Polymeric Nanosystems Applied for Metal-Based Drugs and Photosensitizers Delivery: The State of the Art and Recent Advancements
Abstract
:1. Introduction
2. Metal-Based Therapeutic Agents
3. Polymeric Nanocarriers for Metal-Based Therapeutic Agents’ Delivery
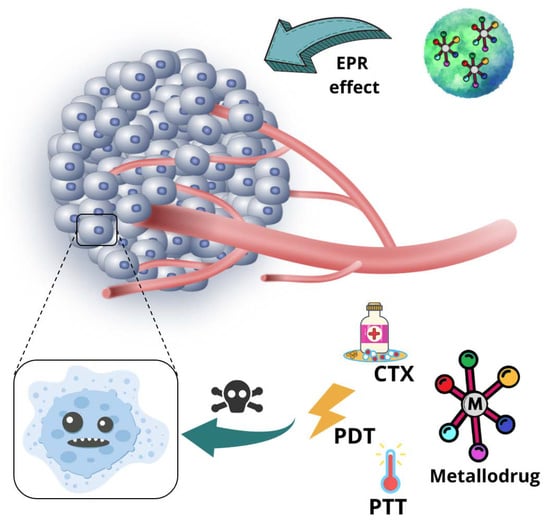
3.1. Advantages of Employing Polymeric Nanoparticles as Nanocarriers for Metal-Based Therapeutic Agents
3.2. Types of Structures of Polymeric Nanoparticles
3.3. Polymers Commonly Employed in NPs for Metal-Based Agent Delivery
3.4. Physical and Chemical Interactions between Metal-Based Agents and Polymeric NPs
3.5. Metal-Based Therapeutic Agents Loading Capacity into Polymeric NPs
3.6. Target Delivery and Controlled Release of Metal-Based Agents by Polymeric NPs
4. Non-Platinum-Containing Metal Therapeutic Agents Loaded into Polymeric Nanosystems
4.1. Ruthenium Complexes
4.1.1. Mono- and Dinuclear Ruthenium(II/III) Based Complexes
4.1.2. Ruthenium(II)-Based Polypyridine Complexes
4.1.3. Organoruthenium Compounds
4.2. Gallium Complexes
4.3. Gold Complexes
4.4. Copper Complexes
4.5. Zinc Complexes
4.6. Iridium Complexes
4.7. Other Metal-Based Compounds
5. Metal-Based Agents Incorporated into Polymeric Nanocarriers Applied for Other Therapeutic Approaches beyond Cancer Treatment
6. New Trends in Nanotechnology Involving Polymeric Nanosized Systems and Metal-Based Compounds
6.1. Metal Coordination-Driven Polymeric Nanosystems for Drug Delivery
6.2. Polymeric Nanocarrier for Delivery of Free Metal Ions
6.3. Polymeric Nanosystems Conjugated to a Metallic Ion Chelator
6.4. Polymer Dots Applied as Phototheranostic Agents
6.5. Polymer Functionalized Upconverting Nanoparticles
7. Conclusions
Funding
Acknowledgments
Conflicts of Interest
Abbreviations
| 6-MP | 6-mercaptopurine |
| CDT | Chemodynamic therapy |
| CTX | Chemotherapy |
| DOX | doxorubicin |
| DSPE | 1,2-distearoyl-sn-glycero-3-phosphoethanolamine |
| DTX | Docetaxel |
| EPR | enhanced permeation and retention |
| FA | Folic acid |
| FeTPP | iron(II) tetraphenylporphyrin |
| FRET | Fluorescence resonance energy transfer |
| GSH | Glutathione |
| HA | Hyaluronic acid |
| HMPA | N-(2-hydroxypropyl)methacrylamide |
| NPs | Nanoparticles |
| NIR | Near-infrared light |
| PACT | Photoactivated chemotherapy |
| PDIM | Photodynamic inactivation of microorganisms |
| PDT | Photodynamic therapy |
| PEG | poly(ethylene glycol) = poly(ethylene oxide) (PEO) |
| PEO | poly(ethylene oxide) = poly(ethylene glycol) (PEG) |
| Pdots | Polymer dots |
| PF127 | Pluronic® F127 |
| PF68 | Pluronic® F68 |
| PGA | poly(glycolic acid) |
| PLA | polylactide |
| PLGA | poly(lactic-co-glycolic acid) |
| PP123 | Pluronic® P123 |
| PPO | poly(propylene oxide) |
| PS | Photosensitizer |
| PTT | Photothermal therapy |
| ROS | Reactive oxygen species |
| SMA | poly(styrene-maleic acid) |
| UCNPs | Upconverting nanoparticles |
| ZnPC | Zinc(II) phthalocyanine |
| ZnPP | Zinc(II) protoporphyrin |
| ZnPPIX | Zinc(II) protoporphyrin-IX |
References
- Napier, M.E.; DeSimone, J.M. Nanoparticle Drug Delivery Platform. Polym. Rev. 2007, 47, 321–327. [Google Scholar] [CrossRef]
- Cho, H.; Lai, T.C.; Tomoda, K.; Kwon, G.S. Polymeric Micelles for Multi-Drug Delivery in Cancer. AAPS PharmSciTech 2014, 16, 10–20. [Google Scholar] [CrossRef] [Green Version]
- George, A.; Shah, P.A.; Shrivastav, P.S. Natural biodegradable polymers based nano-formulations for drug delivery: A review. Int. J. Pharm. 2019, 561, 244–264. [Google Scholar] [CrossRef] [PubMed]
- Silva, K.M.M.N.; de Carvalho, D.L.; Valente, V.M.M.; Rubio, J.C.C.; Faria, P.E.; Silva-Caldeira, P.P. Concomitant and controlled release of furazolidone and bismuth(III) incorporated in a cross-linked sodium alginate-carboxymethyl cellulose hydrogel. Int. J. Biol. Macromol. 2018, 126, 359–366. [Google Scholar] [CrossRef] [PubMed]
- Sumi, V.S.; Kala, R.; Praveen, R.S.; Rao, T.P. Imprinted polymers as drug delivery vehicles for metal-based anti-inflammatory drug. Int. J. Pharm. 2008, 349, 30–37. [Google Scholar] [CrossRef]
- Nave, M.; Castro, R.E.; Rodrigues, C.M.; Casini, A.; Soveral, G.; Gaspar, M.M. Nanoformulations of a potent copper-based aquaporin inhibitor with cytotoxic effect against cancer cells. Nanomedicine 2016, 11, 1817–1830. [Google Scholar] [CrossRef] [Green Version]
- Gorshkov, N.I.; Murko, A.Y.; Gavrilova, I.I.; Bezrukova, M.A.; Kipper, I.; Shatik, S.V.; Tokarev, A.V.; Krasikov, V.D.; Panarin, E.F. Metal-Polymer Complexes of Gallium/Gallium-68 with Copolymers of N-Vinylpyrrolidonewith N-Vinylformamideand N-Vinyliminodiacetic Acid: A Hint for Radiolabeling of Water-Soluble Synthetic Flexible Chain Macromolecules. Polymers 2020, 12, 2889. [Google Scholar] [CrossRef]
- Pinho, J.O.; Amaral, J.D.; E Castro, R.; Rodrigues, C.M.; Casini, A.; Soveral, G.; Gaspar, M.M. Copper complex nanoformulations featuring highly promising therapeutic potential in murine melanoma models. Nanomedicine 2019, 14, 835–850. [Google Scholar] [CrossRef]
- Ma, H.; Darmawan, E.T.; Zhang, M.; Zhang, L.; Bryers, J.D. Development of a poly(ether urethane) system for the controlled release of two novel anti-biofilm agents based on gallium or zinc and its efficacy to prevent bacterial biofilm formation. J. Control. Release 2013, 172, 1035–1044. [Google Scholar] [CrossRef] [Green Version]
- Demirci, S.; Doğan, A.; Türkmen, N.B.; Telci, D.; Rizvanov, A.; Şahin, F. Schiff base-Poloxamer P85 combination demonstrates chemotherapeutic effect on prostate cancer cells in vitro. Biomed. Pharmacother. 2017, 86, 492–501. [Google Scholar] [CrossRef]
- Matos, M.J.; Labão-Almeida, C.; Sayers, C.; Dada, O.; Tacke, M.; Bernardes, G.J.L. Synthesis and Biological Evaluation of Homogeneous Thiol-Linked NHC*-Au-Albumin and -Trastuzumab Bioconjugates. Chem.–A Eur. J. 2018, 24, 12250–12253. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Adhikari, H.S.; Garai, A.; Thapa, M.; Adhikari, R.; Yadav, P.N. Chitosan functionalized thiophene-2-thiosemicarbazones, and their copper(II) complexes: Synthesis, characterization, and anticancer activity. J. Macromol. Sci. Part A 2022, 59, 211–227. [Google Scholar] [CrossRef]
- Callari, M.; Aldrich-Wright, J.R.; de Souza, P.L.; Stenzel, M.H. Polymers with platinum drugs and other macromolecular metal complexes for cancer treatment. Prog. Polym. Sci. 2014, 39, 1614–1643. [Google Scholar] [CrossRef]
- Oberoi, H.S.; Nukolova, N.V.; Kabanov, A.V.; Bronich, T.K. Nanocarriers for delivery of platinum anticancer drugs. Adv. Drug Deliv. Rev. 2013, 65, 1667–1685. [Google Scholar] [CrossRef] [Green Version]
- Xiao, H.; Yan, L.; Dempsey, E.M.; Song, W.; Qi, R.; Li, W.; Huang, Y.; Jing, X.; Zhou, D.; Ding, J.; et al. Recent progress in polymer-based platinum drug delivery systems. Prog. Polym. Sci. 2018, 87, 70–106. [Google Scholar] [CrossRef]
- Johnstone, T.C.; Suntharalingam, K.; Lippard, S.J. The Next Generation of Platinum Drugs: Targeted Pt(II) Agents, Nanoparticle Delivery, and Pt(IV) Prodrugs. Chem. Rev. 2016, 116, 3436–3486. [Google Scholar] [CrossRef] [Green Version]
- Rak, J.; Pouckova, P.; Benes, J.; Vetvicka, D. Drug Delivery Systems for Phthalocyanines for Photodynamic Therapy. Anticancer Res. 2019, 39, 3323–3339. [Google Scholar] [CrossRef] [Green Version]
- Allemann, E.; Brasseur, N.; Benrezzak, O.; Rousseau, J.; Kudrevich, S.V.; Boyle, R.W.; Leroux, J.-C.; Gurny, R.; E van Lier, J. PEG-coated Poly(lactic acid) Nanoparticles for the Delivery of Hexadecafluoro Zinc Phthalocyanine to EMT-6 Mouse Mammary Tumours. J. Pharm. Pharmacol. 1995, 47, 382–387. [Google Scholar] [CrossRef]
- Leroux, J.-C.; Roux, E.; Le Garrec, D.; Hong, K.; Drummond, D.C. N-isopropylacrylamide copolymers for the preparation of pH-sensitive liposomes and polymeric micelles. J. Control. Release 2001, 72, 71–84. [Google Scholar] [CrossRef]
- Poursharifi, M.; Wlodarczyk, M.T.; Mieszawska, A.J. Nano-Based Systems and Biomacromolecules as Carriers for Metallodrugs in Anticancer Therapy. Inorganics 2018, 7, 2. [Google Scholar] [CrossRef] [Green Version]
- Han, X.; Sun, J.; Wang, Y.; He, Z. Recent Advances in Platinum (IV) Complex-Based Delivery Systems to Improve Platinum (II) Anticancer Therapy. Med. Res. Rev. 2015, 35, 1268–1299. [Google Scholar] [CrossRef] [PubMed]
- Gou, Y.; Huang, G.; Li, J.; Yang, F.; Liang, H. Versatile delivery systems for non-platinum metal-based anticancer therapeutic agents. Co-ord. Chem. Rev. 2021, 441, 213975. [Google Scholar] [CrossRef]
- Boros, E.; Dyson, P.J.; Gasser, G. Classification of Metal-Based Drugs according to Their Mechanisms of Action. Chem 2020, 6, 41–60. [Google Scholar] [CrossRef]
- Farinha, P.; Pinho, J.O.; Matias, M.; Gaspar, M.M. Nanomedicines in the treatment of colon cancer: A focus on metallodrugs. Drug Deliv. Transl. Res. 2021, 12, 49–66. [Google Scholar] [CrossRef]
- Gandosio, A.; Purkait, K.; Gasser, G. Recent Approaches towards the Development of Ru(II) Polypyridyl Complexes for Anticancer Photodynamic Therapy. CHIMIA 2021, 75. [Google Scholar] [CrossRef]
