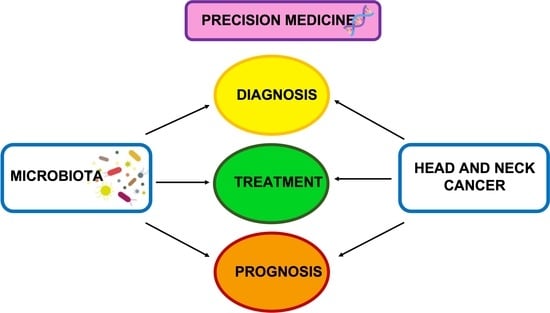
Precision Medicine on the Effects of Microbiota on Head–Neck Diseases and Biomarkers Diagnosis
Abstract
:1. Introduction
2. Materials and Methods
2.1. Protocol and Registration
2.2. Search Processing
2.3. Eligibility Criteria and Study Selection
2.4. Data Processing
2.5. Data Extraction
2.6. Data Analysis
2.7. PICOS Criteria
2.8. Study Evaluation
3. Results
Study Selection and Characteristic
4. Discussion
4.1. Cancer Diagnosis through Biomarkers
4.2. Microbiota and Head and Neck Cancer
4.3. Microbiota and Cancer Treatment
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| AR vs. ARCON | Accelerated radiation with or without carbogen breathing and nicotinamide |
| CTLA-4 | Cytotoxic T-lymphocyte associated protein 4 |
| dTDP-L-rhamnose | Nucleotide sugar precursor |
| GMB | Gut microbiota |
| HIF-1 | Hypoxia-inducible factor 1-alpha |
| HNC | Head and neck cancer |
| HNSCC | Head and neck squamous cell cancer |
| HPV | Human papilloma virus |
| IL-1 | interleukin-1 |
| IL-6 | interleukin-6 |
| LB CD2 | Lactobacillus brevis CD2 |
| LNs | Lymph nodes |
| LPS | Lipopolysaccharides |
| LSCC | Laryngeal squamous cell carcinoma |
| MB | Microbiota |
| miRs | MicroRNAs |
| MM | Microbiome |
| MMP | Matrix metalloproteinases |
| OM | Oral mucositis |
| OC-SCC | oral cavity squamous cell carcinoma |
| OSCC | Oral squamous cell carcinoma of the oral cavity |
| PCR | C-Reactive protein |
| PDL1 | Programmed death ligand 1 |
| PIMO | Pimonidazole |
| PM | Precision medicine |
| PML | Premalignant lesions |
| RCHT | Radio chemotherapy |
| RE | Radiation esophagitis |
| ROS | Reactive oxygen species |
| RNS | Reactive nitrogen species |
| THW | Thyroid hormone withdrawal |
| TM | Translational medicine |
References
- Stark, Z.; Dolman, L.; Manolio, T.A.; Ozenberger, B.; Hill, S.L.; Caulfied, M.J.; Levy, Y.; Glazer, D.; Wilson, J.; Lawler, M.; et al. Integrating Genomics into Healthcare: A Global Responsibility. Am. J. Hum. Genet. 2019, 104, 13–20. [Google Scholar] [CrossRef]
- Chen, Y.; Zhou, J.; Wang, L. Role and Mechanism of Gut Microbiota in Human Disease. Front. Cell. Infect. Microbiol. 2021, 11, 625913. [Google Scholar] [CrossRef] [PubMed]
- Savage, D.C. Microbial Ecology of the Gastrointestinal Tract. Annu. Rev. Microbiol. 1977, 31, 107–133. [Google Scholar] [CrossRef] [PubMed]
- Morrison, D.J.; Preston, T. Formation of Short Chain Fatty Acids by the Gut Microbiota and Their Impact on Human Metabolism. Gut Microbes 2016, 7, 189–200. [Google Scholar] [CrossRef] [PubMed]
- Inchingolo, A.M.; Gargiulo Isacco, C.; Inchingolo, A.D.; Nguyen, K.C.D.; Cantore, S.; Santacroce, L.; Scacco, S.; Cirulli, N.; Corriero, A.; Puntillo, F.; et al. The Human Microbiota Key Role in the Bone Metabolism Activity. Eur. Rev. Med. Pharmacol. Sci. 2023, 27, 2659–2670. [Google Scholar] [CrossRef]
- Ballini, A.; Santacroce, L.; Cantore, S.; Bottalico, L.; Dipalma, G.; Vito, D.D.; Saini, R.; Inchingolo, F. Probiotics Improve Urogenital Health in Women. Open Access Maced. J. Med. Sci. 2018, 6, 1845–1850. [Google Scholar] [CrossRef]
- Ballini, A.; Dipalma, G.; Isacco, C.G.; Boccellino, M.; Di Domenico, M.; Santacroce, L.; Nguyễn, K.C.D.; Scacco, S.; Calvani, M.; Boddi, A.; et al. Oral Microbiota and Immune System Crosstalk: A Translational Research. Biology 2020, 9, 131. [Google Scholar] [CrossRef]
- Corriero, A.; Gadaleta, R.M.; Puntillo, F.; Inchingolo, F.; Moschetta, A.; Brienza, N. The Central Role of the Gut in Intensive Care. Crit. Care 2022, 26, 379. [Google Scholar] [CrossRef]
- Inchingolo, A.D.; Malcangi, G.; Semjonova, A.; Inchingolo, A.M.; Patano, A.; Coloccia, G.; Ceci, S.; Marinelli, G.; Di Pede, C.; Ciocia, A.M.; et al. Oralbiotica/Oralbiotics: The Impact of Oral Microbiota on Dental Health and Demineralization: A Systematic Review of the Literature. Children 2022, 9, 1014. [Google Scholar] [CrossRef]
- European “1+ Million Genomes” Initiative | Shaping Europe’s Digital Future. Available online: https://digital-strategy.ec.europa.eu/en/policies/1-million-genomes (accessed on 24 April 2023).
