Long-Term Results with 187 Frozen Elephant Trunk Procedures
Abstract
:1. Introduction
2. Materials and Methods
2.1. Patient Population
2.2. Operative Strategy
2.3. Endpoints
2.4. Statistical Analysis
3. Results
3.1. Early Outcomes
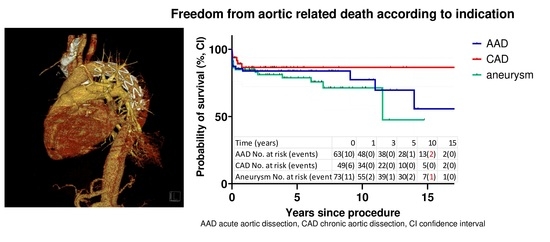
3.2. Late Mortality
3.3. Secondary Aortic Interventions
4. Discussion
5. Conclusions
6. Limitations
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Czerny, M.; Schmidli, J.; Adler, S.; van den Berg, J.C.; Bertoglio, L.; Carrel, T.; Chiesa, R.; Clough, R.E.; Eberle, B.; Etz, C.; et al. Current options and recommendations for the treatment of thoracic aortic pathologies involving the aortic arch: An expert consensus document of the European Association for Cardio-Thoracic surgery (EACTS) and the European Society for Vascular Surgery (ESVS). Eur. J. Cardiothorac. Surg. 2019, 55, 133–162. [Google Scholar] [PubMed] [Green Version]
- Czerny, M.; Rylski, B.; Kari, F.A.; Kreibich, M.; Morlock, J.; Scheumann, J.; Kondov, S.; Südkamp, M.; Siepe, M.; Beyersdorf, F. Technical details making aortic arch replacement a safe procedure using the Thoraflex Hybrid prosthesis. Eur. J. Cardiothorac. Surg. 2017, 51, i15–i19. [Google Scholar] [CrossRef] [PubMed]
- Berger, T.; Weiss, G.; Voetsch, A.; Arnold, Z.; Kreibich, M.; Rylski, B.; Krombholz-Reindl, P.; Winkler, A.; Mach, M.; Geisler, D.; et al. Multicentre experience with two frozen elephant trunk prostheses in the treatment of acute aortic dissectiondagger. Eur. J. Cardiothorac. Surg. 2019, 56, 572–578. [Google Scholar] [CrossRef]
- Leone, A.; Beckmann, E.; Martens, A.; Di Marco, L.; Pantaleo, A.; Reggiani, L.B.; Haverich, A.; Di Bartolomeo, R.; Pacini, D.; Sherestha, M. Total aortic arch replacement with frozen elephant trunk technique: Results from two European institutes. J. Thorac. Cardiovasc. Surg. 2020, 159, 1201–1211. [Google Scholar] [CrossRef]
- Di Bartolomeo, R.; Di Marco, L.; Armaro, A.; Marsilli, D.; Leone, A.; Pilato, E.; Pacini, D. Treatment of complex disease of the thoracic aorta: The frozen elephant trunk technique with the E-vita open prosthesis. Eur. J. Cardiothorac. Surg. 2009, 35, 671–675; discussion 75–76. [Google Scholar] [CrossRef] [PubMed]
- Karck, M.; Chavan, A.; Hagl, C.; Friedrich, H.; Galanski, M.; Haverich, A. The frozen elephant trunk technique: A new treatment for thoracic aortic aneurysms. J. Thorac. Cardiovasc. Surg. 2003, 125, 1550–1553. [Google Scholar] [CrossRef] [Green Version]
- Folkmann, S.; Weiss, G.; Pisarik, H.; Czerny, M.; Grabenwoger, M. Thoracoabdominal aortic aneurysm repair after frozen elephant trunk procedure. Eur. J. Cardiothorac. Surg. 2015, 47, 115–119; discussion 19. [Google Scholar] [CrossRef] [Green Version]