- Yano, S.; Hirohara, S.; Obata, M.; Hagiya, Y.; Ogura, S.-I.; Ikeda, A.; Kataoka, H.; Tanaka, M.; Joh, T. Current states and future views in photodynamic therapy. J. Photochem. Photobiol. C: Photochem. Rev. 2011, 12, 46–67. [Google Scholar] [CrossRef]
- Yu, Y.; Xu, Q.; He, S.; Xiong, H.; Zhang, Q.; Xu, W.; Ricotta, V.; Bai, L.; Zhang, Q.; Yu, Z.; et al. Recent advances in delivery of photosensitive metal-based drugs. Co-ord. Chem. Rev. 2019, 387, 154–179. [Google Scholar] [CrossRef]
- Ringhieri, P.; Morelli, G.; Accardo, A. Supramolecular Delivery Systems for Non-Platinum Metal-Based Anticancer Drugs. Crit. Rev. Ther. Drug Carr. Syst. 2017, 34, 149–183. [Google Scholar] [CrossRef]
- Arias, J.L. (Ed.) Nanotechnology and Drug Delivery, Volume One; CRC Press: Boca Raton, FL, USA, 2014. [Google Scholar] [CrossRef]
- Barry, N.P.E.; Sadler, P.J. Challenges for Metals in Medicine: How Nanotechnology May Help to Shape the Future. ACS Nano 2013, 7, 5654–5659. [Google Scholar] [CrossRef]
- Henna, T.; Pramod, K. Graphene quantum dots redefine nanobiomedicine. Mater. Sci. Eng. C 2020, 110, 110651. [Google Scholar] [CrossRef]
- Thomas, S.C.; Sharma, H.; Mishra, P.K.; Talegaonkar, S. Ceramic Nanoparticles: Fabrication Methods and Applications in Drug Delivery. Curr. Pharm. Des. 2015, 21, 6165–6188. [Google Scholar] [CrossRef] [PubMed]
- Cao, J.; Li, X.; Tian, H. Metal-Organic Framework (MOF)-Based Drug Delivery. Curr. Med. Chem. 2020, 27, 5949–5969. [Google Scholar] [CrossRef] [PubMed]
- Ojea-Jimenez, I.; Comenge, J.; Garcia-Fernandez, L.; Megson, Z.; Casals, E.; Puntes, V. Engineered Inorganic Nanoparticles for Drug Delivery Applications. Curr. Drug Metab. 2013, 14, 518–530. [Google Scholar] [CrossRef] [Green Version]
- MacEwan, S.R.; Callahan, D.J.; Chilkoti, A. Stimulus-responsive macromolecules and nanoparticles for cancer drug delivery. Nanomedicine 2010, 5, 793–806. [Google Scholar] [CrossRef] [Green Version]
- Hoffman, A.S. The origins and evolution of “controlled” drug delivery systems. J. Control. Release 2008, 132, 153–163. [Google Scholar] [CrossRef]
- Kamaly, N.; Xiao, Z.; Valencia, P.M.; Radovic-Moreno, A.F.; Farokhzad, O.C. Targeted polymeric therapeutic nanoparticles: Design, development and clinical translation. Chem. Soc. Rev. 2012, 41, 2971–3010. [Google Scholar] [CrossRef] [PubMed]
- Pearson, S.; Lu, H.; Stenzel, M.H. Glycopolymer Self-Assemblies with Gold(I) Complexed to the Core as a Delivery System for Auranofin. Macromolecules 2015, 48, 1065–1076. [Google Scholar] [CrossRef]
- Ding, J.; Chen, L.; Xiao, C.; Chen, L.; Zhuang, X.; Chen, X. Noncovalent interaction-assisted polymeric micelles for controlled drug delivery. Chem. Commun. 2014, 50, 11274–11290. [Google Scholar] [CrossRef]
- Abyaneh, H.S.; Vakili, M.R.; Zhang, F.; Choi, P.; Lavasanifar, A. Rational design of block copolymer micelles to control burst drug release at a nanoscale dimension. Acta Biomater. 2015, 24, 127–139. [Google Scholar] [CrossRef]
- Hanafy, N.A.N.; El-Kemary, M.; Leporatti, S. Micelles structure development as a strategy to improve smart cancer therapy. Cancers 2018, 10, 238. [Google Scholar] [CrossRef] [Green Version]
- Debele, T.A.; Mekuria, S.L.; Tsai, H.-C. A pH-sensitive micelle composed of heparin, phospholipids, and histidine as the carrier of photosensitizers: Application to enhance photodynamic therapy of cancer. Int. J. Biol. Macromol. 2017, 98, 125–138. [Google Scholar] [CrossRef] [PubMed]
- Song, H.; Wang, R.; Xiao, H.; Cai, H.; Zhang, W.; Xie, Z.; Huang, Y.; Jing, X.; Liu, T. A cross-linked polymeric micellar delivery system for cisplatin(IV) complex. Eur. J. Pharm. Biopharm. 2013, 83, 63–75. [Google Scholar] [CrossRef] [PubMed]
- Neves, A.R.; Reis, S. (Eds.) Nanoparticles in Life Sciences and Biomedicine; Jenny Stanford Publishing: New York, NY, USA, 2018. [Google Scholar] [CrossRef]
- Avgoustakis, K. Pegylated poly(lactide) and poly(lactide-co-glycolide) nanoparticles: Preparation, properties and possible applications in drug delivery. Curr. Drug Deliv. 2004, 1, 321–333. [Google Scholar] [CrossRef] [PubMed]
- Gill, M.R.; Menon, J.U.; Jarman, P.J.; Owen, J.; Skaripa-Koukelli, I.; Able, S.; Thomas, J.A.; Carlisle, R.; Vallis, K.A. 111In-labelled polymeric nanoparticles incorporating a ruthenium-based radiosensitizer for EGFR-targeted combination therapy in oesophageal cancer cells. Nanoscale 2018, 10, 10596–10608. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chung, C.Y.-S.; Fung, S.-K.; Tong, K.-C.; Wan, P.-K.; Lok, C.-N.; Huang, Y.; Chen, T.; Che, C.-M. A multi-functional PEGylated gold(iii) compound: Potent anti-cancer properties and self-assembly into nanostructures for drug co-delivery. Chem. Sci. 2016, 8, 1942–1953. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Conte, C.; Ungaro, F.; Maglio, G.; Tirino, P.; Siracusano, G.; Sciortino, M.; Leone, N.; Palma, G.; Barbieri, A.; Arra, C.; et al. Biodegradable core-shell nanoassemblies for the delivery of docetaxel and Zn(II)-phthalocyanine inspired by combination therapy for cancer. J. Control. Release 2013, 167, 40–52. [Google Scholar] [CrossRef] [PubMed]
- Huang, Z.; Xiao, H.; Lu, X.; Yan, W.; Ji, Z. Enhanced photo/chemo combination efficiency against bladder tumor by encapsulation of DOX and ZnPC into in situ-formed thermosensitive polymer hydrogel. Int. J. Nanomed. 2018, 13, 7623–7631. [Google Scholar] [CrossRef] [Green Version]
- Heffeter, P.; Riabtseva, A.; Senkiv, J.; Kowol, C.R.; Körner, W.; Jungwith, U.; Mitina, N.; Keppler, B.K.; Konstantinova, T.; Yanchuk, I.; et al. Nanoformulation Improves Activity of the (pre)Clinical Anticancer Ruthenium Complex KP1019. J. Biomed. Nanotechnol. 2014, 10, 877–884. [Google Scholar] [CrossRef]
- Dickerson, M.; Howerton, B.; Bae, Y.; Glazer, E.C. Light-sensitive ruthenium complex-loaded cross-linked polymeric nanoassemblies for the treatment of cancer. J. Mater. Chem. B 2015, 4, 394–408. [Google Scholar] [CrossRef] [Green Version]
- Collins, A.M.; Zabkiewicz, J.; Ghiggi, C.; Hauser, J.C.; Burnett, A.K.; Mann, S. Tris(8-hydroxyquinolinato)gallium(III)-Loaded Copolymer Micelles as Cytotoxic Nanoconstructs for Cosolvent-Free Organometallic Drug Delivery. Small 2011, 7, 1635–1640. [Google Scholar] [CrossRef]
- He, M.; Chen, F.; Shao, D.; Weis, P.; Wei, Z.; Sun, W. Photoresponsive metallopolymer nanoparticles for cancer theranostics. Biomaterials 2021, 275, 120915. [Google Scholar] [CrossRef] [PubMed]
- Noh, J.; Jung, E.; Lee, J.; Hyun, H.; Hong, S.; Lee, D. Engineered Polymeric Micelles for Combinational Oxidation Anticancer Therapy through Concurrent HO-1 Inhibition and ROS Generation. Biomacromolecules 2019, 20, 1109–1117. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Y.; Chan, H.F.; Leong, K.W. Advanced materials and processing for drug delivery: The past and the future. Adv. Drug Deliv. Rev. 2012, 65, 104–120. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sun, W.; Wen, Y.; Thiramanas, R.; Chen, M.; Han, J.; Gong, N.; Wagner, M.; Jiang, S.; Meijer, M.; Bonnet, S.; et al. Red-Light-Controlled Release of Drug-Ru Complex Conjugates from Metallopolymer Micelles for Phototherapy in Hypoxic Tumor Environments. Adv. Funct. Mater. 2018, 28. [Google Scholar] [CrossRef] [Green Version]
- Fischer, B.; Heffeter, P.; Kryeziu, K.; Gille, L.; Meier, S.M.; Berger, W.; Kowol, C.R.; Keppler, B.K. Poly(lactic acid) nanoparticles of the lead anticancer ruthenium compound KP1019 and its surfactant-mediated activation. Dalton Trans. 2013, 43, 1096–1104. [Google Scholar] [CrossRef] [Green Version]
- Mir, M.; Ahmed, N.; Rehman, A.U. Recent applications of PLGA based nanostructures in drug delivery. Colloids Surf. B Biointerfaces 2017, 159, 217–231. [Google Scholar] [CrossRef]
- Wen, R.; Umeano, A.C.; Chen, P.; Farooqi, A.A. Polymer-Based Drug Delivery Systems for Cancer. Crit. Rev. Ther. Drug Carr. Syst. 2018, 35, 521–553. [Google Scholar] [CrossRef]
- Gopinath, P.; Kumar, S.U.; Matai, I.; Bhushan, B.; Malwal, D.; Sachdev, A.; Dubey, P. Cancer Nanotheranostics; Springer: Singapore, 2015; pp. 1–93. [Google Scholar] [CrossRef]
- Bœuf, G.; Roullin, G.V.; Moreau, J.; Van Gulick, L.; Pineda, N.Z.; Terryn, C.; Ploton, D.; Andry, M.C.; Chuburu, F.; Dukic, S.; et al. Encapsulated Ruthenium(II) Complexes in Biocompatible Poly(d,l-lactide-co-glycolide) Nanoparticles for Application in Photodynamic Therapy. ChemPlusChem 2014, 79, 171–180. [Google Scholar] [CrossRef]
- Ricci-Júnior, E.; Marchetti, J.M. Zinc(II) phthalocyanine loaded PLGA nanoparticles for photodynamic therapy use. Int. J. Pharm. 2006, 310, 187–195. [Google Scholar] [CrossRef]
- Soliman, N.; Sol, V.; Ouk, T.-S.; Thomas, C.M.; Gasser, G. Encapsulation of a Ru(II) Polypyridyl Complex into Polylactide Nanoparticles for Antimicrobial Photodynamic Therapy. Pharmaceutics 2020, 12, 961. [Google Scholar] [CrossRef]
- Lorenzoni, D.; Souto, C.A.Z.; Araujo, M.B.; Berger, C.D.S.; da Silva, L.C.D.; Baratti, M.O.; Ribeiro, J.N.; Endringer, D.C.; Guimarães, M.C.C.; da Silva, A.R. PLGA-PEG nanoparticles containing gallium phthalocyanine: Preparation, optimization and analysis of its photodynamic efficiency on red blood cell and Hepa-1C1C7. J. Photochem. Photobiol. B Biol. 2019, 198, 111582. [Google Scholar] [CrossRef] [PubMed]
