Changes in Acute Phase Proteins in Bitches after Laparoscopic, Midline, and Flank Ovariectomy Using the Same Method for Hemostasis
Abstract
:Simple Summary
Abstract
1. Introduction
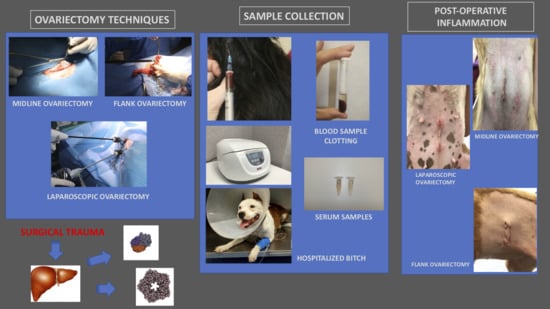
2. Materials and Methods
2.1. Animals
2.2. Study Groups
2.3. Anesthesia and Antibiotic Prophylaxis
2.4. Surgical Procedures
2.5. Blood Sampling
2.6. Statistical Analysis
3. Results
3.1. CRP and Hp
3.2. Alb and PON-1
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Jacobsen, S.; Nielsen, J.V.; Kjelgaard-Hansen, M.; Toelboell, T.; Fjeldborg, J.; Halling-Thomsen, M.; Martinussen, T.; Thoefner, M.B. Acute phase response to surgery of varying intensity in horses: A preliminary study. Vet. Surg. 2009, 38, 762–769. [Google Scholar] [CrossRef] [PubMed]
- Tvarijonaviciute, A.; García-Martínez, J.D.; Caldin, M.; Martínez-Subiela, S.; Tecles, F.; Pastor, J.; Ceron, J.J. Serum paraoxonase 1 (PON1) activity in acute pancreatitis of dogs. J. Small Anim. Pract. 2015, 56, 67–71. [Google Scholar] [CrossRef] [PubMed]
- Gruys, E.; Toussaint, M.J.; Niewold, T.A.; Koopmans, S.J. Acute phase reaction and acute phase proteins. J. Zhejiang Univ. Sci. B 2005, 6, 1045–1056. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cray, C. Acute phase proteins in animals. Prog. Mol. Biol. Transl. Sci. 2012, 105, 113–150. [Google Scholar] [CrossRef]
- Ceron, J.J.; Eckersall, P.D.; Martynez-Subiela, S. Acute phase proteins in dogs and cats: Current knowledge and future perspectives. Vet. Clin. Pathol. 2005, 34, 85–99. [Google Scholar] [CrossRef]
- Murata, H.; Shimada, N.; Yoshioka, M. Current research on acute phase proteins in veterinary diagnosis: An overview. Vet. J. 2004, 168, 28–40. [Google Scholar] [CrossRef]
- Cray, C.; Zaias, J.; Altman, N.H. Acute phase response in animals: A review. Comp. Med. 2009, 59, 517–526. [Google Scholar]
- Martínez-Subiela, S.; Bernal, L.J.; Cerón, J.J. Serum concentrations of acute-phase proteins in dogs with leishmaniosis during short-term treatment. Am. J. Vet. Res. 2003, 64, 1021–1026. [Google Scholar] [CrossRef]
- Yamamoto, S.; Shida, T.; Miyaji, S.; Santsuka, H.; Fujise, H.; Mukawa, K.; Furukawa, E.; Nagae, T.; Naiki, M. Changes in serum C-reactive protein levels in dogs with various disorders and surgical traumas. Vet. Res. Commun. 1993, 17, 85–93. [Google Scholar] [CrossRef]
- Kjelgaard-Hansen, M.; Strom, H.; Mikkelsen, L.F.; Eriksen, T.; Jensen, A.L.; Luntang-Jensen, M. Canine serum C-reactive protein as a quantitative marker of the inflammatory stimulus of aseptic elective soft tissue surgery. Vet. Clin. Pathol. 2013, 42, 342–345. [Google Scholar] [CrossRef]
