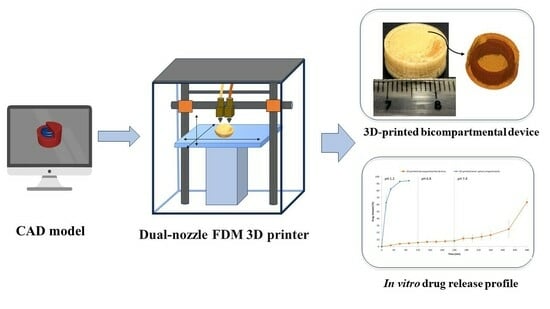
Development of 3D-Printed Bicompartmental Devices by Dual-Nozzle Fused Deposition Modeling (FDM) for Colon-Specific Drug Delivery
Abstract
:1. Introduction
2. Materials and Methods
2.1. Materials
2.2. Preparation of HPMCAS and Drug-Loaded PVA Filaments
2.3. Solid State Characterization and Morphological Evaluation
2.3.1. Differential Scanning Calorimetry (DSC)
2.3.2. Thermogravimetric Analysis (TGA)
2.3.3. X-ray Powder Diffraction (XRPD)
2.3.4. Scanning Electron Microscopy (SEM)
2.4. Mechanical Characterization of Filaments
2.5. Filament Drug Content Determination
2.6. Design and Elaboration of 3D-Printed Systems
2.7. X-ray Microcomputer Tomography (XµCT) of 3D-Printed Devices
2.8. In Vitro Drug Release Studies of 3D-Printed Systems
3. Results and Discussion
3.1. Preparation of HPMCAS and Drug-Loaded PVA Filaments
3.2. Solid State Characterization and Morphological Evaluation
3.2.1. Differential Scanning Calorimetry (DSC)
3.2.2. Thermogravimetric Analysis (TGA)
3.2.3. X-ray Powder Diffraction (XRPD)
3.2.4. Scanning Electron Microscopy (SEM)
3.3. Mechanical Characterization of Filaments
3.4. Filament Drug Content Determination
3.5. Three-Dimensional Printing and Physical Characterization of Three-Dimensional-Printed Systems
3.6. Scanning Electron Microscopy (SEM) of 3D-Printed Devices
3.7. X-ray Microcomputer Tomography (XµCT) of 3D-Printed Devices
3.8. In Vitro Drug Release Studies of 3D-Printed Systems
4. Conclusions
- Drug-free HPMCAS-HG and drug-loaded PVA filaments (20% w/w) were obtained by single-screw extrusion, and their suitability as feedstock materials for the 3D printing process were demonstrated through an extensive physicochemical and mechanical characterization.
- Both filaments were simultaneously printed, combining, in a single and innovative structure, an outer pH-dependent cylindrical compartment and an inner water-soluble compartment (spiral shape) containing the drug. The internal channel communicates with the surrounding media through an opening gap on top of the device. The 3D-printed bicompartmental systems showed high reproducibility despite the challenging design configuration.
- Drug release tests in biorelevant media demonstrated the ability of the novel 3D-printed structure to target 5-ASA to the colonic region. A biphasic drug release profile was obtained with an initial sustained release phase (pH values of 1.2 and 6.8) controlled by the water uptake through the opening gap, and subsequent drug diffusion from the internal PVA-based compartment (<10 wt% cumulative drug release). At pH 7.4, the solubilization of the outer HPMCAS-based compartment increased the surface area of the inner spiral exposed to the dissolution medium. Hence, the drug release kinetics changed from a diffusion-controlled to an erosion-mediated process, considerably increasing the drug release rate (>95 wt% cumulative drug release at the end of the study).