- Eskandari, A.; Boodram, J.N.; Cressey, P.B.; Lu, C.; Bruno, P.M.; Hemann, M.T.; Suntharalingam, K. The breast cancer stem cell potency of copper(ii) complexes bearing nonsteroidal anti-inflammatory drugs and their encapsulation using polymeric nanoparticles. Dalton Trans. 2016, 45, 17867–17873. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chen, W.; Yang, W.; Chen, P.; Huang, Y.; Li, F. Disulfiram Copper Nanoparticles Prepared with a Stabilized Metal Ion Ligand Complex Method for Treating Drug-Resistant Prostate Cancers. ACS Appl. Mater. Interfaces 2018, 10, 41118–41128. [Google Scholar] [CrossRef]
- Hwang, D.; Ramsey, J.D.; Kabanov, A.V. Polymeric micelles for the delivery of poorly soluble drugs: From nanoformulation to clinical approval. Adv. Drug Deliv. Rev. 2020, 156, 80–118. [Google Scholar] [CrossRef] [PubMed]
- Bodratti, A.M.; Alexandridis, P. Formulation of Poloxamers for Drug Delivery. J. Funct. Biomater. 2018, 9, 11. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kabanov, A.V.; Batrakova, E.V.; Alakhov, V.Y. Pluronic® block copolymers as novel polymer therapeutics for drug and gene delivery. J. Control. Release 2002, 82, 189–212. [Google Scholar] [CrossRef]
- Lee, M.H.; Shin, G.H.; Park, H.J. Solid lipid nanoparticles loaded thermoresponsive pluronic-xanthan gum hydrogel as a transdermal delivery system. J. Appl. Polym. Sci. 2017, 135. [Google Scholar] [CrossRef]
- Managa, M.; Ngoy, B.P.; Mafukidze, D.; Nyokong, T. Incorporation of metal free and Ga 5,10,15,20-tetrakis(4-bromophenyl) porphyrin into Pluronic F127-folic acid micelles. J. Lumin. 2018, 194, 739–746. [Google Scholar] [CrossRef]
- Scintilla, S.; Brustolin, L.; Gambalunga, A.; Chiara, F.; Trevisan, A.; Nardon, C.; Fregona, D. Ru(III) anticancer agents with aromatic and non-aromatic dithiocarbamates as ligands: Loading into nanocarriers and preliminary biological studies. J. Inorg. Biochem. 2016, 165, 159–169. [Google Scholar] [CrossRef]
- Karges, J.; Chao, H.; Gasser, G. Synthesis, Characterization, and Biological Evaluation of the Polymeric Encapsulation of a Ruthenium(II) Polypyridine Complex with Pluronic F-127/Poloxamer-407 for Photodynamic Therapy Applications. Eur. J. Inorg. Chem. 2020, 2020, 3242–3248. [Google Scholar] [CrossRef]
- Managa, M.; Ngoy, B.P.; Mafukidze, D.; Britton, J.; Nyokong, T. Photophysical studies of meso-tetrakis(4-nitrophenyl) and meso-tetrakis(4-sulfophenyl) gallium porphyrins loaded into Pluronic F127 polymeric micelles. J. Photochem. Photobiol. A Chem. 2017, 348, 179–187. [Google Scholar] [CrossRef]
- Kulkarni, C.V. Lipid Self-Assemblies and Nanostructured Emulsions for Cosmetic Formulations. Cosmetics 2016, 3, 37. [Google Scholar] [CrossRef] [Green Version]
- Ravera, M.; Gabano, E.; McGlinchey, M.; Osella, D. A view on multi-action Pt(IV) antitumor prodrugs. Inorganica Chim. Acta 2019, 492, 32–47. [Google Scholar] [CrossRef]
- Villemin, E.; Ong, Y.C.; Thomas, C.M.; Gasser, G. Polymer encapsulation of ruthenium complexes for biological and medicinal applications. Nat. Rev. Chem. 2019, 3, 261–282. [Google Scholar] [CrossRef]
- Duan, X.; Liu, D.; Chan, C.; Lin, W. Polymeric Micelle-Mediated Delivery of DNA-Targeting Organometallic Complexes for Resistant Ovarian Cancer Treatment. Small 2015, 11, 3962–3972. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sun, W.; Parowatkin, M.; Steffen, W.; Butt, H.-J.; Mailänder, V.; Wu, S. Ruthenium-Containing Block Copolymer Assemblies: Red-Light-Responsive Metallopolymers with Tunable Nanostructures for Enhanced Cellular Uptake and Anticancer Phototherapy. Adv. Heal. Mater. 2015, 5, 467–473. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.; Pitto-Barry, A.; Habtemariam, A.; Romero-Canelon, I.; Sadler, P.J.; Barry, N.P.E. Nanoparticles of chitosan conjugated to organo-ruthenium complexes. Inorg. Chem. Front. 2016, 3, 1058–1064. [Google Scholar] [CrossRef] [Green Version]
- Moreira, T.; Francisco, R.; Comsa, E.; Duban-Deweer, S.; Labas, V.; Teixeira-Gomes, A.-P.; Combes-Soia, L.; Marques, F.; Matos, A.; Favrelle-Huret, A.; et al. Polymer “ruthenium-cyclopentadienyl” conjugates - New emerging anti-cancer drugs. Eur. J. Med. Chem. 2019, 168, 373–384. [Google Scholar] [CrossRef]
- Shen, S.; Wu, Y.; Liu, Y.; Wu, D. High drug-loading nanomedicines: Progress, current status, and prospects. Int. J. Nanomed. 2017, 12, 4085–4109. [Google Scholar] [CrossRef] [Green Version]
- Alves, S.R.; Colquhoun, A.; Wu, X.Y.; Silva, D.D.O. Synthesis of terpolymer-lipid encapsulated diruthenium(II,III)-anti-inflammatory metallodrug nanoparticles to enhance activity against glioblastoma cancer cells. J. Inorg. Biochem. 2019, 205, 110984. [Google Scholar] [CrossRef]
- Py-Daniel, K.R.; Namban, J.S.; de Andrade, L.R.; de Souza, P.E.; Paterno, L.G.; Azevedo, R.B.; Soler, M.A. Highly efficient photodynamic therapy colloidal system based on chloroaluminum phthalocyanine/pluronic micelles. Eur. J. Pharm. Biopharm. 2016, 103, 23–31. [Google Scholar] [CrossRef] [PubMed]
- Siqueira-Moura, M.P.; Primo, F.L.; Espreafico, E.M.; Tedesco, A.C. Development, characterization, and photocytotoxicity assessment on human melanoma of chloroaluminum phthalocyanine nanocapsules. Mater. Sci. Eng. C 2013, 33, 1744–1752. [Google Scholar] [CrossRef] [PubMed]
- Zatorska, M.; Łazarski, G.; Maziarz, U.; Wilkosz, N.; Honda, T.; Yusa, S.-I.; Bednar, J.; Jamróz, D.; Kepczynski, M. Drug-loading capacity of polylactide-based micro- and nanoparticles – Experimental and molecular modeling study. Int. J. Pharm. 2020, 591, 120031. [Google Scholar] [CrossRef] [PubMed]
- Chan, L.; Huang, Y.; Chen, T. Cancer-targeted tri-block copolymer nanoparticles as payloads of metal complexes to achieve enhanced cancer theranosis. J. Mater. Chem. B 2016, 4, 4517–4525. [Google Scholar] [CrossRef]
- Li, J.; Du, N.; Tan, Y.; Hsu, H.-Y.; Tan, C.; Jiang, Y. Conjugated Polymer Nanoparticles Based on Copper Coordination for Real-Time Monitoring of pH-Responsive Drug Delivery. ACS Appl. Bio Mater. 2021, 4, 2583–2590. [Google Scholar] [CrossRef]
- de Paula, C.S.; Tedesco, A.C.; Primo, F.L.; Vilela, J.M.C.; Andrade, M.S.; Mosqueira, V.C.F. Chloroaluminium phthalocyanine polymeric nanoparticles as photosensitisers: Photophysical and physicochemical characterisation, release and phototoxicity in vitro. Eur. J. Pharm. Sci. 2013, 49, 371–381. [Google Scholar] [CrossRef]
- Wang, J.; Liu, L.; Ying, L.; Chen, L. Acid-responsive metallo-supramolecular micelles for synergistic chemo-photodynamic therapy. Eur. Polym. J. 2017, 93, 87–96. [Google Scholar] [CrossRef]
- Peng, X.; Pan, Q.; Zhang, B.; Wan, S.; Li, S.; Luo, K.; Pu, Y.; He, B. Highly Stable, Coordinated Polymeric Nanoparticles Loading Copper(II) Diethyldithiocarbamate for Combinational Chemo/Chemodynamic Therapy of Cancer. Biomacromolecules 2019, 20, 2372–2383. [Google Scholar] [CrossRef]
- Matsumura, Y.; Maeda, H. A new concept for macromolecular therapeutics in cancer chemotherapy: Mechanism of tumoritropic accumulation of proteins and the antitumor agent smancs. Cancer Res. 1986, 46, 6387–6392. [Google Scholar]
- Danhier, F. To exploit the tumor microenvironment: Since the EPR effect fails in the clinic, what is the future of nanomedicine? J. Control. Release 2016, 244, 108–121. [Google Scholar] [CrossRef]
- Drozdov, A.S.; Nikitin, P.I.; Rozenberg, J.M. Systematic Review of Cancer Targeting by Nanoparticles Revealed a Global Association between Accumulation in Tumors and Spleen. Int. J. Mol. Sci. 2021, 22, 13011. [Google Scholar] [CrossRef] [PubMed]
- Sindhwani, S.; Syed, A.M.; Ngai, J.; Kingston, B.R.; Maiorino, L.; Rothschild, J.; Macmillan, P.; Zhang, Y.; Rajesh, N.U.; Hoang, T.; et al. The entry of nanoparticles into solid tumours. Nat. Mater. 2020, 19, 566–575. [Google Scholar] [CrossRef] [PubMed]
- Neuse, E.W. Synthetic Polymers as Drug-Delivery Vehicles in Medicine. Met. Drugs 2008, 2008, 469531. [Google Scholar] [CrossRef] [Green Version]
- Brustolin, L.; Pettenuzzo, N.; Nardon, C.; Quarta, S.; Montagner, I.; Pontisso, P.; Rosato, A.; Conte, P.; Merigliano, S.; Fregona, D. Labelled micelles for the delivery of cytotoxic Cu(II) and Ru(III) compounds in the treatment of aggressive orphan cancers: Design and biological in vitro data. J. Inorg. Biochem. 2020, 213, 111259. [Google Scholar] [CrossRef]
- Karges, J.; Tharaud, M.; Gasser, G. Polymeric Encapsulation of a Ru(II)-Based Photosensitizer for Folate-Targeted Photodynamic Therapy of Drug Resistant Cancers. J. Med. Chem. 2021, 64, 4612–4622. [Google Scholar] [CrossRef]
- Pramanik, A.; Laha, D.; Dash, S.K.; Chattopadhyay, S.; Roy, S.; Das, D.K.; Pramanik, P.; Karmakar, P. An in-vivo study for targeted delivery of copper-organic complex to breast cancer using chitosan polymer nanoparticles. Mater. Sci. Eng. C 2016, 68, 327–337. [Google Scholar] [CrossRef]
- Su, S.; Kang, P.M. Recent Advances in Nanocarrier-Assisted Therapeutics Delivery Systems. Pharmaceutics 2020, 12, 837. [Google Scholar] [CrossRef]