- Beck, J.D.; Philips, K.; Moss, K.; Divaris, K.; Morelli, T.; Offenbacher, S. Advances in Precision Oral Health. Periodontol. 2000 2020, 82, 268–285. [Google Scholar] [CrossRef]
- Lepage, P.; Häsler, R.; Spehlmann, M.E.; Rehman, A.; Zvirbliene, A.; Begun, A.; Ott, S.; Kupcinskas, L.; Doré, J.; Raedler, A.; et al. Twin Study Indicates Loss of Interaction between Microbiota and Mucosa of Patients with Ulcerative Colitis. Gastroenterology 2011, 141, 227–236. [Google Scholar] [CrossRef] [PubMed]
- Verdam, F.J.; Fuentes, S.; de Jonge, C.; Zoetendal, E.G.; Erbil, R.; Greve, J.W.; Buurman, W.A.; de Vos, W.M.; Rensen, S.S. Human Intestinal Microbiota Composition Is Associated with Local and Systemic Inflammation in Obesity. Obesity 2013, 21, E607–E615. [Google Scholar] [CrossRef] [PubMed]
- Morgan, X.C.; Huttenhower, C. Chapter 12: Human Microbiome Analysis. PLoS Comput. Biol. 2012, 8, e1002808. [Google Scholar] [CrossRef]
- Inchingolo, A.D.; Cazzolla, A.P.; Di Cosola, M.; Greco Lucchina, A.; Santacroce, L.; Charitos, I.A.; Topi, S.; Malcangi, G.; Hazballa, D.; Scarano, A.; et al. The Integumentary System and Its Microbiota between Health and Disease. J. Biol. Regul. Homeost. Agents 2021, 35, 303–321. [Google Scholar] [CrossRef]
- Ballini, A.; Santacroce, L.; Cantore, S.; Bottalico, L.; Dipalma, G.; Topi, S.; Saini, R.; De Vito, D.; Inchingolo, F. Probiotics Efficacy on Oxidative Stress Values in Inflammatory Bowel Disease: A Randomized Double-Blinded Placebo-Controlled Pilot Study. Endocr. Metab. Immune Disord. Drug. Targets 2019, 19, 373–381. [Google Scholar] [CrossRef]
- Diversity, Stability and Resilience of the Human Gut Microbiota | Nature. Available online: https://www.nature.com/articles/nature11550 (accessed on 24 April 2023).
- LaCourse, K.D.; Zepeda-Rivera, M.; Kempchinsky, A.G.; Baryiames, A.; Minot, S.S.; Johnston, C.D.; Bullman, S. The Cancer Chemotherapeutic 5-Fluorouracil Is a Potent Fusobacterium nucleatum Inhibitor and Its Activity Is Modified by Intratumoral Microbiota. Cell Rep. 2022, 41, 111625. [Google Scholar] [CrossRef] [PubMed]
- Kostic, A.D.; Chun, E.; Robertson, L.; Glickman, J.N.; Gallini, C.A.; Michaud, M.; Clancy, T.E.; Chung, D.C.; Lochhead, P.; Hold, G.L.; et al. Fusobacterium nucleatum Potentiates Intestinal Tumorigenesis and Modulates the Tumor-Immune Microenvironment. Cell Host Microbe 2013, 14, 207–215. [Google Scholar] [CrossRef]
- Serna, G.; Ruiz-Pace, F.; Hernando, J.; Alonso, L.; Fasani, R.; Landolfi, S.; Comas, R.; Jimenez, J.; Elez, E.; Bullman, S.; et al. Fusobacterium nucleatum Persistence and Risk of Recurrence after Preoperative Treatment in Locally Advanced Rectal Cancer. Ann. Oncol. 2020, 31, 1366–1375. [Google Scholar] [CrossRef]
- Marchetti, E.; Tecco, S.; Caterini, E.; Casalena, F.; Quinzi, V.; Mattei, A.; Marzo, G. Alcohol-Free Essential Oils Containing Mouthrinse Efficacy on Three-Day Supragingival Plaque Regrowth: A Randomized Crossover Clinical Trial. Trials 2017, 18, 154. [Google Scholar] [CrossRef]
- Baj, J.; Forma, A.; Sitarz, M.; Portincasa, P.; Garruti, G.; Krasowska, D.; Maciejewski, R. Helicobacter pylori Virulence Factors-Mechanisms of Bacterial Pathogenicity in the Gastric Microenvironment. Cells 2020, 10, 27. [Google Scholar] [CrossRef]
- Di Ciaula, A.; Baj, J.; Garruti, G.; Celano, G.; De Angelis, M.; Wang, H.H.; Di Palo, D.M.; Bonfrate, L.; Wang, D.Q.-H.; Portincasa, P. Liver Steatosis, Gut-Liver Axis, Microbiome and Environmental Factors. A Never-Ending Bidirectional Cross-Talk. J. Clin. Med. 2020, 9, 2648. [Google Scholar] [CrossRef] [PubMed]
- Ballini, A.; Gnoni, A.; De Vito, D.; Dipalma, G.; Cantore, S.; Gargiulo Isacco, C.; Saini, R.; Santacroce, L.; Topi, S.; Scarano, A.; et al. Effect of Probiotics on the Occurrence of Nutrition Absorption Capacities in Healthy Children: A Randomized Double-Blinded Placebo-Controlled Pilot Study. Eur. Rev. Med. Pharmacol. Sci. 2019, 23, 8645–8657. [Google Scholar] [CrossRef] [PubMed]
- Zhu, J.; Liao, M.; Yao, Z.; Liang, W.; Li, Q.; Liu, J.; Yang, H.; Ji, Y.; Wei, W.; Tan, A.; et al. Breast Cancer in Postmenopausal Women Is Associated with an Altered Gut Metagenome. Microbiome 2018, 6, 136. [Google Scholar] [CrossRef]
- Signorini, L.; Ballini, A.; Arrigoni, R.; De Leonardis, F.; Saini, R.; Cantore, S.; De Vito, D.; Coscia, M.F.; Dipalma, G.; Santacroce, L.; et al. Evaluation of a Nutraceutical Product with Probiotics, Vitamin D, Plus Banaba Leaf Extracts (Lagerstroemia Speciosa) in Glycemic Control. Endocr. Metab. Immune Disord. Drug Targets 2021, 21, 1356–1365. [Google Scholar] [CrossRef] [PubMed]
- Rajagopala, S.V.; Yooseph, S.; Harkins, D.M.; Moncera, K.J.; Zabokrtsky, K.B.; Torralba, M.G.; Tovchigrechko, A.; Highlander, S.K.; Pieper, R.; Sender, L.; et al. Gastrointestinal Microbial Populations Can Distinguish Pediatric and Adolescent Acute Lymphoblastic Leukemia (ALL) at the Time of Disease Diagnosis. BMC Genom. 2016, 17, 635. [Google Scholar] [CrossRef]
