“Mom Let’s Go to the Dentist!” Preliminary Feasibility of a Tailored Dental Intervention for Children with Autism Spectrum Disorder in the Italian Public Health Service
Abstract
:1. Introduction
2. Method
2.1. Sample
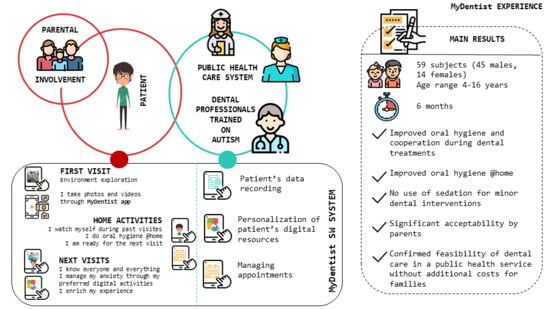
2.2. Intervention
2.2.1. MyDentist
2.2.2. The MyDentist Web Application
- Digital Copybook mode (for all patients): during visits to collect photos and videos (selfies and not) that the child can review and show to family members once at home;
- Mirror mode: during the visits used in camera-selfie mode to allow the child to see himself during dental practices;
- Distractor mode: during the visit to distract or to relax with favorite videos/pictures;
- Reinforcement mode: at the end of the session to perform entertainment and play activities that work both as reinforcement and as consolidation of the activities carried out during the visit;
- Familiarization/learning mode: at home to recall previous visits, to prepare for the next one and to perform digital activities assigned by the dentist (playing games, watching videos, practicing social stories, etc.).
- Dentist Area: where the dentist creates the personalized profile of each patient, in order to schedule a visit, build a personalized clinical path, collect multimedia materials of visits, create personalized clinical programs by customizing games, share resources and assign home tasks.
- Patient Area: where each patient can access his/her personalized path. This includes games showing dental procedures in an amusing way (e.g., sequences, puzzles, memories); video models for dental procedures (for instance showing how to use a toothbrush), interactive PDF files to get used to dental clinic sounds, social stories that introduce the dental environment, procedures and/or objects and photos/videos collected during visits.
2.2.3. The MyDentist Intervention Protocol
3. Procedure
3.1. MyDentist Intervention Path
3.1.1. Preliminary Interview with Parents
3.1.2. First Visit
3.1.3. Familiarization Session via a Psychological Approach
3.1.4. Operative Sessions
4. Instruments
4.1. Questionnaires
4.2. Psychophysiological Assessment
- Heart rate (HR): the number of contractions of the heart occurring per time unit, expressed in bpm;
- Root mean square of successive differences (RMSSD): measure of heart rate variability (HRV), specifically related to parasympathetic activity, expressed in ms;
- Normalized component of the power spectral density of the ECG signal at low frequency (0.04–0.15 Hz) (nLF); it is related both to the sympathetic and parasympathetic response;
- Normalized component of the power spectral density of the ECG spectrum at high frequency (0.15–0.4 Hz) (nHF); it is mainly related to the parasympathetic response;
- Low- vs. high-frequency components of the power spectral density of the ECG spectrum (LF/HF Ratio): under controlled conditions, it expresses the balance between the sympathetic and parasympathetic nervous system branches [49].
5. Descriptive Analysis
6. Results
6.1. Questionnaires
6.2. Psychophysiological Assessment
7. Discussion
- Professionals are trained in how to treat people with ASD. As mentioned in the Introduction, to increase the probability of successful dental treatment for patients with ASD, dentists should have an in-depth interdisciplinary understanding of ASD in terms of symptomatology and functional profiles, but unfortunately the professional training offered by most university programs does not deal specifically with people with ASD.
- Professionals are also trained to use the MyDentist application, which helps to set up a personalized use of the ICT tools
- In the first period of the intervention, an additional person acting as an ICT-mediator for both professionals and patients/caregivers joined the dental clinic staff.
- Cost for the design and development of the MyDentist application;
- Cost of the cloud-storage service;
- Cost of a tablet for the dental clinic;
- A 2-year employment contract for an ICT mediator.
- For professionals:
- -
- Training regarding people with ASD and the most appropriate way to interact with them;
- -
- Training to use the MyDentist application: to this aim, we are finalizing all the documentation such as user manual, tutorials and demo, which will be freely available.
