Stimuli-Responsive Hydrogels for Cancer Treatment: The Role of pH, Light, Ionic Strength and Magnetic Field
Abstract
:Simple Summary
Abstract
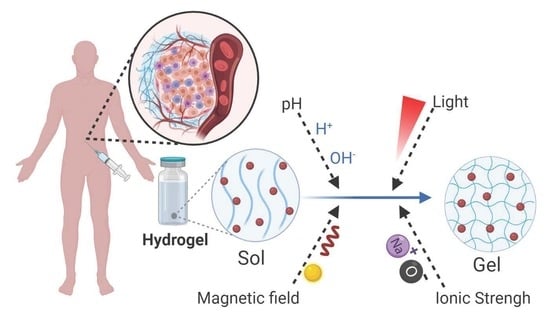
1. Introduction
2. Hydrogels for Biomedical Applications
3. Classification of Hydrogels
4. Stimuli-Responsive Hydrogels
4.1. pH-Sensitive Hydrogels
4.2. Photosensitive Hydrogels
4.3. Ionic Strength and Magnetic-Responsive Hydrogels
4.4. Dual-Responsive Hydrogels
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Bray, F.; Ferlay, J.; Soerjomataram, I.; Siegel, R.L.; Torre, L.A.; Jemal, A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J. Clin. 2018, 68, 394–424. [Google Scholar] [CrossRef] [Green Version]
- Lowenthal, R.M.; Eaton, K. Toxicity of chemotherapy. Hematol. Oncol. Clin. N. Am. 1996, 10, 967–990. [Google Scholar] [CrossRef]
- Chakraborty, S.; Rahman, T. The difficulties in cancer treatment. Ecancermedicalscience 2012, 6, 1–5. [Google Scholar]
- Schirrmacher, V. From chemotherapy to biological therapy: A review of novel concepts to reduce the side effects of systemic cancer treatment (Review). Int. J. Oncol. 2019, 54, 407–419. [Google Scholar] [PubMed]
- National Cancer Institute. Dictionary of Cancer Terms Definition of Local Therapy. Available online: https://www.cancer.gov/publications/dictionaries/cancer-terms/def/local-therapy (accessed on 20 November 2020).
- Chai, Q.; Jiao, Y.; Yu, X. Hydrogels for Biomedical Applications: Their Characteristics and the Mechanisms behind Them. Gels 2017, 3, 6. [Google Scholar] [CrossRef] [Green Version]
- Caló, E.; Khutoryanskiy, V.V. Biomedical applications of hydrogels: A review of patents and commercial products. Eur. Polym. J. 2015, 65, 252–267. [Google Scholar] [CrossRef] [Green Version]
- Peña, B.; Laughter, M.; Jett, S.; Rowland, T.J.; Taylor, M.R.G.; Mestroni, L.; Park, D. Injectable Hydrogels for Cardiac Tissue Engineering. Macromol. Biosci. 2018, 18, e1800079. [Google Scholar] [CrossRef] [PubMed]
- Vega, S.L.; Kwon, M.Y.; Burdick, J.A. Recent advances in hydrogels for cartilage tissue engineering. Eur. Cells Mater. 2017, 33, 59–75. [Google Scholar] [CrossRef] [PubMed]
- Tavakoli, S.; Klar, A.S. Advanced hydrogels as wound dressings. Biomolecules 2020, 10, 1169. [Google Scholar] [CrossRef]
- Wei, W.; Li, H.; Yin, C.; Tang, F. Research progress in the application of in situ hydrogel system in tumor treatment. Drug Deliv. 2020, 27, 460–468. [Google Scholar] [CrossRef] [Green Version]
- de la Puente, P.; Fettig, N.; Luderer, M.J.; Jin, A.; Shah, S.; Muz, B.; Kapoor, V.; Goddu, S.M.; Salama, N.N.; Tsien, C.; et al. Injectable Hydrogels for Localized Chemotherapy and Radiotherapy in Brain Tumors. J. Pharm. Sci. 2018, 107, 922–933. [Google Scholar] [CrossRef]
- Qu, J.; Zhao, X.; Liang, Y.; Zhang, T.; Ma, P.X.; Guo, B. Antibacterial adhesive injectable hydrogels with rapid self-healing, extensibility and compressibility as wound dressing for joints skin wound healing. Biomaterials 2018, 183, 185–199. [Google Scholar] [CrossRef]
- Persi, E.; Duran-frigola, M.; Damaghi, M.; Roush, W.R.; Aloy, P.; Cleveland, J.L.; Gillies, R.J.; Ruppin, E. Systems analysis of intracellular pH vulnerabilities for cancer therapy. Nat. Commun. 2018, 9. [Google Scholar] [CrossRef]
- Bair, R.J.; Bair, E.; Viswanathan, A.N. A radiopaque polymer hydrogel used as a fiducial marker in gynecologic-cancer patients receiving brachytherapy. Brachytherapy 2015, 14, 876–880. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Organ-Sparing with TraceIT® for Rectal Cancer Radiotherapy. Available online: https://clinicaltrials.gov/ct2/show/NCT03258541 (accessed on 20 November 2020).