- Farrell, J.J.; Zhang, L.; Zhou, H.; Chia, D.; Elashoff, D.; Akin, D.; Paster, B.J.; Joshipura, K.; Wong, D.T.W. Variations of Oral Microbiota Are Associated with Pancreatic Diseases Including Pancreatic Cancer. Gut 2012, 61, 582–588. [Google Scholar] [CrossRef]
- Karpiński, T.M. Role of Oral Microbiota in Cancer Development. Microorganisms 2019, 7, 20. [Google Scholar] [CrossRef]
- Inchingolo, F.; Santacroce, L.; Cantore, S.; Ballini, A.; Del Prete, R.; Topi, S.; Saini, R.; Dipalma, G.; Arrigoni, R. Probiotics and EpiCor® in Human Health. J. Biol. Regul. Homeost. Agents 2019, 33, 1973–1979. [Google Scholar] [CrossRef]
- Yan, X.; Yang, M.; Liu, J.; Gao, R.; Hu, J.; Li, J.; Zhang, L.; Shi, Y.; Guo, H.; Cheng, J.; et al. Discovery and Validation of Potential Bacterial Biomarkers for Lung Cancer. Am. J. Cancer Res. 2015, 5, 3111–3122. [Google Scholar]
- Bray, F.; Ferlay, J.; Soerjomataram, I.; Siegel, R.L.; Torre, L.A.; Jemal, A. Global Cancer Statistics 2018: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA Cancer J. Clin. 2018, 68, 394–424. [Google Scholar] [CrossRef]
- Yi, M.; Yu, S.; Qin, S.; Liu, Q.; Xu, H.; Zhao, W.; Chu, Q.; Wu, K. Gut Microbiome Modulates Efficacy of Immune Checkpoint Inhibitors. J. Hematol. Oncol. 2018, 11, 47. [Google Scholar] [CrossRef] [PubMed]
- Libonati, A.; Marzo, G.; Klinger, F.G.; Farini, D.; Gallusi, G.; Tecco, S.; Mummolo, S.; De Felici, M.; Campanella, V. Embryotoxicity Assays for Leached Components from Dental Restorative Materials. Reprod. Biol. Endocrinol. 2011, 9, 136. [Google Scholar] [CrossRef]
- Gargiulo Isacco, C.; Ballini, A.; De Vito, D.; Michele Inchingolo, A.; Cantore, S.; Paduanelli, G.; Cao Diem Nguyen, K.; Danilo Inchingolo, A.; Dipalma, G.; Inchingolo, F. Probiotics in Health and Immunity: A First Step toward Understanding the Importance of Microbiota System in Translational Medicine. In Prebiotics and Probiotics—Potential Benefits in Nutrition and Health; Franco-Robles, E., Ramírez-Emiliano, J., Eds.; IntechOpen: London, UK, 2020; ISBN 978-1-78985-921-8. [Google Scholar]
- Tricco, A.C.; Lillie, E.; Zarin, W.; O’Brien, K.K.; Colquhoun, H.; Levac, D.; Moher, D.; Peters, M.D.J.; Horsley, T.; Weeks, L.; et al. PRISMA Extension for Scoping Reviews (PRISMA-ScR): Checklist and Explanation. Ann. Intern. Med. 2018, 169, 467–473. [Google Scholar] [CrossRef]
- Swartz, J.E.; Smits, H.J.G.; Philippens, M.E.P.; de Bree, R.; Kaanders, J.H.A.M.; Willems, S.M. Correlation and Colocalization of HIF-1α and Pimonidazole Staining for Hypoxia in Laryngeal Squamous Cell Carcinomas: A Digital, Single-Cell-Based Analysis. Oral Oncol. 2022, 128, 105862. [Google Scholar] [CrossRef] [PubMed]
- Nagao, T.; Warnakulasuriya, S.; Sakuma, H.; Miyabe, S.; Hasegawa, S.; Machida, J.; Suzuki, K.; Fukano, H.; Shimozato, K.; Hashimoto, S. P53 and Ki67 as Biomarkers in Determining Response to Chemoprevention for Oral Leukoplakia. J. Oral Pathol. Med. 2017, 46, 346–352. [Google Scholar] [CrossRef]
- Ganly, I.; Yang, L.; Giese, R.A.; Hao, Y.; Nossa, C.W.; Morris, L.G.T.; Rosenthal, M.; Migliacci, J.; Kelly, D.; Tseng, W.; et al. Periodontal Pathogens Are a Risk Factor of Oral Cavity Squamous Cell Carcinoma, Independent of Tobacco and Alcohol and Human Papillomavirus. Int. J. Cancer 2019, 145, 775–784. [Google Scholar] [CrossRef] [PubMed]
- Ganly, I.; Pei, Z.; Hao, Y.; Ma, Y.; Rosenthal, M.; Wu, Z.; Migliacci, J.; Huang, B.; Katabi, N.; Tseng, W.; et al. Case Control Study Comparing the HPV Genome in Patients with Oral Cavity Squamous Cell Carcinoma to Normal Patients Using Metagenomic Shotgun Sequencing. Sci. Rep. 2021, 11, 3867. [Google Scholar] [CrossRef]
- Torralba, M.G.; Aleti, G.; Li, W.; Moncera, K.J.; Lin, Y.-H.; Yu, Y.; Masternak, M.M.; Golusinski, W.; Golusinski, P.; Lamperska, K.; et al. Oral Microbial Species and Virulence Factors Associated with Oral Squamous Cell Carcinoma. Microb. Ecol. 2021, 82, 1030–1046. [Google Scholar] [CrossRef]
- Garajei, A.; Allameh, A.; Azadi, M.; Emami, A.; Atashbasteh, M.; Mostafavi, M.; Ghaderi, B.; Inchingolo, F.; Sadeghi, M.; Tadakamadla, S.K.; et al. Evaluation of the Expression Levels of MiR-21-5p and MiR-429 Genes in Biopsy Samples from Patients with Oral Squamous Cell Carcinoma. Diagnostics 2023, 13, 1244. [Google Scholar] [CrossRef]
- Shah, H.; Wang, Y.; Cheng, S.-C.; Gunasti, L.; Chen, Y.-H.; Lako, A.; Guenette, J.; Rodig, S.; Jo, V.Y.; Uppaluri, R.; et al. Use of Fluoro-[18F]-Deoxy-2-D-Glucose Positron Emission Tomography/Computed Tomography to Predict Immunotherapy Treatment Response in Patients With Squamous Cell Oral Cavity Cancers. JAMA Otolaryngol. Head Neck Surg. 2022, 148, 268. [Google Scholar] [CrossRef]
- Hu, Y.; Shao, Z.; Wang, Q.; Jiang, Y.; Ma, R.; Tang, Z.; Liu, Z.; Liang, J.; Huang, Z. Exploring the Dynamic Core Microbiome of Plaque Microbiota during Head-and-Neck Radiotherapy Using Pyrosequencing. PLoS ONE 2013, 8, e56343. [Google Scholar] [CrossRef]
