Angiographic Features and Clinical Outcomes of Balloon Uncrossable Lesions during Chronic Total Occlusion Percutaneous Coronary Intervention
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Population
2.2. Definitions
2.3. Outcomes
2.4. Statistics
3. Results
4. Discussion
5. Study Limitations
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Patel, S.M.; Pokala, N.R.; Menon, R.V.; Kotsia, A.P.; Raja, V.; Christopoulos, G.; Michael, T.T.; Rangan, B.V.; Sherbet, D.; Patel, V.G.; et al. Prevalence and treatment of "balloon-uncrossable" coronary chronic total occlusions. J. Invasive. Cardiol. 2015, 27, 78–84. [Google Scholar]
- Karacsonyi, J.; Karmpaliotis, D.; Alaswad, K.; Jaffer, F.A.; Yeh, R.W.; Patel, M.; Bahadorani, J.; Doing, A.; Ali, Z.A.; Karatasakis, A.; et al. Prevalence, indications and management of balloon uncrossable chronic total occlusions: Insights from a contemporary multicenter US registry. Catheter. Cardiovasc. Interv. 2017, 90, 12–20. [Google Scholar] [CrossRef]
- Elrayes, M.M.; Xenogiannis, I.; Nikolakopoulos, I.; Vemmou, E.; Wollmuth, J.; Abi Rafeh, N.; Karmpaliotis, D.; Gasparini, G.L.; Burke, M.N.; Brilakis, E.S. An algorithmic approach to balloon-uncrossable coronary lesions. Catheter. Cardiovasc. Interv. 2021, 97, E817–E825. [Google Scholar] [CrossRef] [PubMed]
- Karacsonyi, J.; Alaswad, K.; Choi, J.W.; Vemmou, E.; Nikolakopoulos, I.; Poommipanit, P.; Rafeh, N.A.; ElGuindy, A.; Ungi, I.; Egred, M.; et al. Laser for balloon uncrossable and undilatable chronic total occlusion interventions. Int. J. Cardiol. 2021, 336, 33–37. [Google Scholar] [CrossRef]
- Karacsonyi, J.; Deffenbacher, K.; Benzuly, K.H.; Flaherty, J.D.; Alaswad, K.; Basir, M.; Megaly, M.S.; Jaffer, F.; Doshi, D.; Poommipanit, P.; et al. Use of Mechanical Circulatory Support in Chronic Total Occlusion Percutaneous Coronary Intervention. Am. J. Cardiol. 2023, 189, 76–85. [Google Scholar] [CrossRef] [PubMed]
- Kostantinis, S.; Simsek, B.; Karacsonyi, J.; Alaswad, K.; Krestyaninov, O.; Khelimskii, D.; Karmpaliotis, D.; Jaffer, F.A.; Khatri, J.J.; Poommipanit, P.; et al. In-hospital outcomes and temporal trends of percutaneous coronary interventions for chronic total occlusion. EuroIntervention 2022, 18, e929–e932. [Google Scholar] [CrossRef] [PubMed]
- Kostantinis, S.; Simsek, B.; Karacsonyi, J.; Davies, R.E.; Benton, S.; Nicholson, W.; Rinfret, S.; Jaber, W.A.; Raj, L.; Sandesara, P.B.; et al. Intravascular lithotripsy in chronic total occlusion percutaneous coronary intervention: Insights from the PROGRESS-CTO registry. Catheter. Cardiovasc. Interv. 2022, 100, 512–519. [Google Scholar] [CrossRef]
- Harris, P.A.; Taylor, R.; Minor, B.L.; Elliott, V.; Fernandez, M.; O’Neal, L.; McLeod, L.; Delacqua, G.; Delacqua, F.; Kirby, J.; et al. The REDCap consortium: Building an international community of software platform partners. J. Biomed. Inform. 2019, 95, 103208. [Google Scholar] [CrossRef]
