1. Introduction
Gluteal muscle contracture (GMC) is a clinical syndrome characterized by limited hip joint function attributed to gluteal muscle and corresponding fascia contracture. Patients typically present with an increased hip abduction angle while flexing the hip and knee, an inability to squat down while closing knees together or cross their legs, a positive Ober’s sign, an audible snapping sound during squatting, and even claudication gait in severe cases [
1,
2]. GMC is mainly associated with repeated intramuscular injection in the buttocks of patients in childhood, while a few cases are related to trauma and autoimmune function in terms of etiology [
3]. As reported previously, the incidence of GMC in China ranges from 1–2.5% in China [
4]. As is well-known nationwide, the diagnosis and treatment of GMC are parts of the characteristic specialties of our group-affiliated department, and on average, 2–3 GMC patients visit the hospital every week. In our hospital, such patients are mainly treated with minimally invasive therapy by arthroscopic GMC release [
5]. During clinical practice, the vast majority of patients complain of an inability to squat down while closing their knees together or crossing their legs upon arrival. Most of these patients present with knee pain or discomfort; this is aggravated after vigorous activity and can be relieved after minimally invasive GMC release.
Correlations exist between anterior knee pain and GMC-induced patellofemoral instability. This may trigger repeated patellar dislocation and further develop into patellar cartilage softening or patellofemoral osteoarthritis. As previously reported, patellofemoral instability can be efficiently ameliorated by means of arthroscopic GMC release, thus alleviating the knee pain [
6]. A study conducted by Zhao et al. [
7] analyzed the diagnosis and treatment of 36 GMC patients with anterior knee pain and confirmed that arthroscopic GMC release can relieve anterior knee pain, thus contributing to the prevention of patellofemoral arthritis. Another study reported by Wang et al. [
8] on the diagnosis and treatment of 52 GMC patients with knee osteoarthritis revealed that GMC can affect knee joint stability and induce premature degenerative changes in the knee joints, thus leading to the occurrence of knee osteoarthritis. In addition, Jia et al. [
9] reported that compared with arthroscopic GMC release alone, the combination of arthroscopic GMC release and medial patellar retinaculum plication and lateral patellar retinaculum release can better alleviate anterior knee pain resulting from long-term GMC and reduce patellar lateral displacement, thus indicating that the preoperative assessment and selection of surgical approaches are of great significance for patients with different conditions of GMC and anterior knee pain. However, most existing studies have only reported single-factor analysis for the correlation between GMC and patellofemoral instability. Unfortunately, the influence of multiple confounding factors such as GMC severity and congenital patellofemoral dysplasia has not been considered. This vital omission is not conducive to preoperatively evaluating and formulating clinical therapeutic strategies for GMC with patellofemoral instability or for predicting and assessing the postoperative improvement rate of patellofemoral instability.
The diagnosis, severity assessment, and classification of GMC are mainly based on clinical symptoms, physical examination, imaging data, and intraoperative arthroscopic assessment (
Figure 1) [
1,
2,
6]. Patellofemoral instability is mainly evaluated by means of physical examination and imaging methods. In addition to routine indicators, four novel assessment indicators were specifically designed for this study. First, the knee flexion angle and hip flexion angle in the case of maximally squatting while closing the knees together (
Figure 1(C1,2)). Second, the minimum distance between the feet required for the patient to squat down completely (
Figure 1(C3)). Third, in the axial computed tomography (CT) image of the knee joint, a connecting line was made between the highest point of the lateral femoral condyle and the outermost point of the patella on the plane connecting each of the highest points of the medial and lateral femoral condyles; the length of the connecting line was considered as L, and the angle between the plane and the connecting line was regarded as α. Fourth, in the axial CT image of the knee joint, the cross-sectional area between the femur and the patella was measured on the plane connecting each of the highest points of the medial and lateral femoral condyles. This study aimed to investigate the correlations between GMC severity and patellofemoral instability and to evaluate the reliability of novel indicators by performing multivariate analysis with multiple indicators. We also aimed to investigate the efficacy of arthroscopic GMC release. The present study can provide a reliable basis to investigate the correlations between GMC and patellofemoral instability, and offer theoretical references for preoperative assessment and clinical decision-making for GMC patients with patellofemoral instability.
3. Results
In this study, we enrolled a total of 115 GMC patients with a mean age of 32 ± 6.02 years including 63 females (63/115, 54.78%). Of these, 92.17% (106/115) of patients experienced repeated intramuscular injections during their childhood, 7.83% (9/115) had a history of gluteal muscle trauma in their buttocks, and 35.65% (41/115) of patients suffered from knee pain or discomfort (
Table 1). None of the cases involved autoimmune etiology.
