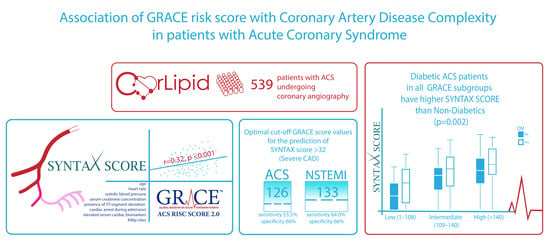
Association of GRACE Risk Score with Coronary Artery Disease Complexity in Patients with Acute Coronary Syndrome
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Study Population
2.3. Coronary Angiography and Scores Calculation
2.4. Statistical Analysis
3. Results
3.1. Population Characteristics
3.2. Correlation between the GRACE Score and Coronary Artery Disease Complexity
3.3. Additional Clinical Predictors of Severe Coronary Artery Disease
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Townsend, N.; Wilson, L.; Bhatnagar, P.; Wickramasinghe, K.; Rayner, M.; Nichols, M. Cardiovascular disease in Europe: Epidemiological update 2016. Eur. Heart J. 2016, 37, 3232–3245. [Google Scholar] [CrossRef] [PubMed]
- Roth, G.A.; Johnson, C.; Abajobir, A.; Abd-Allah, F.; Abera, S.F.; Abyu, G.; Ahmed, M.; Aksut, B.; Alam, T.; Alam, K.; et al. Global, Regional, and National Burden of Cardiovascular Diseases for 10 Causes, 1990 to 2015. J. Am. Coll. Cardiol. 2017, 70, 1–25. [Google Scholar] [CrossRef] [PubMed]
- Yan, A.T.; Yan, R.T.; Tan, M.; Casanova, A.; Labinaz, M.; Sridhar, K.; Fitchett, D.H.; Langer, A.; Goodman, S.G. Risk scores for risk stratification in acute coronary syndromes: Useful but simpler is not necessarily better. Eur. Heart J. 2007, 28, 1072–1078. [Google Scholar] [CrossRef] [PubMed]
- Chan Pin Yin, D.; Azzahhafi, J.; James, S. Risk Assessment Using Risk Scores in Patients with Acute Coronary Syndrome. J. Clin. Med. 2020, 9, 3039. [Google Scholar] [CrossRef] [PubMed]
- Report of the Expert Committee on the Diagnosis and Classification of Diabetes Mellitus. Diabetes Care 1997, 20, 1183–1197. [CrossRef]
- Ibanez, B.; James, S.; Agewall, S.; Antunes, M.J.; Bucciarelli-Ducci, C.; Bueno, H.; Caforio, A.L.P.; Crea, F.; Goudevenos, J.A.; Halvorsen, S.; et al. 2017 ESC Guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation. Eur. Heart J. 2018, 39, 119–177. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- O’Gara, P.T.; Kushner, F.G.; Ascheim, D.D.; Casey, D.E.J.; Chung, M.K.; de Lemos, J.A.; Ettinger, S.M.; Fang, J.C.; Fesmire, F.M.; Franklin, B.A.; et al. 2013 ACCF/AHA guideline for the management of ST-elevation myocardial infarction: A report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. Circulation 2013, 127, e362–e425. [Google Scholar] [CrossRef] [Green Version]
- Collet, J.-P.; Thiele, H.; Barbato, E.; Barthélémy, O.; Bauersachs, J.; Bhatt, D.L.; Dendale, P.; Dorobantu, M.; Edvardsen, T.; Folliguet, T.; et al. 2020 ESC Guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation. Eur. Heart J. 2021, 42, 1289–1367. [Google Scholar] [CrossRef]
- Sianos, G.; Morel, M.-A.; Kappetein, A.P.; Morice, M.-C.; Colombo, A.; Dawkins, K.; van den Brand, M.; Van Dyck, N.; Russell, M.E.; Mohr, F.W.; et al. The SYNTAX Score: An angiographic tool grading the complexity of coronary artery disease. EuroIntervention J. Eur. Collab. with Work. Gr. Interv. Cardiol. Eur. Soc. Cardiol. 2005, 1, 219–227. [Google Scholar]