- Christensen, M.B.; Eriksen, T.; Kjelgaard-Hansen, M. C-reactive protein: Quantitative marker of surgical trauma and post-surgical complications in dogs: A systematic review. Acta Vet. Scand. 2015, 57, 71. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Nevill, B.; Leisewitz, A.; Goddard, A.; Thompson, P. An evaluation of changes over time in serum creatine kinase activity and C-reactive protein concentration in dogs undergoing hemilaminectomy or ovariohysterectomy. J. S. Afr. Vet. Assoc. 2010, 81, 22–26. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zhang, S.X.; Wang, H.B.; Zhang, J.T.; Zhang, N.; Pan, L. Laparoscopic colopexy in dogs. J. Vet. Med. Sci. 2013, 75, 1161–1166. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Dabrowski, R.; Wawron, W.; Kostro, K. Changes in CRP, SAA and haptoglobin produced in response to ovariohysterectomy in healthy bitches and those with pyometra. Theriogenology 2007, 67, 321–327. [Google Scholar] [CrossRef] [PubMed]
- Schmidt, E.M.S.; Rubio, C.P.; Thomas, F.; Ferreira, J.C.P.; Eckersall, D.P. Acute phase proteins in bitches subjected to conventional and minimally invasive ovariohysterectomy. Pesqui. Vet. Bras. 2018, 38, 2124–2128. [Google Scholar] [CrossRef] [Green Version]
- Conceição, M.E.B.A.; Uscategui, R.A.R.; Bertolo, P.H.L.; de Souza, D.C.; Rolemberg, D.D.S.; de Moraes, P.C.; Teixeira, P.P.M.; Dias, L.G.G.G. Assessment of postoperative inflammatory markers and pain in cats after laparoscopy and miniceliotomy ovariectomy. Vet. Rec. 2018, 183, 656. [Google Scholar] [CrossRef]
- Kajikawa, T.; Furuta, A.; Onishi, T.; Tajima, T.; Sugii, S. Changes in concentrations of serum amyloid A protein, alpha 1-acid glycoprotein, haptoglobin, and C-reactive protein in feline sera due to induced inflammation and surgery. Vet. Immunol. Immunopathol. 1999, 68, 91–98. [Google Scholar] [CrossRef]
- Kim, S.; McClave, S.A.; Martindale, R.G.; Miller, K.R.; Hurt, R.T. Hypoalbuminemia and Clinical Outcomes: What is the Mechanism behind the Relationship? Am. Surg. 2017, 83, 1220–1227. [Google Scholar] [CrossRef]
- Daza González, M.A.; Fragío Arnold, C.; Fermín Rodríguez, M.; Checa, R.; Montoya, A.; Portero Fuentes, M.; Rupérez Noguer, C.; Martínez Subiela, S.; Cerón, J.J.; Miró, G. Effect of two treatments on changes in serum acute phase protein concentrations in dogs with clinical leishmaniosis. Vet. J. 2019, 245, 22–28. [Google Scholar] [CrossRef]
- Rossi, G.; Giordano, A.; Pezzia, F.; Kjelgaard-Hansen, M.; Paltrinieri, S. Serum paraoxonase 1 activity in dogs: Preanalytical and analytical factors and correlation with C-reactive protein and alpha-2-globulin. Vet. Clin. Pathol. 2013, 42, 329–341. [Google Scholar] [CrossRef]
- Karnezi, D.; Ceron, J.J.; Theodorou, K.; Leontides, L.; Siarkou, V.I.; Martinez, S.; Tvarijonaviciute, A.; Harrus, S.; Koutinas, C.K.; Pardali, D.; et al. Acute phase protein and antioxidant responses in dogs with experimental acute monocytic ehrlichiosis treated with rifampicin. Vet. Microbiol. 2016, 184, 59–63. [Google Scholar] [CrossRef] [PubMed]
- Motta, S.; Letellier, C.; Ropert, M.; Motta, C.; Thiébault, J.J. Protecting effect of vitamin E supplementation on submaximal exercise-induced oxidative stress in sedentary dogs as assessed by erythrocyte membrane fluidity and paraoxonase-1 activity. Vet. J. 2009, 181, 288–295. [Google Scholar] [CrossRef] [PubMed]
- Bastan, A.; Kanca, H.; Bastan, I.; Salar, S.; Karakas, K.; Alkan, H.; Sel, T. Serum ceruloplasmin and paraoxonase-1 levels in ovariectomized and ovariohysterectomized dogs. Ank. Univ. Vet. Fak. Derg. 2015, 62, 211–215. [Google Scholar] [CrossRef]
