Cognition and Behavior of COVID-19 Vaccination Based on the Health Belief Model: A Cross-Sectional Study
Abstract
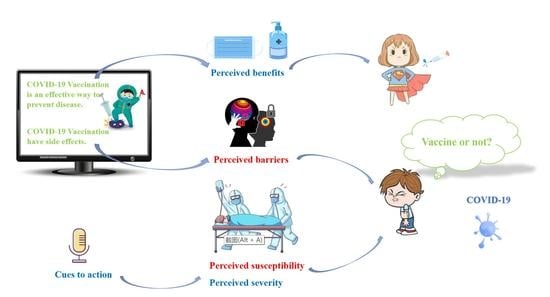
:1. Introduction
2. Materials and Methods
2.1. Study Design and Participants
2.2. Questionnaires
2.3. Statistical Analysis
3. Results
3.1. Demographic Characteristics
3.2. Health Status and Preventive Behaviors
3.3. Willingness to Be Vaccinated and Cognitive Level of COVID-19
3.4. HBM-Based Heterogeneity Factors
4. Discussion
Limitations and Strengths
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Yu, N.; Li, W.; Kang, Q.; Xiong, Z.; Wang, S.; Lin, X.; Liu, Y.; Xiao, J.; Liu, H.; Deng, D.; et al. Clinical features and obstetric and neonatal outcomes of pregnant patients with COVID-19 in Wuhan, China: A retrospective, single-centre, descriptive study. Lancet Infect. Dis. 2020, 20, 559–564. [Google Scholar] [CrossRef] [Green Version]
- Baidu. Real-Time Data Report on the Epidemic Situation of COVID-19. Available online: https://voice.baidu.com/act/newpneumonia/newpneumonia/?from=osari_aladin_banner (accessed on 28 January 2022).
- World Health Organization. Coronavirus Disease (COVID-19) Weekly Epidemiological Update and Weekly Operational Update. Available online: https://www.who.int/emergencies/diseases/novel-coronavirus-2019/situation-reports (accessed on 28 January 2022).
- World Health Organization. Statement on the Tenth Meeting of the International Health Regulations (2005) Emergency Committee Regarding the Coronavirus Disease (COVID-19) Pandemic. Available online: https://www.who.int/news/item/19-01-2022-statement-on-the-tenth-meeting-of-the-international-health-regulations-(2005)-emergency-committee-regarding-the-coronavirus-disease-(covid-19)-pandemic (accessed on 28 January 2022).
- Neumann-Böhme, S.; Varghese, N.E.; Sabat, I.; Barros, P.P.; Brouwer, W.; Van Exel, J.; Schreyögg, J.; Stargardt, T. Once we have it, will we use it? A European survey on willingness to be vaccinated against COVID-19. Eur. J. Health Econ. 2020, 21, 977–982. [Google Scholar] [CrossRef] [PubMed]
- Lin, Y.; Hu, Z.; Zhao, Q.; Alias, H.; Danaee, M.; Wong, L.P. Understanding COVID-19 vaccine demand and hesitancy: A nationwide online survey in China. PLoS Negl. Trop. Dis. 2020, 14, e0008961. [Google Scholar] [CrossRef] [PubMed]
- Geoffard, P.-Y.; Philipson, T. Disease Eradication: Private versus Public Vaccination. Am. Econ. Rev. 1997, 87, 222–230. [Google Scholar]
- Litaker, J.R.; Tamez, N.; Bray, C.L.; Durkalski, W.; Taylor, R. Sociodemographic Factors Associated with Vaccine Hesitancy in Central Texas Immediately Prior to COVID-19 Vaccine Availability. Int. J. Environ. Res. Public Health 2021, 19, 368. [Google Scholar] [CrossRef] [PubMed]