- Serruys, P.W.; Morice, M.-C.; Kappetein, A.P.; Colombo, A.; Holmes, D.R.; Mack, M.J.; Ståhle, E.; Feldman, T.E.; van den Brand, M.; Bass, E.J.; et al. Percutaneous coronary intervention versus coronary-artery bypass grafting for severe coronary artery disease. N. Engl. J. Med. 2009, 360, 961–972. [Google Scholar] [CrossRef]
- Garcia, S.; Canoniero, M.; Peter, A.; de Marchena, E.; Ferreira, A. Correlation of TIMI risk score with angiographic severity and extent of coronary artery disease in patients with non-ST-elevation acute coronary syndromes. Am. J. Cardiol. 2004, 93, 813–816. [Google Scholar] [CrossRef] [PubMed]
- Cakar, M.A.; Sahinkus, S.; Aydin, E.; Vatan, M.B.; Keser, N.; Akdemir, R.; Gunduz, H. Relation between the GRACE score and severity of atherosclerosis in acute coronary syndrome. J. Cardiol. 2014, 63, 24–28. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bekler, A.; Altun, B.; Gazi, E.; Temiz, A.; Barutçu, A.; Güngör, Ö.; Özkan, M.T.A.; Özcan, S.; Gazi, S.; Kırılmaz, B. Comparison of the GRACE risk score and the TIMI risk index in predicting the extent and severity of coronary artery disease in patients with acute coronary syndrome. Anatol. J. Cardiol. 2015, 15, 801–806. [Google Scholar] [CrossRef]
- Wiviott, S.D.; Morrow, D.A.; Frederick, P.D.; Antman, E.M.; Braunwald, E. Application of the Thrombolysis in Myocardial Infarction risk index in non-ST-segment elevation myocardial infarction: Evaluation of patients in the National Registry of Myocardial Infarction. J. Am. Coll. Cardiol. 2006, 47, 1553–1558. [Google Scholar] [CrossRef] [Green Version]
- Isilak, Z.; Kardesoglu, E.; Aparci, M.; Uz, O.; Yalcin, M.; Yiginer, O.; Cingozbay, B.Y.; Uzun, M. Comparison of clinical risk assessment systems in predicting three-vessel coronary artery disease and angiographic culprit lesion in patients with non-ST segment elevated myocardial infarction/unstable angina pectoris. Kardiol. Pol. 2012, 70, 242–250. [Google Scholar]
- Hammami, R.; Jdidi, J.; Mroua, F.; Kallel, R.; Hentati, M.; Abid, L.; Kammoun, S. Accuracy of the TIMI and GRACE scores in predicting coronary disease in patients with non-ST-elevation acute coronary syndrome. Rev. Port. Cardiol. Orgao Of. Soc. Port. Cardiol. Port. J. Cardiol. Off. J. Port. Soc. Cardiol. 2018, 37, 41–49. [Google Scholar] [CrossRef]
- Beigel, R.; Matetzky, S.; Gavrielov-Yusim, N.; Fefer, P.; Gottlieb, S.; Zahger, D.; Atar, S.; Finkelstein, A.; Roguin, A.; Goldenberg, I.; et al. Predictors of high-risk angiographic findings in patients with non-ST-segment elevation acute coronary syndrome. Catheter. Cardiovasc. Interv. 2014, 83, 677–683. [Google Scholar] [CrossRef]
- Avci, B.K.; Ikitimur, B.; Tok, O.O.; Cimci, M.; Erturk, E.; Omar, T.B.; Babayev, I.; Karadag, B.; Ongen, Z. The role of GRACE score in the prediction of high-risk coronary anatomy in patients with non-ST elevation acute coronary syndrome. Kardiol. Pol. 2015, 73, 592–597. [Google Scholar] [CrossRef]
- Rahmani, R.; Majidi, B.; Ariannejad, H.; Shafiee, A. The Value of the GRACE Score for Predicting the SYNTAX Score in Patients with Unstable Angina/Non-ST Elevation Myocardial Infarction. Cardiovasc. Revascularization Med. 2020, 21, 514–517. [Google Scholar] [CrossRef]