- Gkremoutis, A.; Zierer, A.; Schmitz-Rixen, T.; El-Sayed Ahmad, A.; Kaiser, E.; Keese, M.; Schmandra, T. Staged treatment of mega aortic syndrome using the frozen elephant trunk and hybrid thoracoabdominal repair. J. Thorac. Cardiovasc. Surg. 2017, 154, 1842–1849. [Google Scholar] [CrossRef] [Green Version]
- Haensig, M.; Schmidt, A.; Staab, H.; Steiner, S.; Scheinert, D.; Branzan, D. Endovascular repair of the thoracic or thoracoabdominal aorta following the frozen elephant trunk procedure. Ann. Thorac. Surg. 2020, 109, 695–701. [Google Scholar] [CrossRef]
- Erbel, R.; Aboyans, V.; Boileau, C.; Bossone, E.; Di Bartolomeo, R.; Eggebrecht, H.; Evangelista, A.; Falk, V.; Frank, H.; Gaemperli, O.; et al. 2014 ESC guidelines on the diagnosis and treatment of aortic diseases. Kardiol. Pol. (Pol. Heart J.) 2014, 72, 1169–1252. [Google Scholar] [CrossRef] [Green Version]
- Rylski, B.; Pacini, D.; Beyersdorf, F.; Quintana, E.; Schachner, T.; Tsagakis, K.; Ronchey, S.; Durko, A.; De Paulis, R.; Siepe, M.; et al. Standards of reporting in open and endovascular aortic surgery (STORAGE guidelines). Eur. J. Cardiothorac. Surg. 2019, 56, 10–20. [Google Scholar] [CrossRef] [PubMed]
- Gorlitzer, M.; Weiss, G.; Thalmann, M.; Mertikian, G.; Wislocki, W.; Meinhart, J.; Waldenberger, F.; Grabenwogerm, M. Combined surgical and endovascular repair of complex aortic pathologies with a new hybrid prosthesis. Ann. Thorac. Surg. 2007, 84, 1971–1976. [Google Scholar] [CrossRef] [PubMed]
- Weiss, G.; Santer, D.; Dumfarth, J.; Pisarik, H.; Harrer, M.L.; Folkmann, S.; Mach, M.; Moidl, R.; Grabenwoger, M. Evaluation of the downstream aorta after frozen elephant trunk repair for aortic dissections in terms of diameter and false lumen status. Eur. J. Cardiothorac. Surg. 2016, 49, 118–124. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Grabenwöger, M.; Alfonso, F.; Bachet, J.; Bonser, R.; Czerny, M.; Eggebrecht, H.; Evangelista, A.; Fattori, R.; Jakob, H.; Lönn, L.; et al. Thoracic Endovascular Aortic Repair (TEVAR) for the treatment of aortic diseases: A position statement from the European Association for Cardio-Thoracic Surgery (EACTS) and the European Society of Cardiology (ESC), in collaboration with the European Association of Percutaneous Cardiovascular Interventions (EAPCI). Eur. Heart J. 2012, 33, 1558–1563. [Google Scholar]
- Hickey, G.L.; Dunning, J.; Seifert, B.; Sodeck, G.; Carr, M.J.; Burger, H.U.; Beyersdorf, F. Statistical and data reporting guidelines for the European Journal of Cardio-Thoracic Surgery and the Interactive CardioVascular and Thoracic Surgery. Eur. J. Cardiothorac. Surg. 2015, 48, 180–193. [Google Scholar] [CrossRef] [Green Version]