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Krueger, L.; Miles, J.A.; Popat, A. 3D Printing Hybrid Materials Using Fused Deposition Modelling for Solid Oral Dosage Forms. J. Control Release 2022, 351, 444–455. [Google Scholar] [CrossRef] [PubMed]
- Gogolewski, D.; Kozior, T.; Zmarzły, P.; Mathia, T.G. Morphology of Models Manufactured by SLM Technology and the Ti6al4v Titanium Alloy Designed for Medical Applications. Materials 2021, 14, 6249. [Google Scholar] [CrossRef] [PubMed]
- Ceulemans, J.; Ménière, Y.; Nichogiannopoulou, A.; Pose Rodríguez, J.; Rudyk, I. Patents and Additive Manufacturing; European Patent Office: Munich, Germany, 2020. [Google Scholar]
- Hu, Z.; Xu, P.; Zhang, J.; Bandari, S.; Repka, M.A. Development of Controlled Release Oral Dosages by Density Gradient Modification via Three-Dimensional (3D) Printing and Hot-Melt Extrusion (HME) Technology. J. Drug Deliv. Sci. Technol. 2022, 71, 103355. [Google Scholar] [CrossRef]
- Ullah, M.; Wahab, A.; Khan, S.U.; Naeem, M.; ur Rehman, K.; Ali, H.; Ullah, A.; Khan, A.; Khan, N.R.; Rizg, W.Y.; et al. 3D Printing Technology: A New Approach for the Fabrication of Personalized and Customized Pharmaceuticals. Eur. Polym. J. 2023, 195, 112240. [Google Scholar] [CrossRef]
- Varghese, R.; Sood, P.; Salvi, S.; Karsiya, J.; Kumar, D. 3D Printing in the Pharmaceutical Sector: Advances and Evidences. Sens. Int. 2022, 3, 100177. [Google Scholar] [CrossRef]
- Zhang, Z.; Feng, S.; Almotairy, A.; Bandari, S.; Repka, M.A. Development of Multifunctional Drug Delivery System via Hot-Melt Extrusion Paired with Fused Deposition Modeling 3D Printing Techniques. Eur. J. Pharm. Biopharm. 2023, 183, 102–111. [Google Scholar] [CrossRef]
- European Patents Office. Available online: https://worldwide.espacenet.com/patent/ (accessed on 11 September 2023).
- Chung, S.; Zhang, P.; Repka, M.A. Fabrication of Timed-Release Indomethacin Core–Shell Tablets for Chronotherapeutic Drug Delivery Using Dual Nozzle Fused Deposition Modeling (FDM) 3D Printing. Eur. J. Pharm. Biopharm. 2023, 188, 254–264. [Google Scholar] [CrossRef]
- Gottschalk, N.; Bogdahn, M.; Quodbach, J. 3D Printing of Amorphous Solid Dispersions: A Comparison of Fused Deposition Modeling and Drop-on-Powder Printing. Int. J. Pharm. X 2023, 5, 100179. [Google Scholar] [CrossRef]
- Mora-Castaño, G.; Millán-Jiménez, M.; Linares, V.; Caraballo, I. Assessment of the Extrusion Process and Printability of Suspension-Type Drug-Loaded AffinisolTM Filaments for 3D Printing. Pharmaceutics 2022, 14, 871. [Google Scholar] [CrossRef]
- Linares, V.; Aguilar-de-Leyva, Á.; Casas, M.; Caraballo, I. 3D Printed Fractal-like Structures with High Percentage of Drug for Zero-Order Colonic Release. Pharmaceutics 2022, 14, 2298. [Google Scholar] [CrossRef]
- Oladeji, S.; Mohylyuk, V.; Jones, D.S.; Andrews, G.P. 3D Printing of Pharmaceutical Oral Solid Dosage Forms by Fused Deposition: The Enhancement of Printability Using Plasticised HPMCAS. Int. J. Pharm. 2022, 616, 121553. [Google Scholar] [CrossRef] [PubMed]