According to Zhao et al.’s classification [
2], patients with moderate GMC accounted for the majority (n = 59, 51.30%), while those with severe GMC accounted for 36.50%. With regard to Ye et al.’s classification [
1], the proportions of GMC patients with type B2, B3, and C1 GMC were 30.40%, 36.50%, and 19.10%, respectively. Patients with these three types of GMC, in accordance with Zhao et al.’s classification [
2], could be further categorized into either moderate or severe GMC. In addition, we determined the number of patients with patellofemoral dysplasia based on three indicators (SLFR, SA, and TT-TG). We found that abnormal SLFR, SA, and TT-TG were evident in 6, 23, and 15 cases, respectively. The majority of patients had normal femoral trochlea, which reduced the impact of confounding factors when exploring the correlation between GMC and patellofemoral instability (
Table 1).
All patients received arthroscopic GMC release [
6]. The follow-up rate was 100% (115/115) at one month and 94.8% (109/115) at three months after surgery. In addition, because of the excellent postoperative outcome of this operation, many patients are reluctant to come to the outpatient clinic for follow-up after three months, so longer follow-up is not possible. Limited hip movement was remarkably ameliorated after surgery; patients were able to cross their legs and squat down while closing their knees together (
Figure 4). In this study, most of the patients were aged 25–40 years and most were female. The benefits of arthroscopy, therefore, were clearly superior to open surgery for such patients (
Figure 5A). The median Q-angle, feet distance, knee flexion angle, and hip flexion angle, were 16°, 41 cm, 104°, and 125° before surgery, and 13°, 13 cm, 31°, and 76° after surgery, respectively. Preoperative and postoperative comparisons revealed statistically significant differences (non-parametric test,
p < 0.05). More cases were found in the B2, B3, and C1 types (
Figure 5).
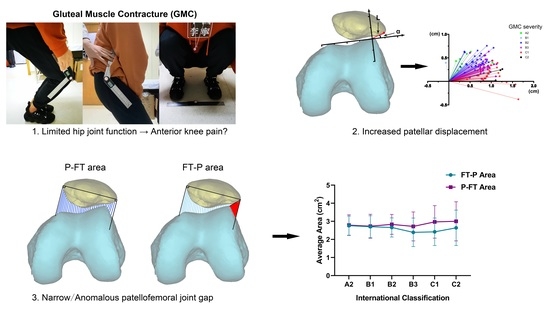
Measurement data of parameters related to patellofemoral instability in knee CT are presented in
Table 2. As the severity of GMC increased, the values of LPD, PCA, and PTA (reflecting the degree of patellar displacement and patellar tilt) also increased (B2 to C1 of the three: 0.46 to 0.65, 19.05 to 27.25, and 19.71 to 24.26, respectively); however, this trend was not notable, and the sensitivity was poor. However, changing trends were apparent for both LPFA and PFI. LPFA gradually declined (a negative number represented inward opening) and the proportion of abnormal PFI increased, thus suggesting that the proportion of lateral displacement of the patella and patellofemoral instability increased as the degree of contracture increased.
The novel indicators designed in this study, distance (L) and angle (α), based on a line connecting each of the highest points of the medial and lateral femoral condyles, underwent prominent changes; the higher the degree of contracture, the longer the L, and the smaller the α (
Table 2). Then, using the line connecting each of the highest points of the medial and lateral femoral condyles as an
X-axis, and using a line from the highest point of the lateral condyle as the
Y-axis, we established a coordinate system for L and α. This analysis showed that as the severity of GMC increased, the outermost point of the patella moved outward and downward. These findings indicated that more lateral displacement and tilt of the patella implies more serious patellar subluxation (
Figure 6A). Changes in the P-FT area and the FT-P area are presented in
Figure 6B; as GMC severity rose, the difference between these two areas became larger (
p = 0.000, B2 to C1, 0.17 cm
2 to 0.55 cm
2) (
Table 2).