- Chotechuang, Y.; Phrommintikul, A.; Kuanprasert, S.; Muenpa, R.; Ruengorn, C.; Patumanond, J.; Chaichuen, T.; Thanachaikun, N.; Benjanuwatra, T.; Sukonthasarn, A. GRACE score and cardiovascular outcomes prediction among the delayed coronary intervention after post-fibrinolytic STEMI patients in a limited PCI-capable hospital. Open Heart 2020, 7, e001133. [Google Scholar] [CrossRef] [Green Version]
- Karagiannidis, E.; Sofidis, G.; Papazoglou, A.S.; Deda, O.; Panteris, E.; Moysidis, D.V.; Stalikas, N.; Kartas, A.; Papadopoulos, A.; Stefanopoulos, L.; et al. Correlation of the severity of coronary artery disease with patients’ metabolic profile- rationale, design and baseline patient characteristics of the CorLipid trial. BMC Cardiovasc. Disord. 2021, 21, 79. [Google Scholar] [CrossRef] [PubMed]
- Thygesen, K.; Alpert, J.S.; Jaffe, A.S.; Chaitman, B.R.; Bax, J.J.; Morrow, D.A.; White, H.D. Fourth universal definition of myocardial infarction (2018). Eur. Heart J. 2019, 40, 237–269. [Google Scholar] [CrossRef] [Green Version]
- World Medical Association declaration of Helsinki: Ethical principles for medical research involving human subjects. JAMA J. Am. Med. Assoc. 2013, 310, 2191–2194. [CrossRef] [PubMed] [Green Version]
- Fox, K.A.A.; FitzGerald, G.; Puymirat, E.; Huang, W.; Carruthers, K.; Simon, T.; Coste, P.; Monsegu, J.; Steg, P.G.; Danchin, N.; et al. Should patients with acute coronary disease be stratified for management according to their risk? Derivation, external validation and outcomes using the updated GRACE risk score. BMJ Open 2014, 4, 1–10. [Google Scholar] [CrossRef]
- Garg, S.; Sarno, G.; Serruys, P.W.; Rodriguez, A.E.; Bolognese, L.; Anselmi, M.; De Cesare, N.; Colangelo, S.; Moreno, R.; Gambetti, S.; et al. Prediction of 1-year clinical outcomes using the SYNTAX score in patients with acute ST-segment elevation myocardial infarction undergoing primary percutaneous coronary intervention: A substudy of the STRATEGY (Single High-Dose Bolus Tirofiban and Siroli. JACC. Cardiovasc. Interv. 2011, 4, 66–75. [Google Scholar] [CrossRef] [Green Version]
- Serruys, P.W.; Onuma, Y.; Garg, S.; Sarno, G.; van den Brand, M.; Kappetein, A.-P.; Van Dyck, N.; Mack, M.; Holmes, D.; Feldman, T.; et al. Assessment of the SYNTAX score in the Syntax study. EuroInterv. J. Eur. Collab. Work. Gr. Interv. Cardiol. Eur. Soc. Cardiol. 2009, 5, 50–56. [Google Scholar] [CrossRef]
- Popovic, Z.B.; Thomas, J.D. Assessing observer variability: A user’s guide. Cardiovasc. Diagn. Ther. 2017, 7, 317–324. [Google Scholar] [CrossRef] [Green Version]
- McHugh, M.L. Interrater reliability: The kappa statistic. Biochem. Med. 2012, 22, 276–282. [Google Scholar] [CrossRef]
- Akyuz, S.; Yazici, S.; Bozbeyoglu, E.; Onuk, T.; Yildirimturk, O.; Karacimen, D.; Hayiroglu, M.I.; Erdogan, G.; Oner, A.O.; Calik, A.N.; et al. Validity of the updated GRACE risk predictor (version 2.0) in patients with non-ST-elevation acute coronary syndrome. Rev. Port. Cardiol. 2016, 35, 25–31. [Google Scholar] [CrossRef]
