Development of Mucoadhesive Buccal Film for Rizatriptan: In Vitro and In Vivo Evaluation
Abstract
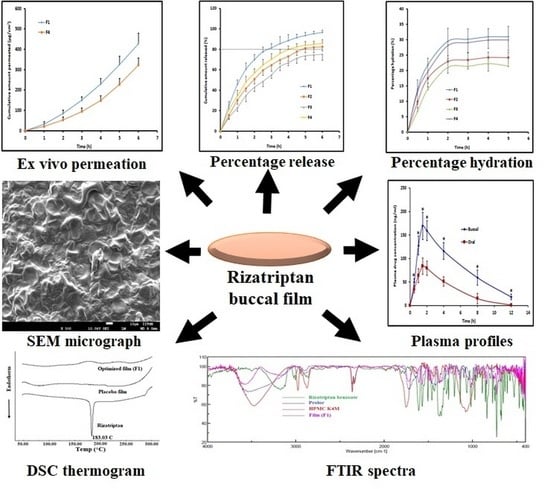
:1. Introduction
2. Materials and Methods
2.1. Materials
2.2. High-Performance Liquid Chromatography (HPLC)
2.3. Formulation of Films
2.4. Formulation of Drug-Loaded Films
2.5. Characterization of Buccal Films
2.5.1. Thickness and pH
2.5.2. Drug Content
2.5.3. Folding Endurance
2.5.4. Mucoadhesive Strength
2.5.5. Percent Hydration
2.6. Fourier Transform Infrared (FTIR)
2.7. Differential Scanning Calorimetry
2.8. Scanning Electron Microscopy
2.9. Drug Release
2.10. Ex Vivo Permeation
2.11. In-Vivo Evaluation
2.12. Data Analysis
3. Results and Discussion
3.1. Formulation of Buccal Films
3.2. Film Characteristics
3.3. FTIR
3.4. DSC
3.5. SEM
3.6. Drug Release
3.7. Ex Vivo Permeation
3.8. In Vivo
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Leonardi, M.; Raggi, A. Burden of migraine: International perspectives. Neurol. Sci. 2013, 34 (Suppl. S1), 117–118. [Google Scholar] [CrossRef] [Green Version]
- Raggi, A.; Giovannetti, A.M.; Quintas, R.; D’Amico, D.; Cieza, A.; Sabariego, C.; Bickenbach, J.E.; Leonardi, M. A systematic review of the psychosocial difficulties relevant to patients with migraine. J. Headache Pain 2012, 13, 595–606. [Google Scholar] [CrossRef] [Green Version]
- Ong, J.J.Y.; De Felice, M. Migraine Treatment: Current Acute Medications and Their Potential Mechanisms of Action. Neurotherapeutics 2018, 15, 274–290. [Google Scholar] [CrossRef] [Green Version]
- Negro, A.; Koverech, A.; Martelletti, P. Serotonin receptor agonists in the acute treatment of migraine: A review on their therapeutic potential. J. Pain Res. 2018, 11, 515–526. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rubio-Beltrán, E.; Labastida-Ramírez, A.; Villalón, C.M.; MaassenVanDenBrink, A. Is selective 5-HT 1F receptor agonism an entity apart from that of the triptans in antimigraine therapy? Pharmacol. Ther. 2018, 186, 88–97. [Google Scholar] [CrossRef] [PubMed]
- Ferrari, M.D.; Goadsby, P.J.; Roon, K.I.; Lipton, R.B. Triptans (serotonin, 5-HT1B/1D agonists) in migraine: Detailed results and methods of a meta-analysis of 53 trials. Cephalalgia 2002, 22, 633–658. [Google Scholar] [CrossRef] [PubMed]
- Krymchantowski, A.V.; Bigal, M.E. Rizatriptan in migraine. Expert Rev. Neurother. 2005, 5, 597–603. [Google Scholar] [CrossRef]
- Láinez, M.J. Rizatriptan in the treatment of migraine. Neuropsychiatr. Dis. Treat. 2006, 2, 247–259. [Google Scholar] [CrossRef] [Green Version]
- McEnroe, J.D.; Fleishaker, J.C. Clinical Pharmacokinetics of Almotriptan, a Serotonin 5-HT1B/1D Receptor Agonist for the Treatment of Migraine. Clin. Pharmacokinet. 2005, 44, 237–246. [Google Scholar] [CrossRef]
- Kassem, A.A. Formulation Approaches of Triptans for Management of Migraine. Curr. Drug Deliv. 2016, 13, 882–898. [Google Scholar] [CrossRef] [PubMed]
- Salehi, S.; Boddohi, S. Design and optimization of kollicoat ® IR based mucoadhesive buccal film for co-delivery of rizatriptan benzoate and propranolol hydrochloride. Mater. Sci. Eng. C 2019, 97, 230–244. [Google Scholar] [CrossRef]
- Montenegro-Nicolini, M.; Morales, J.O. Overview and Future Potential of Buccal Mucoadhesive Films as Drug Delivery Systems for Biologics. AAPS PharmSciTech 2016, 18, 3–14. [Google Scholar] [CrossRef]
- Nair, A.B.; Al-Dhubiab, B.E.; Shah, J.; Jacob, S.; Saraiya, V.; Attimarad, M.; SreeHarsha, N.; Akrawi, S.H.; Shehata, T.M. Mucoadhesive buccal film of almotriptan improved therapeutic delivery in rabbit model. Saudi Pharm. J. 2020, 28, 201–209. [Google Scholar] [CrossRef]
