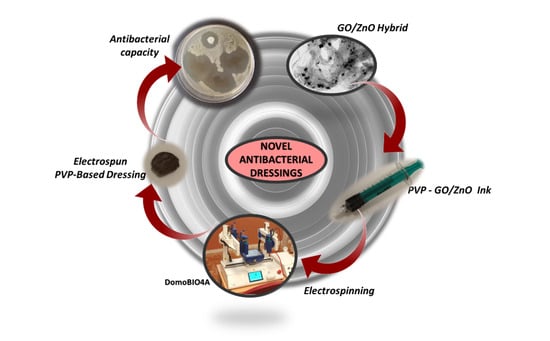
Electrospun Polyvinylpyrrolidone-Based Dressings Containing GO/ZnO Nanocomposites: A Novel Frontier in Antibacterial Wound Care
Abstract
:1. Introduction
2. Experimental Methods
2.1. Materials
2.2. Synthesis of GO/ZnO Nanocomposites
2.3. Characterization of the Nanomaterials
2.4. Synthesis of the Electrospun Dressings
2.5. SEM Characterization of the Electrospun Discs
2.6. Antibacterial Studies
3. Results and Discussion
3.1. Synthesis and Characterization of GO/ZnO Nanocomposites
3.1.1. Physicochemical Properties of GO/ZnO Nanocomposites
3.1.2. Antibacterial Studies of GO/ZnO-Based Nanocomposite Dispersions
3.2. Synthesis, Characterization, and Antibacterial Properties of GO/ZnO-Based Dressings
4. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Ongarora, B.G. Recent Technological Advances in the Management of Chronic Wounds: A Literature Review. Health Sci. Rep. 2022, 5, e641. [Google Scholar] [CrossRef]
- Kolimi, P.; Narala, S.; Nyavanandi, D.; Youssef, A.A.A.; Dudhipala, N. Innovative Treatment Strategies to Accelerate Wound Healing: Trajectory and Recent Advancements. Cells 2022, 11, 2439. [Google Scholar] [CrossRef]
- Yousefian, F.; Hesari, R.; Jensen, T.; Obagi, S.; Rgeai, A.; Damiani, G.; Bunick, C.G.; Grada, A. Antimicrobial Wound Dressings: A Concise Review for Clinicians. Antibiotics 2023, 12, 1434. [Google Scholar] [CrossRef] [PubMed]
- Simões, D.; Miguel, S.P.; Ribeiro, M.P.; Coutinho, P.; Mendonça, A.G.; Correia, I.J. Recent Advances on Antimicrobial Wound Dressing: A Review. Eur. J. Pharm. Biopharm. 2018, 127, 130–141. [Google Scholar] [CrossRef] [PubMed]
- Agarwal, S.; Wendorff, J.H.; Greiner, A. Use of Electrospinning Technique for Biomedical Applications. Polymer 2008, 49, 5603–5621. [Google Scholar] [CrossRef]
- Xue, J.; Wu, T.; Dai, Y.; Xia, Y. Electrospinning and Electrospun Nanofibers: Methods, Materials, and Applications. Chem. Rev. 2019, 119, 5298–5415. [Google Scholar] [CrossRef] [PubMed]
- Jiang, Z.; Zheng, Z.; Yu, S.; Gao, Y.; Ma, J.; Huang, L.; Yang, L. Nanofiber Scaffolds as Drug Delivery Systems Promoting Wound Healing. Pharmaceutics 2023, 15, 1829. [Google Scholar] [CrossRef] [PubMed]
- Anjum, S.; Rahman, F.; Pandey, P.; Arya, D.K.; Alam, M.; Rajinikanth, P.S.; Ao, Q. Electrospun Biomimetic Nanofibrous Scaffolds: A Promising Prospect for Bone Tissue Engineering and Regenerative Medicine. Int. J. Mol. Sci. 2022, 23, 9206. [Google Scholar] [CrossRef] [PubMed]
- Sahu, T.; Ratre, Y.K.; Chauhan, S.; Bhaskar, L.V.K.S.; Nair, M.P.; Verma, H.K. Nanotechnology Based Drug Delivery System: Current Strategies and Emerging Therapeutic Potential for Medical Science. J. Drug Deliv. Sci. Technol. 2021, 63, 102487. [Google Scholar] [CrossRef]
- Moroni, L.; Licht, R.; de Boer, J.; de Wijn, J.R.; van Blitterswijk, C.A. Fiber Diameter and Texture of Electrospun PEOT/PBT Scaffolds Influence Human Mesenchymal Stem Cell Proliferation and Morphology, and the Release of Incorporated Compounds. Biomaterials 2006, 27, 4911–4922. [Google Scholar] [CrossRef]