- For the clinic:
- -
- A 6- or 12-month employment contract for an ICT mediator.
8. Limits of the Study
9. Future Direction
10. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- American Psychiatric Association (APA). Diagnostic and Statistical Manual of Mental Disorders, 5th ed.; American Psychiatric Association: Washington, DC, USA, 2013. [Google Scholar]
- Maenner, M.J.; Shaw, K.A.; Baio, J.; Washington, A.; Patrick, M.; DiRienzo, M.; Christensen, D.L.; Wiggins, L.D.; Pettygrove, S.; Andrews, J.G.; et al. Prevalence of Autism spectrum disorder Among Children Aged 8 Years—Autism and Developmental Disabilities Monitoring Network, 11 Sites, United States, 2016. Mmwr Surveill. Summ. 2020, 69, 1–12. [Google Scholar] [CrossRef] [PubMed]
- Narzisi, A.; Posada, M.; Barbieri, F.; Chericoni, N.; Ciu_olini, D.; Pinzino, M.; Romano, R.; Scattoni, M.L.; Tancredi, R.; Calderoni, S.; et al. Prevalence of Autism spectrum disorder in a large Italian catchment area, a school-based population study within the ASDEU project. Epidemiol. Psychiatr. Sci. 2018, 29, e5. [Google Scholar] [CrossRef] [PubMed]
- Levy, S.E.; Mandell, D.S.; Schultz, R.T. Autism. Lancet 2009, 7, 162738. [Google Scholar] [CrossRef]
- Delli, K.; Reichart, P.A.; Bornstein, M.; Livas, C. Management of children with autism spectrum disorder in the dental setting: Concerns, behavioural approaches and Recommenda-tions. Med. Oral Patol. Oral Y Cir. Bucal 2013, 18, e862–e868. [Google Scholar] [CrossRef]
- Gandhi, R.P.; Klein, U. Autism spectrum disorders: An update on oral health management. J. Evid. Based Dent. Pract. 2014, 14, 115–126. [Google Scholar] [CrossRef]
- Lu, J.; Sun, C.A. Evaluation of the effect of concentrated growth factor in oral rehabilitation. Shanghai Kou Qiang Yi Xue 2018, 27, 93–95. [Google Scholar] [PubMed]
- Robertson, M.D.; Schwendicke, F.; de Araujo, M.P.; Radford, J.R.; Harris, J.C.; McGregor, S.; Innes, N.P.T. Dental caries experience, care index and restorative index in children with learning disabilities and children without learning disabilities; a systematic review and meta-analysis. BMC Oral Health 2019, 19, 146. [Google Scholar] [CrossRef] [Green Version]
- Chandrashekhar, S.; Bommangoudar, J.S. Management of Autistic Patients in Dental Office: A Clinical Update. Int. J. Clin. Pediatr Dent. 2018, 11, 219–227. [Google Scholar] [CrossRef]
- Du, R.Y.; Yiu, C.K.Y.; King, N.G. Oral Health Behaviours of Preschool Children with Autism Spectrum Disorders and Their Barriers to Dental Care. J. Autism Dev. Disord. 2019, 49, 453–459. [Google Scholar] [CrossRef]
- Kuhaneck, H.M.; Chisholm, E.C. Improving Dental Visits for Individuals with Autism Spectrum Disorders Through an Understanding of Sensory Processing. Spec. Care Dent. 2012, 32, 229–233. [Google Scholar] [CrossRef]
- Stein, L.I.; Polido, J.C.; Cermak, S.A. Oral care and sensory over-responsivity in children with autism spectrum disorders. Pediatr Dent. 2013, 35, 230–235. [Google Scholar] [PubMed]
- Stein, L.I.; Lane, C.J.; Williams, M.E.; Dawson, M.E.; Polido, J.C.; Cermak, S.A. Physiological and behavioral stress and anxiety in children with autism spectrum disorders during routine oral care. Biomed. Res. Int. 2014, 2014, 694876. [Google Scholar] [CrossRef]