- Shrestha, M.; Kaufeld, T.; Beckmann, E.; Fleissner, F.; Umminger, J.; Abd Alhadi, F.; Boethig, D.; Krueger, H.; Haverich, A.; Martens, A. Total aortic arch replacement with a novel 4-branched frozen elephant trunk prosthesis: Single-center results of the first 100 patients. J. Thorac. Cardiovasc. Surg. 2016, 152, 148–159.e1. [Google Scholar] [CrossRef] [Green Version]
- Jakob, H.; Dohle, D.; Benedik, J.; Janosi, R.A.; Schlosser, T.; Wendt, D.; Thielmann, M.; Erbel, R.; Tsagakis, K. Long-term experience with the E-vita Open hybrid graft in complex thoracic aortic disease. Eur. J. Cardiothorac. Surg. 2017, 51, 329–338. [Google Scholar] [CrossRef]
- Di Eusanio, M.; Pantaleo, A.; Murana, G.; Pellicciari, G.; Castrovinci, S.; Berretta, P.; Folesani, G.; Di Bartolomeo, R. Frozen elephant trunk surgery-the Bologna’s experience. Ann. Cardiothorac. Surg. 2013, 2, 597–605. [Google Scholar]
- Shi, E.; Gu, T.; Yu, Y.; Yu, L.; Wang, C.; Fang, Q.; Zhang, Y. Early and midterm outcomes of hemiarch replacement combined with stented elephant trunk in the management of acute DeBakey type I aortic dissection: Comparison with total arch replacement. J. Thorac. Cardiovasc. Surg. 2014, 148, 2125–2131. [Google Scholar] [CrossRef] [Green Version]
- Roselli, E.E.; Idrees, J.J.; Bakaeen, F.G.; Tong, M.Z.; Soltesz, E.G.; Mick, S.; Johnston, D.R.; Eagleton, M.J.; Menon, V.; Svensson, L.G. Evolution of simplified frozen elephant trunk repair for acute DeBakey type I dissection: Midterm outcomes. Ann. Thorac. Surg. 2018, 105, 749–755. [Google Scholar] [CrossRef] [Green Version]
- Chen, Q.; Cheng, F.; Chen, T.; Zhao, F.; Jiang, N. Ascending aorta replacement combined with open placement of triple-branched stent graft and total arch replacement combined with stented elephant trunk implantation for treating type A aortic dissection. Int. J. Clin. Exp. Med. 2016, 9, 16070–16077. [Google Scholar]
- Bertoglio, L.; Katsarou, M.; Loschi, D.; Rinaldi, E.; Mascia, D.; Kahlberg, A.; Lembo, R.; Melissano, G.; Chiesa, R. Elective multistaged endovascular repair of thoraco-abdominal aneurysms with fenestrated and branched endografts to mitigate spinal cord ischaemia. Eur. J. Vasc. Endovasc. Surg. 2020, 59, 565–576. [Google Scholar] [CrossRef] [PubMed]
- Kreibich, M.; Berger, T.; Rylski, B.; Chen, Z.; Beyersdorf, F.; Siepe, M.; Czerny, M. Aortic reinterventions after the frozen elephant trunk procedure. J. Thorac. Cardiovasc. Surg. 2020, 159, 392–399.e1. [Google Scholar] [CrossRef]