- Fridman, A.; Gershon, R.; Gneezy, A. COVID-19 and vaccine hesitancy: A longitudinal study. PLoS ONE 2021, 16, e0250123. [Google Scholar] [CrossRef] [PubMed]
- Elharake, J.A.; Shafiq, M.; McFadden, S.M.; Malik, A.A.; Omer, S.B. The Association of COVID-19 Risk Perception, County Death Rates, and Voluntary Health Behaviors among U.S. Adult Population. J. Infect. Dis. 2021, 225, 593–597. [Google Scholar] [CrossRef] [PubMed]
- Girma, S.; Agenagnew, L.; Beressa, G.; Tesfaye, Y.; Alenko, A. Risk perception and precautionary health behavior toward COVID-19 among health professionals working in selected public university hospitals in Ethiopia. PLoS ONE 2020, 15, e0241101. [Google Scholar]
- Kasl, S.V.; Cobb, S. Health behavior, illness behavior, and sick role behavior. I. Health and illness behavior. Arch. Environ. Health 1966, 12, 246–266. [Google Scholar] [CrossRef] [PubMed]
- Brewer, N.T.; Chapman, G.B.; Gibbons, F.X.; Gerrard, M.; McCaul, K.D.; Weinstein, N.D. Meta-analysis of the relationship between risk perception and health behavior: The example of vaccination. Health Psychol. 2007, 26, 136–145. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rosenstock, I.M. The health belief model and preventive health behavior. Health Educ. Monogr. 1974, 2, 354–386. [Google Scholar] [CrossRef]
- Rosenstock, I.M. Historical origins of the health belief model. Health Educ. Monogr. 1974, 2, 328–335. [Google Scholar] [CrossRef]
- Southern Metropolis Daily. 1.21 Billion People Have Been Fully Vaccinated with the COVID-19 Vaccine, with a Coverage Rate of 86% in China. 2022. Available online: https://www.sohu.com/a/515207579_161795?g=0 (accessed on 8 January 2022).
- Rontos, K.; Syrmali, M.-E.; Salvati, L. Unravelling the Role of Socioeconomic Forces in the Early Stage of COVID-19 Pandemic: A Global Analysis. Int. J. Environ. Res. Public Health 2021, 18, 6340. [Google Scholar] [CrossRef] [PubMed]
- Melin, K.; Zhang, C.; Zapata, J.; Rivera, Y.; Fernandez, K.; Shacham, E.; Malavé-Rivera, S.; Rodriguez-Diaz, C. Factors Associated with Intention to Receive Vaccination against COVID-19 in Puerto Rico: An Online Survey of Adults. Int. J. Environ. Res. Public Health 2021, 18, 7743. [Google Scholar] [CrossRef] [PubMed]
- Fisher, K.A.; Bloomstone, S.J.; Walder, J.; Crawford, S.; Fouayzi, H.; Mazor, K.M. Attitudes Toward a Potential SARS-CoV-2 Vaccine: A Survey of U.S. Adults. Ann. Intern. Med. 2020, 173, 964–973. [Google Scholar] [CrossRef] [PubMed]