- Khrautieo, T.; Srimaneekarn, N.; Rirattanapong, P.; Smutkeeree, A. Association of sensory sensitivities and toothbrushing cooperation in autism spectrum disorder. Int. J. Paediatr Dent. 2020, 30, 505–513. [Google Scholar] [CrossRef] [PubMed]
- Bartolomé-Villar, B.; Mourelle-Martínez, M.R.; Diéguez-Pérez, M.; de Nova-García, M.J. Incidence of Oral Health in Paediatric Patients with Disabilities: Sensory Disorders and Autism Spectrum Disorder. Systematic Review II. J. Clin. Exp. Dent. 2016, 8, e344–e351. [Google Scholar] [CrossRef] [PubMed]
- Neil, L.; Choque Olsson, N.; Pellicano, E. The Relationship between Intolerance of Uncertainty, Sensory Sensitivities, and Anxiety in Autistic and Typically Developing Children. J. Autism Dev. Disord. 2016, 46, 1962–1973. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cermak, S.A.; Stein Duker, L.I.; Williams, M.I.; Dawson, M.E.; Lane, C.J.; Polido, J.C. Sensory Adapted Dental Environments to Enhance Oral Care for Children with Autism Spectrum Disorders: A Randomized Controlled Pilot Study. J. Autism Dev. Disord. 2015, 45, 2876–2888. [Google Scholar] [CrossRef]
- Duker, L.I.S.; Henwood, B.F.; Bluthenthal, R.N.; Juhlin, E.; Polido, J.C.; Cermak, S.A. Parents’ perceptions of dental care challenges in male children with autism spectrum disorder: An initial qualitative exploration. Res. Autism Spectr Disord. 2017, 39, 63–67. [Google Scholar] [CrossRef]
- Kilroy, E.; Aziz-Zadeh, L.; Cermak, S. Ayres Theories of Autism and Sensory Integration Revisited: What Contemporary Neuroscience Has to Say. Brain Sci. 2019, 21, 68. [Google Scholar] [CrossRef] [Green Version]
- Robertson, C.E.; Baron-Cohen, S. Sensory perception in autism. Nat. Rev. Neurosci. 2017, 18, 671–684. [Google Scholar] [CrossRef]
- Epitropakis, C.; DiPietro, E.A. Medication Compliance Protocol for Pediatric Patients with Severe Intellectual and Behavioral Disabilities. J. Pediatr Nurs. 2015, 30, 329–332. [Google Scholar] [CrossRef]
- Rouches, A.; Lefer, G.; Dajean-Trutaud, S.; Lopez-Cazaux, S. Amélioration de la santé orale des enfants avec autisme: Les outils à notre disposition. Arch. De Pédiatrie 2018, 25, 145–149. [Google Scholar] [CrossRef] [PubMed]
- Ferrazzano, G.F.; Salerno, C.; Bravaccio, C.; Ingenito, A.; Sangianantoni, G.; Cantile, T. Autism spectrum disorders and oral health status: Review of the literature. Eur. J. Paediatr. Dent. 2020, 21, 9–12. [Google Scholar] [PubMed]
- Capp, P.L.; de Faria, M.E.; Siqueira, S.R.; Cillo, M.T.; Prado, E.G.; de Siqueira, J.T. Special care dentistry: Midazolam conscious sedation for patients with neurological diseases. Eur J. Paediatr Dent. 2010, 11, 162–164. [Google Scholar] [PubMed]
- Summers, J.; Shahrami, A.; Cali, S.; D’Mello, C.; Kdako, M.; Palikucin-Reljin, A.; Lunsky, Y. Self-Injury in Autism spectrum disorder and intellectual disability: Exploring the role of reactivity to pain and sensory input. Brain Sci. 2017, 7, 140. [Google Scholar] [CrossRef] [Green Version]
- Stiefel, D.J. Dental care considerations for disabled adults. Special care in dentistry. American Association of Hospital Dentists, the Academy of Dentistry for the Handicapped, and the American Society for Geriatric Dentistry. Spec. Care Dent. 2002, 22 (Suppl. 3), 26S. [Google Scholar]