- Di Bartolomeo, R.; Pantaleo, A.; Berretta, P.; Murana, G.; Castrovinci, S.; Cefarelli, M.; Folesani, G.; Di Eusanio, M. Frozen elephant trunk surgery in acute aortic dissection. J. Thorac. Cardiovasc. Surg. 2015, 149, S105–S109. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Grabenwoger, M.; Mach, M.; Machler, H.; Arnold, Z.; Pisarik, H.; Folkmann, S.; Harrer, M.-L.; Geisler, D.; Moidl, R.; Winkler, B.; et al. Taking the frozen elephant trunk technique to the next level by a stented side branch for a left subclavian artery connection: A feasibility study. Eur. J. Cardiothorac. Surg. 2021, 59, 1247–1254. [Google Scholar] [CrossRef]
- Ince, H.; Rehders, T.C.; Petzsch, M.; Kische, S.; Nienaber, C.A. Stent-grafts in patients with marfan syndrome. J. Endovasc. Ther. 2005, 12, 82–88. [Google Scholar] [CrossRef]
- Ma, W.G.; Zhang, W.; Zhu, J.M.; Ziganshin, B.A.; Zhi, A.H.; Zheng, J.; Liu, Y.M.; Elefteriades, J.A.; Sun, L.-Z. Long-term outcomes of frozen elephant trunk for type A aortic dissection in patients with Marfan syndrome. J. Thorac. Cardiovasc. Surg. 2017, 154, 1175–1189.e2. [Google Scholar] [CrossRef] [Green Version]
- Pellenc, Q.; Girault, A.; Roussel, A.; De Blic, R.; Cerceau, P.; Raffoul, R.; Milleron, O.; Jondeau, G.; Castier, Y. Optimising aortic endovascular repair in patients with Marfan syndrome. Eur. J. Vasc. Endovasc. Surg. 2020, 59, 577–585. [Google Scholar] [CrossRef]
- Shrestha, M.; Martens, A.; Kaufeld, T.; Beckmann, E.; Bertele, S.; Krueger, H.; Neuser, J.; Fleissner, F.; Ius, F.; Alhadi, F.A.; et al. Single-centre experience with the frozen elephant trunk technique in 251 patients over 15 years. Eur. J. Cardiothorac. Surg. 2017, 52, 858–866. [Google Scholar] [CrossRef]
- Etz, C.D.; Zoli, S.; Mueller, C.S.; Bodian, C.A.; Di Luozzo, G.; Lazala, R.; Plestis, K.A.; Griepp, R.B. Staged repair significantly reduces paraplegia rate after extensive thoracoabdominal aortic aneurysm repair. J. Thorac. Cardiovasc. Surg. 2010, 139, 1464–1472. [Google Scholar] [CrossRef] [Green Version]
- Kremer, J.; Preisner, F.; Dib, B.; Tochtermann, U.; Ruhparwar, A.; Karck, M.; Farag, M. Aortic arch replacement with frozen elephant trunk technique—A single-center study. J. Cardiothorac. Surg. 2019, 14, 147. [Google Scholar] [CrossRef] [PubMed] [Green Version]



| All | AAD | CAD | Aneurysm | p-Value | |
|---|---|---|---|---|---|
| n = 187 (100%) | n = 64 (34.2%) | n = 49 (26.2%) | n = 74 (39.6%) | ||
| Age (years), mean ± SD | 62.1 ± 12.1 | 58.9 ± 11.8 | 56.9 ± 12.9 | 68.3 ± 8.9 | <0.001 |
| Male | 104(55.6) | 49 (76.6) | 26 (53.1) | 29 (39.2) | <0.001 |
| Diagnosis | |||||
| Aneurysm | 74 (39.6) | 0 | 0 | 74 (100) | NC |
| Acute aortic dissection | 64 (34.2) | 64 (100) | 0 | 0 | NC |
| Type A | 45 (24.1) | 45 (70.3) | 0 | 0 | NC |
| Non-A–non-B | 8 (4.3) | 8 (12.5) | 0 | 0 | NC |
| Type B | 11 (5.9) | 11 (17.2) | 0 | 0 | NC |
| Chronic aortic dissection | 49 (26.2) | 0 | 49 (100) | 0 | NC |
| Type A | 20 (10.7) | 0 | 20 (40.8) | 0 | NC |