- Hiby, E.; Atema, K.N.; Brimley, R.; Hammond-Seaman, A.; Jones, M.; Rowan, A.; Fogelberg, E.; Kennedy, M.; Balaram, D.; Nel, L.; et al. Scoping review of indicators and methods of measurement used to evaluate the impact of dog population management interventions. BMC Vet. Res. 2017, 13, 143. [Google Scholar] [CrossRef] [PubMed]
- Schneider, R.; Dorn, C.R.; Taylor, D.O. Factors influencing canine mammary cancer development and postsurgical survival. J. Natl. Cancer Inst. 1969, 43, 1249–1261. [Google Scholar] [PubMed]
- DeTora, M.; McCarthy, R.J. Ovariohysterectomy versus ovariectomy for elective sterilization of female dogs and cats: Is removal of the uterus necessary? J. Am. Vet. Med. Assoc. 2011, 239, 1409–1412. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Van Goethem, B.; Schaefers-Okkens, A.; Kirpensteijn, J. Making a rational choice between ovariectomy and ovariohysterectomy in the dog: A discussion of the benefits of either technique. Vet. Surg. 2006, 35, 136–143. [Google Scholar] [CrossRef]
- Moldal, E.R.; Kjelgaard-Hansen, M.J.; Peeters, M.E.; Nødtvedt, A.; Kirpensteijn, J. C-reactive protein, glucose and iron concentrations are significantly altered in dogs undergoing open ovariohysterectomy or ovariectomy. Acta Vet. Scand. 2018, 60, 32. [Google Scholar] [CrossRef]
- Howe, L.M. Surgical Methods of Contraception and Sterilization; Elsevier/Texas A&M University: College Station, TX, USA, 2006; Volume 66, pp. 500–509. [Google Scholar]
- Okkens, A.C.; Kooistra, H.S.; Nickel, R.F. Comparison of long-term effects of ovariectomy versus ovariohysterectomy in bitches. J. Reprod. Fertil. Suppl. 1997, 51, 227–231. [Google Scholar]
- Reece, J.F.; Nimesh, M.K.; Wyllie, R.E.; Jones, A.K.; Dennison, A.W. Description and evaluation of a right flank, mini-laparotomy approach to canine ovariohysterectomy. Vet. Rec. 2012, 171, 248. [Google Scholar] [CrossRef]
- McGrath, H.; Hardie, R.J.; Davis, E. Lateral Flank Approach for Ovariohisterctomy in Small Animals. Compendium 2004, 26, 927. [Google Scholar]
- Janssens, L.A.A.; Janssens, G.H.R.R. Bilateral flank ovariectomy in the dog: Surgical technique and sequelae in 72 animals. J. Small Anim. Pract. 1991, 32, 249–252. [Google Scholar] [CrossRef]
- Pukacz, M.; Kienzle, B.; Braun, J. Simple, minimally invasive technique for ovariohysterectomy in the dog. Vet. Rec. 2009, 165, 688–690. [Google Scholar]
- Joshua, J.O. The spaying of immature bitches. Vet. Rec. 1968, 83, 393. [Google Scholar] [CrossRef] [PubMed]
- Mayhew, P. Developing minimally invasive surgery in companion animals. Vet. Rec. 2011, 169, 177–178. [Google Scholar] [CrossRef]
- Culp, W.T.N.; Mayhew, P.D.; Brown, D.C. The effect of laparoscopic versus open ovariectomy on postsurgical activity in small dogs. Vet. Surg. 2009, 38, 811–817. [Google Scholar] [CrossRef]
- Halevy, A.; Lin, G.; Gold-Deutsch, R.; Lavi, R.; Negri, M.; Evans, S.; Cotariu, D.; Sackier, J.M. Comparison of serum C-reactive protein concentrations for laparoscopic versus open cholecystectomy. Surg. Endosc. 1995, 9, 280–282. [Google Scholar] [CrossRef]