- Bondioli, M.; Buzzi, M.C.; Buzzi, M.; Pelagatti, S.; Senette, C. ICT to aid dental care of children with autism. In Proceedings of the 19th International ACM SIGACCESS Conference on Computers and Accessibility, Baltimore, MD, USA, 30 October–1 November 2017. [Google Scholar]
- da Silva, S.N.; Gimenez, T.; Souza, R.C.; Mello-Moura, A.C.V.; Raggio, D.P.; Morimoto, S.; Lara, J.S.; Soares, G.C.; Tedesco, T.K. Oral health status of children and young adults with autism spectrum disorders: Systematic review and meta-analysis. Int. J. Paediatr. Dent. 2017, 27, 388–398. [Google Scholar] [CrossRef]
- WHO. Sixty-Seventh World Health Assembly; WHO: Geneva, Switzerland, 2014. [Google Scholar]
- American Academy of Pediatric Dentistry. Reference Manual 2010–2011; American Academy of Pediatric Dentistry: Chicago, IL, USA, 2010. [Google Scholar]
- Grewal, N.; Sethi, T.; Grewal, S. Widening horizons through alternative and augmentative communication systems for managing children with special health care needs in a pediatric dental setup. Spec. Care Dent. 2015, 35, 114–119. [Google Scholar] [CrossRef]
- Popple, B.; Wall, C.; Flink, L.; Powell, K.; Discepolo, K.; Keck, D.; Mademtzi, M.; Volkmar, F.; Shic, F. Brief Report: Remotely Delivered Video Modeling for Improving Oral Hygiene in Children with ASD: A Pilot Study. J. Autism Dev. Disord. 2016, 46, 2791–2796. [Google Scholar] [CrossRef] [Green Version]
- Bernard-Opitz, V.; Sriram, N.; Nakhoda-Sapuan, S. Enhancing social problem solving in children with autism and normal children through computer-assisted instruction. J. Autism Dev. Disord. 2001, 31, 377–384. [Google Scholar] [CrossRef]
- Rank, R.C.I.C.; Vilela, J.E.R.; Rank, M.S.; Ogawa, W.N.; Imparato, J.C.P. Effect of awards after dental care in children’s motivation. Eur. Arch. Paediatr Dent. 2019, 20, 85–93. [Google Scholar] [CrossRef]
- Isong, I.A.; Rao, S.R.; Holifield, C.; Iannuzzi, D.; Hanson, E.; Ware, J.; Nelson, L.P. Addressing Dental Fear in Children With Autism Spectrum Disorders: A Randomized Controlled Pilot Study Using Electronic Screen Media. Clin. Pediatr (Phila.) 2014, 53, 230–237. [Google Scholar] [CrossRef]
- Mah, J.W.; Tsang, P. Visual Schedule System in Dental Care for Patients with Autism: A Pilot Study. J. Clin. Pediatr Dent. 2016, 40, 393–399. [Google Scholar] [CrossRef] [PubMed]
- Nilchian, F.; Shakibaei, F.; Jarah, Z.T. Evaluation of Visual Pedagogy in Dental Check-ups and Preventive Practices Among 6-12-Year-Old Children with Autism. J. Autism Dev. Disord. 2017, 47, 858–864. [Google Scholar] [CrossRef] [PubMed]
- Prado, I.M.; Carcavalli, L.; Abreu, L.G.; Serra-Negra, J.M.; Paiva, S.M.; Martins, C.C. Use of distraction techniques for the management of anxiety and fear in paediatric dental practice: A systematic review of randomized controlled trials. Int J. Paediatr Dent. 2019, 29, 650–668. [Google Scholar] [CrossRef] [PubMed]
- Charlop, M.H.; Milstein, J.P. Teaching autistic children conversational speech using video modeling. J. Appl. Behav. Anal. 1989, 22, 275–285. [Google Scholar] [CrossRef] [Green Version]
- Da Silva, M.L.; Gonçalves, D.; Guerreiro, T.; Silva, H. A web-based application to address individual interests of children with autism spectrum disorders. Procedia Comput. Sci. 2012, 14, 20–27. [Google Scholar] [CrossRef] [Green Version]