| Non-A–non-B | 13 (7.0) | 0 | 13 (26.5) | 0 | NC |
| Type B | 16 (8.6) | 0 | 16 (32.7) | 0 | NC |
| Marfan syndrome | 8 (4.3) | 3 (4.7) | 5 (10.2) | 0 | 0.016 |
| Loeys–Dietz syndrome | 2 (1.1) | 0 | 1 (2.0) | 1 (1.4) | 0.728 |
| Turner syndrome | 1 (0.5) | 1 (1.6) | 0 | 0 | 0.604 |
| Redo operation | 31 (16.6) | 2 (3.1) | 26 (53.1) | 3 (4.1) | <0.001 |
| Previous left carotid-subclavian bypass | 48 (25.7) | 9 (14.1) | 23 (46.9) | 16 (21.6) | <0.001 |
| Previous intervention of descending aorta | 32 (17.1) | 8 (12.5) | 10 (20.4) | 14 (17.1) | 0.471 |
| Endovascular | 23 (12.3) | 8 (12.5) | 5 (10.2) | 10 (13.5) | 0.888 |
| Open | 9 (4.8) | 0 | 5 (10.2) | 4 (5.4) | 0.033 |
| Malperfusion in 113 (100%) aortic dissections | 17 (15.0) | 14 (21.9) | 3 (6.1) | 0 | 0.060 |
| Cerebral and spinal | 4 (3.5) | 4 (6.3) | 0 | 0 | NC |
| Spinal | 1 (0.9) | 1 (1.6) | 0 | 0 | NC |
| Mesenteric | 5 (4.4) | 5 (7.8) | 0 | 0 | NC |
| Renal | 1 (0.9) | 1 (1.6) | 0 | 0 | NC |
| Lower limb | 6 (5.3) | 3 (4.7) | 3 (6.1) | 0 | 1.000 |
| All | AAD | CAD | Aneurysm | p-Value | |
|---|---|---|---|---|---|
| n = 187 (100%) | n = 64 (34.2%) | n = 49 (26.2%) | n = 74 (39.6%) | ||
| Operation time (min), mean ± SD | 347 ± 66 | 370 ± 81 | 357 ± 59 | 323 ± 45 | <0.001 |
| Cardiopulmonary bypass time (min), mean ± SD | 200 ± 44 | 212 ± 55 | 212 ± 44 | 183 ± 26 | <0.001 |
| SACP time (min), mean ± SD | 58 ± 17 | 62 ± 19 | 62 ± 15 | 52 ± 14 | <0.001 |
| Visceral ischemia time (min), mean ± SD | 53 ± 17 | 62 ± 21 | 50 ± 14 | 47 ± 11 | <0.001 |
| Cardiac ischemia time (min), mean ± SD | 108 ± 31 | 113 ± 33 | 112 ± 33 | 100 ± 25 | 0.019 |
| Descending perfusion (min), mean ± SD * | 29 ± 9 | 28 ± 8 | 31 ± 10 | 28 ± 9 | 0.622 |
| Proximal stent-graft landing zone | |||||
| Zone 1 | 4 (2.1) | 0 (0) | 3 (6.1) | 1 (1.4) | 0.625 |
| Zone 2 | 76 (40.6) | 18 (28.1) | 31 (63.3) | 27 (36.5) | 0.174 |
| Zone 3 | 105 (56.1) | 45 (70.3) | 15 (30.6) | 45 (60.8) | <0.001 |
| Zone 4 | 2 (1.1) | 1 (1.6) | 0 (0) | 1 (1.4) | 1 |
| Arch replacement | |||||
| Total | 102 (54.5) | 25 (39.1) | 41 (83.7) | 36 (48.6) | 0.139 |
| Partial | 80 (42.8) | 38 (59.4) | 6 (12.2) | 36 (48.6) | <0.001 |
| None | 5 (2.7) | 1 (1.6) | 2 (4.1) | 2 (2.7) | 1 |
| Ascending aorta and aortic root interventions | |||||
| Modified Bentall–de Bono procedure | 9 (4.8) | 5 (7.8) | 2 (4.1) | 2 (2.7) | |
| Tirone David procedure | 12 (6.4) | 3 (4.7) | 4 (8.2) | 5 (6.8) | |
| AVR with supracoronary ascending replacement | 14 (7.5) | 3 (4.7) | 3 (6.1) | 8 (10.8) | |
| Ascending replacement | 146(78.1) | 52 (81.3) | 37 (75.5) | 57 (77.0) | |
| None | 6 (3.2) | 1 (1.6) | 3 (6.1) | 2 (2.7) | |
| Concomitant procedures | |||||