- Harris, P.A.; Taylor, R.; Thielke, R.; Payne, J.; Gonzalez, N.; Conde, J.G. Research electronic data capture (REDCap)—A metadata-driven methodology and workflow process for providing translational research informatics support. J. Biomed. Inform. 2009, 42, 377–381. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Thygesen, K.; Alpert, J.S.; Jaffe, A.S.; Simoons, M.L.; Chaitman, B.R.; White, H.D.; Joint ESC/ACCF/AHA/WHF Task Force for the Universal Definition of Myocardial Infarction; Katus, H.A.; Lindahl, B.; Morrow, D.A.; et al. Third universal definition of myocardial infarction. Circulation 2012, 126, 2020–2035. [Google Scholar] [CrossRef] [Green Version]
- Morino, Y.; Abe, M.; Morimoto, T.; Kimura, T.; Hayashi, Y.; Muramatsu, T.; Ochiai, M.; Noguchi, Y.; Kato, K.; Shibata, Y.; et al. Predicting successful guidewire crossing through chronic total occlusion of native coronary lesions within 30 minutes: The J-CTO (Multicenter CTO Registry in Japan) score as a difficulty grading and time assessment tool. JACC Cardiovasc. Interv. 2011, 4, 213–221. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Christopoulos, G.; Kandzari, D.E.; Yeh, R.W.; Jaffer, F.A.; Karmpaliotis, D.; Wyman, M.R.; Alaswad, K.; Lombardi, W.; Grantham, J.A.; Moses, J.; et al. Development and Validation of a Novel Scoring System for Predicting Technical Success of Chronic Total Occlusion Percutaneous Coronary Interventions: The PROGRESS CTO (Prospective Global Registry for the Study of Chronic Total Occlusion Intervention) Score. JACC Cardiovasc. Interv. 2016, 9, 1–9. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Simsek, B.; Kostantinis, S.; Karacsonyi, J.; Alaswad, K.; Krestyaninov, O.; Khelimskii, D.; Davies, R.; Rier, J.; Goktekin, O.; Gorgulu, S.; et al. Predicting Periprocedural Complications in Chronic Total Occlusion Percutaneous Coronary Intervention: The PROGRESS-CTO Complication Scores. JACC Cardiovasc. Interv. 2022, 15, 1413–1422. [Google Scholar] [CrossRef]
- Simsek, B.; Kostantinis, S.; Karacsonyi, J.; Alaswad, K.; Karmpaliotis, D.; Masoumi, A.; Jaffer, F.A.; Doshi, D.; Khatri, J.; Poommipanit, P.; et al. Prevalence and outcomes of balloon undilatable chronic total occlusions: Insights from the PROGRESS-CTO. Int. J. Cardiol. 2022, 362, 42–46. [Google Scholar] [CrossRef]
- Kovacic, J.C.; Sharma, A.B.; Roy, S.; Li, J.R.; Narayan, R.; Kim, D.B.; Sharma, S.K.; Kini, A.S. GuideLiner mother-and-child guide catheter extension: A simple adjunctive tool in PCI for balloon uncrossable chronic total occlusions. J. Interv. Cardiol. 2013, 26, 343–350. [Google Scholar] [CrossRef]
- Pagnotta, P.; Briguori, C.; Mango, R.; Visconti, G.; Focaccio, A.; Belli, G.; Presbitero, P. Rotational atherectomy in resistant chronic total occlusions. Catheter. Cardiovasc. Interv. 2010, 76, 366–371. [Google Scholar] [CrossRef]
- Fernandez, J.P.; Hobson, A.R.; McKenzie, D.; Shah, N.; Sinha, M.K.; Wells, T.A.; Levy, T.M.; Swallow, R.A.; Talwar, S.; O’Kane, P.D. Beyond the balloon: Excimer coronary laser atherectomy used alone or in combination with rotational atherectomy in the treatment of chronic total occlusions, non-crossable and non-expansible coronary lesions. EuroIntervention 2013, 9, 243–250. [Google Scholar] [CrossRef]