- DE Sanctis, V.; Belgioia, L.; Cante, D.; LA Porta, M.R.; Caspiani, O.; Guarnaccia, R.; Argenone, A.; Muto, P.; Musio, D.; DE Felice, F.; et al. Lactobacillus brevis CD2 for Prevention of Oral Mucositis in Patients with Head and Neck Tumors: A Multicentric Randomized Study. Anticancer Res. 2019, 39, 1935–1942. [Google Scholar] [CrossRef] [PubMed]
- Jiang, C.; Wang, H.; Xia, C.; Dong, Q.; Chen, E.; Qiu, Y.; Su, Y.; Xie, H.; Zeng, L.; Kuang, J.; et al. A Randomized, Double-Blind, Placebo-Controlled Trial of Probiotics to Reduce the Severity of Oral Mucositis Induced by Chemoradiotherapy for Patients with Nasopharyngeal Carcinoma. Cancer 2019, 125, 1081–1090. [Google Scholar] [CrossRef] [PubMed]
- Kageyama, S.; Nagao, Y.; Ma, J.; Asakawa, M.; Yoshida, R.; Takeshita, T.; Hirosue, A.; Yamashita, Y.; Nakayama, H. Compositional Shift of Oral Microbiota Following Surgical Resection of Tongue Cancer. Front. Cell Infect. Microbiol. 2020, 10, 600884. [Google Scholar] [CrossRef]
- Xu, L.; Li, Y.; Sun, S.; Yue, J. Decrease of Oral Microbial Diversity Might Correlate with Radiation Esophagitis in Patients with Esophageal Cancer Undergoing Chemoradiation: A Pilot Study. Precis. Radiat. Oncol. 2020, 4, 81–88. [Google Scholar] [CrossRef]
- Basak, S.K.; Bera, A.; Yoon, A.J.; Morselli, M.; Jeong, C.; Tosevska, A.; Dong, T.S.; Eklund, M.; Russ, E.; Nasser, H.; et al. A Randomized, Phase 1, Placebo-Controlled Trial of APG-157 in Oral Cancer Demonstrates Systemic Absorption and an Inhibitory Effect on Cytokines and Tumor-Associated Microbes. Cancer 2020, 126, 1668–1682. [Google Scholar] [CrossRef]
- Xia, C.; Jiang, C.; Li, W.; Wei, J.; Hong, H.; Li, J.; Feng, L.; Wei, H.; Xin, H.; Chen, T. A Phase II Randomized Clinical Trial and Mechanistic Studies Using Improved Probiotics to Prevent Oral Mucositis Induced by Concurrent Radiotherapy and Chemotherapy in Nasopharyngeal Carcinoma. Front. Immunol. 2021, 12, 618150. [Google Scholar] [CrossRef]
- Galeano Niño, J.L.; Wu, H.; LaCourse, K.D.; Kempchinsky, A.G.; Baryiames, A.; Barber, B.; Futran, N.; Houlton, J.; Sather, C.; Sicinska, E.; et al. Effect of the Intratumoral Microbiota on Spatial and Cellular Heterogeneity in Cancer. Nature 2022, 611, 810–817. [Google Scholar] [CrossRef]
- Lin, B.; Zhao, F.; Liu, Y.; Wu, X.; Feng, J.; Jin, X.; Yan, W.; Guo, X.; Shi, S.; Li, Z.; et al. Randomized Clinical Trial: Probiotics Alleviated Oral-Gut Microbiota Dysbiosis and Thyroid Hormone Withdrawal-Related Complications in Thyroid Cancer Patients Before Radioiodine Therapy Following Thyroidectomy. Front. Endocrinol. 2022, 13, 834674. [Google Scholar] [CrossRef]
- Li, Z.; Fu, R.; Wen, X.; Wang, Q.; Huang, X.; Zhang, L. The Significant Clinical Correlation of the Intratumor Oral Microbiome in Oral Squamous Cell Carcinoma Based on Tissue-Derived Sequencing. Front. Physiol. 2022, 13, 1089539. [Google Scholar] [CrossRef]
- Li, Z.; Chen, G.; Wang, P.; Sun, M.; Zhao, J.; Li, A.; Sun, Q. Alterations of the Oral Microbiota Profiles in Chinese Patient with Oral Cancer. Front. Cell. Infect. Microbiol. 2021, 11, 780067. [Google Scholar] [CrossRef] [PubMed]
- Chan, J.Y.K.; Cheung, M.K.; Lan, L.; Ng, C.; Lau, E.H.L.; Yeung, Z.W.C.; Wong, E.W.Y.; Leung, L.; Qu, X.; Cai, L.; et al. Characterization of Oral Microbiota in HPV and Non-HPV Head and Neck Squamous Cell Carcinoma and Its Association with Patient Outcomes. Oral Oncol. 2022, 135, 106245. [Google Scholar] [CrossRef] [PubMed]
- Zuo, H.-J.; Fu, M.R.; Zhao, H.-L.; Du, X.-W.; Hu, Z.-Y.; Zhao, X.-Y.; Ji, X.-Q.; Feng, X.-Q.; Zhumajiang, W.; Zhou, T.-H.; et al. Study on the Salivary Microbial Alteration of Men with Head and Neck Cancer and Its Relationship With Symptoms in Southwest China. Front. Cell. Infect. Microbiol. 2020, 10, 514943. [Google Scholar] [CrossRef] [PubMed]
- Al-Qadami, G.; Bowen, J.; Van Sebille, Y.; Secombe, K.; Dorraki, M.; Verjans, J.; Wardill, H.; Le, H. Baseline Gut Microbiota Composition Is Associated with Oral Mucositis and Tumour Recurrence in Patients with Head and Neck Cancer: A Pilot Study. Support. Care Cancer 2023, 31, 98. [Google Scholar] [CrossRef] [PubMed]
- Gooi, Z.; Chan, J.Y.K.; Fakhry, C. The Epidemiology of the Human Papillomavirus Related to Oropharyngeal Head and Neck Cancer. Laryngoscope 2016, 126, 894–900. [Google Scholar] [CrossRef]
- Ren, Z.; Li, A.; Jiang, J.; Zhou, L.; Yu, Z.; Lu, H.; Xie, H.; Chen, X.; Shao, L.; Zhang, R.; et al. Gut Microbiome Analysis as a Tool towards Targeted Non-Invasive Biomarkers for Early Hepatocellular Carcinoma. Gut 2019, 68, 1014–1023. [Google Scholar] [CrossRef] [PubMed]
- Fan, X.; Alekseyenko, A.V.; Wu, J.; Peters, B.A.; Jacobs, E.J.; Gapstur, S.M.; Purdue, M.P.; Abnet, C.C.; Stolzenberg-Solomon, R.; Miller, G.; et al. Human Oral Microbiome and Prospective Risk for Pancreatic Cancer: A Population-Based Nested Case-Control Study. Gut 2018, 67, 120–127. [Google Scholar] [CrossRef]
- Ren, Z.; Fan, Y.; Li, A.; Shen, Q.; Wu, J.; Ren, L.; Lu, H.; Ding, S.; Ren, H.; Liu, C.; et al. Alterations of the Human Gut Microbiome in Chronic Kidney Disease. Adv. Sci. 2020, 7, 2001936. [Google Scholar] [CrossRef]