- He, F.L.; Deng, X.; Zhou, Y.Q.; Zhang, T.D.; Liu, Y.L.; Ye, Y.J.; Yin, D.C. Controlled Release of Antibiotics from Poly-ε-Caprolactone/Polyethylene Glycol Wound Dressing Fabricated by Direct-Writing Melt Electrospinning. Polym. Adv. Technol. 2019, 30, 425–434. [Google Scholar] [CrossRef]
- Yu, D.G.; Nie, W.; Zhu, L.M.; Branford-White, C. Fast Dissolution Nanofiber Membrane of Ferulic Acid Prepared Using Electrospinning. In Proceedings of the 2010 4th International Conference on Bioinformatics and Biomedical Engineering, iCBBE 2010, Chengdu, China, 18–20 June 2010. [Google Scholar] [CrossRef]
- Haaf, F.; Sanner, A.; Straub, F. Polymers of N-Vinylpyrrolidone: Synthesis, Characterization and Uses. Polym. J. 1985, 17, 143–152. [Google Scholar] [CrossRef]
- Dai, M.; Jin, S.; Nugen, S.R. Water-Soluble Electrospun Nanofibers as a Method for on-Chip Reagent Storage. Biosensors 2012, 2, 388–395. [Google Scholar] [CrossRef]
- Alven, S.; Buyana, B.; Feketshane, Z.; Aderibigbe, B.A. Electrospun Nanofibers/Nanofibrous Scaffolds Loaded with Silver Nanoparticles as Effective Antibacterial Wound Dressing Materials. Pharmaceutics 2021, 13, 964. [Google Scholar] [CrossRef]
- Yang, J.; Wang, K.; Yu, D.G.; Yang, Y.; Bligh, S.W.A.; Williams, G.R. Electrospun Janus Nanofibers Loaded with a Drug and Inorganic Nanoparticles as an Effective Antibacterial Wound Dressing. Mater. Sci. Eng. C 2020, 111, 110805. [Google Scholar] [CrossRef]
- Bellier, N.; Baipaywad, P.; Ryu, N.; Lee, J.Y.; Park, H. Recent Biomedical Advancements in Graphene Oxide- and Reduced Graphene Oxide-Based Nanocomposite Nanocarriers. Biomater. Res. 2022, 26, 65. [Google Scholar] [CrossRef]
- Martín, C.; Kostarelos, K.; Prato, M.; Bianco, A. Biocompatibility and Biodegradability of 2D Materials: Graphene and Beyond. Chem. Commun. 2019, 55, 5540–5546. [Google Scholar] [CrossRef]
- Trotta, F.; Caldera, F.; Zarrabi, A.; Ng, I.M.J.; Shamsi, S. Graphene Oxide (GO): A Promising Nanomaterial against Infectious Diseases Caused by Multidrug-Resistant Bacteria. Int. J. Mol. Sci. 2022, 23, 9096. [Google Scholar] [CrossRef]
- Martín, C.; Bachiller, A.; Fernández-Blázquez, J.P.; Nishina, Y.; Jorcano, J.L. Plasma-Derived Fibrin Hydrogels Containing Graphene Oxide for Infections Treatment. ACS Mater. Lett. 2023, 5, 1245–1255. [Google Scholar] [CrossRef]
- Zou, X.; Zhang, L.; Wang, Z.; Luo, Y. Mechanisms of the Antimicrobial Activities of Graphene Materials. J. Am. Chem. Soc. 2016, 138, 2064–2077. [Google Scholar] [CrossRef]
- Colon, G.; Ward, B.C.; Webster, T.J. Increased Osteoblast and Decreased Staphylococcus Epidermidis Functions on Nanophase ZnO and TiO2. J. Biomed. Mater. Res. A 2006, 78, 595–604. [Google Scholar] [CrossRef]
- Brayner, R.; Ferrari-Iliou, R.; Brivois, N.; Djediat, S.; Benedetti, M.F.; Fiévet, F. Toxicological Impact Studies Based on Escherichia Coli Bacteria in Ultrafine ZnO Nanoparticles Colloidal Medium. Nano Lett. 2006, 6, 866–870. [Google Scholar] [CrossRef]