- Wong, M.C.; Wong, E.L.; Huang, J.; Cheung, A.W.; Law, K.; Chong, M.K.; Ng, R.W.; Lai, C.K.; Boon, S.S.; Lau, J.T. Acceptance of the COVID-19 vaccine based on the health belief model: A population-based survey in Hong Kong. Vaccine 2021, 39, 1148–1156. [Google Scholar] [CrossRef] [PubMed]
- Wong, L.P.; Alias, H.; Wong, P.-F.; Lee, H.Y.; Abubakar, S. The use of the health belief model to assess predictors of intent to receive the COVID-19 vaccine and willingness to pay. Hum. Vaccines Immunother. 2020, 16, 2204–2214. [Google Scholar] [CrossRef] [PubMed]
- Mo, P.K.H.; Lau, J.T.F. Influenza vaccination uptake and associated factors among elderly population in Hong Kong: The application of the Health Belief Model. Health Educ. Res. 2015, 30, 706–718. [Google Scholar] [CrossRef] [PubMed] [Green Version]





| Variables | Total | Region Classification | χ2 | p-Value | ||
|---|---|---|---|---|---|---|
| Low-Risk | Medium-Risk | High-Risk | ||||
| Gender | ||||||
| Male | 733 (44.7) | 673 (41.0) | 29 (1.8) | 31 (1.9) | 1.51 | 0.47 |
| Female | 907 (55.3) | 819 (49.9) | 38 (2.3) | 50 (3.0) | ||
| Age | ||||||
| ≤19 | 115 (7.0) | 90 (5.5) | 14 (0.8) | 11 (0.7) | 24.73 | <0.001 |
| 20–29 | 539 (32.9) | 478 (29.1) | 27 (1.7) | 34 (2.1) | ||
| 30–39 | 437 (26.6) | 404 (24.6) | 17 (1.0) | 16 (1.0) | ||
| ≥40 | 549 (33.5) | 516 (31.5) | 13 (0.8) | 20 (1.2) | ||
| Occupation | ||||||
| Medical workers | 299 (18.2) | 267 (16.3) | 10 (0.6) | 22 (1.3) | 38.46 | 0.06 |
| Scientific researchers | 61 (3.7) | 56 (3.4) | 1 (0.1) | 4 (0.2) | ||
| Health system staff | 72 (4.4) | 66 (4.0) | 4 (0.2) | 2 (0.1) | ||
| Civil servants/institution staff | 87 (5.3) | 81 (4.9) | 3 (0.2) | 3 (0.2) | ||
| Teaching staff | 97 (5.9) | 90 (5.5) | 5 (0.3) | 2 (0.1) | ||
| Students | 304 (18.6) | 258 (15.8) | 18 (1.1) | 28 (1.7) | ||
| Company employees | 202 (12.3) | 186 (11.3) | 9 (0.5) | 7 (0.4) | ||
| Social workers | 120 (7.3) | 114 (7.0) | 3 (0.2) | 3 (0.2) | ||
| Service staff | 108 (6.6) | 103 (6.3) | 4 (0.2) | 1 (0.1) | ||
| Farmers/workers | 39 (2.4) | 38 (2.3) | 0 (0.0) | 1 (0.1) | ||
| Liberal professions | 57 (3.5) | 51 (3.1) | 4 (0.2) | 2 (0.1) | ||
| Retirees | 29 (1.8) | 29 (1.8) | 0 (0.0) | 0 (0.0) | ||
| Others | 165 (10.1) | 153 (9.3) | 6 (0.4) | 6 (0.4) | ||
| Educational level | ||||||
| Junior high school or below | 128 (7.8) | 122 (7.4) | 4 (0.2) | 2 (0.1) | 7.70 | 0.26 |
| Senior high school/technical secondary school | 253 (15.4) | 237 (14.5) | 8 (0.5) | 8 (0.5) | ||
| Undergraduate/junior college | 931 (56.8) | 836 (51.0) | 41 (2.5) | 54 (3.3) | ||
| Postgraduate or above | 328 (20.0) | 297 (18.1) | 14 (0.9) | 17 (1.0) | ||
| Marital status | ||||||
| Spinsterhood | 495 (30.2) | 417 (25.4) | 37 (2.3) | 41 (2.5) | 44.19 | <0.001 |
