Changes in the Mean of and Variance in Psychological Disease Incidences before and during the COVID-19 Pandemic in the Korean Adult Population
Abstract
:1. Introduction
2. Materials and Methods
2.1. Ethics
2.2. Participants and Measurement
2.3. Statistics
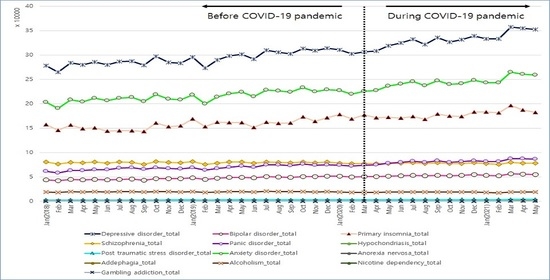
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Park, J.-H.; Jang, W.; Kim, S.-W.; Lee, J.; Lim, Y.-S.; Cho, C.-G.; Park, S.-W.; Kim, B.H. The Clinical Manifestations and Chest Computed Tomography Findings of Coronavirus Disease 2019 (COVID-19) Patients in China: A Proportion Meta-Analysis. Clin. Exp. Otorhinolaryngol. 2020, 13, 95–105. [Google Scholar] [CrossRef] [PubMed]
- Kim, S.Y.; Kim, D.W. Does the Clinical Spectrum of Coronavirus Disease 2019 (COVID-19) Show Regional Differences? Clin. Exp. Otorhinolaryngol. 2020, 13, 83–84. [Google Scholar] [CrossRef] [PubMed]
- Ashraf, A.; AIi, I.; Ullah, F. Domestic and gender-Based violence: Pakistan scenario amidst COVID-19. Asian J. Soc. Health Behav. 2021, 4, 47–50. [Google Scholar] [CrossRef]
- Alimoradi, Z.; Gozal, D.; Tsang, H.W.H.; Lin, C.; Broström, A.; Ohayon, M.M.; Pakpour, A.H. Gender-specific estimates of sleep problems during the COVID-19 pandemic: Systematic review and meta-analysis. J. Sleep Res. 2022, 31, e13432. [Google Scholar] [CrossRef] [PubMed]
- Alimoradi, Z.; Broström, A.; Tsang, H.W.; Griffiths, M.D.; Haghayegh, S.; Ohayon, M.M.; Lin, C.-Y.; Pakpour, A.H. Sleep problems during COVID-19 pandemic and its’ association to psychological distress: A systematic review and meta-analysis. EClinicalMedicine 2021, 36, 100916. [Google Scholar] [CrossRef] [PubMed]
- Olashore, A.A.; Akanni, O.O.; Fela-Thomas, A.L.; Khutsafalo, K. The psychological impact of COVID-19 on health-care workers in African Countries: A systematic review. Asian J. Soc. Health Behav. 2021, 4, 85–97. [Google Scholar]
- Rajabimajd, N.; Alimoradi, Z.; Griffiths, M.D. Impact of COVID-19-related fear and anxiety on job attributes: A systematic review. Asian J. Soc. Health Behav. 2021, 4, 51–55. [Google Scholar] [CrossRef]
- Dong, L.; Bouey, J. Public Mental Health Crisis during COVID-19 Pandemic, China. Emerg. Infect. Dis. 2020, 26, 1616–1618. [Google Scholar] [CrossRef]
- Ferrante, G.; Camussi, E.; Piccinelli, C.; Senore, C.; Armaroli, P.; Ortale, A.; Garena, F.; Giordano, L. Did social isolation during the SARS-CoV-2 epidemic have an impact on the lifestyles of citizens? Epidemiol. Prev. 2020, 44, 353–362. [Google Scholar] [CrossRef]
- Hossain, M.; Tasnim, S.; Sultana, A.; Faizah, F.; Mazumder, H.; Zou, L.; McKyer, E.L.J.; Ahmed, H.U.; Ma, P. Epidemiology of mental health problems in COVID-19: A review. F1000Research 2020, 9, 636. [Google Scholar] [CrossRef]