- Chiriac, V.; Stratulat, D.N.; Calin, G.; Nichitus, S.; Burlui, V.; Stadoleanu, C.; Popa, M.; Popa, I.M. Antimicrobial Property of Zinc Based Nanoparticles. IOP Conf. Ser. Mater. Sci. Eng. 2016, 133, 012055. [Google Scholar] [CrossRef]
- Sirelkhatim, A.; Mahmud, S.; Seeni, A.; Kaus, N.H.M.; Ann, L.C.; Bakhori, S.K.M.; Hasan, H.; Mohamad, D. Review on Zinc Oxide Nanoparticles: Antibacterial Activity and Toxicity Mechanism. Nano-Micro Lett. 2015, 7, 219–242. [Google Scholar] [CrossRef]
- Pasquet, J.; Chevalier, Y.; Pelletier, J.; Couval, E.; Bouvier, D.; Bolzinger, M.A. The Contribution of Zinc Ions to the Antimicrobial Activity of Zinc Oxide. Colloids Surf. A Physicochem. Eng. Asp. 2014, 457, 263–274. [Google Scholar] [CrossRef]
- Usman, O.; Ikram, M.; Abid, N.; Saeed, M.; Bashir, A.; Nabgan, W.; Mushahid, N.; Ikram, M. Enhanced Bactericidal Action of RGO-ZnO Hybrids Prepared by the One-Pot Co-Precipitation Approach. ACS Omega 2022, 7, 26715–26722. [Google Scholar] [CrossRef]
- Rajapaksha, P.; Orrell-Trigg, R.; Shah, D.; Cheeseman, S.; Vu, K.B.; Ngo, S.T.; Murdoch, B.J.; Choudhury, N.R.; Yin, H.; Cozzolino, D.; et al. Broad Spectrum Antibacterial Zinc Oxide-Reduced Graphene Oxide Nanocomposite for Water Depollution. Mater. Today Chem. 2023, 27, 101242. [Google Scholar] [CrossRef]
- Pascucci, M.; Royer, G.; Adamek, J.; Aristizabal, D.; Blanche, L.; Bezzarga, A.; Boissinot, D.; Boniface-Chang, G.; Brunner, A.; Curel, C.; et al. The First AI-Based Mobile Application for Antibiotic Resistance Testing. bioRxiv 2020. [Google Scholar] [CrossRef]
- Bao, Z.; Yuan, Y.; Leng, C.; Li, L.; Zhao, K.; Sun, Z. One-Pot Synthesis of Noble Metal/Zinc Oxide Composites with Controllable Morphology and High Catalytic Performance. ACS Appl. Mater. Interfaces 2017, 9, 16417–16425. [Google Scholar] [CrossRef]
- Alharthi, F.A.; Alsyahi, A.A.; Alshammari, S.G.; AL-Abdulkarim, H.A.; AlFawaz, A.; Alsalme, A. Synthesis and Characterization of RGO@ZnO Nanocomposites for Esterification of Acetic Acid. ACS Omega 2022, 7, 2786–2797. [Google Scholar] [CrossRef]
- Lee, S.; Lee, H.; Sim, J.H.; Sohn, D. Graphene Oxide/Poly(Acrylic Acid) Hydrogel by γ-Ray Pre-Irradiation on Graphene Oxide Surface. Macromol. Res. 2014, 22, 165–172. [Google Scholar] [CrossRef]
- Quadri, T.W.; Olasunkanmi, L.O.; Fayemi, O.E.; Solomon, M.M.; Ebenso, E.E. Zinc Oxide Nanocomposites of Selected Polymers: Synthesis, Characterization, and Corrosion Inhibition Studies on Mild Steel in HCl Solution. ACS Omega 2017, 2, 8421–8437. [Google Scholar] [CrossRef] [PubMed]
- Feng, Y.; Feng, N.; Wei, Y.; Zhang, G. An in Situ Gelatin-Assisted Hydrothermal Synthesis of ZnO-Reduced Graphene Oxide Composites with Enhanced Photocatalytic Performance under Ultraviolet and Visible Light. RSC Adv. 2014, 4, 7933–7943. [Google Scholar] [CrossRef]
- Yang, Y.; Liu, T. Fabrication and Characterization of Graphene Oxide/Zinc Oxide Nanorods Hybrid. Appl. Surf. Sci. 2011, 257, 8950–8954. [Google Scholar] [CrossRef]