- te Velde, B.L.; Westhuyzen, J.; Awad, N.; Wood, M.; Shakespeare, T.P. Late toxicities of prostate cancer radiotherapy with and without hydrogel SpaceAOR insertion. J. Med. Imaging Radiat. Oncol. 2019, 63, 836–841. [Google Scholar] [CrossRef] [PubMed]
- Das, A.K.; Gavel, P.K. Low molecular weight self-assembling peptide-based materials for cell culture, antimicrobial, anti-inflammatory, wound healing, anticancer, drug delivery, bioimaging and 3D bioprinting applications. Soft Matter 2020, 16, 10065–10095. [Google Scholar] [CrossRef] [PubMed]
- Draper, E.R.; Adams, D.J. Low-Molecular-Weight Gels: The State of the Art. Chem 2017, 3, 390–410. [Google Scholar] [CrossRef] [Green Version]
- Ahmed, E.M. Hydrogel: Preparation, characterization, and applications: A review. J. Adv. Res. 2015, 6, 105–121. [Google Scholar] [CrossRef] [Green Version]
- Hu, W.; Wang, Z.; Xiao, Y.; Zhang, S.; Wang, J. Advances in crosslinking strategies of biomedical hydrogels. Biomater. Sci. 2019, 7, 843–855. [Google Scholar] [CrossRef]
- Siqueira, N.M.; Cirne, M.F.R.; Immich, M.F.; Poletto, F. Stimuli-responsive polymeric hydrogels and nanogels for drug delivery applications. In Stimuli Responsive Polymeric Nanocarriers for Drug Delivery Applications: Volume 1: Types and Triggers; Makhlouf, A.S.H., Abu-Thabit, N.Y., Eds.; Elsevier Ltd.: Duxford, UK, 2018; pp. 343–374. [Google Scholar]
- Russo, E.; Villa, C. Poloxamer hydrogels for biomedical applications. Pharmaceutics 2019, 11, 671. [Google Scholar] [CrossRef] [Green Version]
- Kumar, A.; Han, S.S. PVA-based hydrogels for tissue engineering: A review. Int. J. Polym. Mater. Polym. Biomater. 2017, 66, 159–182. [Google Scholar] [CrossRef]
- Choi, J.R.; Yong, K.W.; Choi, J.Y.; Cowie, A.C. Recent advances in photo-crosslinkable hydrogels for biomedical applications. Biotechniques 2019, 66, 40–53. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Akhtar, M.F.; Hanif, M.; Ranjha, N.M. Methods of synthesis of hydrogels … A review. Saudi Pharm. J. 2016, 24, 554–559. [Google Scholar] [CrossRef] [Green Version]
- Liu, J.; Huang, Y.; Kumar, A.; Tan, A.; Jin, S.; Mozhi, A.; Liang, X.J. pH-Sensitive nano-systems for drug delivery in cancer therapy. Biotechnol. Adv. 2014, 32, 693–710. [Google Scholar] [CrossRef] [PubMed]
- Li, J.; Mooney, D.J. Designing hydrogels for controlled drug delivery. Nat. Rev. Mater. 2016, 1, 16071. [Google Scholar] [CrossRef]
- Rizwan, M.; Yahya, R.; Hassan, A.; Yar, M.; Azzahari, A.D.; Selvanathan, V.; Sonsudin, F.; Abouloula, C.N. pH sensitive hydrogels in drug delivery: Brief history, properties, swelling, and release mechanism, material selection and applications. Polymers 2017, 9, 225. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tanaka, M.; Nakahata, M.; Linke, P.; Kaufmann, S. Stimuli-responsive hydrogels as a model of the dynamic cellular microenvironment. Polym. J. 2020, 52, 861–870. [Google Scholar] [CrossRef]
- Sakiyama, T.; Takata, H.; Toga, T.; Nakanishi, K. pH-sensitive shrinking of a dextran sulfate/chitosan complex gel and its promotion effect on the release of polymeric substances. J. Appl. Polym. Sci. 2001, 81, 667–674. [Google Scholar] [CrossRef]