- Zhang, P.; Xu, P.; Chung, S.; Bandari, S.; Repka, M.A. Fabrication of Bilayer Tablets Using Hot Melt Extrusion-Based Dual-Nozzle Fused Deposition Modeling 3D Printing. Int. J. Pharm. 2022, 624, 121972. [Google Scholar] [CrossRef] [PubMed]
- Gioumouxouzis, C.I.; Baklavaridis, A.; Katsamenis, O.L.; Markopoulou, C.K.; Bouropoulos, N.; Tzetzis, D.; Fatouros, D.G. A 3D Printed Bilayer Oral Solid Dosage Form Combining Metformin for Prolonged and Glimepiride for Immediate Drug Delivery. Eur. J. Pharm. Sci. 2018, 120, 40–52. [Google Scholar] [CrossRef]
- Okwuosa, T.C.; Pereira, B.C.; Arafat, B.; Cieszynska, M.; Isreb, A.; Alhnan, M.A. Fabricating a Shell-Core Delayed Release Tablet Using Dual FDM 3D Printing for Patient-Centred Therapy. Pharm. Res. 2017, 34, 427–437. [Google Scholar] [CrossRef]
- Tagami, T.; Nagata, N.; Hayashi, N.; Ogawa, E.; Fukushige, K.; Sakai, N.; Ozeki, T. Defined Drug Release from 3D-Printed Composite Tablets Consisting of Drug-Loaded Polyvinylalcohol and a Water-Soluble or Water-Insoluble Polymer Filler. Int. J. Pharm. 2018, 543, 361–367. [Google Scholar] [CrossRef] [PubMed]
- Goyanes, A.; Wang, J.; Buanz, A.; Martínez-Pacheco, R.; Telford, R.; Gaisford, S.; Basit, A.W. 3D Printing of Medicines: Engineering Novel Oral Devices with Unique Design and Drug Release Characteristics. Mol. Pharm. 2015, 12, 4077–4084. [Google Scholar] [CrossRef]
- Macedo, J.; Marques, R.; Vervaet, C.; Pinto, J.F. Production of Bi-Compartmental Tablets by FDM 3D Printing for the Withdrawal of Diazepam. Pharmaceutics 2023, 15, 538. [Google Scholar] [CrossRef]
- Sadia, M.; Isreb, A.; Abbadi, I.; Isreb, M.; Aziz, D.; Selo, A.; Timmins, P.; Alhnan, M.A. From ‘Fixed Dose Combinations’ to ‘a Dynamic Dose Combiner’: 3D Printed Bi-Layer Antihypertensive Tablets. Eur. J. Pharm. Sci. 2018, 123, 484–494. [Google Scholar] [CrossRef]
- Ghanizadeh Tabriz, A.; Nandi, U.; Hurt, A.P.; Hui, H.W.; Karki, S.; Gong, Y.; Kumar, S.; Douroumis, D. 3D Printed Bilayer Tablet with Dual Controlled Drug Release for Tuberculosis Treatment. Int. J. Pharm. 2021, 593, 120147. [Google Scholar] [CrossRef]
- Kempin, W.; Domsta, V.; Brecht, I.; Semmling, B.; Tillmann, S.; Weitschies, W.; Seidlitz, A. Development of a Dual Extrusion Printing Technique for an Acid- and Thermo-Labile Drug. Eur. J. Pharm. Sci. 2018, 123, 191–198. [Google Scholar] [CrossRef]
- Li, Q.; Wen, H.; Jia, D.; Guan, X.; Pan, H.; Yang, Y.; Yu, S.; Zhu, Z.; Xiang, R.; Pan, W. Preparation and Investigation of Controlled-Release Glipizide Novel Oral Device with Three-Dimensional Printing. Int. J. Pharm. 2017, 525, 5–11. [Google Scholar] [CrossRef] [PubMed]
- Pereira, G.G.; Figueiredo, S.; Fernandes, A.I.; Pinto, J.F. Polymer Selection for Hot-Melt Extrusion Coupled to Fused Deposition Modelling in Pharmaceutics. Pharmaceutics 2020, 12, 795. [Google Scholar] [CrossRef]
- Shin-Etsu AQOAT® Information Sheet; Shin-Etsu Chemical Co., Ltd.: Tokyo, Japan. 2018. Available online: https://www.metolose.jp/en/pharmaceutical/aqoat.html (accessed on 15 April 2021).