- Zhang, X.; Zhang, Y.C.; Ma, L.X. One-Pot Facile Fabrication of Graphene-Zinc Oxide Composite and Its Enhanced Sensitivity for Simultaneous Electrochemical Detection of Ascorbic Acid, Dopamine and Uric Acid. Sens. Actuators B Chem. 2016, 227, 488–496. [Google Scholar] [CrossRef]
- Hwa, K.Y.; Subramani, B. Synthesis of Zinc Oxide Nanoparticles on Graphene-Carbon Nanotube Hybrid for Glucose Biosensor Applications. Biosens. Bioelectron. 2014, 62, 127–133. [Google Scholar] [CrossRef]
- Cai, X.; Cai, Y.; Liu, Y.; Li, H.; Zhang, F.; Wang, Y. Structural and Photocatalytic Properties of Nickel-Doped Zinc Oxide Powders with Variable Dopant Contents. J. Phys. Chem. Solids 2013, 74, 1196–1203. [Google Scholar] [CrossRef]
- Saranya, M.; Ramachandran, R.; Wang, F. Graphene-Zinc Oxide (G-ZnO) Nanocomposite for Electrochemical Supercapacitor Applications. J. Sci. Adv. Mater. Devices 2016, 1, 454–460. [Google Scholar] [CrossRef]
- Trikkaliotis, D.G.; Mitropoulos, A.C.; Kyzas, G.Z. Low-Cost Route for Top-down Synthesis of over- and Low-Oxidized Graphene Oxide. Colloids Surf. A Physicochem. Eng. Asp. 2020, 600, 124928. [Google Scholar] [CrossRef]
- Krishnamoorthy, K.; Veerapandian, M.; Yun, K.; Kim, S.J. The Chemical and Structural Analysis of Graphene Oxide with Different Degrees of Oxidation. Carbon 2013, 53, 38–49. [Google Scholar] [CrossRef]
- Li, M.; Chen, Z.; Yang, L.; Li, J.; Xu, J.; Chen, C.; Wu, Q.; Yang, M.; Liu, T. Antibacterial Activity and Mechanism of GO/Cu2O/ZnO Coating on Ultrafine Glass Fiber. Nanomaterials 2022, 12, 1857. [Google Scholar] [CrossRef]
- Salman, J.A.S.; Al-Ramadhan, Z.A.; Hmud, H.A.K. Antibacterial Effect and Structural Properties of PVA-PVP-AG of Biomedical AND Pharmaceutical Sciences. Eur. J. Biomed. Pharm. Sci. 2016, 3, 35–41. [Google Scholar]
- Abdulrazaq, R.A.; Al-Ramadhan, Z.A.; Khalaf, H.H. Antibacterial Activity of (PVP-ZrO2) Nanocomposite against Pathogenic Bacteria. World News Nat. Sci. 2018, 182, 187–194. [Google Scholar]
- Dey, A.; Dasgupta, A.; Kumar, V.; Tyagi, A.; Verma, A.K. Evaluation of the of Antibacterial Efficacy of Polyvinylpyrrolidone (PVP) and Tri-Sodium Citrate (TSC) Silver Nanoparticles. Int. Nano Lett. 2015, 5, 223–230. [Google Scholar] [CrossRef]
- Szewczyk, P.K.; Stachewicz, U. The Impact of Relative Humidity on Electrospun Polymer Fibers: From Structural Changes to Fiber Morphology. Adv. Colloid. Interface Sci. 2020, 286, 102315. [Google Scholar] [CrossRef]
- Haider, S.; Al-Zeghayer, Y.; Ahmed Ali, F.A.; Haider, A.; Mahmood, A.; Al-Masry, W.A.; Imran, M.; Aijaz, M.O. Highly Aligned Narrow Diameter Chitosan Electrospun Nanofibers. J. Polym. Res. 2013, 20, 105. [Google Scholar] [CrossRef]
- Agarwal, S.; Greiner, A.; Wendorff, J.H. Functional Materials by Electrospinning of Polymers. Prog. Polym. Sci. 2013, 38, 963–991. [Google Scholar] [CrossRef]
- Bhatia, D.; Mittal, A.; Malik, D.K. Antimicrobial Activity of PVP Coated Silver Nanoparticles Synthesized by Lysinibacillus varians. 3 Biotech 2016, 6, 196. [Google Scholar] [CrossRef] [PubMed]