- Gierszewska, M.; Ostrowska-Czubenko, J.; Chrzanowska, E. pH-responsive chitosan/alginate polyelectrolyte complex membranes reinforced by tripolyphosphate. Eur. Polym. J. 2018, 101, 282–290. [Google Scholar] [CrossRef]
- Qu, J.; Zhao, X.; Ma, P.X.; Guo, B. pH-responsive self-healing injectable hydrogel based on N-carboxyethyl chitosan for hepatocellular carcinoma therapy. Acta Biomater. 2017, 58, 168–180. [Google Scholar] [CrossRef] [PubMed]
- Chang, G.; Chen, Y.; Li, Y.; Li, S.; Huang, F.; Shen, Y.; Xie, A. Self-healable hydrogel on tumor cell as drug delivery system for localized and effective therapy. Carbohydr. Polym. 2015, 122, 336–342. [Google Scholar] [CrossRef]
- Kasiński, A.; Zielińska-Pisklak, M.; Oledzka, E.; Sobczak, M. Smart hydrogels—Synthetic stimuli-responsive antitumor drug release systems. Int. J. Nanomed. 2020, 15, 4541–4572. [Google Scholar] [CrossRef]
- Puranik, A.S.; Pao, L.P.; White, V.M.; Peppas, N.A. In Vitro Evaluation of pH-Responsive Nanoscale Hydrogels for the Oral Delivery of Hydrophobic Therapeutics. Ind. Eng. Chem. Res. 2016, 55, 10576–10590. [Google Scholar] [CrossRef]
- Lin, X.; Miao, L.; Wang, X.; Tian, H. Design and evaluation of pH-responsive hydrogel for oral delivery of amifostine and study on its radioprotective effects. Colloids Surf. B Biointerfaces 2020, 195, 111200. [Google Scholar] [CrossRef]
- Anirudhan, T.S.; Mohan, A.M. Novel pH switchable gelatin based hydrogel for the controlled delivery of the anti-cancer drug 5-fluorouracil. RSC Adv. 2014, 4, 12109–12118. [Google Scholar] [CrossRef]
- Rezk, A.I.; Obiweluozor, F.O.; Choukrani, G.; Park, C.H.; Kim, C.S. Drug release and kinetic models of anticancer drug (BTZ) from a pH-responsive alginate polydopamine hydrogel: Towards cancer chemotherapy. Int. J. Biol. Macromol. 2019, 141, 388–400. [Google Scholar] [CrossRef]
- Solomevich, S.O.; Bychkovsky, P.M.; Yurkshtovich, T.L.; Golub, N.V.; Mirchuk, P.Y.; Revtovich, M.Y.; Shmak, A.I. Biodegradable pH-sensitive prospidine-loaded dextran phosphate based hydrogels for local tumor therapy. Carbohydr. Polym. 2019, 226, 115308. [Google Scholar] [CrossRef]
- Muzzalupo, R.; Tavano, L.; Rossi, C.O.; Picci, N.; Ranieri, G.A. Novel pH sensitive ferrogels as new approach in cancer treatment: Effect of the magnetic field on swelling and drug delivery. Colloids Surf. B Biointerfaces 2015, 134, 273–278. [Google Scholar] [CrossRef] [PubMed]
- Raza, F.; Zhu, Y.; Chen, L.; You, X.; Zhang, J.; Khan, A.; Khan, M.W.; Hasnat, M.; Zafar, H.; Wu, J.; et al. Paclitaxel-loaded pH responsive hydrogel based on self-assembled peptides for tumor targeting. Biomater. Sci. 2019, 7, 2023–2036. [Google Scholar] [CrossRef]
- Liao, W.C.; Lilienthal, S.; Kahn, J.S.; Riutin, M.; Sohn, Y.S.; Nechushtai, R.; Willner, I. PH-and ligand-induced release of loads from DNA-acrylamide hydrogel microcapsules. Chem. Sci. 2017, 8, 3362–3373. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Liang, Y.; Zhao, X.; Ma, P.X.; Guo, B.; Du, Y.; Han, X. pH-responsive injectable hydrogels with mucosal adhesiveness based on chitosan-grafted-dihydrocaffeic acid and oxidized pullulan for localized drug delivery. J. Colloid Interface Sci. 2019, 536, 224–234. [Google Scholar] [CrossRef] [PubMed]