As shown in
Table 3, while using Ye et al.’s classification [
1] as the dependent variable, we investigated the correlations between GMC severity and other relevant clinical and imaging parameters. Univariate ordered logistic regression analysis showed that a range of parameters were closely associated with GMC classification including body mass index (BMI), Preop-Q-angle, Preop-feet distance, Preop-knee flexion angle, Preop-hip flexion angle, the difference between the P-FT area and FT-P area, L, α, PTA, PFI, PCA, LPDm, and LPFA. Furthermore, multivariate analysis showed that BMI, Preop-feet distance, [P-FT area]-[FT-P area], and α were independent risk factors for the severity of GMC, in which the odds ratio (OR) or the difference in areas and Preop-feet distance was 1.074 and 1.145, respectively. This indicated that the greater these two parameters are, the more serious the possibility of GMC; α showed the opposite relationship. With respect to BMI (OR = 0.794), the smaller the weight, the higher the risk of severe GMC; this was consistent with clinical observations by our group in that most patients with severe GMC were thin.
Using [P-FT area]-[FT-P area] as the dependent variable, we investigated the associations of cross-sectional area between the patella and femur with other relevant clinical and imaging parameters of patellofemoral instability, as shown in
Table 4. Univariate analysis using GLMM showed that Q-angle, feet distance, knee flexion angle, hip flexion angle, Ye et al.’s classification, L, α, PTA, PFI, PCA, LPD, and LPFA were all significantly related to the difference between areas (
p < 0.10). Furthermore, as identified by multivariate analysis, feet distance, Ye et al.’s classification, L, PTA, PCA, and LPFA were all independent risk factors for the difference in areas. These results showed that when GMC was classified as type B3, the probability of an increase in area difference was elevated by 19.6%; when GMC was classified as type C1, this probability increased by 39.8%. Moreover, for every one-unit increase in L and PCA, the probability of an increase in area difference would be raised by 27.8% and 0.4%, respectively; an increase per unit in PTA and LPFA led to a reduction in the probability of increase in the area difference by 0.9% and 1.7%, respectively. Multivariate analysis showed that the differences in α, PFI, and LPD were not statistically significant (
p > 0.05). This may be attributed to the condition that the change in area differences is mainly dependent on the degree of patellar displacement and patellar tilt. These three indicators often only reflect a single factor change with regard to the patella (displacement or tilt).
4. Discussion
In the present study, the association between GMC and patellofemoral instability was investigated from clinical physical examination and imaging data. Multivariate analysis was conducted to investigate the impact of differing severities of GMC on patellofemoral instability by combining routine assessment parameters relating to patellofemoral instability and new assessment indicators designed by our research group (feet distance, L and α, and [P-FT area]-[FT-P area]). Few studies have performed detailed multivariate analysis on the association between GMC and patellofemoral instability; there is a need for direct data validation and it is particularly easy to ignore the impact of different severities of GMC. This causes risk with regard to the clinical decision-making process for GMC patients who have knee pain or patellar subluxation. Therefore, in this study, we specifically analyzed the association between GMC and patellofemoral instability. We also analyzed the reliability of each assessment indicator for patellofemoral instability in GMC patients. This is useful when making decisions related to the clinical assessment and therapeutic regimen of GMC patients who have patellofemoral instability.
In this study, most of the GMC patients sought medical treatment due to the limitation of range of motion (ROM) in the hips that affected daily life; most patients were women (
Table 1). It has been reported that GMC is more common in men than women [
18]; this opposes our current findings. This may be related to the scope of the study population and the statistical methodology used. Since each patient’s cognition of this disease differs and no large-scale multi-center investigations have been performed, we cannot learn the exact gender difference in the incidence rate of GMC. However, using our own statistical data, most patients who sought medical treatment were female; it is possible that young female patients pay more attention to their posture and hip ROM. This possibility was supported by the fact that our patients were mostly aged between 25 and 35 years (
Figure 5A). In addition, statistical analysis showed that BMI was significantly associated with the severity of GMC (
Table 3). However, whether patients with a lower BMI are indeed prone to more severe GMC cannot be further clarified. This is because many factors can influence the severity of GMC; it is also difficult to investigate and control for these factors. Our data indicate that young women (with a lower BMI) were associated with the highest hospital visitation rate. In addition, it is also possible that males, or stronger and more obese patients, have strong and abundant lower limb muscles. Therefore, the compensatory capability of these patients would be higher and the limitation of hip ROM would not be obvious, thus leading to a lower hospital visiting rate. This possibility requires further biomechanical studies.