- Sandoval, Y.; Lobo, A.S.; Tajti, P.; Brilakis, E.S. Laser-assisted orbital or rotational atherectomy: A hybrid treatment strategy for balloon-uncrossable lesions. Hell. J. Cardiol. 2020, 61, 57–59. [Google Scholar] [CrossRef]
- Vo, M.N.; Christopoulos, G.; Karmpaliotis, D.; Lombardi, W.L.; Grantham, J.A.; Brilakis, E.S. Balloon-Assisted Microdissection “BAM” Technique for Balloon-Uncrossable Chronic Total Occlusions. J. Invasive. Cardiol. 2016, 28, E37–E41. [Google Scholar]
- Megaly, M.; Brilakis, E.S. Primary orbital atherectomy for treating a heavily calcified balloon uncrossable lesion. Cardiovasc. Revasc. Med. 2020, 21, 96–99. [Google Scholar] [CrossRef] [PubMed]
- Christopoulos, G.; Kotsia, A.P.; Rangan, B.V.; Vo, M.; Alaswad, K.; Karmpaliotis, D.; Banerjee, S.; Brilakis, E.S. “Subintimal external crush” technique for a “balloon uncrossable” chronic total occlusion. Cardiovasc. Revasc. Med. 2017, 18, 63–65. [Google Scholar] [CrossRef] [PubMed]
- Vo, M.N.; Ravandi, A.; Grantham, J.A. Subintimal space plaque modification for "balloon-uncrossable" chronic total occlusions. J. Invasive Cardiol. 2014, 26, E133–E136. [Google Scholar] [PubMed]
- Egred, M. RASER angioplasty. Catheter. Cardiovasc. Interv. 2012, 79, 1009–1012. [Google Scholar] [CrossRef]
- Karacsonyi, J.; Armstrong, E.J.; Truong, H.T.D.; Tsuda, R.; Kokkinidis, D.G.; Martinez-Parachini, J.R.; Alame, A.J.; Danek, B.A.; Karatasakis, A.; Roesle, M.; et al. Contemporary Use of Laser During Percutaneous Coronary Interventions: Insights from the Laser Veterans Affairs (LAVA) Multicenter Registry. J. Invasive. Cardiol. 2018, 30, 195–201. [Google Scholar] [CrossRef]
- Brilakis, E.S. Manual of Chronic Total Occlusion Interventions, A Step-by-Step Approach, 2nd ed.; Elsevier: London, UK, 2018. [Google Scholar]
- McQuillan, C.; Jackson, M.W.P.; Brilakis, E.S.; Egred, M. Uncrossable and undilatable lesions-A practical approach to optimizing outcomes in PCI. Catheter. Cardiovasc. Interv. 2021, 97, 121–126. [Google Scholar] [CrossRef] [PubMed]
- Salem, H.; Mintz, G.S.; Matsumura, M.; Zhang, M.; Usui, E.; Seike, F.; Fujimura, T.; Noguchi, M.; Hu, X.; Jin, G.; et al. Reasons for lesion uncrossability as assessed by intravascular ultrasound. Catheter. Cardiovasc. Interv. 2022, 99, 2028–2037. [Google Scholar] [CrossRef]
- Xenogiannis, I.; Karmpaliotis, D.; Alaswad, K.; Jaffer, F.A.; Yeh, R.W.; Patel, M.; Mahmud, E.; Choi, J.W.; Burke, M.N.; Doing, A.H.; et al. Usefulness of Atherectomy in Chronic Total Occlusion Interventions (from the PROGRESS-CTO Registry). Am. J. Cardiol. 2019, 123, 1422–1428. [Google Scholar] [CrossRef]
- Dens, J.; Holvoet, W.; McCutcheon, K.; Ungureanu, C.; Coussement, P.; Haine, S.; De Hemptinne, Q.; Sonck, J.; Eertmans, W.; Bennett, J. A prospective, multi-center, randomised controlled trial for evaluation of the effectiveness of the Blimp scoring balloon in lesions not crossable with a conventional balloon or microcatheter: The BLIMP study. Acta Cardiol. 2022, 78, 1–5. [Google Scholar] [CrossRef]
