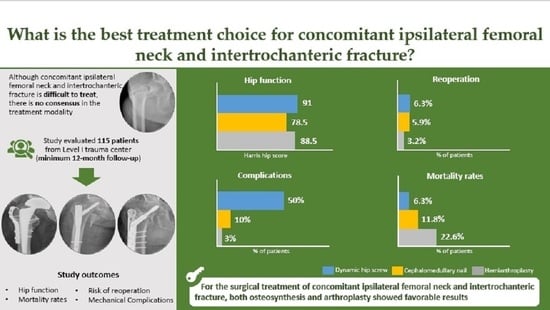
What Is the Best Treatment Choice for Concomitant Ipsilateral Femoral Neck and Intertrochanteric Fracture? A Retrospective Comparative Analysis of 115 Consecutive Patients
Abstract
:1. Introduction
2. Materials and Methods
2.1. Patient Selection
2.2. Surgical Technique
2.3. Data Collection
2.4. Statistical Analysis
3. Results
3.1. Patient Demographics and Perioperative Details
3.2. Postoperative Complications, Mortality Rates and Outcome
3.3. Trend in the Incidence of CIFNITF
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Chang, S.M.; Hou, Z.Y.; Hu, S.J.; Du, S.C. Intertrochanteric Femur Fracture Treatment in Asia: What We Know and What the World Can Learn. Orthop. Clin. N. Am. 2020, 51, 189–205. [Google Scholar] [CrossRef] [PubMed]
- Fischer, H.; Maleitzke, T.; Eder, C.; Ahmad, S.; Stöckle, U.; Braun, K.F. Management of proximal femur fractures in the elderly: Current concepts and treatment options. Eur. J. Med. Res. 2021, 26, 86. [Google Scholar] [CrossRef] [PubMed]
- Ahmed, A.Z.; Shaban, A.M.; Ilyas, I. Ipsilateral femoral neck and complex pertrochanteric fracture of the femur. J. Orthop. Trauma Surg. Relat. Res. 2020, 13, 33–36. [Google Scholar]
- An, H.S.; Wojcieszek, J.M.; Cooke, R.F.; Limbird, R.; Jackson, W.T. Simultaneous ipsilateral intertrochanteric and subcapital fracture of the hip. A case report. Orthopedics 1989, 12, 721–723. [Google Scholar] [CrossRef] [PubMed]
- Biesemans, S. Segmental Fractures of the Neck of Femur: Fix or Replace? Arthroplast. Today 2021, 8, 247–252. [Google Scholar] [CrossRef] [PubMed]
- Butt, M.F.; Dhar, S.A.; Hussain, A.; Gani Nu Kangoo, K.A.; Farooq, M. Femoral Neck Fracture with Ipsilateral Trochanteric Fracture: Is there room for Osteosynthesis? Internet J. Orthop. Surg. 2006, 5. [Google Scholar] [CrossRef]
- Cohen, I.; Rzetelny, V. Simultaneous ipsilateral pertrochanteric and subcapital fractures. Orthopedics 1999, 22, 535–536. [Google Scholar]
- Dhar, S.A.; Mir, M.R.; Butt, M.F.; Farooq, M.; Ali, M.F. Osteosynthesis for a T-shaped fracture of the femoral neck and trochanter: A case report. J. Orthop. Surg. 2008, 16, 257–259. [Google Scholar] [CrossRef] [Green Version]
- Isaacs, C.; Lawrence, B. Concomitant ipsilateral intertrochanteric and subcapital fracture of the hip. J. Orthop. Trauma 1993, 7, 146–148. [Google Scholar] [CrossRef]
- Khan, W.; Williams, R.; Hopwood, S.; Agarwal, S. Combined Intracapsular And Extracapsular Neck Of Femur Fractures Case Series, Literature Review And Management Recommendations. Open Orthop. J. 2017, 11, 600–608. [Google Scholar] [CrossRef] [Green Version]
- Kothari, S.; Prakash, A. Segmental femoral neck fracture in an elderly patient: A rare case report. Indian J. Orthop. Surg. 2019, 5, 162–164. [Google Scholar] [CrossRef]
- Kumar, R.; Khan, R.; Moholkar, K.; Smyth, H.; Borton, D. A rare combination fracture of the neck of femur. Eur. J. Orthop. Surg. Traumatol. 2001, 11, 59–61. [Google Scholar] [CrossRef]
- Kyle, R.F.; Ellis, T.J.; Templeman, D.C. Surgical Treatment of Intertrochanteric Hip Fractures With Associated Femoral Neck Fractures Using a Sliding Hip Screw. J. Orthop. Trauma 2005, 19, 1–4. [Google Scholar] [CrossRef]
- Lakshmanan, P.; Peehal, J.P. Management of an unusual intra- and extra-capsular subcapital femoral neck fracture. Acta Orthop. Belg. 2005, 71, 622–625. [Google Scholar] [PubMed]