| Married | 966 (58.9) | 905 (55.2) | 23 (1.4) | 38 (2.3) | ||
| Divorced | 152 (9.3) | 143 (8.7) | 7 (0.4) | 2 (0.1) | ||
| Widowed | 27 (1.6) | 27 (1.6) | 0 (0.0) | 0 (0.0) | ||
| Residence | ||||||
| Urban area | 1389 (84.7) | 1259 (76.8) | 62 (3.8) | 68 (4.1) | 3.32 | 0.19 |
| Rural area | 251 (15.3) | 233 (14.2) | 5 (0.3) | 13 (0.8) | ||
| Monthly household income (RMB) | ||||||
| ≤3000 | 273 (16.6) | 256 (15.6) | 9 (0.5) | 8 (0.5) | 9.16 | 0.17 |
| 3001–5000 | 385 (23.5) | 359 (21.9) | 11 (0.7) | 15 (0.9) | ||
| 5001–10,000 | 479 (29.2) | 426 (26.0) | 25 (1.5) | 28 (1.7) | ||
| >10,000 | 503 (30.7) | 451 (27.5) | 22 (1.3) | 30 (1.8) | ||
| Variables | Age | Educational Level # | ||||||
|---|---|---|---|---|---|---|---|---|
| ≤19 | 20–29 | 30–39 | ≥40 | I | II | III | IV | |
| Are you willing to have the COVID-19 vaccination? | ||||||||
| Yes | 110 (6.7) | 533 (32.6) | 436 (26.5) | 542 (33.1) | 128 (7.8) | 248 (15.1) | 920 (56.1) | 325 (19.8) |
| No | 5 (0.3) | 6 (0.3) | 1 (0.1) | 7 (0.4) | 0 (0.0) | 5 (0.3) | 11 (0.7) | 3 (0.2) |
| p-value | 0.003 | 0.37 | ||||||
| Have you had the COVID-19 vaccination? | ||||||||
| Yes, all the injections have been administered | 92 (5.6) | 465 (28.4) | 406 (24.7) | 522 (31.8) | 120 (7.3) | 237 (14.4) | 843 (51.4) | 285 (17.4) |
| Yes, but not all of the vaccinations have been administered | 18 (1.1) | 51 (3.1) | 17 (1.0) | 11 (0.7) | 5 (0.3) | 11 (0.7) | 48 (3.0) | 33 (2.0) |
| No | 5 (0.3) | 23 (1.4) | 14 (0.9) | 16 (1.0) | 3 (0.2) | 5 (0.3) | 40 (2.4) | 10 (0.6) |
| p-value | <0.001 | <0.001 | ||||||
| Do you think vaccination is an effective way to prevent disease? | ||||||||
| Yes | 109 (6.6) | 500 (30.6) | 417 (25.4) | 525 (32.0) | 123 (7.5) | 248 (15.1) | 877 (53.5) | 304 (18.5) |
| No | 1 (0.1) | 3 (0.2) | 0 (0.0) | 1 (0.1) | 0 (0.0) | 1 (0.1) | 2 (0.1) | 1 (0.1) |
| Not sure | 5 (0.3) | 36 (2.2) | 20 (1.2) | 23 (1.4) | 5 (0.3) | 4 (0.2) | 52 (3.2) | 23 (1.4) |
| p-value | 0.26 | 0.11 | ||||||
| Do you think the vaccinations from different producers will have an effect on the body? | ||||||||
| Yes | 20 (1.2) | 170 (10.3) | 230 (14.1) | 324 (19.8) | 84 (5.2) | 170 (10.4) | 388 (23.7) | 103 (6.3) |
| No | 32 (2.0) | 80 (4.9) | 42 (2.5) | 45 (2.7) | 4 (0.2) | 12 (0.7) | 138 (8.4) | 47 (2.9) |
| Not sure | 63 (3.8) | 289 (17.7) | 165 (10.0) | 180 (11.0) | 40 (2.4) | 71 (4.3) | 405 (24.7) | 178 (10.8) |
| p-value | <0.001 | <0.001 | ||||||
| How long do you think the full dose of the COVID-19 vaccine will last? | ||||||||
| <6 months | 21 (1.3) | 147 (8.9) | 130 (7.9) | 178 (10.9) | 42 (2.6) | 99 (6.0) | 255 (15.5) | 81 (4.9) |