- Kunjiappan, S.; Theivendran, P.; Baskararaj, S.; Sankaranarayanan, B.; Palanisamy, P.; Saravanan, G.; Arunachalam, S.; Sankaranarayanan, M.; Natarajan, J.; Somasundaram, B.; et al. Modeling a pH-sensitive Zein-co-acrylic acid hybrid hydrogels loaded 5-fluorouracil and rutin for enhanced anticancer efficacy by oral delivery. 3 Biotech 2019, 9, 1–20. [Google Scholar] [CrossRef] [PubMed]
- Salem, H.F.; Kharshoum, R.M.; Gamal, F.A.; Abo El-Ela, F.I.; Abdellatif, K.R.A. Treatment of breast cancer with engineered novel pH-sensitive triaryl-(Z)-olefin niosomes containing hydrogel: An in vitro and in vivo study. J. Liposome Res. 2020, 30, 126–135. [Google Scholar] [CrossRef] [PubMed]
- Kaushik, P.; Priyadarshini, E.; Rawat, K.; Rajamani, P.; Bohidar, H.B. pH responsive doxorubucin loaded zein nanoparticle crosslinked pectin hydrogel as effective site-specific anticancer substrates. Int. J. Biol. Macromol. 2020, 152, 1027–1037. [Google Scholar] [CrossRef] [PubMed]
- Ning, L.; You, C.; Zhang, Y.; Li, X.; Wang, F. Synthesis and biological evaluation of surface-modified nanocellulose hydrogel loaded with paclitaxel. Life Sci. 2020, 241, 117137. [Google Scholar] [CrossRef] [PubMed]
- Zhan, J.; Wu, Y.; Wang, H.; Liu, J.; Ma, Q.; Xiao, K.; Li, Z.; Li, J.; Luo, F.; Tan, H. An injectable hydrogel with pH-sensitive and self-healing properties based on 4armPEGDA and N-carboxyethyl chitosan for local treatment of hepatocellular carcinoma. Int. J. Biol. Macromol. 2020, 163, 1208–1222. [Google Scholar] [CrossRef] [PubMed]
- Qian, C.; Zhang, T.; Gravesande, J.; Baysah, C.; Song, X.; Xing, J. Injectable and self-healing polysaccharide-based hydrogel for pH-responsive drug release. Int. J. Biol. Macromol. 2019, 123, 140–148. [Google Scholar] [CrossRef] [PubMed]
- Li, L.; Scheiger, J.M.; Levkin, P.A. Design and Applications of Photoresponsive Hydrogels. Adv. Mater. 2019, 31, 1807333. [Google Scholar] [CrossRef] [Green Version]
- Pereira, R.F.; Bártolo, P.J. Photopolymerizable hydrogels in regenerative medicine and drug delivery. Hot Top. Biomater. 2014, 6–28. [Google Scholar]
- Wang, Z.J.; Li, C.Y.; Zhao, X.Y.; Wu, Z.L.; Zheng, Q. Thermo- and photo-responsive composite hydrogels with programmed deformations. J. Mater. Chem. B 2019, 7, 1674–1678. [Google Scholar] [CrossRef]
- Tomatsu, I.; Peng, K.; Kros, A. Photoresponsive hydrogels for biomedical applications. Adv. Drug Deliv. Rev. 2011, 63, 1257–1266. [Google Scholar] [CrossRef] [PubMed]
- Qiu, M.; Wang, D.; Liang, W.; Liu, L.; Zhang, Y.; Chen, X.; Sang, D.K.; Xing, C.; Li, Z.; Dong, B.; et al. Novel concept of the smart NIR-light-controlled drug release of black phosphorus nanostructure for cancer therapy. Proc. Natl. Acad. Sci. USA 2018, 115, 501–506. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Yang, M.; Lee, S.Y.; Kim, S.; Koo, J.S.; Seo, J.H.; Jeong, D.I.; Hwang, C.R.; Lee, J.; Cho, H.J. Selenium and dopamine-crosslinked hyaluronic acid hydrogel for chemophotothermal cancer therapy. J. Control Release 2020, 324, 750–764. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.; Han, B.; Shi, R.; Pan, L.; Zhang, H.; Shen, Y.; Li, C.; Huang, F.; Xie, A. Preparation and characterization of a novel hybrid hydrogel shell for localized photodynamic therapy. J. Mater. Chem. B 2013, 1, 6411–6417. [Google Scholar] [CrossRef] [PubMed]