- Michail, D.; Anastasiou, D.; Palaiologou, N.; Avlogiaris, G. Social Climate and Psychological Response in the First Wave of the COVID-19 Pandemic in a Greek Academic Community. Sustainability 2022, 14, 1576. [Google Scholar] [CrossRef]
- Luo, M.; Guo, L.; Yu, M.; Jiang, W.; Wang, H. The psychological and mental impact of coronavirus disease 2019 (COVID-19) on medical staff and general public—A systematic review and meta-analysis. Psychiatry Res. 2020, 291, 113190. [Google Scholar] [CrossRef] [PubMed]
- COVID-19 Mental Disorders Collaborators. Global prevalence and burden of depressive and anxiety disorders in 204 countries and territories in 2020 due to the COVID-19 pandemic. Lancet 2021, 398, 1700–1712. [Google Scholar] [CrossRef]
- Xiong, J.; Lipsitz, O.; Nasri, F.; Lui, L.M.W.; Gill, H.; Phan, L.; Chen-Li, D.; Iacobucci, M.; Ho, R.; Majeed, A.; et al. Impact of COVID-19 pandemic on mental health in the general population: A systematic review. J. Affect. Disord. 2020, 277, 55–64. [Google Scholar] [CrossRef] [PubMed]
- Kim, S.Y.; Yoo, D.M.; Min, C.; Choi, H.G. Assessment of the difference in depressive symptoms of the Korean adult population before and during the COVID-19 pandemic using a community health survey. J. Affect. Disord. 2022, 300, 130–136. [Google Scholar] [CrossRef]
- Lu, M.-Y.; Ahorsu, D.K.; Kukreti, S.; Strong, C.; Lin, Y.-H.; Kuo, Y.-J.; Chen, Y.-P.; Lin, C.-Y.; Chen, P.-L.; Ko, N.-Y.; et al. The Prevalence of Post-traumatic Stress Disorder Symptoms, Sleep Problems, and Psychological Distress Among COVID-19 Frontline Healthcare Workers in Taiwan. Front. Psychiatry 2021, 12, 705657. [Google Scholar] [CrossRef]
- Nordstokke, D.W.; Zumbo, B.D. A New Nonparametric Levene Test for Equal Variances. Psicológica 2010, 31, 401–430. [Google Scholar]
- Lebel, C.; MacKinnon, A.; Bagshawe, M.; Tomfohr-Madsen, L.; Giesbrecht, G. Elevated depression and anxiety symptoms among pregnant individuals during the COVID-19 pandemic. J. Affect. Disord. 2020, 277, 5–13. [Google Scholar] [CrossRef]
- Serafini, G.; Parmigiani, B.; Amerio, A.; Aguglia, A.; Sher, L.; Amore, M. The psychological impact of COVID-19 on the mental health in the general population. QJM Int. J. Med. 2020, 113, 531–537. [Google Scholar] [CrossRef]
- Georgieva, I.; Lepping, P.; Bozev, V.; Lickiewicz, J.; Pekara, J.; Wikman, S.; Loseviča, M.; Raveesh, B.; Mihai, A.; Lantta, T. Prevalence, New Incidence, Course, and Risk Factors of PTSD, Depression, Anxiety, and Panic Disorder during the COVID-19 Pandemic in 11 Countries. Healthcare 2021, 9, 664. [Google Scholar] [CrossRef]