- Zeng, X.; Wang, Y.; Han, J.; Sun, W.; Butt, H.; Liang, X.; Wu, S. Fighting against Drug-Resistant Tumors using a Dual-Responsive Pt(IV)/Ru(II) Bimetallic Polymer. Adv. Mater. 2020, 32, 2004766. [Google Scholar] [CrossRef]
- Lin, Y.-X.; Gao, Y.-J.; Wang, Y.; Qiao, Z.-Y.; Fan, G.; Qiao, S.-L.; Zhang, R.-X.; Wang, L.; Wang, H. pH-Sensitive Polymeric Nanoparticles with Gold(I) Compound Payloads Synergistically Induce Cancer Cell Death through Modulation of Autophagy. Mol. Pharm. 2015, 12, 2869–2878. [Google Scholar] [CrossRef] [PubMed]
- Peng, Y.; Liu, P.; Meng, Y.; Hu, S.; Ding, J.; Zhou, W. Nanoscale Copper(II)–Diethyldithiocarbamate Coordination Polymer as a Drug Self-Delivery System for Highly Robust and Specific Cancer Therapy. Mol. Pharm. 2020, 17, 2864–2873. [Google Scholar] [CrossRef]
- Wheate, N.J.; Walker, S.; Craig, G.E.; Oun, R. The status of platinum anticancer drugs in the clinic and in clinical trials. Dalton Trans. 2010, 39, 8113–8127. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Uivarosi, V.; Olar, R.; Badea, M. Nanoformulation as a Tool for Improve the Pharmacological Profile of Platinum and Ruthenium Anticancer Drugs. In Descriptive Inorganic Chemistry Researches of Metal Compounds; InTech: London, UK, 2017. [Google Scholar] [CrossRef] [Green Version]
- Xiao, H.; Song, H.; Zhang, Y.; Qi, R.; Wang, R.; Xie, Z.; Huang, Y.; Li, Y.; Wu, Y.; Jing, X. The use of polymeric platinum(IV) prodrugs to deliver multinuclear platinum(II) drugs with reduced systemic toxicity and enhanced antitumor efficacy. Biomaterials 2012, 33, 8657–8669. [Google Scholar] [CrossRef] [PubMed]
- Jia, C.; Deacon, G.B.; Zhang, Y.; Gao, C. Platinum(IV) antitumor complexes and their nano-drug delivery. Co-ord. Chem. Rev. 2020, 429, 213640. [Google Scholar] [CrossRef]
- Blunden, B.M.; Rawal, A.; Lu, H.; Stenzel, M.H. Superior Chemotherapeutic Benefits from the Ruthenium-Based Anti-Metastatic Drug NAMI-A through Conjugation to Polymeric Micelles. Macromolecules 2014, 47, 1646–1655. [Google Scholar] [CrossRef]
- Rico, S.R.A.; Abbasi, A.Z.; Ribeiro, G.; Ahmed, T.; Wu, X.Y.; Silva, D.D.O. Diruthenium(ii,iii) metallodrugs of ibuprofen and naproxen encapsulated in intravenously injectable polymer–lipid nanoparticles exhibit enhanced activity against breast and prostate cancer cells. Nanoscale 2017, 9, 10701–10714. [Google Scholar] [CrossRef]
- Appold, M.; Mari, C.; Lederle, C.; Elbert, J.; Schmidt, C.; Ott, I.; Stühn, B.; Gasser, G.; Gallei, M. Multi-stimuli responsive block copolymers as a smart release platform for a polypyridyl ruthenium complex. Polym. Chem. 2016, 8, 890–900. [Google Scholar] [CrossRef] [Green Version]
- Karges, J.; Li, J.; Zeng, L.; Chao, H.; Gasser, G. Polymeric Encapsulation of a Ruthenium Polypyridine Complex for Tumor Targeted One- and Two-Photon Photodynamic Therapy. ACS Appl. Mater. Interfaces 2020, 12, 54433–54444. [Google Scholar] [CrossRef]
- Chen, B.; Sleiman, H.F. Ruthenium Bipyridine-Containing Polymers and Block Copolymers via Ring-Opening Metathesis Polymerization. Macromolecules 2004, 37, 5866–5872. [Google Scholar] [CrossRef]
- Chen, B.; Metera, K.; Sleiman, H.F. Biotin-Terminated Ruthenium Bipyridine Ring-Opening Metathesis Polymerization Copolymers: Synthesis and Self-Assembly with Streptavidin. Macromolecules 2005, 38, 1084–1090. [Google Scholar] [CrossRef]
- Sun, W.; Li, S.; Häupler, B.; Liu, J.; Jin, S.; Steffen, W.; Schubert, U.S.; Butt, H.-J.; Liang, X.-J.; Wu, S. An Amphiphilic Ruthenium Polymetallodrug for Combined Photodynamic Therapy and Photochemotherapy In Vivo. Adv. Mater. 2017, 29, 1603702. [Google Scholar] [CrossRef]
- Chen, M.; Sun, W.; Kretzschmann, A.; Butt, H.-J.; Wu, S. Nanostructured polymer assemblies stabilize photoactivatable anticancer ruthenium complexes under physiological conditions. J. Inorg. Biochem. 2020, 207, 111052. [Google Scholar] [CrossRef] [PubMed]
- Bauer, T.A.; Eckrich, J.; Wiesmann, N.; Kuczelinis, F.; Sun, W.; Zeng, X.; Weber, B.; Wu, S.; Bings, N.H.; Strieth, S.; et al. Photocleavable core cross-linked polymeric micelles of polypept(o)ides and ruthenium(ii) complexes. J. Mater. Chem. B 2021, 9, 8211–8223. [Google Scholar] [CrossRef]
- Romero-Canelon, I.; Phoenix, B.; Pitto-Barry, A.; Tran, J.; Barreda, J.S.; Kirby, N.; Green, S.; Sadler, P.J.; Barry, N.P. Arene ruthenium dithiolato–carborane complexes for boron neutron capture therapy (BNCT). J. Organomet. Chem. 2015, 796, 17–25. [Google Scholar] [CrossRef] [Green Version]
- Kołoczek, P.; Skórska-Stania, A.; Cierniak, A.; Sebastian, V.; Komarnicka, U.K.; Płotek, M.; Kyzioł, A. Polymeric micelle-mediated delivery of half-sandwich ruthenium(II) complexes with phosphanes derived from fluoroloquinolones for lung adenocarcinoma treatment. Eur. J. Pharm. Biopharm. 2018, 128, 69–81. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ringhieri, P.; Iannitti, R.; Nardon, C.; Palumbo, R.; Fregona, D.; Morelli, G.; Accardo, A. Target selective micelles for bombesin receptors incorporating Au(III)-dithiocarbamato complexes. Int. J. Pharm. 2014, 473, 194–202. [Google Scholar] [CrossRef] [PubMed]
- Nardon, C.; Boscutti, G.; Via, L.D.; Ringhieri, P.; Di Noto, V.; Morelli, G.; Accardo, A.; Fregona, D. CCK8 peptide-labeled Pluronic® F127 micelles as a targeted vehicle of gold-based anticancer chemotherapeutics. MedChemComm 2014, 6, 155–163. [Google Scholar] [CrossRef]
- Pearson, S.; Scarano, W.; Stenzel, M.H. Micelles based on gold-glycopolymer complexes as new chemotherapy drug delivery agents. Chem. Commun. 2012, 48, 4695–4697. [Google Scholar] [CrossRef]
- Ahmed, M.; Mamba, S.; Yang, X.-H.; Darkwa, J.; Kumar, P.; Narain, R. Synthesis and Evaluation of Polymeric Gold Glyco-Conjugates as Anti-Cancer Agents. Bioconjugate Chem. 2013, 24, 979–986. [Google Scholar] [CrossRef]
- Pramanik, A.; Laha, D.; Pramanik, P.; Karmakar, P. A novel drug “copper acetylacetonate” loaded in folic acid-tagged chitosan nanoparticle for efficient cancer cell targeting. J. Drug Target. 2013, 22, 23–33. [Google Scholar] [CrossRef]
- Sibata, M.; Tedesco, A.; Marchetti, J. Photophysicals and photochemicals studies of zinc(II) phthalocyanine in long time circulation micelles for Photodynamic Therapy use. Eur. J. Pharm. Sci. 2004, 23, 131–138. [Google Scholar] [CrossRef]
- Lamch, Ł.; Kulbacka, J.; Pietkiewicz, J.; Rossowska, J.; Dubińska-Magiera, M.; Choromańska, A.; Wilk, K.A. Preparation and characterization of new zinc(II) phthalocyanine—Containing poly(l-lactide)-b-poly(ethylene glycol) copolymer micelles for photodynamic therapy. J. Photochem. Photobiol. B Biol. 2016, 160, 185–197. [Google Scholar] [CrossRef] [PubMed]
- Lamch, Ł.; Kulbacka, J.; Dubińska-Magiera, M.; Saczko, J.; Wilk, K.A. Folate-directed zinc (II) phthalocyanine loaded polymeric micelles engineered to generate reactive oxygen species for efficacious photodynamic therapy of cancer. Photodiagnosis Photodyn. Ther. 2019, 25, 480–491. [Google Scholar] [CrossRef] [PubMed]
- Debele, T.A.; Mekuria, S.L.; Lin, S.-Y.; Tsai, H.-C. Synthesis and characterization of bioreducible heparin-polyethyleneimine nanogels: Application as imaging-guided photosensitizer delivery vehicle in photodynamic therapy. RSC Adv. 2016, 6, 14692–14704. [Google Scholar] [CrossRef]
- Obata, M.; Masuda, S.; Takahashi, M.; Yazaki, K.; Hirohara, S. Effect of the hydrophobic segment of an amphiphilic block copolymer on micelle formation, zinc phthalocyanine loading, and photodynamic activity. Eur. Polym. J. 2021, 147, 110325. [Google Scholar] [CrossRef]
- Fu, J.; Li, X.-Y.; Ng, D.K.P.; Wu, C. Encapsulation of Phthalocyanines in Biodegradable Poly(sebacic anhydride) Nanoparticles. Langmuir 2002, 18, 3843–3847. [Google Scholar] [CrossRef]
- Zhang, X.; Li, Q.; Sun, X.; Zhang, B.; Kang, H.; Zhang, F.; Jin, Y. Doxorubicin-Loaded Photosensitizer-Core pH-Responsive Copolymer Nanocarriers for Combining Photodynamic Therapy and Chemotherapy. ACS Biomater. Sci. Eng. 2017, 3, 1008–1016. [Google Scholar] [CrossRef]
- Vior, M.C.G.; Marino, J.; Roguin, L.P.; Sosnik, A.; Awruch, J. Photodynamic Effects of Zinc(II) Phthalocyanine-Loaded Polymeric Micelles in Human Nasopharynx KB Carcinoma Cells. Photochem. Photobiol. 2012, 89, 492–500. [Google Scholar] [CrossRef]
- Fang, J.; Sawa, T.; Akaike, T.; Greish, K.; Maeda, H. Enhancement of chemotherapeutic response of tumor cells by a heme oxygenase inhibitor, pegylated zinc protoporphyrin. Int. J. Cancer 2003, 109, 1–8. [Google Scholar] [CrossRef]
- Sahoo, S.K.; Sawa, T.; Fang, J.; Tanaka, S.; Miyamoto, Y.; Akaike, T.; Maeda, H. Pegylated Zinc Protoporphyrin: A Water-Soluble Heme Oxygenase Inhibitor with Tumor-Targeting Capacity. Bioconjugate Chem. 2002, 13, 1031–1038. [Google Scholar] [CrossRef]
- Iyer, A.K.; Greish, K.; Fang, J.; Murakami, R.; Maeda, H. High-loading nanosized micelles of copoly(styrene–maleic acid)–zinc protoporphyrin for targeted delivery of a potent heme oxygenase inhibitor. Biomaterials 2007, 28, 1871–1881. [Google Scholar] [CrossRef]
- Fang, J.; Tsukigawa, K.; Liao, L.; Yin, H.; Eguchi, K.; Maeda, H. Styrene-maleic acid-copolymer conjugated zinc protoporphyrin as a candidate drug for tumor-targeted therapy and imaging. J. Drug Target. 2015, 24, 399–407. [Google Scholar] [CrossRef] [PubMed]