- Reichart, P.A.; Nguyen, X.H. Betel Quid Chewing, Oral Cancer and Other Oral Mucosal Diseases in Vietnam: A Review. J. Oral Pathol. Med. 2008, 37, 511–514. [Google Scholar] [CrossRef]
- Hashibe, M.; Brennan, P.; Chuang, S.-C.; Boccia, S.; Castellsague, X.; Chen, C.; Curado, M.P.; Dal Maso, L.; Daudt, A.W.; Fabianova, E.; et al. Interaction between Tobacco and Alcohol Use and the Risk of Head and Neck Cancer: Pooled Analysis in the International Head and Neck Cancer Epidemiology Consortium. Cancer Epidemiol. Biomarkers Prev. 2009, 18, 541–550. [Google Scholar] [CrossRef]
- Cook, T.J. Blood Dyscrasias as Related to Periodontal Disease; with Special Reference to Leukemia. J. Periodontol. 1947, 18, 159–165. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.; Wang, Y.; Wang, J. A Comprehensive Analysis of Intratumor Microbiome in Head and Neck Squamous Cell Carcinoma. Eur. Arch. Otorhinolaryngol. 2022, 279, 4127–4136. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Y.; Wang, X.; Li, H.; Ni, C.; Du, Z.; Yan, F. Human Oral Microbiota and Its Modulation for Oral Health. Biomed. Pharmacother. 2018, 99, 883–893. [Google Scholar] [CrossRef] [PubMed]
- Chen, Y.; Peng, Y.; Yu, J.; Chen, T.; Wu, Y.; Shi, L.; Li, Q.; Wu, J.; Fu, X. Invasive Fusobacterium nucleatum Activates Beta-Catenin Signaling in Colorectal Cancer via a TLR4/P-PAK1 Cascade. Oncotarget 2017, 8, 31802–31814. [Google Scholar] [CrossRef]
- Wu, Y.; Wu, J.; Chen, T.; Li, Q.; Peng, W.; Li, H.; Tang, X.; Fu, X. Fusobacterium nucleatum Potentiates Intestinal Tumorigenesis in Mice via a Toll-Like Receptor 4/P21-Activated Kinase 1 Cascade. Dig. Dis. Sci. 2018, 63, 1210–1218. [Google Scholar] [CrossRef]
- Cantore, S.; Ballini, A.; De Vito, D.; Abbinante, A.; Altini, V.; Dipalma, G.; Inchingolo, F.; Saini, R. Clinical Results of Improvement in Periodontal Condition by Administration of Oral Probiotics. J. Biol. Regul. Homeost. Agents 2018, 32, 1329–1334. [Google Scholar]
- Choudhari, S.K.; Chaudhary, M.; Gadbail, A.R.; Sharma, A.; Tekade, S. Oxidative and Antioxidative Mechanisms in Oral Cancer and Precancer: A Review. Oral Oncol. 2014, 50, 10–18. [Google Scholar] [CrossRef]
- Campanella, V.; Syed, J.; Santacroce, L.; Saini, R.; Ballini, A.; Inchingolo, F. Oral Probiotics Influence Oral and Respiratory Tract Infections in Pediatric Population: A Randomized Double-Blinded Placebo-Controlled Pilot Study. Eur. Rev. Med. Pharmacol. Sci. 2018, 22, 8034–8041. [Google Scholar] [CrossRef]
- Gholizadeh, P.; Eslami, H.; Yousefi, M.; Asgharzadeh, M.; Aghazadeh, M.; Kafil, H.S. Role of Oral Microbiome on Oral Cancers, a Review. Biomed. Pharmacother. 2016, 84, 552–558. [Google Scholar] [CrossRef]
- Akoglu, G.; Metin, A.; Kilinc, F.; Pektas, S.D.; Isikoglu, S.; Akbas, A.; Sener, S. Total Serum Oxidant/Antioxidant Status and Arylesterase Activity in Recurrent Aphthous Stomatitis. Ann. Dermatol. 2013, 25, 273–277. [Google Scholar] [CrossRef]
- Nejman, D.; Livyatan, I.; Fuks, G.; Gavert, N.; Zwang, Y.; Geller, L.T.; Rotter-Maskowitz, A.; Weiser, R.; Mallel, G.; Gigi, E.; et al. The Human Tumor Microbiome Is Composed of Tumor Type-Specific Intracellular Bacteria. Science 2020, 368, 973–980. [Google Scholar] [CrossRef] [PubMed]
- Poore, G.D.; Kopylova, E.; Zhu, Q.; Carpenter, C.; Fraraccio, S.; Wandro, S.; Kosciolek, T.; Janssen, S.; Metcalf, J.; Song, S.J.; et al. Microbiome Analyses of Blood and Tissues Suggest Cancer Diagnostic Approach. Nature 2020, 579, 567–574. [Google Scholar] [CrossRef] [PubMed]
- Riquelme, E.; Zhang, Y.; Zhang, L.; Montiel, M.; Zoltan, M.; Dong, W.; Quesada, P.; Sahin, I.; Chandra, V.; San Lucas, A.; et al. Tumor Microbiome Diversity and Composition Influence Pancreatic Cancer Outcomes. Cell 2019, 178, 795–806.e12. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.; Yun, M.J.; Nam, K.H.; Chung, W.Y.; Soh, E.-Y.; Park, C.S. Quality of Life and Effectiveness Comparisons of Thyroxine Withdrawal, Triiodothyronine Withdrawal, and Recombinant Thyroid-Stimulating Hormone Administration for Low-Dose Radioiodine Remnant Ablation of Differentiated Thyroid Carcinoma. Thyroid 2010, 20, 173–179. [Google Scholar] [CrossRef] [PubMed]
- Sigal, G.A.; Tavoni, T.M.; Silva, B.M.O.; Kalil Filho, R.; Brandão, L.G.; Maranhão, R.C. Effects of Short-Term Hypothyroidism on the Lipid Transfer to High-Density Lipoprotein and Other Parameters Related to Lipoprotein Metabolism in Patients Submitted to Thyroidectomy for Thyroid Cancer. Thyroid 2019, 29, 53–58. [Google Scholar] [CrossRef]
- Singh, R.; Tandon, A.; Gupta, S.K.; Saroja, K. Optimal Levothyroxine Replacement Adequately Improves Symptoms of Hypothyroidism; Residual Symptoms Need Further Evaluation for Other than Hypothyroidism Causation. Indian J. Endocrinol. Metab. 2017, 21, 830–835. [Google Scholar] [CrossRef]
- Microbiota in Health and Diseases | Signal Transduction and Targeted Therapy. Available online: https://www.nature.com/articles/s41392-022-00974-4 (accessed on 17 April 2023).