- Passerino, L.M.; Santarosa, L.M.C. Autism and digital learning environments: Processes of interaction and mediation. Comput. Educ. 2018, 51, 385–402. [Google Scholar] [CrossRef]
- Barry, S.M. Improving Access and Reducing Barriers to Dental Care for Children with Autism Spectrum Disorder; University of Leeds: West Yorkshire, UK, 2012. [Google Scholar]
- Porges, S.W. The polyvagal theory: Phylogenetic substrates of a social nervous system. Int. J. Psychophysiol. 2001, 42, 123–146. [Google Scholar] [CrossRef]
- Porges, S.W. The Polyvagal Theory: Phylogenetic contributions to social behavior. Physiol. Behav. 2003, 79, 503–513. [Google Scholar] [CrossRef]
- Billeci, L.; Tonacci, A.; Tartarisco, G.; Narzisi, A.; Di Palma, S.; Corda, D.; Baldus, G.; Cruciani, F.; Anzalone, S.M.; Calderoni, S.; et al. The MICHELANGELO Study Group. An Integrated Approach for the Monitoring of Brain and Autonomic Response of Children with Autism spectrum disorders during Treatment by Wearable Technologies. Front. Neurosci. 2016, 10, 276. [Google Scholar] [CrossRef] [Green Version]
- Di Palma, S.; Tonacci, A.; Narzisi, A.; Domenici, C.; Pioggia, G.; Muratori, F.; Billeci, L. The MICHELANGELO Study Group. Monitoring of autonomic response to sociocognitive tasks during treatment in children with autism spectrum disorders by wearable technologies: A feasibility study. Comp. Biol. Med. 2017, 85, 143–152. [Google Scholar] [CrossRef] [PubMed]
- Billeci, L.; Tonacci, A.; Narzisi, A.; Manigrasso, Z.; Varanini, M.; Fulceri, F.; Lattarulo, C.; Calderoni, S.; Muratori, F. Heart Rate Variability during a Joint Attention Task in Toddlers with Autism spectrum disorders. Front. Physiol. 2018, 9, 467. [Google Scholar] [CrossRef] [Green Version]
- Pan, J.; Tompkins, W.J. A real-time QRS detection algorithm. Ieee Trans. Biomed. Eng. 1985, 32, 230–236. [Google Scholar] [CrossRef] [PubMed]
- Shaffer, F.; Ginsberg, J.P. An Overview of Heart Rate Variability Metrics and Norms. Front. Public Health 2017, 5, 258. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Boucsein, W. Electrodermal Activity; Springer Science & Business Media: Berlin, Germany, 2012. [Google Scholar]
- Hoefman, R.; Payakachat, N.; van Exel, J.; Kuhlthau, K.; Kovacs, E.; Pyne, J.; Tilford, J.M. Caring for a Child with Autism spectrum disorder and Parents’ Quality of Life: Application of the CarerQol. J. Autism Dev. Disord. 2014, 44, 1933–1945. [Google Scholar] [CrossRef] [Green Version]
- Naidoo, M.; Singh, S. A Dental Communication Board as an Oral Care Tool for Children with Autism spectrum disorder. J. Autism Dev. Disord. 2020, 5, 1–13. [Google Scholar] [CrossRef]
- Yamasaki, T.; Maekawa, T.; Takahashi, H.; Fujita, T.; Kamio, Y.; Tobimatsu, S. Electrophysiology of Visual and Auditory Perception in Autism Spectrum Disorders. Compr. Guide Autism 2014, 791–808. [Google Scholar]
- Fakhruddin, K.S.; El Batawi, H.Y. Effectiveness of audiovisual distraction in behavior modification during dental caries assessment and sealant placement in children with autism spectrum disorder. Dent. Res. J. 2017, 14, 177–182. [Google Scholar] [CrossRef]
- Jaber, M.A. Dental caries experience, oral health status and treatment needs of dental pa-tients with autism. J. Appl. Oral Sci. 2011, 19, 212–217. [Google Scholar] [CrossRef] [Green Version]
