Shared Decision Making in Acute Pain Management in Patients with Opioid Use Disorder: A Scoping Review
Abstract
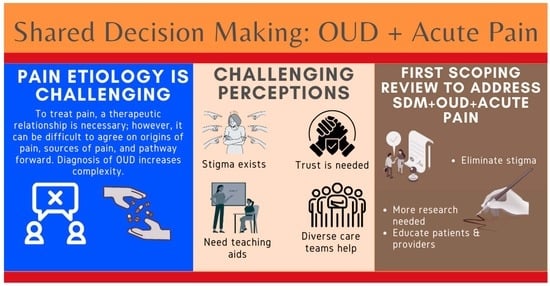
:1. Introduction
2. Materials and Methods
2.1. Design
2.2. Identification of the Research Question
2.3. Search Strategy
2.4. Eligibility Criteria
2.5. Charting the Data
3. Results
3.1. Characteristics of Included Findings
3.2. Study Findings
3.2.1. Prior Judgment and Existing Stigma Related to OUD
3.2.2. Trust and Sharing of Information
3.2.3. Clinical Tools Such as Decision Aids, Guides, and Treatment Plans
3.2.4. Interprofessional Teams
4. Discussion
4.1. Limitations
4.2. Strengths
4.3. Implications for Practice
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Anekar, A.A.; Cascella, M. WHO Analgesic Ladder; [Updated 2022 May 15]; StatsPearls: Treasure Island, FL, USA, 2022. [Google Scholar]
- McGuire, L.S.; Slavin, K. Revisiting the WHO analgesic ladder for surgical management of pain. AMA J. Ethics 2020, 22, 695–701. [Google Scholar]
- Yang, J.; Bauer, B.A.; Wahner-Roedler, D.L.; Chon, T.Y.; Xiao, L. The Modified WHO Analgesic Ladder: Is It Appropriate for Chronic Non-Cancer Pain? J. Pain Res. 2020, 13, 411–417. [Google Scholar] [CrossRef] [PubMed]
- Hyde, C.; Dunn, K.M.; Higginbottom, A.; Chew-Graham, C.A. Process and impact of patient involvement in a systematic review of shared decision making in primary care consultations. Health Expect. 2017, 20, 298–308. [Google Scholar] [CrossRef] [PubMed]
- Shinkunas, L.A.; Klipowicz, C.J.; Carlisle, E.M. Shared decision making in surgery: A scoping review of patient and surgeon preferences. BMC Med. Inform. Decis. Mak. 2020, 20, 190. [Google Scholar] [CrossRef]
- Poprzeczny, A.J.; Stocking, K.; Showell, M.; Duffy, J.M.N. Patient Decision Aids to Facilitate Shared Decision Making in Obstetrics and Gynecology: A Systematic Review and Meta-analysis. Obstet. Gynecol. 2020, 135, 444–451. [Google Scholar] [CrossRef]
- Samalin, L.; Genty, J.B.; Boyer, L.; Lopez-Castroman, J.; Abbar, M.; Llorca, P.M. Shared Decision-Making: A Systematic Review Focusing on Mood Disorders. Curr. Psychiatry Rep. 2018, 20, 23. [Google Scholar] [CrossRef]
- O’Connor, A.M.; Rostom, A.; Fiset, V.; Tetroe, J.; Entwistle, V.; Llewellyn-Thomas, H.; Holmes-Rovner, M.; Barry, M.; Jones, J. Decision aids for patients facing health treatment or screening decisions: Systematic review. BMJ 1999, 319, 731–734. [Google Scholar] [CrossRef]
- Milky, G.; Thomas, J. Shared decision making, satisfaction with care and medication adherence among patients with diabetes. Patient Educ. Couns. 2020, 103, 661–669. [Google Scholar] [CrossRef]
- Tousignant-Laflamme, Y.; Christopher, S.; Clewley, D.; Ledbetter, L.; Cook, C.J.; Cook, C.E. Does shared decision making results in better health related outcomes for individuals with painful musculoskeletal disorders? A systematic review. J. Man Manip. Ther. 2017, 25, 144–150. [Google Scholar] [CrossRef]
- Brant, J.M.; Wujcik, D.; Dudley, W.N.; Petok, A.; Worster, B.; Jones, D.; Bosket, K.; Brady, C.; Stricker, C.T. Shared Decision-Making in Managing Breakthrough Cancer Pain in Patients with Advanced Cancer. J. Adv. Pract. Oncol. 2022, 13, 19–29. [Google Scholar] [CrossRef]
- Kuosmanen, L.; Hupli, M.; Ahtiluoto, S.; Haavisto, E. Patient participation in shared decision-making in palliative care—An integrative review. J. Clin. Nurs. 2021, 30, 3415–3428. [Google Scholar] [CrossRef] [PubMed]