- Roy, S.; Trinchieri, G. Microbiota: A Key Orchestrator of Cancer Therapy. Nat. Rev. Cancer 2017, 17, 271–285. [Google Scholar] [CrossRef]
- Iida, N.; Dzutsev, A.; Stewart, C.A.; Smith, L.; Bouladoux, N.; Weingarten, R.A.; Molina, D.A.; Salcedo, R.; Back, T.; Cramer, S.; et al. Commensal Bacteria Control Cancer Response to Therapy by Modulating the Tumor Microenvironment. Science 2013, 342, 967–970. [Google Scholar] [CrossRef]
- Couzin-Frankel, J. Breakthrough of the Year 2013. Cancer Immunotherapy. Science 2013, 342, 1432–1433. [Google Scholar] [CrossRef]
- Perez-Chanona, E.; Trinchieri, G. The Role of Microbiota in Cancer Therapy. Curr. Opin. Immunol. 2016, 39, 75–81. [Google Scholar] [CrossRef]
- Si, W.; Liang, H.; Bugno, J.; Xu, Q.; Ding, X.; Yang, K.; Fu, Y.; Weichselbaum, R.R.; Zhao, X.; Wang, L. Lactobacillus rhamnosus GG Induces CGAS/STING- Dependent Type I Interferon and Improves Response to Immune Checkpoint Blockade. Gut 2022, 71, 521–533. [Google Scholar] [CrossRef] [PubMed]
- Vétizou, M.; Pitt, J.M.; Daillère, R.; Lepage, P.; Waldschmitt, N.; Flament, C.; Rusakiewicz, S.; Routy, B.; Roberti, M.P.; Duong, C.P.M.; et al. Anticancer Immunotherapy by CTLA-4 Blockade Relies on the Gut Microbiota. Science 2015, 350, 1079–1084. [Google Scholar] [CrossRef] [PubMed]
- Boven, L.; Holmes, S.P.; Latimer, B.; McMartin, K.; Ma, X.; Moore-Medlin, T.; Khandelwal, A.R.; McLarty, J.; Nathan, C.-A.O. Curcumin Gum Formulation for Prevention of Oral Cavity Head and Neck Squamous Cell Carcinoma. Laryngoscope 2019, 129, 1597–1603. [Google Scholar] [CrossRef] [PubMed]
- Purcell, R.V.; Pearson, J.; Aitchison, A.; Dixon, L.; Frizelle, F.A.; Keenan, J.I. Colonization with Enterotoxigenic Bacteroides Fragilis Is Associated with Early-Stage Colorectal Neoplasia. PLoS ONE 2017, 12, e0171602. [Google Scholar] [CrossRef]
- Fessler, J.; Matson, V.; Gajewski, T.F. Exploring the Emerging Role of the Microbiome in Cancer Immunotherapy. J. Immunother. Cancer 2019, 7, 108. [Google Scholar] [CrossRef]
- Assessment of Post-Radiotherapy Salivary Glands—PMC. Available online: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3473647/ (accessed on 24 April 2023).
- Eggermont, A.M.M.; Maio, M.; Robert, C. Immune Checkpoint Inhibitors in Melanoma Provide the Cornerstones for Curative Therapies. Semin. Oncol. 2015, 42, 429–435. [Google Scholar] [CrossRef]
- Topalian, S.L.; Wolchok, J.D.; Chan, T.A.; Mellman, I.; Palucka, K.; Banchereau, J.; Rosenberg, S.A.; Dane Wittrup, K. Immunotherapy: The Path to Win the War on Cancer? Cell 2015, 161, 185–186. [Google Scholar] [CrossRef]
- Shih, A.; Miaskowski, C.; Dodd, M.J.; Stotts, N.A.; MacPhail, L. Mechanisms for Radiation-Induced Oral Mucositis and the Consequences. Cancer Nurs. 2003, 26, 222–229. [Google Scholar] [CrossRef]
- Ionizing Radiation-Induced DNA Damage Response Identified in Marine mussels, Mytilus Sp—PubMed. Available online: https://pubmed.ncbi.nlm.nih.gov/22609861/ (accessed on 24 April 2023).
- Lalla, R.V.; Brennan, M.T.; Gordon, S.M.; Sonis, S.T.; Rosenthal, D.I.; Keefe, D.M. Oral Mucositis Due to High-Dose Chemotherapy and/or Head and Neck Radiation Therapy. J. Natl. Cancer Inst. Monogr. 2019, 2019, lgz011. [Google Scholar] [CrossRef]
- Mucositis Incidence, Severity and Associated Outcomes in Patients with Head and Neck Cancer Receiving Radiotherapy with or without Chemotherapy: A Systematic Literature Review—PubMed. Available online: https://pubmed.ncbi.nlm.nih.gov/12742264/ (accessed on 24 April 2023).
- Xiao, L.; Zhang, Q.; Peng, Y.; Wang, D.; Liu, Y. The Effect of Periodontal Bacteria Infection on Incidence and Prognosis of Cancer. Medicine 2020, 99, e19698. [Google Scholar] [CrossRef]
- Sharma, A.; Rath, G.K.; Chaudhary, S.P.; Thakar, A.; Mohanti, B.K.; Bahadur, S. Lactobacillus brevis CD2 Lozenges Reduce Radiation- and Chemotherapy-Induced Mucositis in Patients with Head and Neck Cancer: A Randomized Double-Blind Placebo-Controlled Study. Eur. J. Cancer 2012, 48, 875–881. [Google Scholar] [CrossRef] [PubMed]
- The Host Microbiome Regulates and Maintains Human Health: A Primer and Perspective for Non-Microbiologists—PMC. Available online: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5392374/ (accessed on 24 April 2023).




| Criteria | Application in the Present Study |
|---|---|
| Population | Subjects diagnosed with head–neck tumors and potentially malignant lesions |
| Intervention | Use of cancer biomarkers. Supplementation with probiotics or prebiotics or symbiotic |
| Comparisons | Comparing before and post cancer intervention MB, MM assessment determined by 16 s rRNA sequencing, Mann–Whitney test on cancer biomarkers: fluorodeoxyglucose-positron emission tomography (FDG-PET/CT) scans |
| Outcomes | Changes in baseline and end in symptom measurements. Changes in MB composition due to the presence of cancer or after cancer treatments |
| Study design | Clinical Trials |
| Authors | Study Type | Aim of the Study | Materials and Methods | Results |
|---|---|---|---|---|
| Swartz et al., 2022 [37] | Case-control Study | Tumor hypoxia compromises local control and patient survival. We used a digital, single-cell analysis to compare two hypoxia biomarkers (hypoxia-inducible factor 1-alpha [HIF-1] and pimonidazole [PIMO]) and their effect on outcome in patients with laryngeal cancer who received accelerated radiotherapy with or without carbogen breathing and nicotinamide (AR versus ARCON). | HIF-1 and PIMO immunohistochemical labeling were carried out in successive sections of 44 laryngeal carcinoma patients randomized between AR and ARCON. HIF-1 expression and PIMO-binding were associated in QuPath utilizing digital image analysis. Each biomarker’s high-density regions were automatically identified, and staining overlap was examined. For each biomarker, Kaplan–Meier survival analyses for local control, regional control, and disease-free survival were performed to predict a response advantage of ARCON over AR alone. | In total, 106 tissue pieces from 44 individuals were examined. On the fragment level, a weak but significant positive connection was found between HIF-1 and PIMO positivity, but not at the patient level. The number of high-density staining patches for both biomarkers showed a moderately strong connection (r = 0.705, p = 0.001). The staining overlap was inadequate. ARCON’s response benefit over AR could not be predicted by HIF-1 expression, PIMO-binding, or a combination of the two. |
| Nagao et al., 2017 [38] | Randomized Controlled Trial | The goal of this study was to see if there were any variations in baseline p53 and ki67 expression between those who responded and those who did not react to our intervention. A secondary goal was to determine whether there was a link between dietary parameters and clinical responses. | We included all nonsmokers in the experimental group (n = 23) for this biomarker investigation. At the 1-year follow-up, there were four responders and 12 non-responders among the 16 who completed the experiment for one year of supplementation. Following p53 and ki67 immunostaining, the proportion of positive cell nuclei was calculated as the labeling index (LI). | The expression of p53 was higher in the basal layers than in the para-basal layers. Non-responsive subjects had a greater mean para-basal LI of p53 (26.0) than responding subjects (11.2) (p = 0.028). The ki67 LIs in the two groups were not substantially different. |