- Cassata, G.; Palumbo, V.D.; Cicero, L.; Damiano, G.; Maenza, A.; Migliazzo, A.; Di Paola, G.; Vicari, D.; Fazzotta, S.; Lo Monte, A.I. Laparotomic vs laparoscopic ovariectomy: Comparing the two methods. The ovariectomy in the bitch in laparoscopic era. Acta Biomed. 2017, 87, 271–274. [Google Scholar]
- Devitt, C.M.; Cox, R.E.; Hailey, J.J. Duration, complications, stress, and pain of open ovariohysterectomy versus a simple method of laparoscopic-assisted ovariohysterectomy in dogs. J. Am. Vet. Med. Assoc. 2005, 227, 921–927. [Google Scholar] [CrossRef] [Green Version]
- PGM, A.M.; Moriel, P.; Arthington, J.D. Effects of storage temperature and repeated freeze-thaw cycles on stability of bovine plasma concentrations of haptoglobin and ceruloplasmin. J. Vet. Diagn. Investig. 2017, 29, 738–740. [Google Scholar] [CrossRef]
- Haraguchi, T.; Kimura, S.; Itoh, H.; Nishikawa, S.; Hiyama, M.; Tani, K.; Iseri, T.; Itoh, Y.; Nakaichi, M.; Taura, Y.; et al. Comparison of postoperative pain and inflammation reaction in dogs undergoing preventive laparoscopic-assisted and incisional gastropexy. J. Vet. Med. Sci. 2017, 79, 1524–1531. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Davidson, E.B.; Moll, H.D.; Payton, M.E. Comparison of laparoscopic ovariohysterectomy and ovariohysterectomy in dogs. Vet. Surg. 2004, 33, 62–69. [Google Scholar] [CrossRef] [PubMed]
- Hancock, R.B.; Lanz, O.I.; Waldron, D.R.; Duncan, R.B.; Broadstone, R.V.; Hendrix, P.K. Comparison of postoperative pain after ovariohysterectomy by harmonic scalpel-assisted laparoscopy compared with median celiotomy and ligation in dogs. Vet. Surg. 2005, 34, 273–282. [Google Scholar] [CrossRef] [PubMed]
- Reid, J.; Nolan, A.M.; Scott, E.M. Measuring pain in dogs and cats using structured behavioural observation. Vet. J. 2018, 236, 72–79. [Google Scholar] [CrossRef] [PubMed]
- Pope, J.F.; Knowles, T.G. Retrospective analysis of the learning curve associated with laparoscopic ovariectomy in dogs and associated perioperative complication rates. Vet. Surg. 2014, 43, 668–677. [Google Scholar] [CrossRef]
- Hsueh, C.; Giuffrida, M.; Mayhew, P.D.; Case, J.B.; Singh, A.; Monnet, E.; Holt, D.E.; Cray, M.; Curcillo, C.; Runge, J.J. Evaluation of pet owner preferences for operative sterilization techniques in female dogs within the veterinary community. Vet. Surg. 2018, 47, O15–O25. [Google Scholar] [CrossRef]
- Quandt, J.E. Anesthetic considerations for laser, laparoscopy, and thoracoscopy procedures. Clin. Tech. Small Anim. Pract. 1999, 14, 50–55. [Google Scholar] [CrossRef]
- Russo, A.; Di Stasio, E.; Scagliusi, A.; Bevilacqua, F.; Isgrò, M.A.; Marana, R.; Marana, E. Positive end-expiratory pressure during laparoscopy: Cardiac and respiratory effects. J. Clin. Anesth. 2013, 25, 314–320. [Google Scholar] [CrossRef]
- Donaldson, L.L.; Trostle, S.S.; White, N.A. Cardiopulmonary changes associated with abdominal insufflation of carbon dioxide in mechanically ventilated, dorsally recumbent, halothane anaesthetised horses. Equine Vet. J. 1998, 30, 144–151. [Google Scholar] [CrossRef]