- Ye, Y.; Zhao, X.; Du, J.; Zeng, Y. Efficacy and safety of balloon-assisted microdissection with Sapphire(R) II 1.0-mm balloon in balloon-uncrossable chronic total occlusion lesions. J. Int. Med. Res. 2020, 48, 300060520965822. [Google Scholar] [CrossRef]
- Ambrosini, V.; Sorropago, G.; Laurenzano, E.; Golino, L.; Casafina, A.; Schiano, V.; Gabrielli, G.; Ettori, F.; Chizzola, G.; Bernardi, G.; et al. Early outcome of high energy Laser (Excimer) facilitated coronary angioplasty ON hARD and complex calcified and balloOn-resistant coronary lesions: LEONARDO Study. Cardiovasc. Revasc. Med. 2015, 16, 141–146. [Google Scholar] [CrossRef]
- Karacsonyi, J.; Brilakis, E.S.; Chandwaney, R.H. Guide-Extension Carlino: A novel technique for crossing a microcatheter uncrossable proximal cap during chronic total occlusion interventions. Catheter. Cardiovasc. Interv. 2022, 99, 2038–2042. [Google Scholar] [CrossRef] [PubMed]
- Michael, T.T.; Banerjee, S.; Brilakis, E.S. Subintimal distal anchor technique for “balloon-uncrossable” chronic total occlusions. J. Invasive Cardiol. 2013, 25, 552–554. [Google Scholar] [PubMed]



| Variable | Balloon Uncrossable (n = 795) | Balloon Crossable (n = 7876) | p Value |
|---|---|---|---|
| Age (years) * | 67.3 ± 9 | 63.9 ± 10 | <0.001 |
| Men | 656 (84.8%) | 6099 (79.9%) | 0.006 |
| BMI (kg/m2) * | 30.0 ± 6 | 30.3 ± 6 | 0.103 |
| Diabetes Mellitus | 379 (50.1%) | 3075 (41.8%) | <0.001 |
| Hypertension | 692 (90.6%) | 6539 (87.9%) | 0.030 |
| Dyslipidemia | 690 (90.8%) | 6233 (84.0%) | <0.001 |
| Smoking (current) | 165 (20.8%) | 1897 (24.1%) | 0.036 |
| LVEF (%) * | 50 ± 12 | 50 ± 13 | 0.670 |
| Family History of CAD | 213 (32.9%) | 2068 (32.1%) | 0.684 |
| Congestive Heart Failure | 226 (30.6%) | 2014 (28.0%) | 0.131 |
| Prior Myocardial Infarction | 330 (46.0%) | 3136 (44.3%) | 0.386 |
| Prior CABG | 303 (40.0%) | 1866 (25.4%) | <0.001 |
| Prior CVD | 81 (10.8%) | 730 (10.1%) | 0.504 |
| Prior PVD | 123 (16.5%) | 928 (12.8%) | 0.004 |
| Clinical presentation | |||
| 477 (63.5%) | 4887 (66.4%) | 0.001 |
| 127 (16.9%) | 1158 (15.7%) | |
| 85 (11.3%) | 578 (7.9%) | |
| 3 (0.4%) | 110 (1.5%) | |
| 20 (2.7%) | 157 (2.1%) | |
| 39 (5.2%) | 470 (6.4%) | |
| Baseline creatinine (mg/dL) † | 1.0 (0.9, 1.2) | 1.0 (0.9, 1.2) | 0.646 |
| CTO Target Vessel | |||
| 435 (56.1%) | 3988 (51.6%) | <0.001 |
| 156 (20.1%) | 2147 (27.8%) | |
| 168 (21.7%) | 1424 (18.4%) | |
| 0 (0%) | 11 (0.1%) | |
| 4 (0.5%) | 38 (0.5%) | |
| 13 (1.7%) | 122 (1.6%) | |
| J-CTO score * | 2.58 ± 1.19 | 2.23 ± 1.28 | <0.001 |
| PROGRESS-CTO score * | 1.30 ± 1.02 | 1.11 ± 0.97 | <0.001 |
| PROGRESS-CTO MACE score | 2.66 ± 1.54 | 2.44 ± 1.64 | <0.001 |
| Calcification (moderate/severe) | 544 (68.4%) | 3105 (39.4%) | <0.001 |
| Proximal vessel tortuosity (moderate/severe) | 289 (36.4%) | 1992 (25.3%) | <0.001 |
| Proximal cap ambiguity | 210 (27.6%) | 2360 (31.6%) | 0.025 |
| In-stent restenosis | 177 (22.9%) | 1185 (15.6%) | <0.001 |