- Loupasis, G.; Ntagiopoulos, P.G.; Asimakopoulos, A. Concomitant ipsilateral subcapital and intertrochanteric fractures of the femur: A case report. J. Med. Case Rep. 2010, 4, 363. [Google Scholar] [CrossRef] [Green Version]
- Neogi, D.S.; Ajay Kumar, K.V.; Trikha, V.; Yadav, C.S. Ipsilateral femoral neck and trochanter fracture. Indian J. Orthop. 2011, 45, 82–86. [Google Scholar] [CrossRef]
- Pemberton, D.J.; Kriebich, D.N.; Moran, C.G. Segmental fracture of the neck of the femur. Injury 1989, 20, 306–307. [Google Scholar] [CrossRef]
- Perry, D.C.; Scott, S.J. Concomitant ipsilateral intracapsular and extracapsular femoral neck fracture: A case report. J. Med. Case Rep. 2008, 2, 68. [Google Scholar] [CrossRef] [Green Version]
- Poulter, R.; Ashworth, M.J. Concomitant ipsilateral subcapital and intertrochanteric fractures of the femur. Inj. Extra 2007, 38, 88–89. [Google Scholar] [CrossRef] [Green Version]
- Saleeb, H.; Kanvinde, R.; Rahman, T. Literature review and case report: Current concepts for concomitant intra and extracapsular fractures of neck of femur in elderly patients. Trauma Case Rep. 2017, 8, 24–31. [Google Scholar] [CrossRef]
- Sayegh, F.E.; Karataglis, D.; Trapotsis, S.J.; Christoforides, J.E.; Pournaras, J.D. Concomitant Ipsilateral Pertrochanteric and Subcapital Fracture of the Proximal Femur. Eur. J. Trauma 2005, 31, 64–67. [Google Scholar] [CrossRef]
- Su, C.; Liu, Y.; Wu, P.; Yuan, J.; Lang, J.; Wu, C.; Zhang, Y.; Chen, L.; Chen, L. Ipsilateral femoral neck and intertrochanteric fractures with posterior dislocation of the hip: A report of two cases. J. Orthop. Surg. 2020, 28, 2309499019900449. [Google Scholar] [CrossRef] [PubMed]
- Tahir, M.; Lakkol, S.; Naique, S. Segmental neck of femur fractures: A unique case report of an ipsilateral subcapital, greater trochanteric and intertrochanteric fracture and proposed management algorithm. Int. J. Surg. Case Rep. 2014, 5, 277–281. [Google Scholar] [CrossRef] [Green Version]
- Taniguchi, D.; Fujiwara, H.; Kobashi, H.; Mori, G.; Yoshida, T.; Oda, R.; Kubo, T. Successful treatment of concomitant ipsilateral intracapsular and extracapsular hip fractures. Orthopedics 2013, 36, 837–839. [Google Scholar] [CrossRef] [Green Version]
- Taylor, P.R.; Hepple, S.; Stanley, D. Combination subcapital and intertrochanteric fractures of the femoral neck. Injury 1996, 27, 68–71. [Google Scholar] [CrossRef]
- Tong, D.K.; Zhou, D.X.; Zhong, X.X.; Zhou, Z.B.; Rui, B.Y.; Yue, F.; Peng, Z.D.; Guang, S.X.; Fang, Z.; Yan, G.; et al. Concomitant Ipsilateral Intracapsular and Extracapsular Hip Fractures Classification and Treatment A Multi-Hospital Experience. Clin. Surg. 2021, 5, 1–7. [Google Scholar]
- Videla-Ces, M.; Sales-Perez, J.M.; Giros-Torres, J.; Sanchez-Naves, R.; Videla, S. A retrospective cohort study of concomitant ipsilateral extra-capsular and intra-capsular fractures of the proximal femur. Are they casual findings or an undervalued reality? Injury 2017, 48, 1558–1564. [Google Scholar] [CrossRef] [PubMed]
- Vluggen, T.P.M.J.; van Vugt, R.; Boonen, B.; Keulen, M.H.F. Management of two-level proximal femoral fractures. BMJ Case Rep. 2021, 14, e240684. [Google Scholar] [CrossRef]
- Yoo, H.; Cho, Y.; Hwang, S. Outcomes of Combined Neck and Trochanter Fractures of the Femur Treated with Cephallomedullary Nail in Elderly. Hip Pelvis 2019, 31, 200–205. [Google Scholar] [CrossRef] [Green Version]