- Almeida, A.V.; Ganem, E.M.; Carraretto, A.R.; Vianna, P.T. Hemodynamic changes during pneumoperitoneum in volume and pressure controlled ventilated dogs. Rev. Bras. Anestesiol. 2003, 53, 756–766. [Google Scholar] [CrossRef] [Green Version]
- Aktas, M.; Vinclair, P.; Lefebvre, H.P.; Toutain, P.L.; Braun, J.P. In vivo quantification of muscle damage in dogs after intramuscular administration of drugs. Br. Vet. J. 1995, 151, 189–196. [Google Scholar] [CrossRef]
- Shin, S.; Na, S.; Kim, O.S.; Choi, Y.S.; Kim, S.H.; Oh, Y.J. Effect of Pneumoperitoneum on Oxidative Stress and Inflammation via the Arginase Pathway in Rats. Yonsei Med. J. 2016, 57, 238–246. [Google Scholar] [CrossRef] [PubMed]
- Stahl, W.M. Acute phase protein response to tissue injury. Crit. Care Med. 1987, 15, 545–550. [Google Scholar] [CrossRef] [PubMed]
- Baigrie, R.J.; Lamont, P.M.; Kwiatkowski, D.; Dallman, M.J.; Morris, P.J. Systemic cytokine response after major surgery. Br. J. Surg. 1992, 79, 757–760. [Google Scholar] [CrossRef] [PubMed]
- Desborough, J.P. The stress response to trauma and surgery. Br. J. Anaesth. 2000, 85, 109–117. [Google Scholar] [CrossRef] [Green Version]
- Schwenk, W.; Jacobi, C.; Mansmann, U.; Böhm, B.; Müller, J.M. Inflammatory response after laparoscopic and conventional colorectal resections-results of a prospective randomized trial. Langenbecks Arch. Surg. 2000, 385, 2–9. [Google Scholar] [CrossRef]
- Serin, G.; Ulutas, P.A. Measurement of serum acute phase proteins to monitor postoperative recovery in anoestrous bitches after ovariohysterectomy. Vet. Rec. 2010, 166, 20–22. [Google Scholar] [CrossRef]
- Dabrowski, R.; Kostro, K.; Lisiecka, U.; Szczubiał, M.; Krakowski, L. Usefulness of C-reactive protein, serum amyloid A component, and haptoglobin determinations in bitches with pyometra for monitoring early post-ovariohysterectomy complications. Theriogenology 2009, 72, 471–476. [Google Scholar] [CrossRef]
- Alves, A.E.; Ribeiro, A.P.C.; Di Filippo, P.A.; Apparicio, M.F.; Fagliari, J.J.; Vicente, W.R.R. Leucogram and serum acute phase protein concentrations in queens submitted to conventional or videolaparoscopic ovariectomy. Arq. Bras. Med. Vet. E Zootec. 2010, 62, 86–91. [Google Scholar] [CrossRef] [Green Version]
- Dabrowski, R.; Wawron, W. Acute-phase response in monitoring postoperative recovery in bitches after ovariohisterectomy. Ann. Anim. Sci. 2014, 14, 287–295. [Google Scholar] [CrossRef] [Green Version]
- Welsch, T.; Müller, S.A.; Ulrich, A.; Kischlat, A.; Hinz, U.; Kienle, P.; Büchler, M.W.; Schmidt, J.; Schmied, B.M. C-reactive protein as early predictor for infectious postoperative complications in rectal surgery. Int. J. Colorectal Dis. 2007, 22, 1499–1507. [Google Scholar] [CrossRef] [PubMed]
- Hirvonen, J.; Pyörälä, S. Acute-phase response in dairy cows with surgically-treated abdominal disorders. Vet. J. 1998, 155, 53–61. [Google Scholar] [CrossRef]