- Nakamura, H.; Liao, L.; Hitaka, Y.; Tsukigawa, K.; Subr, V.; Fang, J.; Ulbrich, K.; Maeda, H. Micelles of zinc protoporphyrin conjugated to N-(2-hydroxypropyl)methacrylamide (HPMA) copolymer for imaging and light-induced antitumor effects in vivo. J. Control. Release 2012, 165, 191–198. [Google Scholar] [CrossRef] [PubMed]
- Tsukigawa, K.; Nakamura, H.; Fang, J.; Otagiri, M.; Maeda, H. Effect of different chemical bonds in pegylation of zinc protoporphyrin that affects drug release, intracellular uptake, and therapeutic effect in the tumor. Eur. J. Pharm. Biopharm. 2014, 89, 259–270. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wenceslau, A.C.; Ferreira, G.L.Q.C.; Hioka, N.; Caetano, W. Spectroscopic studies of pyridil and methoxyphenyl porphyrins in homogeneous and Pluronic®-based nanostructured systems. J. Porphyr. Phthalocyanines 2015, 19, 1168–1176. [Google Scholar] [CrossRef]
- Karges, J.; Blacque, O.; Chao, H.; Gasser, G. Polymeric Bis(dipyrrinato) Zinc(II) Nanoparticles as Selective Imaging Probes for Lysosomes of Cancer Cells. Inorg. Chem. 2019, 58, 12422–12432. [Google Scholar] [CrossRef] [PubMed]
- Karges, J.; Basu, U.; Blacque, O.; Chao, H.; Gasser, G. Polymeric Encapsulation of Novel Homoleptic Bis(dipyrrinato) Zinc(II) Complexes with Long Lifetimes for Applications as Photodynamic Therapy Photosensitisers. Angew. Chem. Int. Ed. 2019, 58, 14334–14340. [Google Scholar] [CrossRef]
- Guo, B.; Feng, G.; Manghnani, P.; Cai, X.; Liu, J.; Wu, W.; Xu, S.; Cheng, X.; Teh, C.; Liu, B. A Porphyrin-Based Conjugated Polymer for Highly Efficient In Vitro and In Vivo Photothermal Therapy. Small 2016, 12, 6243–6254. [Google Scholar] [CrossRef]
- Zhang, J.; Yang, C.; Zhang, R.; Chen, R.; Zhang, Z.; Zhang, W.; Peng, S.-H.; Chen, X.; Liu, G.; Hsu, C.-S.; et al. Biocompatible D-A Semiconducting Polymer Nanoparticle with Light-Harvesting Unit for Highly Effective Photoacoustic Imaging Guided Photothermal Therapy. Adv. Funct. Mater. 2017, 27, 1605094. [Google Scholar] [CrossRef]
- Jin, Y.; Zhang, X.; Zhang, B.; Kang, H.; Du, L.; Li, M. Nanostructures of an amphiphilic zinc phthalocyanine polymer conjugate for photodynamic therapy of psoriasis. Colloids Surf. B Biointerfaces 2015, 128, 405–409. [Google Scholar] [CrossRef]
- Tong, W.; Xiong, Y.; Duan, S.; Ding, X.; Xu, F.-J. Phthalocyanine functionalized poly(glycidyl methacrylate) nano-assemblies for photodynamic inactivation of bacteria. Biomater. Sci. 2019, 7, 1905–1918. [Google Scholar] [CrossRef]
- Fan, Y.; Li, C.; Cao, H.; Li, F.; Chen, D. The intranuclear release of a potential anticancer drug from small nanoparticles that are derived from intracellular dissociation of large nanoparticles. Biomaterials 2012, 33, 4220–4228. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.; Wu, Y.; Li, F.; Chen, D. Folic acid-modified iridium(III) coordination polymeric nanoparticles facilitating intracellular release of a phosphorescent residue capable of nuclear entry. Inorg. Chem. Commun. 2014, 40, 143–147. [Google Scholar] [CrossRef]
- Fan, Y.; Li, C.; Li, F.; Chen, D. pH-activated size reduction of large compound nanoparticles for in vivo nucleus-targeted drug delivery. Biomaterials 2016, 85, 30–39. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lv, W.; Xia, H.; Zhang, K.Y.; Chen, Z.; Liu, S.; Huang, W.; Zhao, Q. Photothermal-triggered release of singlet oxygen from an endoperoxide-containing polymeric carrier for killing cancer cells. Mater. Horizons 2017, 4, 1185–1189. [Google Scholar] [CrossRef]
- Sun, P.; Wang, G.; Hou, H.; Yuan, P.; Deng, W.; Wang, C.; Lu, X.; Fan, Q.; Huang, W. A water-soluble phosphorescent conjugated polymer brush for tumor-targeted photodynamic therapy. Polym. Chem. 2017, 8, 5836–5844. [Google Scholar] [CrossRef]
- Tsakaraki, D.; Andreopoulou, A.K.; Bokias, G. pH-Responsive Emission of Novel Water-Soluble Polymeric Iridium(III) Complexes. Nanomaterials 2022, 12, 927. [Google Scholar] [CrossRef] [PubMed]
- Wang, J.; Liu, L.; Yin, L.; Chen, L. Acid-triggered synergistic chemo-photodynamic therapy systems based on metal-coordinated supramolecular interaction. J. Biomed. Mater. Res. Part A 2018, 106, 2955–2962. [Google Scholar] [CrossRef]
- Elsey, J.; Bubley, J.A.; Zhu, L.; Rao, S.; Sasaki, M.; Pollack, B.P.; Yang, L.; Arbiser, J.L. Palladium based nanoparticles for the treatment of advanced melanoma. Sci. Rep. 2019, 9, 3255. [Google Scholar] [CrossRef]
- Talebi, S.; Amani, V.; Saber-Tehrani, M.; Abedi, A. Improvement of the Biological Activity of a New Cobalt(III) Complex through Loading into a Nanocarrier, and the Characterization Thereof. ChemistrySelect 2019, 4, 13235–13240. [Google Scholar] [CrossRef]
- Eskandari, A.; Suntharalingam, K. A reactive oxygen species-generating, cancer stem cell-potent manganese(ii) complex and its encapsulation into polymeric nanoparticles. Chem. Sci. 2019, 10, 7792–7800. [Google Scholar] [CrossRef]
- Youngs, W.J.; Knapp, A.R.; Wagers, P.O.; Tessier, C.A. Nanoparticle encapsulated silvercarbene complexes and their antimicrobial and anticancer properties: A perspective. Dalton Trans. 2011, 41, 327–336. [Google Scholar] [CrossRef] [PubMed]
- Li, Y.; Hindi, K.; Watts, K.M.; Taylor, J.B.; Zhang, K.; Li, Z.; Hunstad, D.A.; Cannon, C.L.; Youngs, W.J.; Wooley, K.L. Shell crosslinked nanoparticles carrying silver antimicrobials as therapeutics. Chem. Commun. 2009, 46, 121–123. [Google Scholar] [CrossRef] [PubMed]
- Lim, Y.H.; Tiemann, K.M.; Heo, G.S.; Wagers, P.O.; Rezenom, Y.H.; Zhang, S.; Zhang, F.; Youngs, W.J.; Hunstad, D.A.; Wooley, K.L. Preparation and in Vitro Antimicrobial Activity of Silver-Bearing Degradable Polymeric Nanoparticles of Polyphosphoester-block-Poly(l-lactide). ACS Nano 2015, 9, 1995–2008. [Google Scholar] [CrossRef] [Green Version]
- de Camargo, B.A.F.; Silva, D.E.S.; da Silva, A.N.; Campos, D.L.; Ribeiro, T.R.M.; Mieli, M.J.; Zanatta, M.B.T.; da Silva, P.B.; Pavan, F.R.; Moreira, C.G.; et al. New Silver(I) Coordination Compound Loaded into Polymeric Nanoparticles as a Strategy to Improve In Vitro Anti-Helicobacter pylori Activity. Mol. Pharm. 2020, 17, 2287–2298. [Google Scholar] [CrossRef] [PubMed]
- Alves, E.; Iglesias, B.A.; Deda, D.K.; Budu, A.; Matias, T.A.; Bueno, V.B.; Maluf, F.V.; Guido, R.V.; Oliva, G.; Catalani, L.H.; et al. Encapsulation of metalloporphyrins improves their capacity to block the viability of the human malaria parasite Plasmodium falciparum. Nanomed. Nanotechnol. Biol. Med. 2014, 11, 351–358. [Google Scholar] [CrossRef]
- Li, F.; Collins, J.G.; Keene, F.R. Ruthenium complexes as antimicrobial agents. Chem. Soc. Rev. 2015, 44, 2529–2542. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Reedijk, B.J. Metal-Ligand Exchange Kinetics in Platinum and Ruthenium Complexes. Platin. Met. Rev. 2008, 52, 2–11. [Google Scholar] [CrossRef]
- Antonarakis, E.S.; Emadi, A. Ruthenium-based chemotherapeutics: Are they ready for prime time? Cancer Chemother. Pharmacol. 2010, 66, 1–9. [Google Scholar] [CrossRef] [Green Version]
- McFarland, S.A.; Mandel, A.; Dumoulin-White, R.; Gasser, G. Metal-based photosensitizers for photodynamic therapy: The future of multimodal oncology? Curr. Opin. Chem. Biol. 2019, 56, 23–27. [Google Scholar] [CrossRef] [PubMed]
- Monro, S.; Colón, K.L.; Yin, H.; Roque, J., III; Konda, P.; Gujar, S.; Thummel, R.P.; Lilge, L.; Cameron, C.G.; McFarland, S.A. Transition Metal Complexes and Photodynamic Therapy from a Tumor-Centered Approach: Challenges, Opportunities, and Highlights from the Development of TLD1433. Chem. Rev. 2019, 119, 797–828. [Google Scholar] [CrossRef]
- Alessio, E.; Messori, L. NAMI-A and KP1019/1339, Two Iconic Ruthenium Anticancer Drug Candidates Face-to-Face: A Case Story in Medicinal Inorganic Chemistry. Molecules 2019, 24, 1995. [Google Scholar] [CrossRef] [Green Version]
- Brabec, V.; Nováková, O. DNA binding mode of ruthenium complexes and relationship to tumor cell toxicity. Drug Resist. Updat. 2006, 9, 111–122. [Google Scholar] [CrossRef] [PubMed]
- Zeng, L.; Gupta, P.; Chen, Y.; Wang, E.; Ji, L.; Chao, H.; Chen, Z.-S. The development of anticancer ruthenium(ii) complexes: From single molecule compounds to nanomaterials. Chem. Soc. Rev. 2017, 46, 5771–5804. [Google Scholar] [CrossRef] [PubMed]
- Alessio, E. Thirty Years of the Drug Candidate NAMI-A and the Myths in the Field of Ruthenium Anticancer Compounds: A Personal Perspective. Eur. J. Inorg. Chem. 2016, 2017, 1549–1560. [Google Scholar] [CrossRef]
- Bytzek, A.K.; Koellensperger, G.; Keppler, B.K.; Hartinger, C.G. Biodistribution of the novel anticancer drug sodium trans -[tetrachloridobis(1 H -indazole)ruthenate(III)] KP-1339/IT139 in nude BALB/c mice and implications on its mode of action. J. Inorg. Biochem. 2016, 160, 250–255. [Google Scholar] [CrossRef] [PubMed]
- Clinicaltrials.gov, Intravesical Photodynamic Therapy (PDT) in BCG Refractory/Intolerant Non-Muscle Invasive Bladder Cancer (NMIBC) Patients. 2019. Available online: https://www.clinicaltrials.gov/ct2/show/NCT03945162?term=TLD1433&draw=2&rank=2 (accessed on 19 April 2022).