- Montero-Padilla, S.; Velaga, S.; Morales, J.O. Buccal Dosage Forms: General Considerations for Pediatric Patients. AAPS PharmSciTech 2016, 18, 273–282. [Google Scholar] [CrossRef] [PubMed]
- Mahajan, A.; Chhabra, N.; Aggarwal, G. Formulation and characterization of fast dissolving buccal films: A review. Der Pharm. Lett. 2011, 3, 152–165. [Google Scholar]
- Nair, A.B.; Kumria, R.; Harsha, S.; Attimarad, M.; Al-Dhubiab, B.E.; Alhaider, I.A. In vitro techniques to evaluate buccal films. J. Control. Release 2013, 166, 10–21. [Google Scholar] [CrossRef] [PubMed]
- Jacob, S.; Nair, A.B.; Patel, V.; Shah, J. 3D Printing Technologies: Recent Development and Emerging Applications in Various Drug Delivery Systems. AAPS PharmSciTech 2020, 21, 1–16. [Google Scholar] [CrossRef]
- Laffleur, F. Mucoadhesive polymers for buccal drug delivery. Drug Dev. Ind. Pharm. 2014, 40, 591–598. [Google Scholar] [CrossRef]
- Bagan, J.; Paderni, C.; Termine, N.; Campisi, G.; Russo, L.L.; Compilato, D.; Di Fede, O. Mucoadhesive polymers for oral transmucosal drug delivery: A review. Curr. Pharm. Des. 2012, 18, 5497–5514. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Agarwal, S.; Aggarwal, S. Mucoadhesive polymeric platform for drug delivery; a comprehensive review. Curr. Drug Deliv. 2015, 12, 139–156. [Google Scholar] [CrossRef]
- Duggan, S.; Cummins, W.; Donovan, O.O.; Hughes, H.; Owens, E. Thiolated polymers as mucoadhesive drug delivery systems. Eur. J. Pharm. Sci. 2017, 100, 64–78. [Google Scholar] [CrossRef]
- Jacob, S.; Nair, A.B. Cyclodextrin complexes: Perspective from drug delivery and formulation. Drug Dev. Res. 2018, 79, 201–217. [Google Scholar] [CrossRef] [PubMed]
- Pendekal, M.S.; Tegginamat, P.K. Formulation and evaluation of a bioadhesive patch for buccal delivery of tizanidine. Acta Pharm. Sin. B 2012, 2, 318–324. [Google Scholar] [CrossRef] [Green Version]
- Nair, A.; Gupta, R.; Vasanti, S. In vitro controlled release of alfuzosin hydrochloride using hpmc-based matrix tablets and its comparison with marketed product. Pharm. Dev. Technol. 2007, 12, 621–625. [Google Scholar] [CrossRef] [PubMed]
- Prabhu, P.; Malli, R.; Koland, M.; Vijaynarayana, K.; D′souza, U.; Harish, N.; Shastry, C.; Charyulu, R. Formulation and evaluation of fast dissolving films of levocitirizine di hydrochloride. Int. J. Pharm. Investig. 2011, 1, 99–104. [Google Scholar] [CrossRef] [Green Version]
- Alhijjaj, M.; Bouman, J.; Wellner, N.; Belton, P.; Qi, S. Creating Drug Solubilization Compartments via Phase Separation in Multicomponent Buccal Patches Prepared by Direct Hot Melt Extrusion–Injection Molding. Mol. Pharm. 2015, 12, 4349–4362. [Google Scholar] [CrossRef]
- Lavudu, P.; Rani, A.P.; Divya, C.; Sekharan, C.B. High performance liquid chromatographic analysis of almotriptan malate in bulk and tablets. Adv. Pharm. Bull. 2013, 3, 183–188. [Google Scholar]
- Kumria, R.; Nair, A.B.; Goomber, G.; Gupta, S. Buccal films of prednisolone with enhanced bioavailability. Drug Deliv. 2014, 23, 471–478. [Google Scholar] [CrossRef] [Green Version]
- SreeHarsha, N.; Hiremath, J.G.; Sarudkar, S.; Attimarad, M.; Al-Dhubiab, B.; Nair, A.B.; Venugopala, K.N.; Asif, A.H. Spray Dried Amorphous Form of Simvastatin: Preparation and Evaluation of the Buccal Tablet. Indian J. Pharm. Educ. Res. 2019, 54, 46–54. [Google Scholar] [CrossRef] [Green Version]
- Kumria, R.; Al-Dhubiab, B.E.; Shah, J.; Nair, A.B. Formulation and Evaluation of Chitosan-Based Buccal Bioadhesive Films of Zolmitriptan. J. Pharm. Innov. 2018, 13, 133–143. [Google Scholar] [CrossRef]