- Peres, C.; Moreira, E.; Junqueira, G.; Feio da Maia, A.; Amaro, T.; Guidio, R.; Barbosa, L. Acute phase response following ovariohysterectomy in female dogs. Comp. Clin. Pathol. 2014, 797–804. [Google Scholar] [CrossRef]
- Freeman, L.J.; Rahmani, E.Y.; Al-Haddad, M.; Sherman, S.; Chiorean, M.V.; Selzer, D.J.; Snyder, P.W.; Constable, P.D. Comparison of pain and postoperative stress in dogs undergoing natural orifice transluminal endoscopic surgery, laparoscopic, and open oophorectomy. Gastrointest. Endosc. 2010, 72, 373–380. [Google Scholar] [CrossRef] [PubMed]
- Mayhew, P.D.; Brown, D.C. Comparison of three techniques for ovarian pedicle hemostasis during laparoscopic-assisted ovariohysterectomy. Vet. Surg. 2007, 36, 541–547. [Google Scholar] [CrossRef]
- Dripps, R.D. New Classification of Physical Status. Anesthesiology 1963, 24, 111. [Google Scholar]
- Milovancev, M.; Townsend, K.L. Current Concepts in Minimally Invasive Surgery of the Abdomen. Vet. Clin. N. Am.-Small Anim. Pract. 2015, 45, 507–522. [Google Scholar] [CrossRef]
- Bula, E.; Upchurch, D.A.; Wang, Y.; Chen, S.; Roccabianca, S. Comparison of tensile strength and time to closure between an intermittent Aberdeen suture pattern and conventional methods of closure for the body wall of dogs. Am. J. Vet. Res. 2018, 79, 115–123. [Google Scholar] [CrossRef]
- Munoz-Prieto, A.; Tvarijonaviciute, A.; Escribano, D.; Martinez-Subiela, S.; Ceron, J.J. Use of heterologous immunoassays for quantification of serum proteins: The case of canine C-reactive protein. PLoS ONE 2017, 12, e0172188. [Google Scholar] [CrossRef]
- Tvarijonaviciute, A.; Tecles, F.; Caldin, M.; Tasca, S.; Cerón, J. Validation of spectrophotometric assays for serum paraoxonase type-1 measurement in dogs. Am. J. Vet. Res. 2012, 73, 34–41. [Google Scholar] [CrossRef]
- Martinez-Subiela, S.; Ceron, J.J. Analytical validation of commercial assays for the determination of haptoglobin, C-reactive protein and serum amyloid A in dogs. Arch. Med. Vet. 2005, 37, 61–66. [Google Scholar] [CrossRef]
- Dąbrowski, R.; Szczubiał, M.; Kostro, K.; Wawron, W.; Ceron, J.J.; Tvarijonaviciute, A. Serum insulin-like growth factor-1 and C-reactive protein concentrations before and after ovariohysterectomy in bitches with pyometra. Theriogenology 2015, 83, 474–477. [Google Scholar] [CrossRef] [PubMed]
- Ribeiro, S.C.; Ribeiro, R.M.; Santos, N.C.; Pinotti, J.A. A randomized study of total abdominal, vaginal and laparoscopic hysterectomy. Int. J. Gynaecol. Obstet. 2003, 83, 37–43. [Google Scholar] [CrossRef]
- Conner, J.G.; Eckersall, P.D.; Ferguson, J.; Douglas, T.A. Acute phase response in the dog following surgical trauma. Res. Vet. Sci. 1988, 45, 107–110. [Google Scholar] [CrossRef]
- Eckersall, P.D. Proteins, Proteomics, and the Dysproteinemias. In Clinical Biochemistry of Domestic Animals, 6th ed.; Kaneko, J.J., Harvey, J.W., Bruss, M.L., Eds.; Clinical Biochemistry of Domestic Animals, Academic Press: Burlington, VT, USA, 2008; pp. 117–155. [Google Scholar]