| Side branch at the proximal cap | 388 (51.6%) | 3965 (54.5%) | 0.123 |
| Blunt/no stump, % | 379 (47.7%) | 4002 (50.8%) | 0.092 |
| Vessel diameter (mm) † | 3.0 (2.5, 3.0) | 3.0 (2.5, 3.0) | 0.033 |
| Occlusion length (mm) † | 25 (15, 40) | 25 (15, 40) | 0.060 |
| Number of stents used * | 2.3 ± 1.1 | 2.3 ± 1.1 | 0.234 |
| Variable | Balloon Uncrossable (n = 795) | Balloon Crossable (n = 7876) | p Value |
|---|---|---|---|
| Successful Crossing Strategy | |||
| 571 (72.0%) | 5141 (65.6%) | <0.001 |
| 118 (14.9%) | 1621 (20.7%) | |
| 104 (13.1%) | 1070 (13.7%) | |
| First Crossing Strategy | |||
| 712 (89.7%) | 6706 (85.6%) | 0.006 |
| 62 (7.8%) | 891 (11.4%) | |
| 20 (2.5%) | 237 (3.0%) | |
| Retrograde crossing strategy | 174 (21.9%) | 2187 (27.8%) | <0.001 |
| ADR crossing strategy | 143 (18.0%) | 1393 (17.7%) | 0.832 |
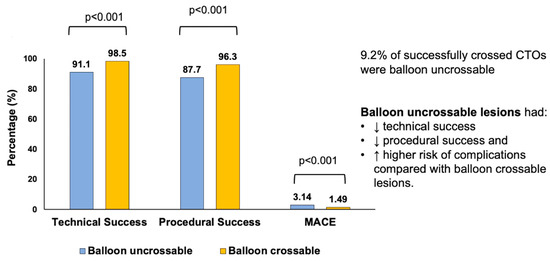
| Technical Success | 724 (91.1%) | 7761 (98.5%) | <0.001 |
| Procedural Success | 697 (87.7%) | 7585 (96.3%) | <0.001 |
| Procedural time (min) † | 132 (90, 197) | 109 (71, 160) | <0.001 |
| Fluoroscopy time (min) † | 52 (34, 79) | 39 (24, 63) | <0.001 |
| Air kerma radiation dose (Gray) † | 2.55 (1.41, 4.23) | 1.97 (1.10, 3.40) | <0.001 |
| Contrast volume (mL) † | 210 (150, 300) | 200 (145, 280) | 0.001 |
| MACE | 25 (3.14%) | 117 (1.49%) | <0.001 |
| Death | 4 (0.50%) | 26 (0.33%) | 0.428 |
| Acute MI | 7 (0.88%) | 31 (0.39%) | 0.048 |
| Re-PCI | 2 (0.25%) | 13 (0.17%) | 0.576 |
| Stroke | 0 (0.13%) | 13 (0.17%) | 0.793 |
| Emergency CABG | 0 (0%) | 1 (0.01%) | 0.751 |
| Pericardiocentesis | 14 (1.76%) | 54 (0.69%) | 0.001 |
| Perforation | 48 (6.04%) | 269 (3.42%) | <0.001 |
| Dissection/Thrombus of Donor Artery | 4 (0.50%) | 51 (0.65%) | 0.625 |
| Aortocoronary Dissection | 1 (0.13%) | 22 (0.28%) | 0.422 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Karacsonyi, J.; Kostantinis, S.; Simsek, B.; Rempakos, A.; Allana, S.S.; Alaswad, K.; Krestyaninov, O.; Khatri, J.; Poommipanit, P.; Jaffer, F.A.; et al. Angiographic Features and Clinical Outcomes of Balloon Uncrossable Lesions during Chronic Total Occlusion Percutaneous Coronary Intervention. J. Pers. Med. 2023, 13, 515. https://doi.org/10.3390/jpm13030515
Karacsonyi J, Kostantinis S, Simsek B, Rempakos A, Allana SS, Alaswad K, Krestyaninov O, Khatri J, Poommipanit P, Jaffer FA, et al. Angiographic Features and Clinical Outcomes of Balloon Uncrossable Lesions during Chronic Total Occlusion Percutaneous Coronary Intervention. Journal of Personalized Medicine. 2023; 13(3):515. https://doi.org/10.3390/jpm13030515
Chicago/Turabian StyleKaracsonyi, Judit, Spyridon Kostantinis, Bahadir Simsek, Athanasios Rempakos, Salman S. Allana, Khaldoon Alaswad, Oleg Krestyaninov, Jaikirshan Khatri, Paul Poommipanit, Farouc A. Jaffer, and et al. 2023. "Angiographic Features and Clinical Outcomes of Balloon Uncrossable Lesions during Chronic Total Occlusion Percutaneous Coronary Intervention" Journal of Personalized Medicine 13, no. 3: 515. https://doi.org/10.3390/jpm13030515