- Parveen, S. Recent advances in anticancer ruthenium Schiff base complexes. Appl. Organomet. Chem. 2020, 34. [Google Scholar] [CrossRef]
- Sonkar, C.; Sarkar, S.; Mukhopadhyay, S. Ruthenium(ii)–arene complexes as anti-metastatic agents, and related techniques. RSC Med. Chem. 2021, 13, 22–38. [Google Scholar] [CrossRef]
- Thangavel, P.; Viswanath, B.; Kim, S. Recent developments in the nanostructured materials functionalized with ruthenium complexes for targeted drug delivery to tumors. Int. J. Nanomed. 2017, 12, 2749–2758. [Google Scholar] [CrossRef] [Green Version]
- Soliman, N.; Gasser, G.; Thomas, C.M. Incorporation of Ru(II) Polypyridyl Complexes into Nanomaterials for Cancer Therapy and Diagnosis. Adv. Mater. 2020, 32, e2003294. [Google Scholar] [CrossRef]
- Blunden, B.M.; Stenzel, M.H. Incorporating ruthenium into advanced drug delivery carriers - an innovative generation of chemotherapeutics. J. Chem. Technol. Biotechnol. 2014, 90, 1177–1195. [Google Scholar] [CrossRef]
- Riccardi, C.; Musumeci, D.; Trifuoggi, M.; Irace, C.; Paduano, L.; Montesarchio, D. Anticancer Ruthenium(III) Complexes and Ru(III)-Containing Nanoformulations: An Update on the Mechanism of Action and Biological Activity. Pharmaceuticals 2019, 12, 146. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zhou, H.; Chen, M.; Liu, Y.; Wu, S. Stimuli-Responsive Ruthenium-Containing Polymers. Macromol. Rapid Commun. 2018, 39, e1800372. [Google Scholar] [CrossRef]
- Sun, W.; Zeng, X.; Wu, S. Photoresponsive ruthenium-containing polymers: Potential polymeric metallodrugs for anticancer phototherapy. Dalton Trans. 2017, 47, 283–286. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Soliman, N.; McKenzie, L.K.; Karges, J.; Bertrand, E.; Tharaud, M.; Jakubaszek, M.; Guérineau, V.; Goud, B.; Hollenstein, M.; Gasser, G.; et al. Ruthenium-initiated polymerization of lactide: A route to remarkable cellular uptake for photodynamic therapy of cancer. Chem. Sci. 2020, 11, 2657–2663. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Barry, N.P.E.; Pitto-Barry, A.; Romero-Canelón, I.; Tran, J.; Soldevila-Barreda, J.J.; Hands-Portman, I.; Smith, C.J.; Kirby, N.; Dove, A.P.; O’Reilly, R.K.; et al. Precious metal carborane polymer nanoparticles: Characterisation of micellar formulations and anticancer activity. Faraday Discuss. 2014, 175, 229–240. [Google Scholar] [CrossRef] [Green Version]
- Ballinger, J.R. Theranostic radiopharmaceuticals: Established agents in current use. Br. J. Radiol. 2018, 91, 20170969. [Google Scholar] [CrossRef]
- Timerbaev, A.R. Advances in developing tris(8-quinolinolato)gallium(iii) as an anticancer drug: Critical appraisal and prospects. Metallomics 2009, 1, 193–198. [Google Scholar] [CrossRef] [PubMed]
- Clinicaltrials.gov, Oral Gallium Maltolate for the Treatment of Relapsed and Refractory Glioblastoma. 2022. Available online: https://clinicaltrials.gov/ct2/show/NCT04319276?term=gallium+maltolate&draw=2&rank=1 (accessed on 19 April 2022).
- Chitambar, C.R. 10. Gallium Complexes as anticancer drugs. In Metallo-Drugs: Development and Action of Anticancer Agents; De Gruyter: Berlin, Germany, 2018; Volume 18, pp. 281–302. [Google Scholar] [CrossRef]
- Chitambar, C.R. Gallium and its competing roles with iron in biological systems. Biochim. Biophys. Acta 2016, 1863, 2044–2053. [Google Scholar] [CrossRef]
- Tiekink, E.R.T. Anti-cancer potential of gold complexes. Inflammopharmacology 2008, 16, 138–142. [Google Scholar] [CrossRef] [PubMed]
- Urig, S.; Fritz-Wolf, K.; Réau, R.; Herold-Mende, C.; T´oth, K.; Davioud-Charvet, E.; Becker, K. Undressing of Phosphine Gold(I) Complexes as Irreversible Inhibitors of Human Disulfide Reductases. Angew. Chem. Int. Ed. 2006, 45, 1881–1886. [Google Scholar] [CrossRef]
- Tiekink, E.R. Gold derivatives for the treatment of cancer. Crit. Rev. Oncol. 2002, 42, 225–248. [Google Scholar] [CrossRef]
- Maret, W.; Wedd, A. (Eds.) Binding, Transport and Storage of Metal Ions in Biological Cells; Royal Society of Chemistry: Cambridge, UK, 2014. [Google Scholar] [CrossRef] [Green Version]
- Santini, C.; Pellei, M.; Gandin, V.; Porchia, M.; Tisato, F.; Marzano, C. Advances in Copper Complexes as Anticancer Agents. Chem. Rev. 2013, 114, 815–862. [Google Scholar] [CrossRef]
- McGivern, T.; Afsharpour, S.; Marmion, C. Copper complexes as artificial DNA metallonucleases: From Sigman’s reagent to next generation anti-cancer agent? Inorganica Chim. Acta 2018, 472, 12–39. [Google Scholar] [CrossRef]
- Molinaro, C.; Martoriati, A.; Pelinski, L.; Cailliau, K. Copper Complexes as Anticancer Agents Targeting Topoisomerases I and II. Cancers 2020, 12, 2863. [Google Scholar] [CrossRef]
- Lü, W.; Sun, C.; Lu, Q.; Li, N.; Wu, D.; Yao, Y.; Chen, W. Synthesis and photoactivity of pH-responsive amphiphilic block polymer photosensitizer bonded zinc phthalocyanine. Sci. China Ser. B Chem. 2012, 55, 1108–1114. [Google Scholar] [CrossRef]
- Balendiran, G.K.; Dabur, R.; Fraser, D. The role of glutathione in cancer. Cell Biochem. Funct. 2004, 22, 343–352. [Google Scholar] [CrossRef]
- Parkin, G. The bioinorganic chemistry of zinc: Synthetic analogues of zinc enzymes that feature tripodal ligands. Chem. Commun. 2000, 1971–1985. [Google Scholar] [CrossRef]
- Roguin, L.P.; Chiarante, N.; García Vior, M.C.; Marino, J. Zinc(II) phthalocyanines as photosensitizers for antitumor photodynamic therapy. Int. J. Biochem. Cell Biol. 2019, 114, 105575. [Google Scholar] [CrossRef]
- Fang, J.; Sawa, T.; Akaike, T.; Akuta, T.; Sahoo, S.K.; Khaled, G.; Hamada, A.; Maeda, H. In vivo antitumor activity of pegylated zinc protoporphyrin: Targeted inhibition of heme oxygenase in solid tumor. Cancer Res. 2003, 63. [Google Scholar]
- Iyer, A.K.; Iyer, A.K.; Greish, K.; Greish, K.; Seki, T.; Seki, T.; Okazaki, S.; Okazaki, S.; Fang, J.; Fang, J.; et al. Polymeric micelles of zinc protoporphyrin for tumor targeted delivery based on EPR effect and singlet oxygen generation. J. Drug Target. 2007, 15, 496–506. [Google Scholar] [CrossRef] [PubMed]
- Nakamura, H.; Fang, J.; Gahininath, B.; Tsukigawa, K.; Maeda, H. Intracellular uptake and behavior of two types zinc protoporphyrin (ZnPP) micelles, SMA-ZnPP and PEG-ZnPP as anticancer agents; unique intracellular disintegration of SMA micelles. J. Control. Release 2011, 155, 367–375. [Google Scholar] [CrossRef] [PubMed]
- Fang, J.; Liao, L.; Yin, H.; Nakamura, H.; Subr, V.; Ulbrich, K.; Maeda, H. Photodynamic therapy and imaging based on tumor-targeted nanoprobe, polymer-conjugated zinc protoporphyrin. Futur. Sci. OA 2015, 1, FSO4. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rouhani, H.; Sepehri, N.; Montazeri, H.; Khoshayand, M.R.; Ghahremani, M.H.; Ostad, S.N.; Atyabi, F.; Dinarvand, R. Zinc Protoporphyrin Polymeric Nanoparticles: Potent Heme Oxygenase Inhibitor for Cancer Therapy. Pharm. Res. 2014, 31, 2124–2139. [Google Scholar] [CrossRef]
- Chen, F.; Cai, W. Nanomedicine for targeted photothermal cancer therapy: Where are we now? Nanomedicine 2015, 10, 1–3. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ma, D.-L.; Wu, C.; Wu, K.-J.; Leung, C.-H. Iridium(III) Complexes Targeting Apoptotic Cell Death in Cancer Cells. Molecules 2019, 24, 2739. [Google Scholar] [CrossRef] [Green Version]
- Liu, G.; Men, P.; Harris, P.L.; Rolston, R.K.; Perry, G.; Smith, M.A. Nanoparticle iron chelators: A new therapeutic approach in Alzheimer disease and other neurologic disorders associated with trace metal imbalance. Neurosci. Lett. 2006, 406, 189–193. [Google Scholar] [CrossRef]
- Bonda, D.J.; Liu, G.; Men, P.; Perry, G.; Smith, M.A.; Zhu, X. Nanoparticle delivery of transition-metal chelators to the brain: Oxidative stress will never see it coming! CNS Neurol. Disord.-Drug Targets 2012, 11, 81–85. [Google Scholar] [CrossRef]
- Wu, S.; Helal-Neto, E.; Matos, A.P.D.S.; Jafari, A.; Kozempel, J.; Silva, Y.J.D.A.; Serrano-Larrea, C.; Junior, S.A.; Ricci-Junior, E.; Alexis, F.; et al. Radioactive polymeric nanoparticles for biomedical application. Drug Deliv. 2020, 27, 1544–1561. [Google Scholar] [CrossRef]
- Hwang, H.; Kwon, J.; Oh, P.-S.; Lee, T.-K.; Na, K.-S.; Lee, C.-M.; Jeong, H.-J.; Lim, S.T.; Sohn, M.-H. Peptide-loaded Nanoparticles and Radionuclide Imaging for Individualized Treatment of Myocardial Ischemia. Radiology 2014, 273, 160–167. [Google Scholar] [CrossRef] [Green Version]
- Trujillo-Nolasco, R.M.; Morales-Avila, E.; Ocampo-García, B.E.; Ferro-Flores, G.; Gibbens-Bandala, B.V.; Escudero-Castellanos, A.; Isaac-Olive, K. Preparation and in vitro evaluation of radiolabeled HA-PLGA nanoparticles as novel MTX delivery system for local treatment of rheumatoid arthritis. Mater. Sci. Eng. C 2019, 103, 109766. [Google Scholar] [CrossRef]
- Xing, L.; Zheng, H.; Che, S. A pH-Responsive Cleavage Route Based on a Metal–Organic Coordination Bond. Chem.–A Eur. J. 2011, 17, 7271–7275. [Google Scholar] [CrossRef] [PubMed]
- Novio, F.; Simmchen, J.; Vázquez-Mera, N.; Amorín-Ferré, L.; Ruiz-Molina, D. Coordination polymer nanoparticles in medicine. Co-ord. Chem. Rev. 2013, 257, 2839–2847. [Google Scholar] [CrossRef] [Green Version]