- Matijatko, V.; Mrljak, V.; Kis, I.; Kucer, N.; Forsek, J.; Zivicnjak, T.; Romić, Z.; Simec, Z.; Ceron, J.J. Evidence of an acute phase response in dogs naturally infected with Babesia canis. Vet. Parasitol. 2007, 144, 242–250. [Google Scholar] [CrossRef]
- Weidmeyer, C.E.; Solter, P.F. Validation of human haptoglobin immunoturbidimetric assay for detection of haptoglobin in equine and canine serum and plasma. Vet. Clin. Pathol. 1996, 25, 141–146. [Google Scholar] [CrossRef]
- Smith, D.J.; Roberts, D. Effects of high volume and/or intense exercise on selected blood chemistry parameters. Clin. Biochem. 1994, 27, 435–440. [Google Scholar] [CrossRef]
- Shariati, E.; Bakhtiari, J.; Khalaj, A.; Niasari-Naslaji, A. Comparison between two portal laparoscopy and open surgery for ovariectomy in dogs. Vet. Res. Forum Int. Q. J. 2014, 5, 219–223. [Google Scholar]
- Lee, M.H.; Ingvertsen, B.T.; Kirpensteijn, J.; Jensen, A.L.; Kristensen, A.T. Quantification of surgical blood loss. Vet. Surg. 2006, 35, 388–393. [Google Scholar] [CrossRef]
- Sammour, T.; Mittal, A.; Loveday, B.P.; Kahokehr, A.; Phillips, A.R.; Windsor, J.A.; Hill, A.G. Systematic review of oxidative stress associated with pneumoperitoneum. Br. J. Surg. 2009, 96, 836–850. [Google Scholar] [CrossRef]
- Demyttenaere, S.; Feldman, L.S.; Fried, G.M. Effect of pneumoperitoneum on renal perfusion and function: A systematic review. Surg. Endosc. 2007, 21, 152–160. [Google Scholar] [CrossRef] [PubMed]
- Mouton, W.G.; Bessell, J.R.; Otten, K.T.; Maddern, G.J. Pain after laparoscopy. Surg. Endosc. 1999, 13, 445–448. [Google Scholar] [CrossRef] [PubMed]
- Volz, J.; Köster, S.; Spacek, Z.; Paweletz, N. Characteristic alterations of the peritoneum after carbon dioxide pneumoperitoneum. Surg. Endosc. 1999, 13, 611–614. [Google Scholar] [CrossRef] [PubMed]
- Mylonakis, M.E.; Ceron, J.J.; Leontides, L.; Siarkou, V.I.; Martinez, S.; Tvarijonaviciute, A.; Koutinas, A.F.; Harrus, S. Serum acute phase proteins as clinical phase indicators and outcome predictors in naturally occurring canine monocytic ehrlichiosis. J. Vet. Intern. Med. 2011, 25, 811–817. [Google Scholar] [CrossRef] [PubMed]
- Shenkin, A.; Fraser, W.D.; Series, J.; Winstanley, F.P.; McCartney, A.C.; Burns, H.J.; Van Damme, J. The serum interleukin 6 response to elective surgery. Lymphokine Res. 1989, 8, 123–127. [Google Scholar] [PubMed]
- Liu, H.F.; Ren, Q.M.; Wang, Z.B.; Li, X.; Jiang, S.; Zhang, J.T.; Wang, H.B. Comparison of acute phase protein and hemodynamic variables in dogs undergoing video-assisted thoracoscopic vs. open pneumonectomy. Exp. Ther. Med. 2017, 13, 2391–2398. [Google Scholar] [CrossRef] [Green Version]
- Michelsen, J.; Heller, J.; Wills, F.; Noble, G.K. Effect of surgeon experience on postoperative plasma cortisol and C-reactive protein concentrations after ovariohysterectomy in the dog: A randomised trial. Aust. Vet. J. 2012, 90, 474–478. [Google Scholar] [CrossRef]
- Heller, M.C.; Johns, J.L. Acute phase proteins in healthy goats: Establishment of reference intervals. J. Vet. Diagn. Investig. 2015, 27, 177–181. [Google Scholar] [CrossRef] [Green Version]