- Bäuerle, A.; Teufel, M.; Musche, V.; Weismüller, B.; Kohler, H.; Hetkamp, M.; Dörrie, N.; Schweda, A.; Skoda, E.-M. Increased generalized anxiety, depression and distress during the COVID-19 pandemic: A cross-sectional study in Germany. J. Public Health 2020, 42, 672–678. [Google Scholar] [CrossRef]
- Deng, J.; Zhou, F.; Hou, W.; Silver, Z.; Wong, C.Y.; Chang, O.; Huang, E.; Zuo, Q.K. The prevalence of depression, anxiety, and sleep disturbances in COVID-19 patients: A meta-analysis. Ann. N. Y. Acad. Sci. 2021, 1486, 90–111. [Google Scholar] [CrossRef]
- Pantelis, C.; Jayaram, M.; Hannan, A.J.; Wesselingh, R.; Nithianantharajah, J.; Wannan, C.M.; Syeda, W.T.; Choy, K.C.; Zantomio, D.; Christopoulos, A.; et al. Neurological, neuropsychiatric and neurodevelopmental complications of COVID-19. Aust. N. Z. J. Psychiatry 2021, 55, 750–762. [Google Scholar] [CrossRef] [PubMed]
- Ahn, E.-J.; Min, H.J. Prevalence of Olfactory or Gustatory Dysfunction in COVID-19 Patients: An Analysis Based on Korean Nationwide Claims Data. Clin. Exp. Otorhinolaryngol. 2021, 14, 427–430. [Google Scholar] [CrossRef] [PubMed]
- Kim, D.H.; Kim, S.W.; Stybayeva, G.; Lim, S.Y.; Hwang, S.H. Predictive Value of Olfactory and Taste Symptoms in the Diagnosis of COVID-19: A Systematic Review and Meta-Analysis. Clin. Exp. Otorhinolaryngol. 2021, 14, 312–320. [Google Scholar] [CrossRef] [PubMed]
- Barlati, S.; Nibbio, G.; Vita, A. Schizophrenia during the COVID-19 pandemic. Curr. Opin. Psychiatry 2021, 34, 203–210. [Google Scholar] [CrossRef] [PubMed]
- Kozloff, N.; Mulsant, B.H.; Stergiopoulos, V.; Voineskos, A.N. The COVID-19 Global Pandemic: Implications for People With Schizophrenia and Related Disorders. Schizophr. Bull. 2020, 46, 752–757. [Google Scholar] [CrossRef]
- Mallet, J.; Dubertret, C.; Le Strat, Y. Addictions in the COVID-19 era: Current evidence, future perspectives a comprehensive review. Prog. Neuro-Psychopharmacol. Biol. Psychiatry 2021, 106, 110070. [Google Scholar] [CrossRef]
- Jackson, S.E.; Garnett, C.; Shahab, L.; Oldham, M.; Brown, J. Association of the COVID-19 lockdown with smoking, drinking and attempts to quit in England: An analysis of 2019–20 data. Addiction 2021, 116, 1233–1244. [Google Scholar] [CrossRef]
- Armitage, R.; Nellums, L.B. COVID-19 and the consequences of isolating the elderly. Lancet Public Health 2020, 5, e256. [Google Scholar] [CrossRef] [Green Version]
- Santini, Z.I.; Jose, P.E.; Cornwell, E.Y.; Koyanagi, A.; Nielsen, L.; Hinrichsen, C.; Meilstrup, C.; Madsen, K.R.; Koushede, V. Social disconnectedness, perceived isolation, and symptoms of depression and anxiety among older Americans (NSHAP): A longitudinal mediation analysis. Lancet Public Health 2020, 5, e62–e70. [Google Scholar] [CrossRef] [Green Version]