- Thakkar, R.; Pillai, A.R.; Zhang, J.; Zhang, Y.; Kulkarni, V.; Maniruzzaman, M. Novel On-Demand 3-Dimensional (3-d) Printed Tablets Using Fill Density as an Effective Release-Controlling Tool. Polymers 2020, 12, 1872. [Google Scholar] [CrossRef] [PubMed]
- Goyanes, A.; Fina, F.; Martorana, A.; Sedough, D.; Gaisford, S.; Basit, A.W. Development of Modified Release 3D Printed Tablets (Printlets) with Pharmaceutical Excipients Using Additive Manufacturing. Int. J. Pharm. 2017, 527, 21–30. [Google Scholar] [CrossRef]
- Goyanes, A.; Fernández-Ferreiro, A.; Majeed, A.; Gomez-Lado, N.; Awad, A.; Luaces-Rodríguez, A.; Gaisford, S.; Aguiar, P.; Basit, A.W. PET/CT Imaging of 3D Printed Devices in the Gastrointestinal Tract of Rodents. Int. J. Pharm. 2018, 536, 158–164. [Google Scholar] [CrossRef]
- Maroni, A.; Melocchi, A.; Parietti, F.; Foppoli, A.; Zema, L.; Gazzaniga, A. 3D Printed Multi-Compartment Capsular Devices for Two-Pulse Oral Drug Delivery. J. Control Release 2017, 268, 10–18. [Google Scholar] [CrossRef] [PubMed]
- Scoutaris, N.; Ross, S.A.; Douroumis, D. 3D Printed “Starmix” Drug Loaded Dosage Forms for Paediatric Applications. Pharm. Res. 2018, 35, 34. [Google Scholar] [CrossRef] [PubMed]
- Zhang, J.; Xu, P.; Vo, A.Q.; Bandari, S.; Yang, F.; Durig, T.; Repka, M.A. Development and Evaluation of Pharmaceutical 3D Printability for Hot Melt Extruded Cellulose-Based Filaments. J. Drug Deliv. Sci. Technol. 2019, 52, 292–302. [Google Scholar] [CrossRef] [PubMed]
- De Jaeghere, W.; De Beer, T.; Van Bocxlaer, J.; Remon, J.P.; Vervaet, C. Hot-Melt Extrusion of Polyvinyl Alcohol for Oral Immediate Release Applications. Int. J. Pharm. 2015, 492, 1–9. [Google Scholar] [CrossRef]
- Parteck MXP® Technical Information; Merck KGaA: Darmstadt, Germany. 2016. Available online: https://www.merckmillipore.com/ES/es/products/small-molecule-pharmaceuticals/formulation/solid-dosage-form/parteck-excipients/parteck-mxp/Ieyb.qB.lAcAAAFYLEQeWww_,nav (accessed on 23 January 2022).
- Crișan, A.G.; Porfire, A.; Ambrus, R.; Katona, G.; Rus, L.M.; Porav, A.S.; Ilyés, K.; Tomuță, I. Polyvinyl Alcohol-Based 3D Printed Tablets: Novel Insight into the Influence of Polymer Particle Size on Filament Preparation and Drug Release Performance. Pharmaceuticals 2021, 14, 418. [Google Scholar] [CrossRef]
- Gioumouxouzis, C.I.; Tzimtzimis, E.; Katsamenis, O.L.; Dourou, A.; Markopoulou, C.; Bouropoulos, N.; Tzetzis, D.; Fatouros, D.G. Fabrication of an Osmotic 3D Printed Solid Dosage Form for Controlled Release of Active Pharmaceutical Ingredients. Eur. J. Pharm. Sci. 2020, 143, 105176. [Google Scholar] [CrossRef] [PubMed]
- Palekar, S.; Nukala, P.K.; Mishra, S.M.; Kipping, T.; Patel, K. Application of 3D Printing Technology and Quality by Design Approach for Development of Age-Appropriate Pediatric Formulation of Baclofen. Int. J. Pharm. 2019, 556, 106–116. [Google Scholar] [CrossRef] [PubMed]