- Chotechuang, Y.; Phrommintikul, A.; Muenpa, R.; Patumanond, J.; Chaichuen, T.; Kuanprasert, S.; Thanachikun, N.; Benjanuwatra, T.; Sukonthasarn, A. The prognostic utility of GRACE risk score in predictive cardiovascular event rate in STEMI patients with successful fibrinolysis and delay intervention in non PCI-capable hospital: A retrospective cohort study. BMC Cardiovasc. Disord. 2016, 16, 1–10. [Google Scholar] [CrossRef] [Green Version]
- Shuvy, M.; Beeri, G.; Klein, E.; Cohen, T.; Shlomo, N.; Minha, S.; Pereg, D. Accuracy of the Global Registry of Acute Coronary Events (GRACE) Risk Score in Contemporary Treatment of Patients With Acute Coronary Syndrome. Can. J. Cardiol. 2018, 34, 1613–1617. [Google Scholar] [CrossRef]
- Viana, M.S.; Correia, V.C.A.; Ferreira, F.M.; Lacerda, Y.F.; Bagano, G.O.; Fonseca, L.L.; Kertzman, L.Q.; Melo, M.V.; Noya-Rabelo, M.M.; Correia, L.C.L. Prognostic contrast between anatomical and clinical models regarding fatal and non-fatal outcomes in acute coronary syndromes. Arq. Bras. Cardiol. 2020, 115, 219–225. [Google Scholar] [CrossRef] [PubMed]
- Viana, M.D.S.; Lopes, F.; Cerqueira Junior, A.M.D.S.; Suerdieck, J.G.; Silva, A.B.D.; Silva, A.C.B.D.; Souza, T.M.B.D.; Carvalhal, M.C.; Rabelo, M.M.N.; Correia, L.C.L. Incremental prognostic value of the incorporation of clinical data Into coronary anatomy data in acute coronary syndromes: SYNTAX-GRACE score. Arq. Bras. Cardiol. 2017, 109, 527–532. [Google Scholar] [CrossRef] [PubMed]
- Takahashi, K.; Serruys, P.W.; Fuster, V.; Farkouh, M.E.; Spertus, J.A.; Cohen, D.J.; Park, S.J.; Park, D.W.; Ahn, J.M.; Kappetein, A.P.; et al. Redevelopment and validation of the SYNTAX score II to individualise decision making between percutaneous and surgical revascularisation in patients with complex coronary artery disease: Secondary analysis of the multicentre randomised controlled SYNTAXES. Lancet 2020, 396, 1399–1412. [Google Scholar] [CrossRef]
- Kang, J.; Zheng, C.; Park, K.W.; Park, J.; Rhee, T.; Lee, H.S.; Han, J.-K.; Yang, H.-M.; Kang, H.-J.; Koo, B.-K.; et al. Complete Revascularization of Multivessel Coronary Artery Disease Does Not Improve Clinical Outcome in ST-Segment Elevation Myocardial Infarction Patients with Reduced Left Ventricular Ejection Fraction. J. Clin. Med. 2020, 9, 232. [Google Scholar] [CrossRef] [Green Version]
- Aktürk, E.; Aşkln, L.; Taşolar, H.; Türkmen, S.; Kaya, H. Comparison of the predictive roles of risk scores of in-hospital major adverse cardiovascular events in patients with Non-ST elevation myocardial infarction undergoing percutaneous coronary intervention. Med. Princ. Pract. 2018, 27, 459–465. [Google Scholar] [CrossRef]
- Barbosa, C.E.; Viana, M.; Brito, M.; Sabino, M.; Garcia, G.; Maraux, M.; Souza, A.C.; Noya-Rabelo, M.; Esteves, J.P.; Correia, L.C.L. Accuracy of the GRACE and TIMI scores in predicting the angiographic severity of acute coronary syndrome. Arq. Bras. Cardiol. 2012, 99, 818–824. [Google Scholar] [CrossRef] [Green Version]