| Ganly et al., 2019 [39] | Case-control Study | The goal of this study was to see if the oral was linked to OC-SCC in nonsmokers with HPV negative. We investigated the oral MMs of HPV-negative nonsmokers with OC-SCC (n = 18), premalignant lesions (n = 8), and healthy controls (n = 12). | Their oral MB was obtained using an oral wash and characterized using 16S rRNA gene sequencing. | In OC-SCC, the periodontal pathogens Fusobacterium, Prevotella, and Alloprevotella were abundant, but commensal Streptococcus was decreased. We divided the oral MM into two categories based on the four species plus a marker genus Veillonella for PML. |
| Ganly et al., 2021 [40] | Case-control Study | The goal of this study was to use metagenomic shotgun sequencing to compare the HPV genome in patients with oral cavity squamous cell carcinoma (OCSCC) to normal people. | They gathered 50 OCSCC patients and compared them with a control patient based on age, gender, race, smoking status, and alcohol status. All patients’ DNA was collected from oral wash samples and full genome shotgun sequencing was carried out. The raw sequencing data was cleaned, reads were matched with the human genome (GRCH38), nonhuman reads were detected, and HPV genotypes were determined using HPViewer. The tongue was the most prevalent subsite in 26 (52% of the 50 individuals with OCSCC). Primary resection and neck dissection were performed in all patients. | p16 immunohistochemistry was negative in all but two tumors. In terms of gender, age, race/ethnicity, alcohol use, and cigarette smoking, there were no statistically significant differences between the cases and controls. In the nonhuman DNA readings, there was no statistically significant difference between the cancer samples and the control samples. HPV was found in 5 instances (10%) of OCSCC (genotypes 10, 16, and 98), although only 1 tumor sample (genotype 16) produced enough reads to imply an involvement in the genesis of OCSCC. HPV was found in four healthy people, however each had just 1–2 HPV readings per human genome. HPV genotypes are uncommon in patients with oral cancer. |
| Torralba et al., 2021 [41] | Prospective Observational Study | To elucidate the links between the oral MB and cancer virulence factors | They employed 16S rDNA and metagenomic sequencing to evaluate the microbial makeup and functional content of 18 OSCC patients’ tumor tissue, non-tumor tissue, and saliva. | When compared with all other sample categories, the results show a larger number of bacteria from the phyla Fusobacteria, Bacteroidetes, and Firmicutes linked with tumor tissue. Furthermore, saliva metaproteomics indicated a substantial rise in Prevotella in five OSCC patients, whereas Corynebacterium was predominantly related to 10 healthy patients. Finally, we discovered adhesion and virulence factors linked with Streptococcus gordonii as well as recognized oral pathogens belonging to the Fusobacterium genera, which were primarily detected in OSCC tissues. |
| Garajei et al., 2023 [42] | Case-control Study | This study compares the expression of the miR-21-5p and miR-429 genes in biopsy samples from patients with OSCC to that of controls. | Tissue samples were collected from 40 people (20 OSCC patients and 20 healthy controls) and analyzed using the Mann–Whitney test to evaluate miR-21-5p and miR-429 expression. | The individuals in the control and sick groups were 47.15 and 53.8 years old, respectively. The Mann–Whitney test revealed significant differences in miR-21-5p (p = 0.0001) and miR-429 (p = 0.0191) expression levels between the two groups (p = 0.05). |
| Shah et al., 2022 [43] | A retrospective study of serial FDG-PET/CT scans collected prospectively as part of a phase 2 open-label randomized clinical trial examining neoadjuvant immunotherapy in patients with untreated OCSCC between 2016 and 2019 was performed. | To connect variations in fluoro-[18F]FDG-PET/CT scans with primary tumor pathologic response and immunologic biomarkers in patients with OCSCC undergoing neoadjuvant immunotherapy. | In total, 29 patients with untreated OCSCC (T2, or clinically node positive) from a single academic medical center were randomized 1:1 to receive neoadjuvant therapy with single agent nivolumab or combination nivolumab and ipilimumab, followed by surgery and standard of care adjuvant therapy. FDG-PET/CT scans were performed before (T0) and after (T1) preoperative immunotherapy in this investigation. | There was no relationship between pathologic response and SUVmax change in primary OCSCC between T0 and T1. Thirteen of the 27 subjects had newly FDG-avid ipsilateral LNs at T1, with the majority being pathologically negative. A total of 9 patients experienced radiologic irAEs, the most frequent of which was sarcoid-like LN (7 of 27). There were no relationships between primary OCSCC SUVmax at T0 and CD8+ T-cell number in the main tumor biopsy, and there were no associations between primary OCSCC SUVmax at T1 and CD8+ T-cell number in the original tumor during surgery. |
| Hu et al., 2013 [44] | Prospective study | The purpose is to investigate the dynamic core microbiome of oral microbiota in supragingival plaque during head-and-neck radiation. | Dental plaque samples were collected from 8 subjects before and during radiotherapy. | During radiation, 4 phyla and 11 genera were detected, validating the hypothesis of a core microbiome. |
| De Sanctis et al., 2019 [45] | Clinical Trial | To evaluate the effect of lactobacillus brevis CD2 (LB CD2) in preventing oral mucositis in patients with head and neck cancers (HNC). | In total, 75 patients were included to receive either LB CD2 lozenges or a mouthwash routine with sodium bicarbonate. | The trial failed to establish the effectiveness of LB CD2 in reducing radiotherapy-induced OM. |
| Jiang et al., 2019 [46] | Randomized Controlled Trial | Probiotics will be used to decrease the severity of OM caused by chemoradiotherapy in patients with nasopharyngeal cancer. | During radiotherapy, 99 patients were randomly randomized to receive a probiotic or a placebo. | The gravity of OM was significantly reduced in those who took the probiotic combination. |
| Kageyama et al., 2020 [47] | Prospective study | To evaluate the compositional shift of oral microbiota after surgical resection of tongue cancer. | Saliva samples were collected from 25 tongue cancer patients before and after resection of the tongue. Quantitative PCR analysis and 16S ribosomal RNA (rRNA) gene sequencing were used to determine bacterial density and composition. | The surgical resection of the tongue caused a shift in the structure of the salivary microbiota, with an increase in bacterial species from dental plaque, especially periodontal pathogens. |