- Park, Y.C.; Um, K.S.; Hong, S.P.; Oh, C.W.; Kim, S.; Yang, K.H. Preoperative “Computed tomography capsular sign” for the detection of occult ipsilateral femoral neck fractures associated with femoral shaft fractures. Injury 2020, 51, 1051–1056. [Google Scholar] [CrossRef]
- Ito, J.; Takakubo, Y.; Sasaki, K.; Sasaki, J.; Owashi, K.; Takagi, M. Prevention of excessive postoperative sliding of the short femoral nail in femoral trochanteric fractures. Arch. Orthop. Trauma Surg. 2015, 135, 651–657. [Google Scholar] [CrossRef] [PubMed]
- John, B.; Sharma, A.; Mahajan, A.; Pandey, R. Tip-apex distance and other predictors of outcome in cephalomedullary nailing of unstable trochanteric fractures. J. Clin. Orthop. Trauma 2019, 10, S88–S94. [Google Scholar] [CrossRef] [PubMed]
- Cho, M.R.; Lee, J.H.; Kwon, J.B.; Do, J.S.; Chae, S.B.; Choi, W.-K. The Effect of Positive Medial Cortical Support in Reduction of Pertrochanteric Fractures with Posteromedial Wall Defect Using a Dynamic Hip Screw. Clin. Orthop. Surg. 2018, 10, 292–298. [Google Scholar] [CrossRef] [PubMed]
- Dhammi, I.; Jain, A.; Singh, A.; Rehan Ul, H.; Mishra, P.; Jain, S. Primary nonunion of intertrochanteric fractures of femur: An analysis of results of valgization and bone grafting. Indian J. Orthop. 2011, 45, 514–519. [Google Scholar] [CrossRef] [PubMed]
- Chan, D.S. Femoral Neck Fractures in Young Patients: State of the Art. J. Orthop. Trauma 2019, 33 (Suppl. S1), S7–S11. [Google Scholar] [CrossRef] [PubMed]
- Slobogean, G.P.; Sprague, S.A.; Scott, T.; McKee, M.; Bhandari, M. Management of young femoral neck fractures: Is there a consensus? Injury 2015, 46, 435–440. [Google Scholar] [CrossRef]
- Ma, H.H.; Chou, T.A.; Tsai, S.W.; Chen, C.F.; Wu, P.K.; Chen, W.M. Outcomes of internal fixation versus hemiarthroplasty for elderly patients with an undisplaced femoral neck fracture: A systematic review and meta-analysis. J. Orthop. Surg. Res. 2019, 14, 320. [Google Scholar] [CrossRef] [Green Version]
- Cheng, Y.X.; Sheng, X. Optimal surgical methods to treat intertrochanteric fracture: A Bayesian network meta-analysis based on 36 randomized controlled trials. J. Orthop. Surg. Res. 2020, 15, 402. [Google Scholar] [CrossRef]
- Hongku, N.; Woratanarat, P.; Nitiwarangkul, L.; Rattanasiri, S.; Thakkinstian, A. Fracture fixation versus hemiarthroplasty for unstable intertrochanteric fractures in elderly patients: A systematic review and network meta-analysis of randomized controlled trials. Orthop. Traumatol. Surg. Res. 2022, 108, 102838. [Google Scholar] [CrossRef]
- Huang, X.; Leung, F.; Xiang, Z.; Tan, P.Y.; Yang, J.; Wei, D.Q.; Yu, X. Proximal Femoral Nail versus Dynamic Hip Screw Fixation for Trochanteric Fractures: A Meta-Analysis of Randomized Controlled Trials. Sci. World J. 2013, 2013, 805805. [Google Scholar] [CrossRef] [Green Version]
- Parker, M.J.; Bowers, T.R.; Pryor, G.A. Sliding hip screw versus the Targon PF nail in the treatment of trochanteric fractures of the hip. J. Bone Jt. Surg. Br. 2012, 94-B, 391–397. [Google Scholar] [CrossRef] [PubMed]
- Radford, P.J.; Needoff, M.; Webb, J.K. A prospective randomised comparison of the dynamic hip screw and the gamma locking nail. J. Bone Jt. Surg. Br. 1993, 75-B, 789–793. [Google Scholar] [CrossRef] [PubMed]
- Palm, H.; Jacobsen, S.; Sonne-Holm, S.; Gebuhr, P.; Hip Fracture Study, G. Integrity of the lateral femoral wall in intertrochanteric hip fractures: An important predictor of a reoperation. J. Bone Jt. Surg. Am. 2007, 89, 470–475. [Google Scholar]