- dos Santos, E.S.; Filho, L.d.F.A.; Fonseca, D.M.; Londero, H.J.; Xavier, R.M.; Pereira, M.P.; Minuzzo, L.; de Souza, R.; Timerman, A. Correlação dos escores de risco com a anatomia coronária na síndrome coronária aguda sem supra-ST. Arq. Bras. Cardiol. 2013, 100, 511–517. [Google Scholar] [CrossRef]
- Saha, T.; Khalequzzaman, M.; Akanda, M.A.K.; Saha, S.; Tushar, A.Z.; Ahmed, R.; Saha, G.K.; Ullah, M. Association of GRACE Risk Score with Angiographic Severity of Coronary Artery Disease in patients with ST Elevation Myocardial Infarction. Cardiovasc. J. 2015, 8, 30–34. [Google Scholar] [CrossRef] [Green Version]
- Taşolar, H.; Çetin, M.; Ballı, M.; Bayramoğlu, A.; Otlu, Y.Ö.; Türkmen, S.; Aktürk, E. CHA2DS2-VASc-HS score in non-ST elevation acute coronary syndrome patients: Assessment of coronary artery disease severity and complexity and comparison to other scoring systems in the prediction of in-hospital major adverse cardiovascular events. Anatol. J. Cardiol. 2016, 16, 742–748. [Google Scholar] [CrossRef]
- Tanaka, T.; Miki, K.; Akahori, H.; Imanaka, T.; Yoshihara, N.; Kimura, T.; Yanaka, K.; Asakura, M.; Ishihara, M. Comparison of coronary atherosclerotic disease burden between ST-elevation myocardial infarction and non-ST-elevation myocardial infarction: Non-culprit Gensini score and non-culprit SYNTAX score. Clin. Cardiol. 2020. [Google Scholar] [CrossRef]
- Karagiannidis, E.; Papazoglou, A.S.; Sofidis, G.; Chatzinikolaou, E.; Keklikoglou, K.; Panteris, E.; Kartas, A.; Stalikas, N.; Zegkos, T.; Girtovitis, F.; et al. Micro-CT-Based Quantification of Extracted Thrombus Burden Characteristics and Association With Angiographic Outcomes in Patients With ST-Elevation Myocardial Infarction: The QUEST-STEMI Study. Front. Cardiovasc. Med. 2021, 8, 168. [Google Scholar] [CrossRef]
- Zhou, M.; Liu, J.; Hao, Y.; Liu, J.; Huo, Y.; Smith, S.C.; Ge, J.; Ma, C.; Han, Y.; Fonarow, G.C.; et al. Prevalence and in-hospital outcomes of diabetes among patients with acute coronary syndrome in China: Findings from the Improving Care for Cardiovascular Disease in China-Acute Coronary Syndrome Project. Cardiovasc. Diabetol. 2018, 17, 147. [Google Scholar] [CrossRef] [Green Version]
- Esper, R.B.; Farkouh, M.E.; Ribeiro, E.E.; Hueb, W.; Domanski, M.; Hamza, T.H.; Siami, F.S.; Godoy, L.C.; Mathew, V.; French, J.; et al. SYNTAX Score in Patients With Diabetes Undergoing Coronary Revascularization in the FREEDOM Trial. J. Am. Coll. Cardiol. 2018, 72, 2826–2837. [Google Scholar] [CrossRef] [PubMed]
- Colaiori, I.; Izzo, R.; Barbato, E.; Franco, D.; Di Gioia, G.; Rapacciuolo, A.; Bartunek, J.; Mancusi, C.; Losi, M.A.; Strisciuglio, T.; et al. Severity of Coronary Atherosclerosis and Risk of Diabetes Mellitus. J. Clin. Med. 2019, 8, 1069. [Google Scholar] [CrossRef] [Green Version]



| Parameters | SYNTAX < 33 (Ν = 477) | SYNTAX ≥ 33 (Ν = 62) | p-Value |
|---|---|---|---|
| Demographics | |||
| Female Sex–No (%) | 115 (24.2%) | 14 (23.3%) | 0.87 |
| Age (Years)–mean (±SD) | 62 (±13.0) | 69 (±11.0) | <0.01 |