- Chang, G.; Zhang, H.; Li, S.; Huang, F.; Shen, Y.; Xie, A. Effective photodynamic therapy of polymer hydrogel on tumor cells prepared using methylene blue sensitized mesoporous titania nanocrystal. Mater. Sci. Eng. C 2019, 99, 1392–1398. [Google Scholar] [CrossRef]
- Hou, M.; Liu, W.; Zhang, L.; Zhang, L.; Xu, Z.; Cao, Y.; Kang, Y.; Xue, P. Responsive agarose hydrogel incorporated with natural humic acid and MnO2 nanoparticles for effective relief of tumor hypoxia and enhanced photo-induced tumor therapy. Biomater. Sci. 2020, 8, 353–369. [Google Scholar] [CrossRef] [PubMed]
- Gao, F.; Xie, W.; Miao, Y.; Wang, D.; Guo, Z.; Ghosal, A.; Li, Y.; Wei, Y.; Feng, S.S.; Zhao, L.; et al. Magnetic Hydrogel with Optimally Adaptive Functions for Breast Cancer Recurrence Prevention. Adv. Healthc. Mater. 2019, 8, e1900203. [Google Scholar] [CrossRef] [PubMed]
- Wu, H.; Song, L.; Chen, L.; Zhang, W.; Chen, Y.; Zang, F.; Chen, H.; Ma, M.; Gu, N.; Zhang, Y. Injectable magnetic supramolecular hydrogel with magnetocaloric liquid-conformal property prevents post-operative recurrence in a breast cancer model. Acta Biomater. 2018, 74, 302–311. [Google Scholar] [CrossRef] [PubMed]
- Xiang, T.; Lu, T.; Zhao, W.F.; Zhao, C.S. Ionic-Strength Responsive Zwitterionic Copolymer Hydrogels with Tunable Swelling and Adsorption Behaviors. Langmuir 2019, 35, 1146–1155. [Google Scholar] [CrossRef]
- Ma, G.; Lin, W.; Yuan, Z.; Wu, J.; Qian, H.; Xu, L.; Chen, S. Development of ionic strength/pH/enzyme triple-responsive zwitterionic hydrogel of the mixed l-glutamic acid and l-lysine polypeptide for site-specific drug delivery. J. Mater. Chem. B 2017, 5, 935–943. [Google Scholar] [CrossRef]
- Fathi, M.; Alami-Milani, M.; Geranmayeh, M.H.; Barar, J.; Erfan-Niya, H.; Omidi, Y. Dual thermo-and pH-sensitive injectable hydrogels of chitosan/(poly(N-isopropylacrylamide-co-itaconic acid)) for doxorubicin delivery in breast cancer. Int. J. Biol. Macromol. 2019, 128, 957–964. [Google Scholar] [CrossRef] [PubMed]
- Farjadian, F.; Rezaeifard, S.; Naeimi, M.; Ghasemi, S.; Mohammadi-Samani, S.; Welland, M.E.; Tayebi, L. Temperature and pH-responsive nano-hydrogel drug delivery system based on lysine-modified poly (vinylcaprolactam). Int. J. Nanomed. 2019, 14, 6901–6915. [Google Scholar] [CrossRef] [Green Version]
- Yue, Z.; Che, Y.J.; Jin, Z.; Wang, S.; Ma, Q.; Zhang, Q.; Tan, Y.; Meng, F. A facile method to fabricate thermo- and pH-sensitive hydrogels with good mechanical performance based on poly(ethylene glycol) methyl ether methacrylate and acrylic acid as a potential drug carriers. J. Biomater. Sci. Polym. Ed. 2019, 30, 1375–1398. [Google Scholar] [CrossRef] [PubMed]
- Pang, X.; Liang, S.; Wang, T.; Yu, S.; Yang, R.; Hou, T.; Liu, Y.; He, C.; Zhang, N. Engineering thermo-ph dual responsive hydrogel for enhanced tumor accumulation, penetration, and chemo-protein combination therapy. Int. J. Nanomed. 2020, 15, 4739–4752. [Google Scholar] [CrossRef] [PubMed]