- Kyriakopoulos, G.; Panagopoulos, A.; Pasiou, E.; Kourkoulis, S.K.; Diamantakos, I.; Anastopoulos, G.; Tserpes, K.; Tatani, I.; Lakoumentas, J.; Megas, P. Optimizing fixation methods for stable and unstable intertrochanteric hip fractures treated with sliding hip screw or cephalomedullary nailing: A comparative biomechanical and finite element analysis study. Injury 2022, in press. [Google Scholar] [CrossRef]
- Downey, C.; Kelly, M.; Quinlan, J.F. Changing trends in the mortality rate at 1-year post hip fracture—A systematic review. World J. Orthop. 2019, 10, 166–175. [Google Scholar] [CrossRef]





| All (n = 115) | CMN (n = 68) | DHS (n = 16) | HR (n = 31) | p Value | ||||
|---|---|---|---|---|---|---|---|---|
| CMN vs. DHS | CMN vs. HR | DHS vs. HR | Overall | |||||
| Age | 79 (40 to 95) | 47 (40 to 90) | 79.5 (42 to 94) | 81 (56 to 95) | 0.669 | 0.125 | 0.574 | 0.338 |
| Female | 73 (63.5%) | 39 (57.4%) | 9 (56.3%) | 25 (80.6%) | 0.936 | 0.025 | 0.096 | 0.075 |
| BMD (T-score) | −3.3 (−7.2 to 0.8) | −3.2 (−4.9 to 0.8) | −3.9 (−4.6 to −3.1) | −3.9 (−7.2 to −0.5) | 0.112 | 0.197 | 0.881 | 0.077 |
| Op time (min) | 92.7 (33.0) | 85.6 (31.1) | 94.7 (22.3) | 107.3 (37.2) | 0.174 | 0.003 | 0.025 | 0.021 |
| Anesthesia a | 53 (46.1%) | 36 (52.9%) | 6 (37.5%) | 11 (35.5%) | 0.266 | 0.107 | 0.892 | 0.236 |
| LOS (day) | 14 (3 to 125) | 14 (3 to 119) | 16 (6 to 55) | 15 (7 to 125) | 0.249 | 0.280 | 0.991 | 0.250 |
| All Patients (n = 115) | CMN (n = 68) | DHS (n = 16) | Arthroplasty (n = 31) | p Value | |
|---|---|---|---|---|---|
| Osteosynthesis | |||||
| ONFH | 7 (10.3%) | 2 (12.5%) | N/A | 0.679 | |
| Cut-out | 2 (2.9%) | 0 (0%) | N/A | 1.000 | |
| Cut-through | 1 (1.5%) | 0 (0%) | N/A | 1.000 | |
| Excessive sliding | 1 (1.5%) | 4 (25.0%) | N/A | 0.004 | |
| Nonunion | 3 (4.4%) | 4 (25.0%) | N/A | 0.022 | |
| Arthroplasty | |||||
| Dislocation | N/A | N/A | 1 (3.2%) | N/A | |
| Implant loosening | N/A | N/A | 0 (0%) | N/A | |
| Total | |||||
| HO | 5 (4.3%) | 4 (5.9%) | 0 (0%) | 1 (3.2%) | 1.000 |
| VTE | 4 (3.5%) | 4 (5.9%) | 0 (0%) | 0 (0%) | 0.459 |
| Infection | 6 (5.2%) | 2 (2.9%) | 1 (6.3%) | 3 (9.7%) | 0.269 |
| Revision surgery | 6 (5.2%) | 4 (5.9%) | 1 (6.3%) | 1 (3.2%) | 1.000 |
| In-hospital mortality | 5 (4.3%) | 3 (4.4%) | 0 (0%) | 2 (6.5%) | 0.674 |
| 1-year mortality | 16 (13.9%) | 8 (11.8%) | 1 (6.3%) | 7 (22.6%) | 0.293 |
| HHS at final f/u | 84.2 (65–95) | 73.4 (65–91) | 89.5 (85–95) | 87.2 (85–95) | 0.819 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kim, H.S.; Lee, D.K.; Mun, K.U.; Moon, D.H.; Kim, C.-H. What Is the Best Treatment Choice for Concomitant Ipsilateral Femoral Neck and Intertrochanteric Fracture? A Retrospective Comparative Analysis of 115 Consecutive Patients. J. Pers. Med. 2022, 12, 1908. https://doi.org/10.3390/jpm12111908
Kim HS, Lee DK, Mun KU, Moon DH, Kim C-H. What Is the Best Treatment Choice for Concomitant Ipsilateral Femoral Neck and Intertrochanteric Fracture? A Retrospective Comparative Analysis of 115 Consecutive Patients. Journal of Personalized Medicine. 2022; 12(11):1908. https://doi.org/10.3390/jpm12111908
Chicago/Turabian StyleKim, Han Soul, Dong Keun Lee, Ki Uk Mun, Dou Hyun Moon, and Chul-Ho Kim. 2022. "What Is the Best Treatment Choice for Concomitant Ipsilateral Femoral Neck and Intertrochanteric Fracture? A Retrospective Comparative Analysis of 115 Consecutive Patients" Journal of Personalized Medicine 12, no. 11: 1908. https://doi.org/10.3390/jpm12111908