| Xu et al., 2020 [48] | Pilot study | The objective is to examine the relationship between oral bacterial variety and radiation esophagitis in chemoradiotherapy patients with esophageal cancer. | Oral mucosal swabs were obtained from 10 patients who did not have RE, 11 patients who had grade 1 RE, and 10 patients who had grade 2 RE. The diversity of oral bacteria was measured using 16S rRNA gene sequencing. | In patients with esophageal cancer following chemoradiotherapy, a reduction in oral bacterial diversity may be associated with RE. |
| Basak et al., 2020 [49] | Randomized Controlled Trial | The purpose of this research is to evaluate the effect of APG-157 on cytokines and microbiota. | APG-157 was given to 13 healthy people and 12 patients with oral cancer. Blood and saliva samples were collected before, 1, 2, 3, and 24 h after therapy. | This study shows that APG-157 is a strategic therapy combined with immunotherapy in cancer. |
| Xia et al., 2021 [50] | Randomized Clinical Trial | The purpose is to use Probiotics to prevent radiochemotherapy-induced OM in patients with nasopharyngeal carcinoma. | In total, 77 individuals were chosen and randomly selected to receive either a probiotic cocktail or a placebo. After 7, 14, and 21 days, tongue, blood, fecal, and proximal colon tissue samples were examined. | The improved probiotic cocktail considerably decreases the severity of OM by improving patients’ immune responses and changing the composition of their gut microbiota. |
| Niño et al., 2022 [51] | Observational study | To evaluate the effect of the intratumoral microbiome on cancer spatial and cellular heterogeneity. | Spatial profiling and single-cell RNA sequencing are used in situ to identify cellular, molecular, and spacial host-microbe interactions. | Inside a tumor, the microbiota is well structured in microniches with immune and epithelial cell activities that support cancer growth. |
| Lin et al., 2022 [52] | Randomized Clinical Trial | To assess the oral-gut microbiota profiles of THW patients and then see if probiotics can help with THW-related problems. | In total, 50 thyroid cancer patients were randomly randomized to receive probiotics or a placebo during thyroidectomy. | Probiotics significantly improved gut and oral microbial diversity and reduced thyroid hormone withdrawal-related problems in thyroid cancer patients prior to radioiodine treatment after thyroidectomy. |
| Li et al., 2023 [53] | Observational study | Based on tissue sequencing, this study intends to assess the clinical association of the intratumoral oral microbiome in oral squamous cell cancer. | The oral microbiota was analyzed in 133 OSCC samples to assess its composition compared with healthy patients and also determine its diagnostic and prognostic value. | Differences in bacterial composition have been found between the oral microbiota in OSCC and healthy patients, and only some of these bacteria can be used as diagnostic and prognostic predictors. |
| Li, Z. et al., 2021 [54] | Prospective study | To assess the prevalence and distribution of the oral microbiota in oral cancer patients, populations without precancerous lesions, and healthy individuals. To assess the connection between oral cancer incidence and the microbiome of oral bacteria. | In total, 10 patients who had been diagnosed with oral cancer, 10 healthy subjects and 6 patients with oral precancerous lesions were enrolled. Salivary samples were collected from these patients and the microbiome was analyzed | At many species levels, there were significant structural alterations in the oral microbiota of patients with oral cancer, patients with precancerous lesions, and healthy controls. Some metabolic pathways are altered by dysbiosis of the oral microbiota, which has an impact on oral health. |
| Chan, J.Y.K. et al., 2022 [55] | Prospective cohort study | The purpose of the study is to understand the correlation between oral microbiome, HPV infection, conventional risk factors, and head and neck squamous cell cancer (HNSCC). | By sequencing 16S rRNA V3-V4 bacterial and HPV L1 sections, respectively, the oral microbiota and HPV infection of tissues of 166 Chinese people were analyzed. the relationship between oral microbiota, HPV and clinical features was analyzed. | It is inferred that dysbiosis of the oral microbiota is involved in the pathogenesis of OSCC. Fusobacterium is involved in improving outcomes of patients with OSCC, especially in patients without traditional risk factors. Understanding how the oral microbiome, HPV infection, and other risk factors for HNSCC interact will be crucial to understanding the pathophysiology of this disease. |
| Zuo, H.-J. et al., 2020 [56] | Prospective study | In this study, oral microbial traits and new biomarkers will be assessed for HNC patients, and the relationship between oral microorganisms and HNC-related symptoms will be evaluated prior to surgical intervention. | Overall, 56 patients with HNC and 64 healthy controls were recruited. Salivary samples were taken in order to do 16S rRNA gene sequencing on the microbes. | A decrease in health-related bacteria, such as Peptococcus, and a rise in potentially pathogenic bacteria, such as Capnocytophaga and other LPS-producing bacteria such as Neisseria, were seen in the oral microbiome of HNC patients. Additionally, HNC-related symptoms in conjunction with salivary microorganisms such as Capnocytophaga may be employed as a noninvasive technique for screening, identification, and treatment monitoring of HNC. |
| Al-Qadami, G. et al., 2023 [57] | Prospective pilot study | To assess the relationships between a patient’s pre-treatment gut flora and the severity of radiotherapy-induced oral mucositis (OM) and recurrence risk in those with head and neck cancer (HNC). | Patients who were scheduled to receive radiotherapy or chemoradiotherapy for HNC were enrolled in this trial. Before therapy, stool samples were taken, and 16S rRNA gene sequencing was used to analyze the microbial composition. | OM severity and recurrence risk are related to a patient’s gut microbiota makeup at the beginning of therapy. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Inchingolo, A.M.; Malcangi, G.; Piras, F.; Palmieri, G.; Settanni, V.; Riccaldo, L.; Morolla, R.; Buongiorno, S.; de Ruvo, E.; Inchingolo, A.D.; et al. Precision Medicine on the Effects of Microbiota on Head–Neck Diseases and Biomarkers Diagnosis. J. Pers. Med. 2023, 13, 933. https://doi.org/10.3390/jpm13060933
Inchingolo AM, Malcangi G, Piras F, Palmieri G, Settanni V, Riccaldo L, Morolla R, Buongiorno S, de Ruvo E, Inchingolo AD, et al. Precision Medicine on the Effects of Microbiota on Head–Neck Diseases and Biomarkers Diagnosis. Journal of Personalized Medicine. 2023; 13(6):933. https://doi.org/10.3390/jpm13060933
Chicago/Turabian StyleInchingolo, Angelo Michele, Giuseppina Malcangi, Fabio Piras, Giulia Palmieri, Vito Settanni, Lilla Riccaldo, Roberta Morolla, Silvio Buongiorno, Elisabetta de Ruvo, Alessio Danilo Inchingolo, and et al. 2023. "Precision Medicine on the Effects of Microbiota on Head–Neck Diseases and Biomarkers Diagnosis" Journal of Personalized Medicine 13, no. 6: 933. https://doi.org/10.3390/jpm13060933