| CABG | 27 (14.4) | 0 (0) | 3 (6.1) | 24 (32.4) | |
| Mitral or tricuspid repair | 4 (2.1) | 0 (0) | 2 (4.1) | 2 (2.7) | |
| Maze procedure | 1 (0.5) | 0 (0) | 0 (0) | 1 (1.4) | |
| Intraoperative TEVAR | 6 (3.2) | 5 (7.8) | 0 (0) | 1 (1.4) |
| All | AAD | CAD | Aneurysm | p-Value | |
|---|---|---|---|---|---|
| n = 187 (100%) | n = 64 (34.2%) | n = 49 (26.2%) | n = 74 (39.6%) | ||
| 30 days mortality | 17 (9.1) | 8 (12.5) | 3 (6.1) | 6 (8.1) | 0.474 |
| In-hospital mortality | 24 (12.8) | 9 (14.1) | 4 (8.2) | 11 (14.9) | 0.533 |
| Prolonged ventilation (>72 h) | 49 (26.2) | 22 (34.4) | 13 (26.5) | 14 (18.9) | 0.120 |
| Stroke | 19 (10.2) | 9 (14.1) | 4 (8.2) | 6 (8.1) | 0.464 |
| Paraparesis | 5 (2.7) | 1 (1.6) | 2 (4.1) | 2 (2.7) | 0.852 |
| Dialysis | |||||
| permanent | 4 (2.1) | 1 (1.6) | 1 (2.0) | 2 (2.7) | 1 |
| temporary | 30 (16.0) | 14 (21.9) | 8 (16.3) | 8 (10.8) | 0.210 |
| Recurrent nerve palsy | 8 (4.4) | 1 (1.6) | 4 (8.2) | 3 (4.1) | 0.280 |
| Rethoracotomy for bleeding or infection | 20 (10.7) | 8 (12.5) | 5 (10.2) | 7 (9.5) | 0.840 |
| ICU stay (days), mean ± SD | 10.3 ± 18.0 | 11.4 ± 13.5 | 10.4 ± 14.5 | 9.4 ± 22.9 | 0.825 |
| Hospital stay (days) mean ± SD | 29 ± 30 | 36 ± 37 | 26 ± 21 | 26 ± 30 | 0.127 |
| Patients in follow-up | 186 (99.5) | 63 | 49 | 74 | |
| Follow-up time (years), mean ± SD | 4.2 ± 4.1 | 5.1 ± 4.6 | 3.3 ± 3.8 | 4.1 ± 3.6 | 0.066 |
| Secondary interventions | 62 (33.2) | 14 (21.9) | 19 (38.8) | 29 (39.2) | 0.061 |
| Open TAAA repair | 12 (6.4) | 0 (0) | 4 (8.2) | 8 (10.8) | 0.030 |
| TEVAR | 45 (24.1) | 10 (15.6) | 15 (30.6) | 20 (27.0) | 0.135 |
| Aortic root/arch | 5 (2.7) | 4 (6.3) | 0 (0) | 1 (1.4) | 0.074 |
| Time to first re-intervention (years), mean ± SD | 2.2 ± 3.1 | 4.8 ± 4.3 | 1.3 ± 1.6 | 1.4 ± 2.4 | <0.001 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Arnold, Z.; Geisler, D.; Aschacher, T.; Winkler, B.; Lenz, V.; Crailsheim, I.; Folkmann, S.; Harrer, M.; Moidl, R.; Grabenwöger, M.; et al. Long-Term Results with 187 Frozen Elephant Trunk Procedures. J. Clin. Med. 2023, 12, 4143. https://doi.org/10.3390/jcm12124143
Arnold Z, Geisler D, Aschacher T, Winkler B, Lenz V, Crailsheim I, Folkmann S, Harrer M, Moidl R, Grabenwöger M, et al. Long-Term Results with 187 Frozen Elephant Trunk Procedures. Journal of Clinical Medicine. 2023; 12(12):4143. https://doi.org/10.3390/jcm12124143
Chicago/Turabian StyleArnold, Zsuzsanna, Daniela Geisler, Thomas Aschacher, Bernhard Winkler, Verena Lenz, Ingo Crailsheim, Sandra Folkmann, Marieluise Harrer, Reinhard Moidl, Martin Grabenwöger, and et al. 2023. "Long-Term Results with 187 Frozen Elephant Trunk Procedures" Journal of Clinical Medicine 12, no. 12: 4143. https://doi.org/10.3390/jcm12124143