| Body Mass Index (Kg/m2)–mean (±SD) | 28.3 (±4.5) | 28.6 (±4.7) | 0.63 |
| Coronary Heart Disease risk factors | |||
| Diabetes Mellitus–No (%) | 106 (22.3%) | 25 (41.7%) | <0.01 |
| Hypertension–No (%) | 244 (51.4%) | 41 (68.3%) | 0.01 |
| Dyslipidemia–No (%) | 150 (31.6%) | 20 (33.3%) | 0.79 |
| Smoking–No (%) | 257 (54.1%) | 29 (48.3%) | 0.39 |
| Family history–No (%) | 99 (20.8%) | 11 (18.3%) | 0.64 |
| Medical History/Underlying Diseases | |||
| Chronic kidney Disease–No (%) | 24 (5.1%) | 6 (10.0%) | 0.11 |
| Atrial Fibrillation–No (%) | 38 (8.0%) | 5 (8.3%) | 0.92 |
| Previous stroke–No (%) | 13 (2.7%) | 1 (1.7%) | 0.63 |
| Aortic Aneurysms–No (%) | 3 (0.6%) | 1 (1.7%) | 0.38 |
| Peripheral Vascular Disease–No (%) | 22 (4.6%) | 3 (5.0%) | 0.89 |
| Chronic Obstructive Pulmonary Disease–No (%) | 26 (5.5%) | 2 (3.3%) | 0.48 |
| Autoimmune Disease–No (%) | 7 (1.5%) | 3 (5.0%) | 0.04 |
| Risk Scores | |||
| GRACE Score–mean (±SD) | 115 (±39) | 126 (±37) | 0.01 |
| SYNTAX score–mean (±SD) | 12.8 (±9.4) | 42.9 (±9.6) | |
| Parameters on Admission-Means(±SD) | |||
| LVEF (%)–mean (±SD) | 48 (±11) | 44 (±11) | 0.01 |
| eGFR (mL/min)–mean (±SD) | 95 (±37) | 83 (±37) | 0.04 |
| Creatinine (mg/dL)–mean (±SD) | 1.09 (±0.93) | 1.09 (±1.29) | 0.37 |
| TnThs (ng/dL)–mean (±SD) | 1203 (±209) | 1153 (±191) | 0.70 |
| CPK (U/L)–mean (±SD) | 639 (±194) | 436 (±69) | 0.49 |
| LDH (U/L)–mean (±SD) | 423 (±46) | 393 (±28) | 0.84 |
| Total Cholesterol (mg/dL)–mean (±SD) | 166 (±43) | 154 (±46) | 0.07 |
| LDL (mg/dL)–mean (±SD) | 96 (±37) | 88 (±42) | 0.09 |
| HDL (mg/dL)–mean (±SD) | 40 (±11) | 43 (±14) | 0.17 |
| Bootstrapped Multivariate Analysis | 95% CI | |||
|---|---|---|---|---|
| Variables | Beta | Lower | Upper | p-Value (2-Tailed) |
| Diabetes Mellitus | 4.738 | 1.909 | 7.402 | 0.002 |
| Age | 0.106 | 0.014 | 0.200 | 0.027 |
| Gender | 2.979 | 0.409 | 5.575 | 0.020 |
| GRACE Groups | 3.261 | 1.711 | 4.769 | 0.001 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sofidis, G.; Otountzidis, N.; Stalikas, N.; Karagiannidis, E.; Papazoglou, A.S.; Moysidis, D.V.; Panteris, E.; Deda, O.; Kartas, A.; Zegkos, T.; et al. Association of GRACE Risk Score with Coronary Artery Disease Complexity in Patients with Acute Coronary Syndrome. J. Clin. Med. 2021, 10, 2210. https://doi.org/10.3390/jcm10102210
Sofidis G, Otountzidis N, Stalikas N, Karagiannidis E, Papazoglou AS, Moysidis DV, Panteris E, Deda O, Kartas A, Zegkos T, et al. Association of GRACE Risk Score with Coronary Artery Disease Complexity in Patients with Acute Coronary Syndrome. Journal of Clinical Medicine. 2021; 10(10):2210. https://doi.org/10.3390/jcm10102210
Chicago/Turabian StyleSofidis, Georgios, Nikolaos Otountzidis, Nikolaos Stalikas, Efstratios Karagiannidis, Andreas S. Papazoglou, Dimitrios V. Moysidis, Eleftherios Panteris, Olga Deda, Anastasios Kartas, Thomas Zegkos, and et al. 2021. "Association of GRACE Risk Score with Coronary Artery Disease Complexity in Patients with Acute Coronary Syndrome" Journal of Clinical Medicine 10, no. 10: 2210. https://doi.org/10.3390/jcm10102210