Inflammatory Microenvironment in Early Non-Small Cell Lung Cancer: Exploring the Predictive Value of Radiomics
Abstract
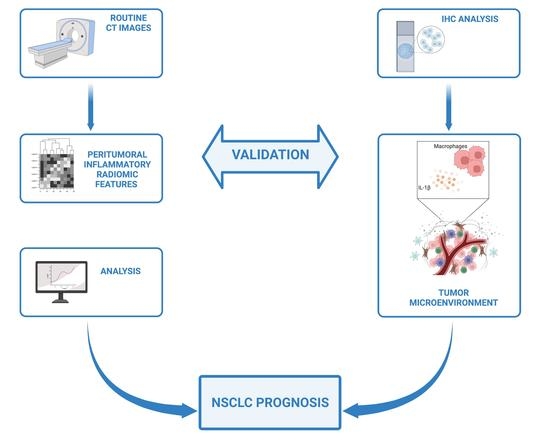
:Simple Summary
Abstract
1. Introduction
2. Materials and Methods
2.1. Patient Screening
2.2. Immunohistochemistry in Tissue Specimens
2.3. Radiomic Feature Extraction on CT Images
2.4. Statistical Analysis
3. Results
3.1. Clinical Outcomes
3.2. Biological Outcomes
3.3. Radiomic Outcomes
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Novello, S.; Asamura, H.; Bazan, J.; Carbone, D.; Goldstraw, P.; Grunenwald, D.; Ricardi, U.; Vansteenkiste, J. Early Stage Lung Cancer: Progress in the Last 40 Years. J. Thorac. Oncol. 2014, 9, 1434–1442. [Google Scholar] [CrossRef] [Green Version]
- Nagasaka, M.; Gadgeel, S.M. Role of chemotherapy and targeted therapy in early-stage non-small cell lung cancer. Expert Rev. Anticancer Ther. 2017, 18, 63–70. [Google Scholar] [CrossRef]
- Soares, M.; Antunes, L.; Redondo, P.; Borges, M.; Hermans, R.; Patel, D.; Grimson, F.; Munro, R.; Chaib, C.; Lacoin, L.; et al. Treatment and outcomes for early non-small-cell lung cancer: A retrospective analysis of a Portuguese hospital database. Lung Cancer Manag. 2021, 10, LMT46. [Google Scholar] [CrossRef]
- Fan, H.; Shao, Z.-Y.; Xiao, Y.-Y.; Xie, Z.-H.; Chen, W.; Xie, H.; Qin, G.-Y.; Zhao, N.-Q. Incidence and survival of non-small cell lung cancer in Shanghai: A population-based cohort study. BMJ Open 2015, 5, e009419. [Google Scholar] [CrossRef] [Green Version]
- Ekman, S.; Horvat, P.; Rosenlund, M.; Kejs, A.M.; Patel, D.; Juarez-Garcia, A.; Lacoin, L.; Daumont, M.J.; Penrod, J.R.; Brustugun, O.T.; et al. Epidemiology and Survival Outcomes for Patients with NSCLC in Scandinavia in the Preimmunotherapy Era: A SCAN-LEAF Retrospective Analysis from the I-O Optimise Initiative. JTO Clin. Res. Rep. 2021, 2, 100165. [Google Scholar] [CrossRef]
- Giraldo, N.A.; Sanchez-Salas, R.; Peske, J.D.; Vano, Y.A.; Becht, E.; Petitprez, F.; Validire, P.; Ingels, A.; Cathelineau, X.; Fridman, W.H.; et al. The clinical role of the TME in solid cancer. Br. J. Cancer 2018, 120, 45–53. [Google Scholar] [CrossRef]
- Missiroli, S.; Perrone, M.; Boncompagni, C.; Borghi, C.; Campagnaro, A.; Marchetti, F.; Anania, G.; Greco, P.; Fiorica, F.; Pinton, P.; et al. Targeting the NLRP3 Inflammasome as a New Therapeutic Option for Overcoming Cancer. Cancers 2021, 13, 2297. [Google Scholar] [CrossRef]
- Edge, S.B.; Compton, C.C. The American Joint Committee on Cancer: The 7th Edition of the AJCC Cancer Staging Manual and the Future of TNM. Ann. Surg. Oncol. 2010, 17, 1471–1474. [Google Scholar] [CrossRef] [PubMed]
- Charlson, M.; Szatrowski, T.P.; Peterson, J.; Gold, J. Validation of a combined comorbidity index. J. Clin. Epidemiol. 1994, 47, 1245–1251. [Google Scholar] [CrossRef]
- Novello, S.; Barlesi, F.; Califano, R.; Cufer, T.; Ekman, S.; Levra, M.G.; Kerr, K.; Popat, S.; Reck, M.; Senan, S.; et al. Metastatic non-small-cell lung cancer: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann. Oncol. 2016, 27, v1–v27. [Google Scholar] [CrossRef] [PubMed]
- DeMars, R.; Chang, C.C.; Rudersdorf, R.A. Dissection of the D-region of the human major histocompatibility complex by means of induced mutations in a lymphoblastoid cell line. Hum. Immunol. 1983, 8, 123–139. [Google Scholar] [CrossRef]