- Pereira, B.C.; Isreb, A.; Forbes, R.T.; Dores, F.; Habashy, R.; Petit, J.B.; Alhnan, M.A.; Oga, E.F. ‘Temporary Plasticiser’: A Novel Solution to Fabricate 3D Printed Patient-Centred Cardiovascular ‘Polypill’ Architectures. Eur. J. Pharm. Biopharm. 2019, 135, 94–103. [Google Scholar] [CrossRef] [PubMed]
- Saviano, M.; Aquino, R.P.; Del Gaudio, P.; Sansone, F.; Russo, P. Poly(Vinyl Alcohol) 3D Printed Tablets: The Effect of Polymer Particle Size on Drug Loading and Process Efficiency. Int. J. Pharm. 2019, 561, 1–8. [Google Scholar] [CrossRef]
- Bruce, L.D.; Shah, N.H.; Waseem Malick, A.; Infeld, M.H.; McGinity, J.W. Properties of Hot-Melt Extruded Tablet Formulations for the Colonic Delivery of 5-Aminosalicylic Acid. Eur. J. Pharm. Biopharm. 2005, 59, 85–97. [Google Scholar] [CrossRef]
- Liu, J.; Di, B.; Xu, L. Recent Advances in the Treatment of IBD: Targets, Mechanisms and Related Therapies. Cytokine Growth Factor Rev. 2023, 71–72, 1–12. [Google Scholar] [CrossRef]
- Shahdadi Sardo, H.; Saremnejad, F.; Bagheri, S.; Akhgari, A.; Afrasiabi Garekani, H.; Sadeghi, F. A Review on 5-Aminosalicylic Acid Colon-Targeted Oral Drug Delivery Systems. Int. J. Pharm. 2019, 558, 367–379. [Google Scholar] [CrossRef]
- Williams, C.; Panaccione, R.; Ghosh, S.; Rioux, K. Optimizing Clinical Use of Mesalazine (5-Aminosalicylic Acid) in Inflammatory Bowel Disease. Ther. Adv. Gastroenterol. 2011, 4, 237–248. [Google Scholar] [CrossRef]
- Goyanes, A.; Buanz, A.B.M.; Hatton, G.B.; Gaisford, S.; Basit, A.W. 3D Printing of Modified-Release Aminosalicylate (4-ASA and 5-ASA) Tablets. Eur. J. Pharm. Biopharm. 2015, 89, 157–162. [Google Scholar] [CrossRef]
- Xu, P.; Li, J.; Meda, A.; Osei-Yeboah, F.; Peterson, M.L.; Repka, M.; Zhan, X. Development of a Quantitative Method to Evaluate the Printability of Filaments for Fused Deposition Modeling 3D Printing. Int. J. Pharm. 2020, 588, 119760. [Google Scholar] [CrossRef]
- Costa, P.; Sousa Lobo, J.M. Modeling and Comparison of Dissolution Profiles. Eur. J. Pharm. Sci. 2001, 13, 123–133. [Google Scholar] [CrossRef] [PubMed]
- Peppas, N.A.; Sahlin, J.J. A Simple Equation for the Description of Solute Release. III. Coupling of Diffusion and Relaxation. Int. J. Pharm. 1989, 57, 169–172. [Google Scholar] [CrossRef]
- Lang, B.; Liu, S.; McGinity, J.W.; Williams, R.O. Effect of Hydrophilic Additives on the Dissolution and Pharmacokinetic Properties of Itraconazole-Enteric Polymer Hot-Melt Extruded Amorphous Solid Dispersions. Drug Dev. Ind. Pharm. 2016, 42, 429–445. [Google Scholar] [CrossRef] [PubMed]
- Roulon, S.; Soulairol, I.; Lavastre, V.; Payre, N.; Cazes, M.; Delbreilh, L.; Alié, J. Production of Reproducible Filament Batches for the Fabrication of 3D Printed Oral Forms. Pharmaceutics 2021, 13, 472. [Google Scholar] [CrossRef] [PubMed]