- Wang, C.; Zhang, G.; Liu, G.; Hu, J.; Liu, S. Photo- and thermo-responsive multicompartment hydrogels for synergistic delivery of gemcitabine and doxorubicin. J. Control Release 2017, 259, 149–159. [Google Scholar] [CrossRef]





| Polymer | Chemical Structure |
|---|---|
| Acrylamide Polymer base for a variety of derivatives including polyacrylamide, bisacrylamide, N-Isopropylacrylamide, N-N′-dimethylacrylamide |  |
| Methacrylate Polymer base for a variety of derivatives including poly-2-hydroxyethylmethacrylate, poly(N,N′-dimethyl aminoethyl methacrylate), tert-butyl methacrylate, n-butyl methacrylate, n-butyl acrylate, and methyl methacrylate |  |
| PLGA (x = number of units of lactic acid and y = number of units of glycolic acid) |  |
| PEG (n = number of units of ethylene glycol) |  |
| PEGDA (n = number of units of ethylene glycol) |  |
| Chitosan (n = number of units of β-(1→4)-linked D-glucosamine and N-acetyl-D-glucosamine) |  |
| Alginate (x = number of units of (1,4)-linked β-D-mannuronate and y = number of units of α-L-guluronate) |  |
| PVA (n = number of units of vinyl alcohol) |  |
| Poloxamer (x = number of units of ethylene glycol and y = number of units of propylene glycol) |  |
| Date | Drug | In vitro model | In vivo model | Hydrogel formulation | Highlights | References |
|---|---|---|---|---|---|---|
| 2014 | 5-FU | HT-29 cells (colorectal adenocarcinoma) | n.a. | β-CD-graft-gelatin crosslinked with oxidized dextran | Presence of β-CD increase drug loading. Swelling and drug release is low at pH 1.2 and high at pH 7.4, being appropriate for drug release at colon. Hydrogels were biocompatible and increase the efficacy of 5-FU. | [38] |
| 2019 | Bortezomib | MC3T3E1 (osteoblast) and NIH-3T3 (fibroblast) cells | n.a. | Alginate-conjugated polydopamine | The release mechanism followed non-Fickian diffusion. FACS analysis revealed cell apoptosis defined by loss of cell viability for colon cancer cells. | [39] |
| 2019 | Prospidin | HeLa (cervical adenocarcinoma) and HeP-2 (human hepatocellular liver carcinoma) cells | Zajdel hepatoma Mongrel white rats | Dextran phosphate (DP) | At low pH, the swelling of hydrogels is 4.6–12.3 times lower than at pH 7.4. Susceptible to degradation by the simulated physiological conditions. The amount of drug release is dependent on the pH of outer media and decreases with the growth of phosphoric group content in DP hydrogels | [40] |
| 2015 | 5-FU | n.a. | n.a. | N-N′-dimethylacrylamide monomers polymerized in presence of methacrylic acid or 2-aminoethyl methacrylate hydrochloride containing ferro-nanoparticles | Drug release is always higher in the presence of a magnetic field and generally increases with its intensity. | [41] |
| 2017 | DOX | HepG2 cells (human hepatocellular liver carcinoma) | Sprague-Dawley rat | N-carboxyethyl chitosan + PEGDA | Exhibited in vitro pH-dependent gel degradation and doxorubicin release. No hydrogel diffusion after subcutaneous injection. | [33] |