- Holland, W.C.; Hunold, K.M.; Mangipudi, S.A.; Rittenberg, A.M.; Yosipovitch, N.; Platts-Mills, T.F. A Prospective Evaluation of Shared Decision-making Regarding Analgesics Selection for Older Emergency Department Patients with Acute Musculoskeletal Pain. Acad. Emerg. Med. 2016, 23, 306–314. [Google Scholar] [CrossRef] [PubMed]
- Sanders, A.R.J.; de Wit, N.J.; Zuithoff, N.P.A.; van Dulmen, S. The effect of shared decision-making on recovery from non-chronic aspecific low back pain in primary care; a post-hoc analysis from the patient, physician and observer perspectives. BMC Prim. Care 2022, 23, 22. [Google Scholar] [CrossRef] [PubMed]
- Jairam, V.; Yang, D.X.; Pasha, S.; Soulos, P.R.; Gross, C.P.; Yu, J.B.; Park, H.S. Temporal Trends in Opioid Prescribing Patterns among Oncologists in the Medicare Population. J. Natl. Cancer Inst. 2021, 113, 274–281. [Google Scholar] [CrossRef]
- Penney, L.S.; Ritenbaugh, C.; DeBar, L.L.; Elder, C.; Deyo, R.A. Provider and patient perspectives on opioids and alternative treatments for managing chronic pain: A qualitative study. BMC Fam. Pract. 2017, 17, 164. [Google Scholar] [CrossRef]
- Blanco, C.; Volkow, N.D. Management of opioid use disorder in the USA: Present status and future directions. Lancet 2019, 393, 1760–1772. [Google Scholar] [CrossRef]
- Alford, D.P.; Compton, P.; Samet, J.H. Acute pain management for patients receiving maintenance methadone or buprenorphine therapy. Ann. Intern. Med. 2006, 144, 127–134. [Google Scholar] [CrossRef]
- Algera, M.H.; Olofsen, E.; Moss, L.; Dobbins, R.L.; Niesters, M.; van Velzen, M.; Groeneveld, G.J.; Heuberger, J.; Laffont, C.M.; Dahan, A. Tolerance to Opioid-Induced Respiratory Depression in Chronic High-Dose Opioid Users: A Model-Based Comparison with Opioid-Naïve Individuals. Clin. Pharmacol. Ther. 2021, 109, 637–645. [Google Scholar] [CrossRef]
- Krashin, D.; Murinova, N.; Ballantyne, J. Management of pain with comorbid substance abuse. Curr. Psychiatry Rep. 2012, 14, 462–468. [Google Scholar] [CrossRef]
- Tricco, A.C.; Lillie, E.; Zarin, W.; O’Brien, K.K.; Colquhoun, H.; Levac, D.; Moher, D.; Peters, M.D.J.; Horsley, T.; Weeks, L.; et al. PRISMA Extension for Scoping Reviews (PRISMA-ScR): Checklist and Explanation. Ann. Intern. Med. 2018, 169, 467–473. [Google Scholar] [CrossRef]
- Charles, C.; Gafni, A.; Whelan, T. Shared decision-making in the medical encounter: What does it mean? (or it takes at least two to tango). Soc. Sci. Med. 1997, 44, 681–692. [Google Scholar] [CrossRef] [PubMed]
- Broughton-Miller, K.D.; Urquhart, G.E. Improving acute pain management of trauma patients on medication-assisted therapy. J. Am. Assoc. Nurse Pract. 2022, 34, 924–931. [Google Scholar] [CrossRef]
- Buresh, M.; Ratner, J.; Zgierska, A.; Gordin, V.; Alvanzo, A. Treating Perioperative and Acute Pain in Patients on Buprenorphine: Narrative Literature Review and Practice Recommendations. J. Gen. Intern. Med. 2020, 35, 3635–3643. [Google Scholar] [CrossRef] [PubMed]
- Butt, S.; McClean, M.; Turner, J.; Roth, S.; Rollins, A.L. Health care workers’ perspectives on care for patients with injection drug use associated infective endocarditis (IDU-IE). BMC Health Serv. Res. 2022, 22, 719. [Google Scholar] [CrossRef] [PubMed]