- Tao, B.; Yin, Z. Redox-Responsive Coordination Polymers of Dopamine-Modified Hyaluronic Acid with Copper and 6-Mercaptopurine for Targeted Drug Delivery and Improvement of Anticancer Activity against Cancer Cells. Polymers 2020, 12, 1132. [Google Scholar] [CrossRef]
- Tang, Z.; Liu, Y.; He, M.; Bu, W. Chemodynamic Therapy: Tumour Microenvironment-Mediated Fenton and Fenton-like Reactions. Angew. Chem. Int. Ed. 2019, 58, 946–956. [Google Scholar] [CrossRef] [PubMed]
- Liu, X.; Jin, Y.; Liu, T.; Yang, S.; Zhou, M.; Wang, W.; Yu, H. Iron-Based Theranostic Nanoplatform for Improving Chemodynamic Therapy of Cancer. ACS Biomater. Sci. Eng. 2020, 6, 4834–4845. [Google Scholar] [CrossRef]
- Ruan, L.; Wang, M.; Zhou, M.; Lu, H.; Zhang, J.; Gao, J.; Chen, J.; Hu, Y. Doxorubicin–Metal Coordinated Micellar Nanoparticles for Intracellular Codelivery and Chemo/Chemodynamic Therapy in Vitro. ACS Appl. Bio Mater. 2019, 2, 4703–4707. [Google Scholar] [CrossRef]
- Lin, L.; Wang, S.; Deng, H.; Yang, W.; Rao, L.; Tian, R.; Liu, Y.; Yu, G.; Zhou, Z.; Song, J.; et al. Endogenous Labile Iron Pool-Mediated Free Radical Generation for Cancer Chemodynamic Therapy. J. Am. Chem. Soc. 2020, 142, 15320–15330. [Google Scholar] [CrossRef]
- Wang, S.; Yu, G.; Wang, Z.; Jacobson, O.; Lin, L.; Yang, W.; Deng, H.; He, Z.; Liu, Y.; Chen, Z.; et al. Enhanced Antitumor Efficacy by a Cascade of Reactive Oxygen Species Generation and Drug Release. Angew. Chem. Int. Ed. 2019, 58, 14758–14763. [Google Scholar] [CrossRef]
- Li, J.; Li, J.; Pu, Y.; Li, S.; Gao, W.; He, B. PDT-Enhanced Ferroptosis by a Polymer Nanoparticle with pH-Activated Singlet Oxygen Generation and Superb Biocompatibility for Cancer Therapy. Biomacromolecules 2021, 22, 1167–1176. [Google Scholar] [CrossRef]
- Sun, T.; Zhang, G.; Guo, Z.; Chen, Q.; Zhang, Y.; Chu, Y.; Guo, Q.; Li, C.; Zhou, W.; Zhang, Y.; et al. Co-delivery of Cu(I) chelator and chemotherapeutics as a new strategy for tumor theranostic. J. Control. Release 2020, 321, 483–496. [Google Scholar] [CrossRef]
- Guo, L.; Ge, J.; Wang, P. Polymer Dots as Effective Phototheranostic Agents. Photochem. Photobiol. 2018, 94, 916–934. [Google Scholar] [CrossRef] [PubMed]
- Zhu, C.; Liu, L.; Yang, Q.; Lv, F.; Wang, S. Water-Soluble Conjugated Polymers for Imaging, Diagnosis, and Therapy. Chem. Rev. 2012, 112, 4687–4735. [Google Scholar] [CrossRef]
- Ruggiero, E.; Alonso-de Castro, S.; Habtemariam, A.; Salassa, L. Upconverting nanoparticles for the near infrared photoactivation of transition metal complexes: New opportunities and challenges in medicinal inorganic photochemistry. Dalton Trans. 2016, 45, 13012–13020. [Google Scholar] [CrossRef] [Green Version]
- Feng, Z.; Tao, P.; Zou, L.; Gao, P.; Liu, Y.; Liu, X.; Wang, H.; Liu, S.; Dong, Q.; Li, J.; et al. Hyperbranched Phosphorescent Conjugated Polymer Dots with Iridium(III) Complex as the Core for Hypoxia Imaging and Photodynamic Therapy. ACS Appl. Mater. Interfaces 2017, 9, 28319–28330. [Google Scholar] [CrossRef] [PubMed]
- Shi, H.; Ma, X.; Zhao, Q.; Liu, B.; Qu, Q.; An, Z.; Zhao, Y.; Huang, W. Ultrasmall Phosphorescent Polymer Dots for Ratiometric Oxygen Sensing and Photodynamic Cancer Therapy. Adv. Funct. Mater. 2014, 24, 4823–4830. [Google Scholar] [CrossRef]
- Jiang, J.; Qian, Y.; Xu, Z.; Lv, Z.; Tao, P.; Xie, M.; Liu, S.; Huang, W.; Zhao, Q. Enhancing singlet oxygen generation in semiconducting polymer nanoparticles through fluorescence resonance energy transfer for tumor treatment. Chem. Sci. 2019, 10, 5085–5094. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fang, X.; Ju, B.; Liu, Z.; Wang, F.; Xi, G.; Sun, Z.; Chen, H.; Sui, C.; Wang, M.; Wu, C. Compact Conjugated Polymer Dots with Covalently Incorporated Metalloporphyrins for Hypoxia Bioimaging. ChemBioChem 2018, 20, 521–525. [Google Scholar] [CrossRef]
- Zhou, X.; Liang, H.; Jiang, P.; Zhang, K.Y.; Liu, S.; Yang, T.; Zhao, Q.; Yang, L.; Lv, W.; Yu, Q.; et al. Multifunctional Phosphorescent Conjugated Polymer Dots for Hypoxia Imaging and Photodynamic Therapy of Cancer Cells. Adv. Sci. 2016, 3, 1500155. [Google Scholar] [CrossRef] [Green Version]
- Chen, Y.; Jiang, G.; Zhou, Q.; Zhang, Y.; Li, K.; Zheng, Y.; Zhang, B.; Wang, X. An upconversion nanoparticle/Ru(ii) polypyridyl complex assembly for NIR-activated release of a DNA covalent-binding agent. RSC Adv. 2016, 6, 23804–23808. [Google Scholar] [CrossRef]
- Bagheri, A.; Arandiyan, H.; Boyer, C.; Lim, M. Lanthanide-Doped Upconversion Nanoparticles: Emerging Intelligent Light-Activated Drug Delivery Systems. Adv. Sci. 2016, 3, 1500437. [Google Scholar] [CrossRef] [Green Version]
- Zhao, J.; Zhang, X.; Fang, L.; Gao, C.; Xu, C.; Gou, S. Iridium(III) Complex–Derived Polymeric Micelles with Low Dark Toxicity and Strong NIR Excitation for Phototherapy and Chemotherapy. Small 2020, 16, e2000363. [Google Scholar] [CrossRef] [PubMed]
- Xia, L.; Kong, X.; Liu, X.; Tu, L.; Zhang, Y.; Chang, Y.; Liu, K.; Shen, D.; Zhao, H.; Zhang, H. An upconversion nanoparticle – Zinc phthalocyanine based nanophotosensitizer for photodynamic therapy. Biomaterials 2014, 35, 4146–4156. [Google Scholar] [CrossRef] [PubMed]
- Dai, Y.; Xiao, H.; Liu, J.; Yuan, Q.; Ma, P.; Yang, D.; Li, C.; Cheng, Z.; Hou, Z.; Yang, P.; et al. In Vivo Multimodality Imaging and Cancer Therapy by Near-Infrared Light-Triggered trans-Platinum Pro-Drug-Conjugated Upconverison Nanoparticles. J. Am. Chem. Soc. 2013, 135, 18920–18929. [Google Scholar] [CrossRef] [PubMed]
- Ruggiero, E.; Hernández-Gil, J.; Mareque-Rivas, J.C.; Salassa, L. Near infrared activation of an anticancer PtIV complex by Tm-doped upconversion nanoparticles. Chem. Commun. 2014, 51, 2091–2094. [Google Scholar] [CrossRef] [PubMed]
- Pierri, A.E.; Huang, P.-J.; Garcia, J.V.; Stanfill, J.G.; Chui, M.; Wu, G.; Zheng, N.; Ford, P.C. A photoCORM nanocarrier for CO release using NIR light. Chem. Commun. 2014, 51, 2072–2075. [Google Scholar] [CrossRef] [Green Version]








| Structures of Metal-Based Drug/ Metallopolymer Prodrug * | Metallic Center | Polymer/Copolymer Blocks | Method of Incorporation | Type of Nanocarrier | Average Diameter Size (nm) | Responsive Delivery/ Specific Targeting Moieties/Co-Delivery | Potential Therapeutic Approaches | Ref. |
|---|---|---|---|---|---|---|---|---|
 (KP1019)—Ru1 | Ru3+ | PLA | Physical encap. | Micelles | 163 | - | CTX | [57] |
| PEG | Physical encap. | Micelles | <100 | - | CTX | [50] | ||
 (NAMI-A prodrug)—Ru2 | Ru2+ | PEG-methyl ether acrylate | Covalent conjug. | Micelles | 90 | - | CTX | [108] |
 Ru3 | Ru3+ | PF127 | Physical encap. | Micelles | 24 | PF127 was functionalized with carbohydrate (fluorescein, glucosamine, and β-D-glucopyranoside) for target delivery. | CTX | [97] |
 Ru4–Ru8 | Ru3+ | PF127 | Physical encap. | Micelles | - | - | CTX | [72] |
 Ru9 and Ru10 | Ru3+/ Ru2+ | stearate-PEG40/100, ethyl arachidate, and myristic acid | Physical encap. | NPs | 120 | - | CTX | [109] |
| poly(methacrylic acid)-PS80-starch | Physical encap. | NPs | 130 | - | CTX | [83] | ||
 Ru11 and Ru12 | Ru2+ | PLGA | Physical encap. | Nanosphere | 100 | - | CTX | [61] |
 Ru13 | Ru2+ | PEI-mPEG5000/PLGA (PEI = polyethyleneimine) | Physical encap. | Nanosphere | 153 | Biotin was conjugated to polymer chain for target delivery | CTX | [87] |
 Ru14–Ru16 | Ru2+ | PEG- poly(aspartate) | Physical encap. | NPs | 19 | - | PDT | [51] |
 Ru17 | Ru2+ | poly(N,N-dimethylaminoethylmetha-cry-late-co-poly (methyl methacrylate) | Physical encap. | Micelles | 8 | - | PDT | [110] |
 Ru18 | Ru2+ | PF127 | Physical encap. | Nanosphere | 31–162 | - | PDT | [73] |
 Ru19 | Ru2+ | DSPE-PEG2000 | Physical encap. | NPs | 100 | Biotin was conjugated to the polymer chain for target delivery | PDT | [111] |
 Ru20 | Ru2+ | DSPE-PEG2000 | Physical encap. | Micelles | 122 | FA was conjugated to the polymer chain for target delivery | PDT | [98] |
 Ru21 | Ru2+ | PLGA | Physical encap. | NPs | 130–140 | Co-delivery of Ru-based radiosensitizer alongside radionuclide (111In). The functionalized PLGA surface incorporates the metal ion chelator DTPA for radiolabelling and the targeting ligand for EGF receptor (EGFR) | Ionizing radiation and radiosensitizing CTX. | [46] |
 Ru22–Ru27 | Ru2+ | bipyridine-containing block copolymers | Covalent conjug. | Micelles | 41 (Ru22 and Ru23) 100–1000 with the protein streptavinmmndin. | Biotin was conjugated to polymer chain. Addition of streptavidin to the Ru-loaded micelles induces their cross-linking into larger networks, through biotin-streptavidin binding | Luminescent detector of biomolecules | [112,113] |
 Ru28–Ru30 | Ru2+ | PEG-b-poly(6-(4-cyano-phenoxy) hexyl methacrylate) | Covalent conjug. | Micelles | Ru28 = 12; Ru29 = 48; Ru30 = 120 | Photo-controlled delivery of Ru2+ complexes | PDT | [79] |
 Ru31 | Ru2+ | 2,4-diisocyanato-1-methy-lbenzene-PEG monomethyl ether | Covalent conjug. | Micelles | 180 | Photo-controlled delivery of Ru2+ complex | PDT + PACT | [114,115] |
 Ru32 | Ru2+ | PEG-b-poly (6-(4-cyano-phenoxy) hexyl methacrylate) | Covalent conjug. | Micelles | 15 | Photo-controlled delivery of Ru2+ complex. Polymer chain was covalently attached to anticancer drug chlorambucil | PACT | [56] |
 Ru33 | Ru2+ | PEG-b-poly (6-(4-cyano-phenoxy) hexyl methacrylate) | Covalent conjug. | Micelles | 22 | Photo-controlled delivery of Ru2+ complex | PDT | [115] |