- Bryaskova, R.; Pencheva, D.; Nikolov, S.; Kantardjiev, T. Synthesis and Comparative Study on the Antimicrobial Activity of Hybrid Materials Based on Silver Nanoparticles (AgNps) Stabilized by Polyvinylpyrrolidone (PVP). J. Chem. Biol. 2011, 4, 185–191. [Google Scholar] [CrossRef] [PubMed]
- Aboelwafa, M.A.; Abdelghany, A.M.; Meikhail, M.S. Preparation, Characterization, and Antibacterial Activity of Zns-Np’s Filled Polyvinylpyrrolidone/Chitosan Thin Films. Biointerface Res. Appl. Chem. 2021, 11, 14336–14343. [Google Scholar] [CrossRef]
- Bari, A.; Ikram, M.; Haider, A.; Ul-Hamid, A.; Haider, J.; Shahzadi, I.; Nazir, G.; Shahzadi, A.; Imran, M.; Ghaffar, A. Evaluation of Bactericidal Potential and Catalytic Dye Degradation of Multiple Morphology Based Chitosan/Polyvinylpyrrolidone-Doped Bismuth Oxide Nanostructures. Nanoscale Adv. 2022, 4, 2713–2728. [Google Scholar] [CrossRef] [PubMed]
- Yu, H.; Xu, X.; Chen, X.; Lu, T.; Zhang, P.; Jing, X. Preparation and Antibacterial Effects of PVA-PVP Hydrogels Containing Silver Nanoparticles. J. Appl. Polym. Sci. 2007, 103, 125–133. [Google Scholar] [CrossRef]
- Prema, D.; Prakash, J.; Vignesh, S.; Veluchamy, P.; Ramachandran, C.; Samal, D.B.; Oh, D.H.; Sahabudeen, S.; Devanand Venkatasubbu, G. Mechanism of Inhibition of Graphene Oxide/Zinc Oxide Nanocomposite against Wound Infection Causing Pathogens. Appl. Nanosci. 2020, 10, 827–849. [Google Scholar] [CrossRef]
- Li, Y.; Yang, Y.; Qing, Y.; Li, R.; Tang, X.; Guo, D.; Qin, Y. Enhancing Zno-Np Antibacterial and Osteogenesis Properties in Orthopedic Applications: A Review. Int. J. Nanomed. 2020, 15, 6247–6262. [Google Scholar] [CrossRef]
- Ndayishimiye, J.; Kumeria, T.; Popat, A.; Falconer, J.R.; Blaskovich, M.A.T. Nanomaterials: The New Antimicrobial Magic Bullet. ACS Infect. Dis. 2022, 8, 693–712. [Google Scholar] [CrossRef] [PubMed]






| Element (mass%) | |||
|---|---|---|---|
| Sample | C | O | Zn |
| GO control | 74.3 | 22.8 | |
| ZnO control | 24.7 | 75.3 | |
| GO/ZnO_1:1 | 56.2 | 31.8 | 9.4 |
| GO/ZnO_2:1 | 55.9 | 29.2 | 5.9 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Martín, C.; Ferreiro Fernández, A.; Salazar Romero, J.C.; Fernández-Blázquez, J.P.; Mendizabal, J.; Artola, K.; Jorcano, J.L.; Rabanal, M.E. Electrospun Polyvinylpyrrolidone-Based Dressings Containing GO/ZnO Nanocomposites: A Novel Frontier in Antibacterial Wound Care. Pharmaceutics 2024, 16, 305. https://doi.org/10.3390/pharmaceutics16030305
Martín C, Ferreiro Fernández A, Salazar Romero JC, Fernández-Blázquez JP, Mendizabal J, Artola K, Jorcano JL, Rabanal ME. Electrospun Polyvinylpyrrolidone-Based Dressings Containing GO/ZnO Nanocomposites: A Novel Frontier in Antibacterial Wound Care. Pharmaceutics. 2024; 16(3):305. https://doi.org/10.3390/pharmaceutics16030305
Chicago/Turabian StyleMartín, Cristina, Adalyz Ferreiro Fernández, Julia C. Salazar Romero, Juan P. Fernández-Blázquez, Jabier Mendizabal, Koldo Artola, José L. Jorcano, and M. Eugenia Rabanal. 2024. "Electrospun Polyvinylpyrrolidone-Based Dressings Containing GO/ZnO Nanocomposites: A Novel Frontier in Antibacterial Wound Care" Pharmaceutics 16, no. 3: 305. https://doi.org/10.3390/pharmaceutics16030305