- Rehman, U.; Shahnawaz, M.G.; Khan, N.H.; Kharshiing, K.D.; Khursheed, M.; Gupta, K.; Kashyap, D.; Uniyal, R. Depression, Anxiety and Stress Among Indians in Times of COVID-19 Lockdown. Community Ment. Health J. 2021, 57, 42–48. [Google Scholar] [CrossRef] [PubMed]

| Diseases | Before COVID-19 | During COVID-19 | p-Values of Difference | |||
|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | Mean | Variance | |
| Depressive disorder | 292,620.1 | 13,403.1 | 331,656.6 | 15,192.2 | <0.001 * | 0.065 |
| Bipolar disorder | 47,067.7 | 2728.7 | 52,970.3 | 1708.0 | <0.001 * | 0.046 † |
| Primary insomnia | 157,690.5 | 9721.9 | 178,290.8 | 7332.3 | <0.001 * | 0.100 |
| Schizophrenia | 79,229.4 | 1583.9 | 77,719.1 | 1073.1 | <0.001 * | 0.113 |
| Panic disorder | 68,631.9 | 4846.0 | 81,340.6 | 3953.8 | <0.001 * | 0.046 † |
| Hypochondriasis | 704.7 | 35.5 | 895.8 | 120.0 | <0.001 * | 0.224 |
| Posttraumatic stress disorder | 2606.5 | 228.9 | 3211.4 | 279.5 | <0.001 * | 0.140 |
| Anxiety disorder | 215,058.6 | 10,457.6 | 244,046.6 | 11,009.8 | <0.001 * | 0.052 |
| Anorexia nervosa | 605.0 | 95.3 | 729.1 | 53.1 | <0.001 * | 0.080 |
| Addephagia | 690.5 | 43.7 | 832.1 | 65.2 | <0.001 * | 0.108 |
| Alcoholism | 19,248.2 | 482.0 | 18,489.0 | 535.9 | <0.001 * | 0.115 |
| Nicotine dependency | 380.4 | 47.4 | 308.5 | 33.6 | <0.001 * | 0.279 |
| Gambling addiction | 297.5 | 32.3 | 414.1 | 69.0 | <0.001 * | 0.014 † |
| Diseases | Before COVID-19 | During COVID-19 | p-Values of Difference | |||
|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | Mean | Variance | |
| Men | ||||||
| Depressive disorder | 93,001.0 | 4416.1 | 103,448.4 | 3957.7 | <0.001 * | <0.001 † |
| Bipolar disorder | 18,939.4 | 999.0 | 20,628.0 | 537.7 | <0.001 * | <0.001 † |
| Primary insomnia | 62,275.8 | 4002.0 | 70,463.9 | 2474.7 | <0.001 * | <0.001 † |
| Schizophrenia | 36,100.1 | 741.9 | 35,035.8 | 446.3 | <0.001 * | <0.001 † |
| Panic disorder | 32,491.6 | 2103.5 | 37,652.8 | 1529.4 | <0.001 * | <0.001 † |
| Hypochondriasis | 367.3 | 18.9 | 487.4 | 88.1 | <0.001 * | <0.001 † |
| Posttraumatic stress disorder | 1016.6 | 84.1 | 1209.3 | 97.0 | <0.001 * | <0.001 † |
| Anxiety disorder | 88,061.0 | 4359.1 | 98,208.9 | 3824.1 | <0.001 * | <0.001 † |
| Anorexia nervosa | 125.0 | 21.6 | 147.8 | 18.1 | 0.004 * | 0.001 † |
| Addephagia | 56.7 | 7.1 | 54.6 | 5.9 | 0.283 | 0.352 |
| Alcoholism | 15,908.8 | 388.4 | 14,929.1 | 422.6 | <0.001 * | <0.001 † |
| Nicotine dependency | 338.4 | 42.9 | 267.1 | 30.0 | <0.001 * | <0.001 † |
| Gambling addiction | 284.1 | 30.6 | 397.7 | 68.6 | <0.001 * | <0.001 † |