- Hickey, T.; Abelleira, A.; Acampora, G.; Becker, W.C.; Falker, C.G.; Nazario, M.; Weimer, M.B. Perioperative Buprenorphine Management: A Multidisciplinary Approach. Med. Clin. N. Am. 2022, 106, 169–185. [Google Scholar] [CrossRef] [PubMed]
- Kurtz, D.R. Managing acute pain in admitted or suspected substance abusers. Physician Assist. (1983) 2003, 27, 36. [Google Scholar]
- Mefford, B.; Donaldson, J.C. Managing Acute Pain in Opioid Use Disorder. U.S. Pharm. 2022, 42, HS2–HS6. [Google Scholar]
- Mitchell, L.M.; Milliken, A.; Montgomery, M.W.; Singh, S.K.; Suzuki, J. The Opioid Crisis and the Inpatient Floor: Considering Injection Drug Use in the Management of Infective Endocarditis and Acute Pain. Harv. Rev. Psychiatry 2020, 28, 334–340. [Google Scholar] [CrossRef]
- Smith, K.; Wang, M.; Abdukalikov, R.; McAullife, A.; Whitesell, D.; Richard, J.; Sauer, W.; Quaye, A. Pain Management Considerations in Patients with Opioid Use Disorder Requiring Critical Care. J. Clin. Pharmacol. 2022, 62, 449–462. [Google Scholar] [CrossRef]
- Stumbo, S.P.; Yarborough, B.J.; McCarty, D.; Weisner, C.; Green, C.A. Patient-reported pathways to opioid use disorders and pain-related barriers to treatment engagement. J. Subst. Abus. Treat. 2017, 73, 47–54. [Google Scholar] [CrossRef]
- The SHARE Approach. Content Last Reviewed October 2020. Available online: https://www.ahrq.gov/health-literacy/professional-training/shared-decision/index.html (accessed on 15 February 2023).
- Tofighi, B.; Williams, A.R.; Chemi, C.; Suhail-Sindhu, S.; Dickson, V.; Lee, J.D. Patient Barriers and Facilitators to Medications for Opioid Use Disorder in Primary Care. Subst. Use Misuse 2019, 54, 2409–2419. [Google Scholar] [CrossRef] [PubMed]
- Crowley, D.; Homeniuk, R.; Delargy, I. Scoping review protocol: The use of telemedicine in providing opioid agonist treatment and related psychosocial supports. BMJ Open 2020, 10, e040556. [Google Scholar] [CrossRef] [PubMed]
- Schiff, D.M.; Work, E.C.; Muftu, S.; Partridge, S.; MacMillan, K.D.L.; Gray, J.R.; Hoeppner, B.B.; Kelly, J.F.; Greenfield, S.F.; Jones, H.E.; et al. You have to take this medication, but then you get punished for taking it: Lack of agency, choice, and fear of medications to treat opioid use disorder across the perinatal period. J. Subst. Abus. Treat. 2022, 139, 108765. [Google Scholar] [CrossRef] [PubMed]
- Proulx, D.; Fantasia, H.C. The Lived Experience of Postpartum Women Attending Outpatient Substance Treatment for Opioid or Heroin Use. J. Midwifery Womens Health 2021, 66, 211–217. [Google Scholar] [CrossRef]
- Pergolizzi, J.V.; Magnusson, P.; Christo, P.J.; LeQuang, J.A.; Breve, F.; Mitchell, K.; Varrassi, G. Opioid Therapy in Cancer Patients and Survivors at Risk of Addiction, Misuse or Complex Dependency. Front. Pain Res. 2021, 2, 691720. [Google Scholar] [CrossRef]
- Korpaisarn, S.; Safer, J.D. Gaps in transgender medical education among healthcare providers: A major barrier to care for transgender persons. Rev. Endocr. Metab. Disord. 2018, 19, 271–275. [Google Scholar] [CrossRef]
- Safer, J.D.; Coleman, E.; Feldman, J.; Garofalo, R.; Hembree, W.; Radix, A.; Sevelius, J. Barriers to healthcare for transgender individuals. Curr. Opin. Endocrinol. Diabetes Obes. 2016, 23, 168–171. [Google Scholar] [CrossRef]