- Miglio, A.; Moscati, L.; Scoccia, E.; Maresca, C.; Antognoni, M.T.; Felici, A. Reference values for serum amyloid A, haptoglobin, lysozyme, zinc and iron in healthy lactating Lacaune sheep. Acta Vet. Scand. 2018, 60, 46. [Google Scholar] [CrossRef] [Green Version]
- Couto, C.G.; Cerón, J.J.; Parra, M.D.; Martínez-Subiela, S.; Iazbik, M.C.; Lazbik, M.C. Acute phase protein concentrations in retired racing Greyhounds. Vet. Clin. Pathol. 2009, 38, 219–223. [Google Scholar] [CrossRef]
- Gomez-Fernandez-Blanco, C.; Peeters, D.; Moyse, E.; Farnir, F.; Höglund, K.; Gouni, V.; Wiberg, M.; Lundgren Willesen, J.; Hanås, S.; McEntee, K.; et al. Interbreed variation of biomarkers of lipid and glucose metabolism in dogs. Vet. Clin. Pathol. 2018, 47, 582–588. [Google Scholar] [CrossRef] [PubMed]
- Kuribayashi, T.; Shimada, T.; Matsumoto, M.; Kawato, K.; Honjyo, T.; Fukuyama, M.; Yamamoto, Y.; Yamamoto, S. Determination of serum C-reactive protein (CRP) in healthy beagle dogs of various ages and pregnant beagle dogs. Exp. Anim. 2003, 52, 387–390. [Google Scholar] [CrossRef] [PubMed] [Green Version]





| Dog | Breed | Dog | Breed | Dog | Breed |
|---|---|---|---|---|---|
| 1 | Crossbreed | 17 | Shih-Tzu | 32 | Podenco |
| 2 | Crossbreed | 18 | Mastiff | 33 | Crossbreed |
| 3 | Crossbreed | 19 | Maltese | 34 | Crossbreed |
| 4 | Crossbreed | 20 | Crossbreed | 35 | Yorkshire terrier |
| 5 | Weimaraner | 21 | Podenco | 36 | Crossbreed |
| 6 | Am Staffordshire | 22 | Am Staffordshire | 37 | Siberian husky |
| 7 | Podenco | 23 | Beagle | 38 | Podenco |
| 8 | Bull Terrier | 24 | Yorkshire terrier | 39 | Crossbreed |
| 9 | Crossbreed | 25 | Jack Russell | 40 | Crossbreed |
| 10 | Spaniel Breton | 26 | Yorkshire terrier | 41 | Crossbreed |
| 11 | Crossbreed | 27 | Crossbreed | 42 | Podenco |
| 12 | Crossbreed | 28 | Crossbreed | 43 | Podenco |
| 13 | Am. Staffordshire | 29 | Podenco | 44 | Mastiff |
| 14 | Pinscher | 30 | Podenco | 45 | Crossbreed |
| 15 | Crossbreed | 31 | Greyhound | 46 | Crossbreed |
| 16 | Crossbreed | 32 | Dachshund |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Del Romero, A.; Cuervo, B.; Peláez, P.; Miguel, L.; Torres, M.; Yeste, M.; Rivera del Alamo, M.M.; Rubio, C.P.; Rubio, M. Changes in Acute Phase Proteins in Bitches after Laparoscopic, Midline, and Flank Ovariectomy Using the Same Method for Hemostasis. Animals 2020, 10, 2223. https://doi.org/10.3390/ani10122223
Del Romero A, Cuervo B, Peláez P, Miguel L, Torres M, Yeste M, Rivera del Alamo MM, Rubio CP, Rubio M. Changes in Acute Phase Proteins in Bitches after Laparoscopic, Midline, and Flank Ovariectomy Using the Same Method for Hemostasis. Animals. 2020; 10(12):2223. https://doi.org/10.3390/ani10122223
Chicago/Turabian StyleDel Romero, Ayla, Belén Cuervo, Pau Peláez, Laura Miguel, Marta Torres, Marc Yeste, Maria Montserrat Rivera del Alamo, Camila P. Rubio, and Mónica Rubio. 2020. "Changes in Acute Phase Proteins in Bitches after Laparoscopic, Midline, and Flank Ovariectomy Using the Same Method for Hemostasis" Animals 10, no. 12: 2223. https://doi.org/10.3390/ani10122223