- Corridore, D.; Zumbo, G.; Corvino, I.; Guaragna, M.; Bossù, M.; Polimeni, A.; Vozza, I. Prevalence of oral disease and treatment types proposed to children affected by Autistic Spectrum Disorder in Pediatric Dentistry: A Systematic Review. Clin. Ter. 2020, 171, e275–e282. [Google Scholar]
- Penmetsa, C.; Penmetcha, S.; Cheruku, S.R.; Mallineni, S.K.; Patil, A.K.; Namineni, S. Role of Dental Discomfort Questionnaire-Based Approach in Recognition of Symptomatic Expressions Due to Dental Pain in Children with Autism spectrum disorders. Contemp Clin. Dent. 2019, 10, 446–451. [Google Scholar] [PubMed]
- Elmore, J.L.; Bruhn, A.M.; Bobzien, J.L. Interventions for the Reduction of Dental Anxiety and Corresponding Behavioral Deficits in Children with Autism Spectrum Disorder. J. Dent. Hyg. 2016, 90, 111–120. [Google Scholar] [PubMed]
- Shah, A.; Singh, S.; Ajithkrishnan, C.G.; Bipinkumar Kariya, P.; Patel, H.; Ghosh, A. Caregiver’s Sense of Coherence: A Predictor of Oral Health-Related Behaviors of Autistic Children in India. Contemp. Clin. Dent. 2019, 10, 197–202. [Google Scholar] [PubMed]





| Age | (in Years) |
|---|---|
| Mean | 9.9 |
| SD | 5.43 |
| Gender | n |
| Males | 45 |
| Females | 14 |
| DSM-5–ASD Severity Levels | |
| Level 1 | 5 |
| Level 2 | 37 |
| Level 3 | 17 |
| Cognitive Functioning | |
| Normal range | 5 |
| Mild | 4 |
| Moderate | 28 |
| Severe | 19 |
| Language | |
| No words | 29 |
| 2–3 words | 14 |
| Fluent | 16 |
| Never (0) | Sometimes (1) | Often (2) | Regularly (3) | Chi Square | |||||
|---|---|---|---|---|---|---|---|---|---|
| t0 | t1 | t0 | t1 | t0 | t1 | t0 | t1 | χ2; p | |
| n | n | n | n | n | n | n | n | ||
| Q.1 Does your child like to brush his teeth? | 12 | 8 | 33 | 27 | 9 | 12 | 5 | 11 | 4.07; ns |
| Q.2 Is it possible to teach oral hygiene? | 9 | 8 | 34 | 8 | 11 | 34 | 5 | 8 | 28.59; <0.001 |
| Q.3 Is your child able to follow the rules for proper dental hygiene? | 15 | 1 | 28 | 8 | 6 | 26 | 10 | 25 | 42.28; <0.001 |
| Q.4 Is your child capable of using a toothbrush? | 27 | 8 | 20 | 34 | 5 | 8 | 3 | 8 | 16.84; 0.001 |
| Q.5 Is your child capable of putting toothpaste on the toothbrush? | 32 | 17 | 16 | 8 | 6 | 17 | 5 | 17 | 19.06; <0.001 |
| Q.6 Does the child use dental floss? | 55 | 55 | 2 | 2 | 1 | 1 | 1 | 1 | 0; ns |
| Q.7 Does the child brush his teeth independently? | 32 | 8 | 19 | 25 | 6 | 24 | 2 | 1 | 26.34; <0.001 |
| Q.8 Is your child able to brush his teeth independently? | 8 | 1 | 1 | 8 | 8 | 39 | 38 | 8 | 50.89; <0.001 |
| Q.9 Is your child capable of brushing his teeth properly? | 13 | 8 | 21 | 17 | 12 | 8 | 13 | 25 | 6.19; ns |
| Q.10 Is your child able to brush his teeth twice a day after meals? | 13 | 25 | 26 | 8 | 11 | 24 | 9 | 1 | 24.54; <0.001 |
| Q.11 Does the child brush his teeth after meals? | 23 | 8 | 15 | 17 | 9 | 8 | 12 | 25 | 12; 0.007 |
| Q.12 Does the child experience hypersensitivity (i.e., toothbrush)? | 25 | 42 | 20 | 12 | 8 | 3 | 6 | 2 | 10.58; 0.014 |
| Q.13 Has the child ever had dental treatment? | 48 | 29 | 1 | 17 | 6 | 2 | 4 | 10 | 23.47; <0.001 |
| Q.14 Has it ever been necessary to resort to general sedation? | 29 | 1 | 9 | 1 | 5 | 1 | 15 | 56 | 58.87; <0.001 |
| Q.15 Does the child have a dental visit at least once a year? | 24 | 55 | 15 | 2 | 9 | 1 | 10 | 1 | 35.86; <0.001 |