- Gering, D.; Sun, K.; Avery, A.; Chylla, R.; Vivekanandan, A.; Kohli, L.; Knapp, H.; Paschke, B.; Young-Moxon, B.; King, N.; et al. Semi-automatic Brain Tumor Segmentation by Drawing Long Axes on Multi-plane Reformat. In Brainlesion: Glioma, Multiple Sclerosis, Stroke and Traumatic Brain Injuries; Springer: Cham, Switzerland, 2019; pp. 441–455. [Google Scholar]
- Gering, D.; Kotrotsou, A.; Young-Moxon, B.; Miller, N.; Avery, A.; Kohli, L.; Knapp, H.; Hoffman, J.; Chylla, R.; Peitzman, L.; et al. Measuring Efficiency of Semi-automated Brain Tumor Segmentation by Simulating User Interaction. Front. Comput. Neurosci. 2020, 14, 32. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fusco, R.; Granata, V.; Mazzei, M.A.; Di Meglio, N.; Del Roscio, D.; Moroni, C.; Monti, R.; Cappabianca, C.; Picone, C.; Neri, E.; et al. Quantitative imaging decision support (QIDSTM) tool consistency evaluation and radiomic analysis by means of 594 metrics in lung carcinoma on chest CT scan. Cancer Control 2021, 28, 107327482098578. [Google Scholar] [CrossRef]
- Reginelli, A.; Belfiore, M.P.; Monti, R.; Cozzolino, I.; Costa, M.; Vicidomini, G.; Grassi, R.; Morgillo, F.; Urraro, F.; Nardone, V.; et al. The texture analysis as a predictive method in the assessment of the cytological specimen of CT-guided FNAC of the lung cancer. Med Oncol. 2020, 37, 54. [Google Scholar] [CrossRef]
- Zwanenburg, A.; Vallières, M.; Abdalah, M.A.; Aerts, H.J.W.L.; Andrearczyk, V.; Apte, A.; Ashrafinia, S.; Bakas, S.; Beukinga, R.J.; Boellaard, R.; et al. The Image Biomarker Standardization Initiative: Standardized Quantitative Radiomics for High-Throughput Image-based Phenotyping. Radiology 2020, 295, 328–338. [Google Scholar] [CrossRef] [Green Version]
- Kaplan, E.L.; Meier, P. Nonparametric Estimation from Incomplete Observations. J. Am. Stat. Assoc. 1958, 53, 457. [Google Scholar] [CrossRef]
- Chen, Y.; Song, Y.; Du, W.; Gong, L.; Chang, H.; Zou, Z. Tumor-associated macrophages: An accomplice in solid tumor progression. J. Biomed. Sci. 2019, 26, 78. [Google Scholar] [CrossRef]
- Wu, T.; Dai, Y. Tumor microenvironment and therapeutic response. Cancer Lett. 2016, 387, 61–68. [Google Scholar] [CrossRef]
- Takebe, N.; McShane, L.; Conley, B. Exceptional responders—Discovering predictive biomarkers. Nat. Rev. Clin. Oncol. 2015, 12, 132–134. [Google Scholar] [CrossRef]
- Menon, H.; Ramapriyan, R.; Cushman, T.R.; Verma, V.; Kim, H.H.; Schoenhals, J.E.; Atalar, C.; Selek, U.; Chun, S.G.; Chang, J.Y.; et al. Role of Radiation Therapy in Modulation of the Tumor Stroma and Microenvironment. Front. Immunol. 2019, 10, 193. [Google Scholar] [CrossRef] [Green Version]
- Greten, F.R.; Grivennikov, S.I. Inflammation and Cancer: Triggers, Mechanisms, and Consequences. Immunity 2019, 51, 27–41. [Google Scholar] [CrossRef]
- Schroder, K.; Tschopp, J. The Inflammasomes. Cell 2010, 140, 821–832. [Google Scholar] [CrossRef] [Green Version]
- Voronov, E.; Apte, R.N. Targeting the Tumor Microenvironment by Intervention in Interleukin-1 Biology. Curr. Pharm. Des. 2017, 23, 4893–4905. [Google Scholar] [CrossRef]
- Betjes, M.G.; Haks, M.C.; Tuk, C.W.; Beelen, R.H. Monoclonal Antibody EBM11 (Anti-CD68) Discriminates between Dendritic Cells and Macrophages after Short-Term Culture. Immunobiology 1991, 183, 79–87. [Google Scholar] [CrossRef]