- Ritter, S.; Stirnemann, J.; Breckwoldt, J.; Stocker, H.; Fischler, M.; Mauler, S.; Fuhrer-Soulier, V.; Meier, C.A.; Nendaz, M. Shared Decision-Making Training in Internal Medicine: A Multisite Intervention Study. J. Grad. Med. Educ. 2019, 11, 146–151. [Google Scholar] [CrossRef]
- Bakos-Block, C.; Nash, A.J.; Cohen, A.S.; Champagne-Langabeer, T. Experiences of Parents with Opioid Use Disorder during Their Attempts to Seek Treatment: A Qualitative Analysis. Int. J. Environ. Res. Public Health 2022, 19, 16660. [Google Scholar] [CrossRef]
- Coronado-Vázquez, V.; Canet-Fajas, C.; Delgado-Marroquín, M.T.; Magallón-Botaya, R.; Romero-Martín, M.; Gómez-Salgado, J. Interventions to facilitate shared decision-making using decision aids with patients in Primary Health Care: A systematic review. Medicine 2020, 99, e21389. [Google Scholar] [CrossRef]
- Aarts, J.W.M.; Thompson, R.; Alam, S.S.; Dannenberg, M.; Elwyn, G.; Foster, T.C. Encounter decision aids to facilitate shared decision-making with women experiencing heavy menstrual bleeding or symptomatic uterine fibroids: A before-after study. Patient Educ. Couns. 2021, 104, 2259–2265. [Google Scholar] [CrossRef] [PubMed]
- Niburski, K.; Guadagno, E.; Abbasgholizadeh-Rahimi, S.; Poenaru, D. Shared Decision Making in Surgery: A Meta-Analysis of Existing Literature. Patient 2020, 13, 667–681. [Google Scholar] [CrossRef]
- Guille, C.; Jones, H.E.; Abuhamad, A.; Brady, K.T. Shared Decision-Making Tool for Treatment of Perinatal Opioid Use Disorder. Psychiatr. Res. Clin. Pract. 2019, 1, 27–31. [Google Scholar] [CrossRef]
- Mooney, L.J.; Valdez, J.; Cousins, S.J.; Yoo, C.; Zhu, Y.; Hser, Y.I. Patient decision aid for medication treatment for opioid use disorder (PtDA-MOUD): Rationale, methodology, and preliminary results. J. Subst. Abus. Treat. 2020, 108, 115–122. [Google Scholar] [CrossRef] [PubMed]
- Bakos-Block, C.R.; Al Rawwad, T.; Cardenas-Turanzas, M.; Champagne-Langabeer, T. Contact based intervention reduces stigma among pharmacy students. Curr. Pharm. Teach. Learn. 2022, 14, 1471–1477. [Google Scholar] [CrossRef]
- Quinn, T.D.; Wolczynski, P.; Sroka, R.; Urman, R.D. Creating a Pathway for Multidisciplinary Shared Decision-Making to Improve Communication during Preoperative Assessment. Anesthesiol. Clin. 2018, 36, 653–662. [Google Scholar] [CrossRef] [PubMed]
- Nanapragasam, A.; Lim, C.K.; Maskell, G. Patient involvement and shared decision-making in the management of back pain: A proposed multidisciplinary team model. Clin. Radiol. 2019, 74, 76–77. [Google Scholar] [CrossRef]
- Jones, C.M.; Noonan, R.K.; Compton, W.M. Prevalence and correlates of ever having a substance use problem and substance use recovery status among adults in the United States, 2018. Drug Alcohol Depend. 2020, 214, 108169. [Google Scholar] [CrossRef]
- Kerensky, T.; Walley, A.Y. Opioid overdose prevention and naloxone rescue kits: What we know and what we don’t know. Addict. Sci. Clin. Pract. 2017, 12, 4. [Google Scholar] [CrossRef]

| Study | Type of Article | Patient Population | Outcomes and Findings | Subtopic |
|---|---|---|---|---|
| Broughton-Miller and Urquhart, 2022 [23] | Original Research | Inpatient trauma patients with OUD and on MOUD | Modified Ottawa Personal Decision tool led to high levels of patient engagement Improved pain outcomes with four-pronged intervention: risk assessment, provider checklist, and healthcare team engagement | CT, MT |