 Ru34 | Pt4+/Ru2+ | PEG | Covalent conjug. | NPs | 90 | Dual-Responsive Pt4+/Ru2+. Reduction-responsive Pt4+ and red-light-responsive Ru2+ moieties. | CTX + PDT | [101] |
 Ru35 and Ru36 | Ru2+ | polysarcosine-b-poly (glutamic acid) | Covalent conjug. | Micelles | 91 | Photo-controlled delivery of Ru2+ complexes | PDT + PACT | [116] |
 Ru37 | Ru2+ | PLA | Covalent conjug. | NPs | 120–310 | Photo-controlled delivery of Ru2+ complex | PDT + PDIM | [63] |
 Ru38 and Os1 | Ru2+ or Os2+ | PP123 | Physical encap. | Micelles | 15 | - | CTX | [117] |
 Ru39 | Ru3+ | caffeic acid-modified chitosan | Covalent conjug. | Micelles | 30–120 | - | CTX | [80] |
 Ru40 and Ru41 | Ru2+ | PP123 | Physical encap. | Micelles | 26 | - | CTX | [118] |
 Ru42 | Ru2+ | PEG-b-poly(glutamic acid) | Covalent conjug. | Micelles | 60 | - | CTX | [78] |
 (KP46)—Ga1 | Ga 3+ | PEG-b-poly(glutamic acid) | Physical encap. | Micelles | 17 | - | CTX | [52] |
 Ga2 and Ga3 | Ga3+ | PF127 | Physical encap. | Micelles | 31–40 | - | PDT | [74] |
 Ga4 | Ga3+ | PF127 | Physical encap. | Micelles | 33 | Polymer chain was functionalized with FA for target delivery | PDT | [71] |
 Ga5 | Ga3+ | PLGA–PEG | Physical encap. | Nanosphere | 86–204 | - | PDT | [64] |
 Au1 | Au+ | PEG-poly(β-amino ester) | Physical encap. | Micelles | 43–50 | pH-responsive drug delivery | CTX | [102] |
 Au2 | Au3+ | DSPE-PEG2000 | Physical encap. | Micelles | 17–21 | - | CTX | [119] |
| PF127 | Physical encap. | Micelles | 26–32 | The hydrophilic shell of micelles was labeled with bioactive CCK8 peptide for target-selective delivery | CTX | [120] | ||
 Au3 | Au+ | Oligo-(ethylene glycol) methyl ether methacrylate | Covalent conjug. | Micelles | 160 | - | CTX | [38] |
 Au4 | Au+ | Poly(2-hydroxy- ethyl acrylate) | Covalent conjug. | Micelles | 75 | - | CTX | [121] |
 Au5 | Au+ | Glycopolymer based on 3-Gluconamido-propyl metha-crylamid and 3-aminopro-pyl methacry-lamid (10 and 30 KDa) | Covalent conjug. | - | 100–250 | - | CTX | [122] |
 Au6 and Au7 | Au3+ | PEG | Covalent conjug. | Micelles | 121 | Co-delivery of DOX | CTX | [47] |
 Cu1 | Cu2+ | PF127 | Physical encap. | Micelles | 23–26 | PF127 was functionalized with carbohydrates (fluorescein, glucosamine, or β-D-glucopyranoside) for target delivery. | CTX | [97] |
 Cu2 | Cu2+ | Chitosan | Physical encap. | NPs | 240 | FA was conjugated to chitosan for target delivery | CTX | [123] |
 Cu3 | Cu2+ | PEG-PLGA | Physical encap. | Nanosphere | 145 | - | CTX | [65] |
 Cu4 | Cu+ | PLA–PEG | Physical encap. | NPs | 50–150 | - | CTX | [66] |
 Cu5 | Cu+/Cu2+ | PEG-b-poly(ester-carbonate) | Covalent conjug. | NPs | 120−135 | - | CTX + CDT | [91] |
 Cu6 | Cu2+ | Hyaluronic acid | Physical encap. | NPs | 125 | pH/GSH dual-responsive drug delivery | CTX | [103] |
 Cu7 | Cu2+ | Chitosan | Physical encap. | NPs | 50–65 | FA or her-2 (specific peptide overexpressed in many cancer cells) was attached to stearic acid-modified chitosan | CTX | [99] |
 Zn1 | Zn2+ | PEG5000-DSPE | Physical encap. | Micelles | 160 | - | PDT | [124] |
| PLGA | Physical encap. | NPs | 285 | - | PDT | [62] | ||
| metoxiPEG-b-PLA | Physical encap. | Micelles | 32–35 | Polymer chain was functionalized with FA for target delivery | PDT | [125] | ||
| PEG-b-PLLA | Physical encap. | Micelles | <150 | Polymer chain was functionalized with FA for target delivery | PDT | [126] | ||
| Heparin, polyethyleneimine and L-cysteine | Physical encap. | Spherical NPs | <200 nm | - | PDT | [127] | ||
| Heparin, DSPE, and l-histidine | Physical encap. | Micelles | 111 | pH-responsive drug delivery | PDT | [42] | ||
| poly(N-acrylamide)-b-PEG-monomethyl ether acrylate) | Physical encap. | Micelles | 167–230 | - | PDT | [128] | ||
| poly(ε-capro-lactone)-PEO | Physical encap. | Micelles | 61–97 | Co-delivery of DTX. | PDT + CTX | [48] | ||
| 3-caprolactone, 1,4,8-trioxa [4.6]spiro-9-undecanone and PEG | Physical encap. | NPs | 108 nm | Co-delivery of DOX. | PDT + CTX | [49] | ||
 Zn2 | Zn2+ | PEG-PLA | Physical encap. | NPs | 464–988 | PDT | [18] | |
 Zn3 | Zn2+ | poly(phthalocyanine-co-sebacic anhydride) | Covalent conjug. | NPs | 166 | - | PDT | [129] |
 Zn4 | Zn2+ | tetra-(methoxy-PEGl)-poly(2-(N,N-diethyl-amino)ethyl methacrylate)-poly(ε-caprolactone) pentaerythritol | Covalent conjug. | NPs | 51–342 (dependent on pH) | pH-responsive drug delivery and co-delivery of DOX | PDT + CTX | [130] |
 Zn5 | Zn2+ | PEO-poly(propylene oxide) | Physical encap. | Micelles | <405 nm | - | PDT | [131] |
 Zn6 | Zn2+ | PEG | Covalent conjug. | Micelles | 350 | - | CTX (HO-1 inhibitor) | [132,133] |
 Zn7 | Zn2+ | SMA | Physical encap. | Micelles | 176 | - | CTX (HO-1 Inhibitor) | [134] |
 Zn8 | Zn2+ | SMA | Covalent conjug. | Micelles | 112 | - | Tumor imaging + PDT | [135] |
 Zn9 | Zn2+ | HPMA | Covalent conjug. | Micelles | 30–80 | - | Tumor imaging + PDT | [136] |
 Zn10 and Zn11 | Zn2+ | PEG | Covalent conjug. | Micelles | - | - | PDT | [137] |
 Zn12 | Zn2+ | PEG | Covalent conjug. | Micelles | 100–150 | Cinnamaldehyde was incorporated in polymer chain to enhance the ROS generation | CTX (oxidation and HO-1 inhibition) | [54] |
 Zn13 and Zn14 | Zn2+ | PP123 and PF127 | Physical encap. | Micelles | - | - | PDT | [138] |
 Zn15 | Zn2+ | DSPE-PEG2000 | Physical encap. | Nanocapsule | 100 | Biotin was conjugated to polymer chain for target-selective drug delivery | PDT | [139] |
 Zn16 | Zn2+ | DSPE-PEG2000-OCH3 | Physical encap. | Nanocapsule | 119 | - | PDT | [140] |
 Zn17 | Zn2+ | DSPE-PEG2000- N-maleimide | Physical encap. | NPs | 39 | The NPs surface was modified with cell penetrating peptide (Tat) to enhance the cellular uptake | PTT | [141] |
 Zn18 | Zn2+ | HOOC-PEG-COOH, and PMHC18-mPEG | Physical encap. | NPs | 81 | - | Imaging and PTT | [142] |
 Zn19 | Zn2+ | PEG | Covalent conjug. | Micelles | 25 | - | PDT of psoriasis | [143] |
 Zn20 | Zn2+ | poly(glycidyl methacrylate) | Covalent conjug. | NPs | 160 | - | PDIM | [144] |
 Ir1 | Ir3+ | oligo-L-lysine Lys30 | Covalent conjug. | NPs | 128 | - | CTX | [145] |
 Ir2 | Ir3+ | PEG-b-P4VP (poly(4-vinylpyridine) | Covalent conjug. | Micelles | 50 | Polymeric chain was functionalized with FA for target delivery | CTX | [146] |
 Ir3 | Ir3+ | PEG-benzoic imine-oligo-L-lysine | Covalent conjug. | NPs | 150 | pH-responsive drug delivery and the nanosystem was FA-modified for target drug release | CTX | [147] |
 Ir4 and Ir5 | Ir3+ | PEG-b-poly(glutamic acid) | Covalent conjug. | Micelles | 58–69 | - | CTX | [78] |
 Ir6 | Ir3+ | 1,4-dimethyl- naphthalene, PEG, and a modifiable disulfide group | Covalent conjug. | NPs | - | Photothermal-responsive delivery of extracellular 1O2 | Phothermal release of 1O2 | [148] |
 Ir7 | Ir3+ | POEGMA-b-PGal | Covalent conjug. | NPs | 65 | Photo-responsive drug delivery | PDT | [149] |
 Ir8 and Ir9 | Ir3+ | P [DMAM-co-VQPy] VQPy (quinoline-based unit 2-(pyridin-2-ylo)-6-styrene-4-phenylquinoline) | Covalent conjug. | NPs | - | pH responsive iridium-complex delivery. | PDT + CTX | [150] |
 Al1 | Al3+ | N-isopropylacrylamide | Physical encap. | Micelles | 35 | pH-responsive drug delivery | PDT | [19] |
| PLGA, PLA, and PLA–PEG | Physical encap. | NPs | 139–199 | - | PDT | [89] | ||
| PF127 | Physical encap. | Micelles | 6 | - | PDT | [84] | ||
 Fe1 | Fe2+ | PEG-PLA | Covalent conjug. | Micelles | 59 | pH-responsive drug delivery and co-delivery of DOX | PDT + CTX | [90] |
 Fe2 | Fe2+ | polycaprolactone modified with histidine and PEG | Covalent conjug. | Micelles | 33 | pH-responsive drug delivery and co-delivery of DOX | PDT + CTX | [151] |
 Pd1 | Pd+ | Hyaluronic acid | Physical encap. | NPs | 204 | - | CTX of advanced melanoma | [152] |
 Co1 | Co3+ | PEG-PLGA | Physical encap. | Nanosphere | 191 | pH-dependent drug release | CTX against cancer and bacterial infection | [153] |
 Mn1 | Mn2+ | PEG-PLGA | Physical encap. | Nanosphere | 93 | - | CTX | [154] |
 Ag1 | Ag+ | Poly(acrylic acid)-b-polystryrene/PEG/PEG-PLGA/polyphosphoester | Physical encap. | NPs | - | - | Antimicrobial treatment | [155,156,157] |
 Ag2 | Ag+ | Poly(e-caprolactone) | Physical encap. | NPs | 155–162 | - | Anti-Helicobacter pylori activity | [158] |
 MPPIX | Fe2+ Co2+ Cu2+ Mn2+ Ni2+ Zn2+ | Marine atelocollagen | Physical encap. | Nanocapsules | - | - | Treat human malaria parasite | [159] |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Dantas, K.C.F.; Rosário, J.d.S.; Silva-Caldeira, P.P. Polymeric Nanosystems Applied for Metal-Based Drugs and Photosensitizers Delivery: The State of the Art and Recent Advancements. Pharmaceutics 2022, 14, 1506. https://doi.org/10.3390/pharmaceutics14071506
Dantas KCF, Rosário JdS, Silva-Caldeira PP. Polymeric Nanosystems Applied for Metal-Based Drugs and Photosensitizers Delivery: The State of the Art and Recent Advancements. Pharmaceutics. 2022; 14(7):1506. https://doi.org/10.3390/pharmaceutics14071506
Chicago/Turabian StyleDantas, Kele Cristina Ferreira, Jânia dos Santos Rosário, and Priscila Pereira Silva-Caldeira. 2022. "Polymeric Nanosystems Applied for Metal-Based Drugs and Photosensitizers Delivery: The State of the Art and Recent Advancements" Pharmaceutics 14, no. 7: 1506. https://doi.org/10.3390/pharmaceutics14071506