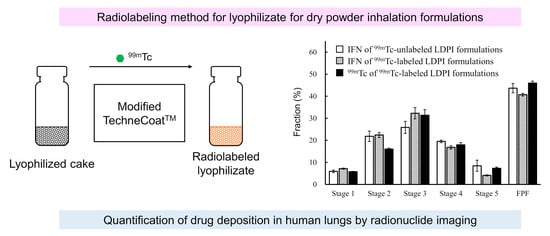
Radiolabeling Method for Lyophilizate for Dry Powder Inhalation Formulations
Abstract
:1. Introduction
2. Materials and Methods
2.1. Materials
2.2. Preparation of Freeze-Dried Cake of IFN
2.3. Radiolabeling of Freeze-Dried Cake by Modified TechneCoat Appartus
2.4. Quantification of IFN by Immunoassay
2.5. Counting Method for Radiolabeling of 99mTc
2.6. Emitted Dose Test for LDPI Formulations of IFN
2.7. Measurement Method for Aerodynamic Particle Size Distribution of IFN and Radiolabel
3. Results
3.1. Validation of the Lyophilizate Transfer Process
3.2. Validation of Radiolabeling Method for LDPI Formulations
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Patton, J.S.; Byron, P.R. Inhaling medicines: Delivering drugs to the body through the lungs. Nat. Rev. Drug Discov. 2007, 6, 67–74. [Google Scholar] [CrossRef]
- Sahane, S.; Nikhar, A.; Bhaskaran, S.; Mundhada, D. Dry powder inhaler: An advance technique for pulmonary drug delivery system. Int. J. Pharm. Chem. Sci. 2012, 1, 1376–1383. [Google Scholar]
- Bajracharya, R.; Song, J.G.; Back, S.Y.; Han, H.-K. Recent advancements in non-invasive formulations for protein drug delivery. Comput. Struct. Biotechnol. J. 2019, 17, 1290–1308. [Google Scholar] [CrossRef]
- Pandaya, S.; Misra, A. Inhalable glucagon-like peptide 1 porous particles prepared by spray freeze drying technique. J. Aerosol Med. Pulm. Drug Deliv. 2016, 29, A16. [Google Scholar]
- Owens, D.R. New horizons—Alternative routes for insulin therapy. Nat. Rev. Drug Discov. 2002, 1, 529–540. [Google Scholar] [CrossRef]
- Yamashita, C.; Ibaragi, S.; Fukunaga, Y.; Akagi, A. Composition, Vessel, Dry Powder Inhalation System, and Related Methods for Transpulmonary Administration. U.S. Patent 7448379, 11 November 2008. [Google Scholar]
- Yamashita, C.; Matsushita, H.; Ibaragi, S.; Akagi, A. Inhalation Device for Transpulmonary Administration. U.S. Patent 7708014, 4 May 2010. [Google Scholar]
- Yamashita, C.; Fukunaga, Y.; Akagi, A. Dry Powder Inhalation System for Transpulmonary Administration. U.S. Patent 7735485, 15 June 2010. [Google Scholar]
- Miyamoto, K.; Ishibashi, Y.; Akita, T.; Yamashita, C. Systemic delivery of hGhrelin derivative by lyophilizate for dry powder inhalation system in monkeys. Pharmaceutics 2021, 13, 233. [Google Scholar] [CrossRef]
- Ohori, R.; Kiuchi, S.; Sugiyama, S.; Miyamoto, K.; Akita, T.; Yamashita, C. Efficient optimization of high-dose formulation of novel lyophilizates for dry powder inhalation by the combination of response surface methodology and time-of-flight measurement. Int. J. Pharm. 2020, 581, 119255. [Google Scholar] [CrossRef] [PubMed]
- Miyamoto, K.; Yanagisawa, M.; Taga, H.; Yamaji, H.; Akita, T.; Yamashita, C. Optimization of very low-dose formulation of vitamin D3 with lyophilizate for dry powder inhalation system by simple method based on time-of-flight theory. Pharmaceutics 2021, 13, 632. [Google Scholar] [CrossRef] [PubMed]