| Women | ||||||
| Depressive disorder | 199,619.1 | 9033.8 | 228,208.2 | 11,259.4 | <0.001 * | <0.001 † |
| Bipolar disorder | 28,128.2 | 1735.0 | 32,342.3 | 1176.9 | <0.001 * | <0.001 † |
| Primary insomnia | 95,414.7 | 5747.8 | 107,826.9 | 4878.0 | <0.001 * | <0.001 † |
| Schizophrenia | 43,129.3 | 895.2 | 42,683.3 | 647.1 | 0.036 * | 0.099 |
| Panic disorder | 36,140.3 | 2746.4 | 43,687.8 | 2437.3 | <0.001 * | <0.001 † |
| Hypochondriasis | 337.5 | 24.0 | 408.4 | 35.6 | <0.001 * | <0.001 † |
| Posttraumatic stress disorder | 1589.9 | 148.0 | 2002.1 | 184.8 | <0.001 * | <0.001 † |
| Anxiety disorder | 126,997.6 | 6125.2 | 145,837.7 | 7225.4 | <0.001 * | <0.001 † |
| Anorexia nervosa | 479.9 | 75.5 | 581.3 | 41.3 | <0.001 * | <0.001 † |
| Addephagia | 633.9 | 41.3 | 777.5 | 64.9 | <0.001 * | <0.001 † |
| Alcoholism | 3339.4 | 115.7 | 3559.9 | 147.5 | <0.001 * | <0.001 † |
| Nicotine dependency | 42.0 | 10.4 | 41.5 | 7.4 | 0.947 | 0.863 |
| Gambling addiction | 13.5 | 3.8 | 16.4 | 3.2 | 0.018 * | 0.016 † |
| Diseases | Before COVID-19 | During COVID-19 | p-Values of Difference | |||
|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | Mean | Variance | |
| Age 20–39 years old | ||||||
| Depressive disorder | 71,186.6 | 8426.6 | 98,224.07 | 8281.236 | <0.001 * | <0.001 † |
| Bipolar disorder | 16,655.5 | 1345.4 | 20,394.40 | 1039.450 | <0.001 * | <0.001 † |
| Primary insomnia | 23,920.1 | 1123.4 | 26,040.13 | 657.012 | <0.001 * | <0.001 † |
| Schizophrenia | 25,253.5 | 535.2 | 24,169.13 | 364.634 | <0.001 * | <0.001 † |
| Panic disorder | 21,229.2 | 1928.8 | 25,956.20 | 1309.550 | <0.001 * | <0.001 † |
| Hypochondriasis | 147.6 | 13.5 | 192.33 | 32.797 | <0.001 * | <0.001 † |
| Posttraumatic stress disorder | 1157.4 | 107.9 | 1538.40 | 158.457 | <0.001 * | <0.001 † |
| Anxiety disorder | 49,638.9 | 4329.4 | 61,145.00 | 3890.384 | <0.001 * | <0.001 † |
| Anorexia nervosa | 151.7 | 13.4 | 177.80 | 17.729 | <0.001 * | <0.001 † |
| Addephagia | 507.9 | 34.0 | 631.20 | 51.985 | <0.001 * | <0.001 † |
| Alcoholism | 2800.4 | 142.0 | 2944.40 | 124.962 | 0.003 * | 0.002 † |
| Nicotine dependency | 80.0 | 15.7 | 67.47 | 14.918 | 0.014 * | 0.017 † |
| Gambling addiction | 209.5 | 29.3 | 304.93 | 54.928 | <0.001 * | <0.001 † |
| Age 40–59 years old | ||||||
| Depressive disorder | 93,126.1 | 2946.4 | 98,709.6 | 3436.8 | <0.001 * | <0.001 † |
| Bipolar disorder | 17,747.2 | 650.9 | 18,579.3 | 403.8 | <0.001 * | <0.001 † |
| Primary insomnia | 53,514.6 | 2709.5 | 58,857.4 | 1673.9 | <0.001 * | <0.001 † |
| Schizophrenia | 39,003.7 | 913.6 | 37,193.2 | 574.2 | <0.001 * | <0.001 † |