| ≥6 months | 36 (2.2) | 188 (11.5) | 215 (13.1) | 264 (16.1) | 63 (3.8) | 123 (7.6) | 395 (24.2) | 124 (7.6) |
| Lifelong | 3 (0.2) | 14 (0.9) | 18 (1.1) | 23 (1.4) | 9 (0.5) | 9 (0.5) | 33 (2.0) | 6 (0.4) |
| Not sure | 55 (3.3) | 190 (11.6) | 74 (4.5) | 84 (5.1) | 14 (0.9) | 22 (1.3) | 248 (15.1) | 117 (7.1) |
| p-value | <0.001 | <0.001 | ||||||
| Variables | Model 1 | Model 2 | ||||
|---|---|---|---|---|---|---|
| B | OR (95% CI) | p-Value | B | OR (95% CI) | p-Value | |
| HBM | ||||||
| Perceived severity | 0.16 | 1.18 (0.88,1.57) | 0.27 | 0.13 | 1.13 (0.84,1.54) | 0.42 |
| Perceived susceptibility | −0.73 | 0.48 (0.31,0.75) | 0.001 | −0.75 | 0.47 (0.30,0.74) | 0.001 |
| Perceived benefits | 1.01 | 2.76 (1.62,4.70) | <0.001 | 1.14 | 3.13 (1.79,5.47) | <0.001 |
| Perceived barriers | −0.72 | 0.49 (0.32,0.76) | 0.001 | −0.81 | 0.44 (0.29,0.69) | <0.001 |
| Cues to action | 0.83 | 2.30 (1.71,3.09) | <0.001 | 0.80 | 2.23 (1.60,3.11) | <0.001 |
| Health behavior | −0.04 | 0.96 (0.74,1.24) | 0.76 | −0.03 | 0.97 (0.75,1.27) | 0.84 |
| Demographic factors | ||||||
| Gender | 0.46 | 1.58 (0.88,2.83) | 0.13 | |||
| Age | 0.08 | 1.08 (0.60, 1.95) | 0.80 | |||
| Occupation | 0.12 | 1.13 (1.04, 1.23) | 0.003 | |||
| Educational level | 0.08 | 1.08 (0.71, 1.64) | 0.71 | |||
| Marital status | −0.34 | 0.71 (0.38, 1.35) | 0.30 | |||
| Residence | 0.44 | 1.56 (0.74, 3.28) | 0.24 | |||
| Household income | 0.25 | 1.28 (0.97, 1.69) | 0.08 | |||
| Health factors | ||||||
| Health status | 0.70 | 2.02 (0.86, 4.71) | 0.10 | |||
| Health perception | −0.64 | 0.53 (0.12,2.43) | 0.41 | |||
| Comparison of the two models | ||||||
| Index of modelfitting effect | Model 1 | Model 2 | ||||
| Rho-squared | 0.16 | 0.18 | ||||
| Final log-likelihood | −149.13 | −143.63 | ||||
| Akaike information criterion | 467.26 | 460.26 | ||||
| Bayesian nformation riterion | 953.26 | 897.86 | ||||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cai, Z.; Hu, W.; Zheng, S.; Wen, X.; Wu, K. Cognition and Behavior of COVID-19 Vaccination Based on the Health Belief Model: A Cross-Sectional Study. Vaccines 2022, 10, 544. https://doi.org/10.3390/vaccines10040544
Cai Z, Hu W, Zheng S, Wen X, Wu K. Cognition and Behavior of COVID-19 Vaccination Based on the Health Belief Model: A Cross-Sectional Study. Vaccines. 2022; 10(4):544. https://doi.org/10.3390/vaccines10040544
Chicago/Turabian StyleCai, Zemin, Wei Hu, Shukai Zheng, Xilin Wen, and Kusheng Wu. 2022. "Cognition and Behavior of COVID-19 Vaccination Based on the Health Belief Model: A Cross-Sectional Study" Vaccines 10, no. 4: 544. https://doi.org/10.3390/vaccines10040544