Journal of Clinical Medicine 12, no. 18: 5946. https://doi.org/10.3390/jcm12185946