- Van Griethuysen, J.J.M.; Fedorov, A.; Parmar, C.; Hosny, A.; Aucoin, N.; Narayan, V.; Beets-Tan, R.G.H.; Fillion-Robin, J.-C.; Pieper, S.; Aerts, H.J.W.L. Computational Radiomics System to Decode the Radiographic Phenotype. Cancer Res. 2017, 77, e104–e107. [Google Scholar] [CrossRef] [Green Version]
- Karimi, R.; Tornling, G.; Forsslund, H.; Mikko, M.; Wheelock, M.; Nyrén, S.; Sköld, C.M. Lung density on high resolution computer tomography (HRCT) reflects degree of inflammation in smokers. Respir. Res. 2014, 15, 23. [Google Scholar] [CrossRef] [Green Version]
- Liu, Y.; Cao, X. Characteristics and Significance of the Pre-metastatic Niche. Cancer Cell 2016, 30, 668–681. [Google Scholar] [CrossRef] [Green Version]
- Marien, E.; Hillen, A.; Vanderhoydonc, F.; Swinnen, J.V.; Velde, G.V. Longitudinal microcomputed tomography-derived biomarkers for lung metastasis detection in a syngeneic mouse model: Added value to bioluminescence imaging. Lab. Investig. 2016, 97, 24–33. [Google Scholar] [CrossRef]
- Sun, R.; Limkin, E.J.; Vakalopoulou, M.; Dercle, L.; Champiat, S.; Han, S.R.; Verlingue, L.; Brandao, D.; Lancia, A.; Ammari, S.; et al. A radiomics approach to assess tumour-infiltrating CD8 cells and response to anti-PD-1 or anti-PD-L1 immunotherapy: An imaging biomarker, retrospective multicohort study. Lancet Oncol. 2018, 19, 1180–1191. [Google Scholar] [CrossRef]





| All Patients Stage I (n = 35) | Long Survival Group (n = 8) | Short Survival Group (n = 7) | |
|---|---|---|---|
| age (mean, range) | 72 (42–84) | 72.4 (66–80) | 73.6 (65–78) |
| male/female | 27/8 | 4/4 | 2/5 |
| ECOG 0 | 20 (57.1%) | 8 (100%) | 7 (100%) |
| ECOG 1 | 14 (40%) | - | - |
| ECOG 2 | 1 (2.9%) | - | - |
| Charlson index (mean, range) | 4 (2–8) | ||
| adenocarcinoma | 20 (57.1%) | 5 (62.5%) | 5 (71.4%) |
| squamous cell carcinoma | 15 (42.9%) | 3 (37.5%) | 2 (28.6%) |
| grading G1 | 7 (20%) | 1 (12.5%) | 2 (28.6%) |
| grading G2 | 22 (62.8%) | 6 (75%) | 4 (57.1%) |
| grading G3 | 6 (17.2%) | 1 (12.5%) | 1 (14.3%) |
| EGFR mutations | 12 (34.3%) | 4 (50%) | 4 (57.1%) |
| Stage Ia | 20 (57.1%) | 4 (50%) | 5 (71.4%) |
| Stage Ib | 15 (42.9%) | 4 (50%) | 2 (28.6%) |
| Surgery/Stereotactic Radiotherapy | 32/3 | 8/0 | 7/0 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Perrone, M.; Raimondi, E.; Costa, M.; Rasetto, G.; Rizzati, R.; Lanza, G.; Gafà, R.; Cavallesco, G.; Tamburini, N.; Maniscalco, P.; et al. Inflammatory Microenvironment in Early Non-Small Cell Lung Cancer: Exploring the Predictive Value of Radiomics. Cancers 2022, 14, 3335. https://doi.org/10.3390/cancers14143335
Perrone M, Raimondi E, Costa M, Rasetto G, Rizzati R, Lanza G, Gafà R, Cavallesco G, Tamburini N, Maniscalco P, et al. Inflammatory Microenvironment in Early Non-Small Cell Lung Cancer: Exploring the Predictive Value of Radiomics. Cancers. 2022; 14(14):3335. https://doi.org/10.3390/cancers14143335
Chicago/Turabian StylePerrone, Mariasole, Edoardo Raimondi, Matilde Costa, Gianluca Rasetto, Roberto Rizzati, Giovanni Lanza, Roberta Gafà, Giorgio Cavallesco, Nicola Tamburini, Pio Maniscalco, and et al. 2022. "Inflammatory Microenvironment in Early Non-Small Cell Lung Cancer: Exploring the Predictive Value of Radiomics" Cancers 14, no. 14: 3335. https://doi.org/10.3390/cancers14143335