- Miyamoto, K.; Taga, H.; Akita, T.; Yamashita, C. Simple method to measure the aerodynamic size distribution of porous particles generated on lyophilizate for dry powder inhalation. Pharmaceutics 2020, 12, 976. [Google Scholar] [CrossRef] [PubMed]
- Labiris, N.R.; Dolovich, M.B. Pulmonary drug delivery. Part I: Physiological factors affecting therapeutic effectiveness of aerosolized medications. Br. J. Clin. Pharmacol. 2003, 56, 588–599. [Google Scholar] [CrossRef] [PubMed]
- Bondesson, E.; Bengtsson, T.; Borgström, L.; Nilsson, L.-E.; Norrgren, K.; Trofast, E.; Wollmer, P. Planar gamma scintigraphy—Points to consider when quantifying pulmonary dry powder aerosol deposition. Int. J. Pharm. 2003, 251, 33–47. [Google Scholar] [CrossRef]
- Newman, S.P.; Wilding, I.R.; Hirst, P.H. Human lung deposition data: The bridge between in vitro and clinical evaluations for inhaled drug products? Int. J. Pharm. 2000, 208, 49–60. [Google Scholar] [CrossRef]
- Groneberg, D.A.; Witt, C.; Wagner, U.; Chung, K.F.; Fischer, A. Fundamentals of pulmonary drug delivery. Respir. Med. 2003, 97, 382–387. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Newman, S.P. Can lung deposition data act as a surrogate for the clinical response to inhaled asthma drugs? Br. J. Clin. Pharmacol. 2000, 49, 529–537. [Google Scholar] [CrossRef] [PubMed]
- Devadason, S.G.; Chan, H.-K.; Haeussermann, S.; Kietzig, C.; Kuehl, P.J.; Newman, S.; Sommerer, K.; Taylor, G. Validation of radiolabeling of drug formulations for aerosol deposition assessment of orally inhaled products. J. Aerosol Med. Pulm. Drug Deliv. 2012, 25, S-6–S-9. [Google Scholar] [CrossRef] [PubMed]
- Newman, S.P. Characteristics of radiolabelled versus unlabelled inhaler formulations. J. Aerosol Med. 1996, 9 (Suppl. 1), S37–S47. [Google Scholar] [CrossRef]
- Snell, N.J.; Ganderton, D. Assessing lung deposition of inhaled medications. Consensus statement from a workshop of the british association for lung research, Held at the Institute of Biology, London, U.K. on 17 April 1998. Respir. Med. 1999, 93, 123–133. [Google Scholar] [CrossRef] [Green Version]
- Scheuch, G.; Bennett, W.; Borgström, L.; Clark, A.; Dalby, R.; Dolovich, M.; Fleming, J.; Gehr, P.; Gonda, I.; O’Callaghan, C.; et al. Deposition, imaging, and clearance: What remains to be done? J. Aerosol Med. Pulm. Drug Deliv. 2010, 23, S-39–S-57. [Google Scholar] [CrossRef] [PubMed]
- Pitcairn, G.R. Dry Powder Compositions Comprising Labelled Particles for Inhalation. Patent WO-02/074348, 26 September 2002. [Google Scholar]
- Newman, S.P.; Pitcairn, G.R.; Hirst, P.H.; Rankin, L. Radionuclide imaging technologies and their use in evaluating asthma drug deposition in the lungs. Adv. Drug Deliv. Rev. 2003, 55, 851–867. [Google Scholar] [CrossRef]
- Stass, H.; Nagelschmitz, J.; Kappeler, D.; Sommerer, K.; Kietzig, C.; Weimann, B. Ciprofloxacin dry powder for inhalation in patients with non-cystic fibrosis bronchiectasis or chronic obstructive pulmonary disease, and in healthy volunteers. J. Aerosol Med. Pulm. Drug Deliv. 2017, 30, 53–63. [Google Scholar] [CrossRef]