In addition to the limitation of hip ROM, knee pain or knee discomfort after hypermobility occurred in about one-third of the GMC patients (
Table 1). Some of these patients saw a doctor due to anterior knee pain and were not diagnosed with GMC until further physical examination (probably because they had insufficient cognition of GMC in the early stage). According to some studies [
6,
7,
8,
9,
18], anterior knee pain is induced by GMC and can be relieved after GMC release. Previously, our research group found that the rate of patellofemoral instability was significantly higher in GMC patients, especially those accompanied by anterior knee pain; this pain was significantly improved after arthroscopic GMC release [
6]. A previous research group adopted arthroscopic GMC release combined with medial patellar retinaculum plication and lateral retinaculum release for the treatment of GMC accompanied by patellofemoral instability. These authors found that this combined form of surgery could effectively alleviate anterior knee pain caused by long-term GMC and reduced LPD when compared to arthroscopic GMC release alone [
9]. The most common contracture in GMC occurs in the iliotibial tract [
18]. From the anatomical perspective, contracture of the iliotibial tract and its fascia will induce LPD. Long-term patellofemoral malalignment will cause patellofemoral articular cartilage wear or osteoarthritis, thus inducing anterior knee pain or discomfort after hypermobility [
19]. Therefore, it is critical to correctly assess the condition of GMC and patellofemoral instability and identify congenital patellofemoral dysplasia when selecting the therapeutic regimen for GMC patients accompanied by patellofemoral instability.
The diagnosis and conditional assessment of GMC are primarily based on clinical physical examination and intraoperative arthroscopic assessment (
Figure 1 and
Figure 4). The classifications of Ye et al. [
1] and Zhao et al. [
2] are currently the most practical and highly recognized assessment criteria. As shown in
Table 1, most patients had moderate GMC; there were few patients with mild or highly severe GMC that cannot be released during surgery (classification of Ye et al. [
1]: A1, A2, B1, and C2). Since the main symptom of the vast majority of GMC patients is difficulty in knee squatting, we designed a simple assessment indicator for GMC (feet distance, knee flexion angle and hip flexion angle) (
Figure 1C). As shown in
Table 3, feet distance was clearly associated with the severity of GMC; the larger the feet distance, the more serious the GMC (OR = 1.145). This association with the severity of GMC showed no statistically significant difference between knee flexion angle and hip flexion angle. This is probably because both waist and calf muscles are needed when the patient stands, thus weakening the ability of the two indicators to reflect the severity of GMC. However, feet distance, knee flexion angle, and hip flexion angle were all obviously ameliorated after arthroscopic GMC release (
Figure 5B,D,E). Therefore, feet distance may serve as a simple assessment indicator for GMC in the clinic, although the corresponding relationship between feet distance and the severity of GMC requires further investigation.
First, it is important to assess congenital patellofemoral dysplasia (SLFR, SA, and TT-TG) for the assessment and analysis of patellofemoral instability. In this study, patients with congenital patellofemoral dysplasia were in the minority (
Table 1), and there was no direct relationship with the severity of GMC (
p > 0.05,
Table 3). The Dejour classification [
20,
21] is commonly used for femoral trochlear dysplasia, however, this classification may be affected by subjective factors and the boundary of this classification is not obvious in some cases. In fact, SLFR, SA, and TT-TG can reflect the status of trochlear development via objective data; therefore, the Dejour classification was not adopted in this study. It has been proven in many studies that patients with trochlear dysplasia are more prone to patellofemoral instability, thus inducing patellar subluxation or dislocation [
13,
15,
22,
23]. In the present study, we did not find a significant association between the three indicators and GMC. This created favorable conditions for the analysis of GMC-induced patellofemoral instability and reduced the impact of congenital factors.
Q-angle is the most common and simple assessment indicator for the clinical assessment of patellofemoral instability and patellar subluxation [
10,
24]. In previous studies, we found that arthroscopic GMC release could significantly reduce the Q-angle of GMC patients, thereby improving patellofemoral instability [
7]. The results of this study revealed that the preoperative Q-angle was significantly associated with the severity of GMC, but it was not an independent risk factor for the severity of GMC (
p > 0.05, multivariate analysis,
Table 3). Following arthroscopic GMC release, the Q-angle was significantly reduced; the more serious the GMC, the better the improvement (
Figure 5C). Therefore, it is evident that GMC has a significant impact on patellofemoral instability and patellar subluxation. However, the Q-angle is not a reliable independent assessment indicator and may be related to the less accurate measurement method of the Q-angle.