| Q.16 Does your child become upset when he has to go to the dentist? | 30 | 1 | 20 | 7 | 7 | 25 | 2 | 25 | 63.10; <0.001 |
| Q.17 Is your child collaborative during dental visits? | 17 | 17 | 13 | 25 | 17 | 8 | 12 | 8 | 7.82; 0.049 |
| Q.18 Does he have difficulty remaining seated for the duration of the visit? | 12 | 9 | 33 | 29 | 9 | 11 | 5 | 9 | 2.02; ns |
| Questions | No | Little | Quite | Very | |
|---|---|---|---|---|---|
| % | % | % | % | ||
| Q.1 | Was the multimedia support used in MyDentist (MD) useful? | 0 | 0 | 40 | 60 |
| Q.2 | Was the multimedia support appropriately customized? | 0 | 0 | 37.9 | 62.1 |
| Q.3 | Was the experience of MD appreciated by your child? | 0 | 0 | 33.3 | 66.7 |
| Q.4 | Do you think that the tablet was hyper-stimulating for your child? | 38.7 | 19.4 | 9.7 | 32.3 |
| Q.5 | Did the use of the tablet facilitate good compliance of the child with the dental setting? | 0 | 0 | 35.5 | 64.6 |
| Q.6 | Did the use of the tablet reduce the child’s stress during the dental examination? | 14.2 | 0 | 42.9 | 42.9 |
| Q.7 | Did the child also use the tablet to become familiar with dental hygiene? | 3.2 | 22.6 | 51.6 | 22.6 |
| Q.8 | Have you found the child to be better adapted to the dental setting? | 0 | 0 | 71 | 29 |
| Q.9 | Is the child more cooperative during the dental examination? | 0 | 6.2 | 25 | 68.8 |
| Q.10 | Is the child more able to control sensory issues during the dental examination? | 0 | 0 | 48.9 | 51.6 |
| Q.11 | If present, have problematic behaviors during the dental examination decreased? | 7.7 | 13.3 | 36.7 | 43.3 |
| Q.12 | Is the child more collaborative in performing home hygiene? | 0 | 11.7 | 50 | 38.3 |
| Q.13 | Is the child more autonomous in the use of the suggested tools for dental hygiene? | 9.4 | 15.6 | 46.9 | 28.1 |
| Q.14 | Was the MD project useful? | 0 | 0 | 10.3 | 89.7 |
| Q.15 | Can you apply at home any advice received during the MD experience? | 0 | 0 | 69 | 31 |
| Q.16 | Would you recommend MD to parents of children with autism? | 0 | 0 | 0 | 100 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Narzisi, A.; Bondioli, M.; Pardossi, F.; Billeci, L.; Buzzi, M.C.; Buzzi, M.; Pinzino, M.; Senette, C.; Semucci, V.; Tonacci, A.; et al. “Mom Let’s Go to the Dentist!” Preliminary Feasibility of a Tailored Dental Intervention for Children with Autism Spectrum Disorder in the Italian Public Health Service. Brain Sci. 2020, 10, 444. https://doi.org/10.3390/brainsci10070444
Narzisi A, Bondioli M, Pardossi F, Billeci L, Buzzi MC, Buzzi M, Pinzino M, Senette C, Semucci V, Tonacci A, et al. “Mom Let’s Go to the Dentist!” Preliminary Feasibility of a Tailored Dental Intervention for Children with Autism Spectrum Disorder in the Italian Public Health Service. Brain Sciences. 2020; 10(7):444. https://doi.org/10.3390/brainsci10070444
Chicago/Turabian StyleNarzisi, Antonio, Mariasole Bondioli, Francesca Pardossi, Lucia Billeci, Maria Claudia Buzzi, Marina Buzzi, Martina Pinzino, Caterina Senette, Valentina Semucci, Alessandro Tonacci, and et al. 2020. "“Mom Let’s Go to the Dentist!” Preliminary Feasibility of a Tailored Dental Intervention for Children with Autism Spectrum Disorder in the Italian Public Health Service" Brain Sciences 10, no. 7: 444. https://doi.org/10.3390/brainsci10070444