- Newman, S.P.; Pitcairn, G.R.; Hirst, P.H.; Bacon, R.E.; O’Keefe, E.; Reiners, M.; Hermann, R. Scintigraphic comparison of budesonide deposition from two dry powder inhalers. Eur. Respir. J. 2000, 16, 178–183. [Google Scholar] [CrossRef]
- Senden, T.J.; Moock, K.H.; Gerald, J.F.; Burch, W.M.; Browitt, R.J.; Ling, C.D.; Heath, G.A. The physical and chemical nature of technegas. J. Nucl. Med. 1997, 38, 1327–1333. [Google Scholar] [PubMed]
- Longest, P.W.; Tian, G.; Walenga, R.L.; Hindle, M. Comparing MDI and DPI aerosol deposition using in vitro experiments and a new stochastic individual path (SIP) model of the conducting airways. Pharm. Res. 2012, 29, 1670–1688. [Google Scholar] [CrossRef] [PubMed]
- Dolovich, M. In vitro measurements of delivery of medications from MDIs and spacer devices. J. Aerosol Med. 1996, 9, S-49–S-58. [Google Scholar] [CrossRef]
- Evans, C.; Cipolla, D.; Chesworth, T.; Agurell, E.; Ahrens, R.; Conner, D.; Dissanayake, S.; Dolovich, M.; Doub, W.; Fuglsang, A.; et al. Equivalence considerations for orally inhaled products for local action—ISAM/IPAC-RS European Workshop Report. J. Aerosol Med. Pulm. Drug Deliv. 2012, 25, 117–139. [Google Scholar] [CrossRef]
- European Medicines Agency Guideline on the Requirements for Clinical Documentation Orally Inhaled Products (OIP) Including the Requirements Demonstration of Therapeutic Equivalence between Two Use in Treatment Asthma and Chronic Obstructive Pulmonary Disease (COPD) in Adults and for Use in the Treatment of Asthma in Children and Adolescents. Available online: https://www.ema.europa.eu/en/requirements-clinical-documentation-orally-inhaled-products-oip-including-requirements-demonstration (accessed on 19 December 2021).
- Biddiscombe, M.F.; Meah, S.N.; Underwood, S.R.; Usmani, O.S. Comparing lung regions of interest in gamma scintigraphy for assessing inhaled therapeutic aerosol deposition. J. Aerosol Med. Pulm. Drug Deliv. 2011, 24, 165–173. [Google Scholar] [CrossRef]
- Newman, S.P.; Pitcairn, G.R.; Hirst, P.H. A brief history of gamma scintigraphy. J. Aerosol Med. 2001, 14, 139–145. [Google Scholar] [CrossRef]
- Borgström, L.; Newman, S.; Weisz, A.; Morén, F. Pulmonary deposition of inhaled terbutaline: Comparison of scanning gamma camera and urinary excretion methods. J. Pharm. Sci. 1992, 81, 753–755. [Google Scholar] [CrossRef]






Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Miyamoto, K.; Akita, T.; Yamashita, C. Radiolabeling Method for Lyophilizate for Dry Powder Inhalation Formulations. Pharmaceutics 2022, 14, 759. https://doi.org/10.3390/pharmaceutics14040759
Miyamoto K, Akita T, Yamashita C. Radiolabeling Method for Lyophilizate for Dry Powder Inhalation Formulations. Pharmaceutics. 2022; 14(4):759. https://doi.org/10.3390/pharmaceutics14040759
Chicago/Turabian StyleMiyamoto, Kahori, Tomomi Akita, and Chikamasa Yamashita. 2022. "Radiolabeling Method for Lyophilizate for Dry Powder Inhalation Formulations" Pharmaceutics 14, no. 4: 759. https://doi.org/10.3390/pharmaceutics14040759