| 2019 | PTX | HepG2 (human hepatocellular liver carcinoma), H22 (murine hepatoma) | H22 subcutaneous xenograft BALB/c mice | Self-assembling octapeptides | In vitro controlled release of PTX at pH 5.5 for 6 days. In vivo hydrogel retention at the tumor site. Increased antitumor efficacy compared to free PTX (reduced tumor weight and volume), and reduced toxicity (low weight loss). | [42] |
| 2017 | DOX | MDA-MB-231 cells (breast cancer) | n.a. | DNA hairpin conjugated with polyacrylamide | pH-induced separation of the nucleic acid duplex units causing DOX release at pH 5.0. Increase DOX cellular uptake and efficacy. | [43] |
| 2019 | DOX | HCT116 cells (colorectal adenocarcinoma) | Kunming Mice | Chitosan-grafted-dihydrocaffeic acid/oxidized pullulan | 87% DOX release over 60 h at pH 5.5 over 52% at pH 7.4. In vitro enhancement of DOX therapeutic efficacy. In vivo adhesion in the injection site. | [44] |
| 2019 | 5-FU and Rutin | MDA-MB-231 and MCF-7 cells (breast cancer) | n.a. | Zein, acrylic acid, N, N-methylene bisacrylamide, and ammonium persulphate | Improved release at pH 7.4 over pH 1.2. Improved in vitro pharmacological activity by apoptosis induction by oxidative stress. | [45] |
| 2020 | Triaryl-(Z)-olefin | n.a. | Ehrlich carcinoma cell subcutaneous xenograft Swiss albino mice | Cholesterol and span 60 niosomes in chitosan and glyceryl monooleate-based hydrogels | Controlled release of drug and improved tumor regression | [46] |
| 2020 | DOX | HeLa cells (cervical adenocarcinoma) | n.a. | Zein nanoparticle crosslinked pectin | Improved DOX cellular internalization and cytotoxicity | [47] |
| 2020 | PTX | A549 (lung cancer) and HepG2 (human hepatocellular liver carcinoma) cells | n.a. | Long-chain hexadecyl amine modified nanocellulose | Improved release at pH < 6.8. Improved PTX internalization by cells and therapeutic efficacy. | [48] |
| 2020 | DOX | HepG2 cells (human hepatocellular liver carcinoma) | HepG2 xenograft BALB/c nude mouse model | 4armPEG-benzaldehyde and N-carboxyethyl chitosan | Degradation occurs at pH 5.6 which contributes for controlled DOX release. In vivo biocompatibility, degradation over 5 days, and improved tumor inhibition | [49] |
| 2019 | DOX | HeLa cells (cervical adenocarcinoma) | n.a. | Carboxyethyl modified chitosan and aldehyde modified hyaluronic acid | Improved drug release at pH < 6.8. Biocompatibility and biodegradability. In vitro pharmacological efficacy | [50] |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Andrade, F.; Roca-Melendres, M.M.; Durán-Lara, E.F.; Rafael, D.; Schwartz, S., Jr. Stimuli-Responsive Hydrogels for Cancer Treatment: The Role of pH, Light, Ionic Strength and Magnetic Field. Cancers 2021, 13, 1164. https://doi.org/10.3390/cancers13051164
Andrade F, Roca-Melendres MM, Durán-Lara EF, Rafael D, Schwartz S Jr. Stimuli-Responsive Hydrogels for Cancer Treatment: The Role of pH, Light, Ionic Strength and Magnetic Field. Cancers. 2021; 13(5):1164. https://doi.org/10.3390/cancers13051164
Chicago/Turabian StyleAndrade, Fernanda, Maria Mercé Roca-Melendres, Esteban F. Durán-Lara, Diana Rafael, and Simó Schwartz, Jr. 2021. "Stimuli-Responsive Hydrogels for Cancer Treatment: The Role of pH, Light, Ionic Strength and Magnetic Field" Cancers 13, no. 5: 1164. https://doi.org/10.3390/cancers13051164