| Buresh et al., 2020 [24] | Review | Men and women on buprenorphine undergoing surgery | Continue buprenorphine and use a multimodal pain management approach Close communication with the patient’s outpatient MOUD provider General mention of shared decision making and individualized care but no detailed recommendations | TS, MT |
| Butt, et al., 2022 [25] | Original research | IV drug use and infective endocarditis | Healthcare workers’ stigma led to barriers in care Need for improved communication SDM needs to also include post-hospital substance use treatment | JM |
| Hickey et al., 2022 [26] | Review of clinical guidelines | OUD patients on buprenorphine undergoing surgery | Multidisciplinary approach Mention of patient-centered care but no mention of shared decision making between patient and provider | MT |
| Krashin et al., 2012 [20] | Review | Acute and chronic pain patients with a history of SUD | Frank and open discussions regarding pain management and planning Patient education and treatment agreements Universal risk assessment Motivational interviewing for patients active in SUD | TS, CT |
| Kurtz, 2003 [27] | Review of clinical guidelines | Acute pain patients with a history of SUD | Improve patient education and empowerment Active discussion of available therapies Coordination of treatment goals between patients and providers | TS, MT |
| Mefford and Donaldson, 2022 [28] | Review of clinical guidelines | OUD patients on MOUD with acute pain | Barrier: Provider perceptions of OUD patients Barrier: Provider lack of knowledge on MOUD Mention of including patient preferences in the management of MOUD and pain | JM, TS |
| Mitchell et al., 2020 [29] | Original research | Endocarditis associated with IV drug use | Involve addiction specialists Nursing education Tools to identify aberrant behavior may be useful Acute pain an opportunity for SDM in recovery engagement | TS, CT, MT |
| Smith et al., 2022 [30] | Review | ICU/perioperative OUD patients | Pain scales and monitoring for withdrawal symptoms Multidisciplinary team and discharge planning | TS, CT, MT |
| Stumbo et al., 2017 [31] | Original research | Pathways to OUD and pain barriers | Prescription of opioids may result in recurrence even after years of abstinence Patients with previous substance use may not disclose their history | JM, TS |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Vu, P.D.; Malik, A.; Cohen, A.S.; Bansal, V.; Cowan, M.R.; Blazek, G.M.; Champagne-Langabeer, T. Shared Decision Making in Acute Pain Management in Patients with Opioid Use Disorder: A Scoping Review. J. Clin. Med. 2023, 12, 3555. https://doi.org/10.3390/jcm12103555
Vu PD, Malik A, Cohen AS, Bansal V, Cowan MR, Blazek GM, Champagne-Langabeer T. Shared Decision Making in Acute Pain Management in Patients with Opioid Use Disorder: A Scoping Review. Journal of Clinical Medicine. 2023; 12(10):3555. https://doi.org/10.3390/jcm12103555
Chicago/Turabian StyleVu, Peter D., Aila Malik, A. Sarah Cohen, Vishal Bansal, Morgan R. Cowan, Gregory M. Blazek, and Tiffany Champagne-Langabeer. 2023. "Shared Decision Making in Acute Pain Management in Patients with Opioid Use Disorder: A Scoping Review" Journal of Clinical Medicine 12, no. 10: 3555. https://doi.org/10.3390/jcm12103555