| Panic disorder | 33,226.0 | 2009.9 | 37,970.7 | 1675.0 | <0.001 * | <0.001 † |
| Hypochondriasis | 286.6 | 16.8 | 374.6 | 55.5 | <0.001 * | <0.001 † |
| Posttraumatic stress disorder | 949.5 | 80.0 | 1072.3 | 78.5 | <0.001 * | <0.001 † |
| Anxiety disorder | 83,498.2 | 3552.9 | 90,802.9 | 3552.5 | <0.001 * | <0.001 † |
| Anorexia nervosa | 75.3 | 11.4 | 82.5 | 5.4 | 0.024 * | 0.029 † |
| Addephagia | 136.4 | 11.7 | 153.3 | 16.2 | 0.002 * | <0.001 † |
| Alcoholism | 9555.7 | 286.1 | 8812.7 | 284.2 | <0.001 * | <0.001 † |
| Nicotine dependency | 203.0 | 32.1 | 160.9 | 19.2 | <0.001 * | <0.001 † |
| Gambling addiction | 69.5 | 7.9 | 87.6 | 11.9 | <0.001 * | <0.001 † |
| Age 60+ years old | ||||||
| Depressive disorder | 128,307.4 | 3547.4 | 134,722.9 | 3962.8 | <0.001 * | <0.001 † |
| Bipolar disorder | 12,665.0 | 770.7 | 13,996.6 | 345.2 | <0.001 * | <0.001 † |
| Primary insomnia | 80,255.8 | 6311.4 | 93,393.3 | 5484.8 | <0.001 * | <0.001 † |
| Schizophrenia | 14,972.2 | 636.7 | 16,356.7 | 485.1 | <0.001 * | <0.001 † |
| Panic disorder | 14,176.7 | 975.5 | 17,413.7 | 1064.2 | <0.001 * | <0.001 † |
| Hypochondriasis | 270.5 | 16.0 | 328.9 | 36.1 | <0.001 * | <0.001 † |
| Posttraumatic stress disorder | 499.5 | 50.3 | 600.7 | 48.3 | <0.001 * | <0.001 † |
| Anxiety disorder | 81,921.5 | 3288.4 | 92,098.7 | 3965.8 | <0.001 * | <0.001 † |
| Anorexia nervosa | 377.9 | 83.8 | 468.9 | 41.1 | 0.002 * | <0.001 † |
| Addephagia | 46.2 | 6.0 | 47.6 | 9.0 | 0.569 | <0.001 † |
| Alcoholism | 6892.1 | 148.7 | 6731.9 | 173.4 | 0.007 * | 0.003 † |
| Nicotine dependency | 97.5 | 14.8 | 80.1 | 13.4 | 0.001 * | 0.001 † |
| Gambling addiction | 18.5 | 3.5 | 21.5 | 4.3 | 0.023 * | 0.020 † |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kim, S.Y.; Yoo, D.M.; Kwon, M.-J.; Kim, J.-H.; Kim, J.-H.; Bang, W.-J.; Choi, H.G. Changes in the Mean of and Variance in Psychological Disease Incidences before and during the COVID-19 Pandemic in the Korean Adult Population. J. Pers. Med. 2022, 12, 576. https://doi.org/10.3390/jpm12040576
Kim SY, Yoo DM, Kwon M-J, Kim J-H, Kim J-H, Bang W-J, Choi HG. Changes in the Mean of and Variance in Psychological Disease Incidences before and during the COVID-19 Pandemic in the Korean Adult Population. Journal of Personalized Medicine. 2022; 12(4):576. https://doi.org/10.3390/jpm12040576
Chicago/Turabian StyleKim, So Young, Dae Myoung Yoo, Mi-Jung Kwon, Ji-Hee Kim, Joo-Hee Kim, Woo-Jin Bang, and Hyo Geun Choi. 2022. "Changes in the Mean of and Variance in Psychological Disease Incidences before and during the COVID-19 Pandemic in the Korean Adult Population" Journal of Personalized Medicine 12, no. 4: 576. https://doi.org/10.3390/jpm12040576