- Nokhodchi, A.; Okwudarue, O.N.; Valizadeh, H.; Momin, M.N. Cogrinding as a Tool to Produce Sustained Release Behavior for Theophylline Particles Containing Magnesium Stearate. AAPS PharmSciTech 2009, 10, 1243–1251. [Google Scholar] [CrossRef]
- Mirankó, M.; Trif, L.; Tóth, J.; Feczkó, T. Nanostructured Micronized Solid Dispersion of Crystalline-Amorphous Metronidazole Embedded in Amorphous Polymer Matrix Prepared by Nano Spray Drying. Adv. Powder Technol. 2021, 32, 2621–2633. [Google Scholar] [CrossRef]
- Bhagwat, D.A.; D’Souza, J.I. Formulation and Evaluation of Solid Self Micro Emulsifying Drug Delivery System Using Aerosil 200 as Solid Carrier. Int. Curr. Pharm. J. 2012, 1, 414–419. [Google Scholar] [CrossRef]
- Roulon, S.; Soulairol, I.; Cazes, M.; Lemierre, L.; Payre, N.; Delbreilh, L.; Alié, J. D-Sorbitol Physical Properties Effects on Filaments Used by 3D Printing Process for Personalized Medicine. Molecules 2021, 26, 3000. [Google Scholar] [CrossRef]
- de Assis, J.M.C.; Barbosa, E.J.; Bezzon, V.D.N.; Lourenço, F.R.; Carvalho, F.M.S.; Matos, J.R.; Araci Bou-Chacra, N.; Benmore, C.J.; Byrn, S.R.; Costa, F.N.; et al. Hot-Melt Extrudability of Amorphous Solid Dispersions of Flubendazole-Copovidone: An Exploratory Study of the Effect of Drug Loading and the Balance of Adjuvants on Extrudability and Dissolution. Int. J. Pharm. 2022, 614, 121456. [Google Scholar] [CrossRef]
- Crișan, A.G.; Iurian, S.; Porfire, A.; Rus, L.M.; Bogdan, C.; Casian, T.; Lucacel, R.C.; Turza, A.; Porav, S.; Tomuță, I. QbD Guided Development of Immediate Release FDM-3D Printed Tablets with Customizable API Doses. Int. J. Pharm. 2022, 613, 121411. [Google Scholar] [CrossRef]
- Zhang, J.; Feng, X.; Patil, H.; Tiwari, R.V.; Repka, M.A. Coupling 3D Printing with Hot-Melt Extrusion to Produce Controlled-Release Tablets. Int. J. Pharm. 2017, 519, 186–197. [Google Scholar] [CrossRef] [PubMed]
- Gorkem Buyukgoz, G.; Soffer, D.; Defendre, J.; Pizzano, G.M.; Davé, R.N. Exploring Tablet Design Options for Tailoring Drug Release and Dose via Fused Deposition Modeling (FDM) 3D Printing. Int. J. Pharm. 2020, 591, 119987. [Google Scholar] [CrossRef] [PubMed]
- European Directorate for the Quality of Medicines and Healthcare. European Pharmacopeia, 11th ed.; Council of Europe: Strasbourg, France, 2023. [Google Scholar]
- Markl, D.; Zeitler, J.A.; Rasch, C.; Michaelsen, M.H.; Müllertz, A.; Rantanen, J.; Rades, T.; Bøtker, J. Analysis of 3D Prints by X-ray Computed Microtomography and Terahertz Pulsed Imaging. Pharm. Res. 2017, 34, 1037–1052. [Google Scholar] [CrossRef] [PubMed]
- Skowyra, J.; Pietrzak, K.; Alhnan, M.A. Fabrication of Extended-Release Patient-Tailored Prednisolone Tablets via Fused Deposition Modelling (FDM) 3D Printing. Eur. J. Pharm. Sci. 2015, 68, 11–17. [Google Scholar] [CrossRef] [PubMed]











| Filament | Filament Composition (% w/w) | |||
|---|---|---|---|---|
| Polymer | Plasticizer | Drug | Lubricant/Glidant | |