Currently, knee imaging examinations (CT or magnetic resonance imaging) remain the most reliable method with which to assess patellofemoral instability and patellar subluxation. The most commonly used assessment indicators include PTA, PFI, PCA, LPD, and LPFA [
6,
11,
12,
14]. PTA and LPFA have higher reference values for the assessment of the degree of patellar tilt. LPD directly reflects the degree of outward displacement of the patella. The degree of patellar tilt and the degree of outward displacement both exert a significant impact on PFI and PCA; these indicators are also highly sensitive for the assessment of patellofemoral instability. Of course, outward displacement and tilt of the patella often occur simultaneously and affect each other; these changes exert an impact on the above indicators, but in different manners. In this study, univariate analysis showed that PTA, PFI, PCA, LPD, and LPFA all showed statistically significant differences when compared across GMC patients with differing severities (
p < 0.05,
Table 3), thus suggesting that GMC has a significant impact on patellofemoral instability. Moreover, the more serious the GMC, the higher the risk of patellofemoral instability; this trend is clearly evident in
Table 2. The reference value for B2, B3, and C1 was high; this was due to the large sample size. However, the five indicators showed statistically significant differences in multivariate analysis, further suggesting that these indicators may have a mutual correlation or have a direct influence on each other. Of course, the influence of statistical errors (sample size, sample source, and measurement errors) cannot be excluded. When assessing patellofemoral instability, therefore, multiple indicators should be combined for analysis. It is also necessary to refer to the results of univariate analysis. A single indicator, or the blind use of multivariate models, may lead to inaccurate results.
Interestingly, the assessment indicators for GMC accompanied by patellofemoral instability that were designed by our group (the distance L and the angle α between the outermost point of the patella and the highest point of the lateral femoral condyle; [P-FT area]-[FT-P area]) were closely related to the severity of GMC (
Table 3). First, the assessment of patellar subluxation in patellofemoral instability is primarily used to assess the outward displacement and tilt of the patella; L and α appear to be new and reliable assessment indicators. A previous study showed that the lateral tilt of the patella had a greater impact on anterior knee pain in the patellofemoral joint than lateral displacement [
25]. Therefore, the combination of L and α is more valuable than LPD when assessing patellar subluxation. Multivariate analysis showed that α was clearly associated with the severity of GMC and served as an independent risk factor for the severity of GMC; the risk of severe GMC increased by 8.7% for each unit of decrease in α (OR = 0.913,
Table 3). At the same time, as shown in
Table 2 and
Figure 6, the more serious the GMC, the higher the proportion of patellofemoral instability or patellar subluxation (lateral displacement and lateral tilt). Therefore, L and α can serve as simple, intuitive, and reliable assessment indicators for GMC accompanied by patellofemoral instability in the clinic.
In addition, it has been shown that the patellofemoral joint space is of importance for the soft tissue balance in the patellofemoral joint and knee ROM [
26]. The outermost point of the normal patella and the highest point of the lateral femoral condyle are almost on the same sagittal plane or lie close to each other. Therefore, it can be speculated, based on our new indicators (P-FT area and FT-P area), that the difference between these two is relatively small, or may even be zero, in the normal patellofemoral joint. However, this will be significantly increased in the case of lateral tilt and lateral displacement of the patella. This area can reflect the gap between the patella and femur more comprehensively than points or lines. However, excessively small gaps or abnormal shapes (
Figure 3) will worsen the patellofemoral joint wear, thus inducing osteoarthritis.
Figure 6 and
Table 4 show that the difference between P-FT area and FT-P area was closely related to the severity of GMC, and that severe GMC (classification of Ye et al. [
1] and Preop-Feet distance) corresponded to a larger difference. Other indicators assessing lateral tilt and lateral displacement of the patella such as L, PTA, PCA, and LPFA were also closely correlated with this difference in area. Therefore, it is evident that the newly-designed indicators ([P-FT area]-[FT-P area]) can be used to verify the close association between GMC and patellofemoral instability, and may also represent reliable indicators to reflect the patellofemoral joint space and patellofemoral instability.
However, there are still some deficiencies in this study that need to be considered. First, the sample size was not large, especially for types A1, A2, B1, and C1. This was also a single-center study; therefore, our conclusions may include certain errors. Second, we used knee CT images in the extension position rather than that in the flexion position, thus leading to certain limitations when assessing the patellofemoral joint. Third, postoperative data by knee CT were not obtained; this was due to a range of factors including patient cooperation, hospitalization costs, demand for diagnosis and treatment, and the effects of CT radiation. Consequently, we were not able to investigate imaging indicators for the patellofemoral joint of GMC patients following surgery. However, a clinical physical examination (
Figure 4 and
Figure 5) was performed after surgery, and the Q-angle was used to indirectly assess the patellofemoral joint after surgery. In the future, our research group will address these deficiencies, expand the sample size and sources, and improve the assessment indicators to fully investigate the pathophysiological and biomechanical relationships between GMC and patellofemoral instability.