| HPMCAS | HPMCAS-HG (88%) | TEC (10%) | - | MgS (2%) |
| Drug-loaded PVA | PVA-MXP (51%) | Sorbitol SI 150 (27%) | 5-ASA (20%) | Aerosil® (2%) |
| Printing Parameters | Set Values | |
|---|---|---|
| Bicompartmental Device | Spiral Compartment | |
| First layer height (mm) | 0.1 | 0.01 |
| Layer height (mm) | 0.05 | 0.05 |
| Platform temperature (°C) | 60 | 65 |
| First layer speed (mm/s) | 10 | 5 |
| Printing speed (mm/s) | 40 | 10 |
| Infill flowrate (%) | 100 | 100 |
| Infill density (%) | 100 | 100 |
| Infill pattern | Rectilinear | Rectilinear |
| Shells | 2 | 2 |
| Filament | Temperature (°C) | Screw Speed (rpm) | Flow Speed (mm/min) | Residence Time (min) | Diameter (mm) |
|---|---|---|---|---|---|
| HPMCAS-HG | 150 | 20 1 | 16.4 | 4 | 1.79 ± 0.05 |
| Drug-loaded PVA | 180 | 30 2 | 15.9 | 11 | 1.77 ± 0.04 |
| Filament | 3-Point Bending Test | Stiffness Test | |||
|---|---|---|---|---|---|
| Maximum Stress (g/mm²) | Strain 1 at Maximum Stress (%) | Brittleness 2 (kg/mm²)·% | Maximum Stress (g/mm²) | Stiffness (kg/mm²)·% | |
| HPMCAS-HG | 179.22 ± 21.14 RSD 11.80 | 329.46 ± 39.72 RSD 12.06 | 55.00 ± 6.57 RSD 11.95 | 2870.34 ± 303.65 RSD 10.58 | 74.48 ± 1.95 RSD 2.62 |
| Drug-loaded PVA | 132.83 ± 10.87 RSD 8.18 | 355.25 ± 44.51 RSD 12.53 | 44.94 ± 5.51 RSD 12.25 | 2523.49 ± 193.82 RSD 7.68 | 52.86 ± 5.61 RSD 10.61 |
| Weight (mg) | Diameter (mm) | Thickness (mm) |
|---|---|---|
| 811.3 ± 31.2 | 14.06 ± 0.07 | 5.09 ± 0.16 |
| RSD 3.8 | RSD 0.50 | RSD 3.24 |
| Kinetic Model | Parameters | First Phase (pH 1.2 and 6.8) | Second Phase (pH 7.4) |
| Higuchi (1) | kH (h−0.5) | 0.0060 | 0.0334 |
| r2adj | 0.9775 (F = 305) | 0.8703 (F = 28) | |
| Korsmeyer–Peppas (2) | n | 0.67 | 1.78 |
| kK (h−n) | 0.0022 | 0.000005 | |
| r2adj | 0.9495 (F = 133) | 0.9122 (F = 43) | |
| Peppas–Sahlin (3) | kd (h−0.44) | 0.0150 | −0.5252 |
| kr (h−0.88) | −0.0004 | 0.0222 | |
| r2adj | 0.9870 (F = 268) | 0.9975 (F = 785) | |
| Zero-order (4) | k0 (h−1) | 0.0003 | 0.0009 |
| r2adj | 0.9252 (F = 88) | 0.8963 (F = 36) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Shojaie, F.; Ferrero, C.; Caraballo, I. Development of 3D-Printed Bicompartmental Devices by Dual-Nozzle Fused Deposition Modeling (FDM) for Colon-Specific Drug Delivery. Pharmaceutics 2023, 15, 2362. https://doi.org/10.3390/pharmaceutics15092362
Shojaie F, Ferrero C, Caraballo I. Development of 3D-Printed Bicompartmental Devices by Dual-Nozzle Fused Deposition Modeling (FDM) for Colon-Specific Drug Delivery. Pharmaceutics. 2023; 15(9):2362. https://doi.org/10.3390/pharmaceutics15092362
Chicago/Turabian StyleShojaie, Fatemeh, Carmen Ferrero, and Isidoro Caraballo. 2023. "Development of 3D-Printed Bicompartmental Devices by Dual-Nozzle Fused Deposition Modeling (FDM) for Colon-Specific Drug Delivery" Pharmaceutics 15, no. 9: 2362. https://doi.org/10.3390/pharmaceutics15092362