- Kumria, R.; Nair, A.; Al-Dhubiab, B.E. Loratidine buccal films for allergic rhinitis: Development and evaluation. Drug Dev. Ind. Pharm. 2014, 40, 625–631. [Google Scholar] [CrossRef]
- Nair, A.B.; Gupta, S.; Al-Dhubiab, B.E.; Jacob, S.; Shinu, P.; Shah, J.; Morsy, M.A.; Sreeharsha, N.; Attimarad, M.; Venugopala, K.N.; et al. Effective Therapeutic Delivery and Bioavailability Enhancement of Pioglitazone Using Drug in Adhesive Transdermal Patch. Pharmaceutics 2019, 11, 359. [Google Scholar] [CrossRef] [PubMed]
- Jug, M.; Hafner, A.; Lovrić, J.; Kregar, M.L.; Pepić, I.; Vanić, Ž.; Cetina-Čižmek, B.; Filipović-Grčić, J. An overview of in vitro dissolution/release methods for novel mucosal drug delivery systems. J. Pharm. Biomed. Anal. 2018, 147, 350–366. [Google Scholar] [CrossRef]
- Repka, M.A.; Gutta, K.; Prodduturi, S.; Munjal, M.; Stodghill, S.P. Characterization of cellulosic hot-melt extruded films containing lidocaine. Eur. J. Pharm. Biopharm. 2005, 59, 189–196. [Google Scholar] [CrossRef]
- Shah, J.; Nair, A.B.; Jacob, S.; Patel, R.K.; Shah, H.; Shehata, T.M.; Morsy, M.A. Nanoemulsion Based Vehicle for Effective Ocular Delivery of Moxifloxacin Using Experimental Design and Pharmacokinetic Study in Rabbits. Pharmaceutics 2019, 11, 230. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Nair, A.; Reddy, C.; Jacob, S. Delivery of a classical antihypertensive agent through the skin by chemical enhancers and iontophoresis. Ski. Res. Technol. 2009, 15, 187–194. [Google Scholar] [CrossRef]
- Nair, A.; Morsy, M.A.; Jacob, S. Dose translation between laboratory animals and human in preclinical and clinical phases of drug development. Drug Dev. Res. 2018, 79, 373–382. [Google Scholar] [CrossRef]
- Al-Dhubiab, B.E.; Nair, A.B.; Kumria, R.; Attimarad, M.; Harsha, S. Development and evaluation of buccal films impregnated with selegiline-loaded nanospheres. Drug Deliv. 2014, 23, 2154–2162. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Nair, A.B.; Al-Dhubiab, B.E.; Shah, J.; Vimal, P.; Attimarad, M.; Harsha, S. Development and evaluation of palonosetron loaded mucoadhesive buccal films. J. Drug Deliv. Sci. Technol. 2018, 47, 351–358. [Google Scholar] [CrossRef]
- Sandri, G.; Rossi, S.; Ferrari, F.; Bonferoni, M.C.; Muzzarelli, C.; Caramella, C. Assessment of chitosan derivatives as buccal and vaginal penetration enhancers. Eur. J. Pharm. Sci. 2004, 21, 351–359. [Google Scholar] [CrossRef]
- Boateng, J.; Okeke, O. Evaluation of Clay-Functionalized Wafers and Films for Nicotine Replacement Therapy via Buccal Mucosa. Pharmaceutics 2019, 11, 104. [Google Scholar] [CrossRef] [Green Version]
- Avachat, A.M.; Gujar, K.N.; Wagh, K.V. Development and evaluation of tamarind seed xyloglucan-based mucoadhesive buccal films of rizatriptan benzoate. Carbohydr. Polym. 2013, 91, 537–542. [Google Scholar] [CrossRef]
- Salamat-Miller, N.; Chittchang, M.; Johnston, T.P. The use of mucoadhesive polymers in buccal drug delivery. Adv. Drug Deliv. Rev. 2005, 57, 1666–1691. [Google Scholar] [CrossRef]
- Asane, G.S.; Nirmal, S.A.; Rasal, K.B.; Naik, A.A.; Mahadik, M.S.; Rao, Y.M. Polymers for mucoadhesive drug delivery system: A current status. Drug Dev. Ind. Pharm. 2008, 34, 1246–1266. [Google Scholar] [CrossRef] [PubMed]
- Bharate, S.S.; Bharate, S.B.; Bajaj, A.N. Interactions and incompatibilities of pharmaceutical excipients with active pharmaceutical ingredients: A comprehensive review. J. Excip. Food Chem. 2016, 1, 1131. [Google Scholar]
- Dungarwal, U.N.; Patil, S.B. Development of orodispersible tablets of taste masked rizatriptan benzoate using hydroxypropyl β cyclodextrin. J. Pharm. Investig. 2016, 46, 537–545. [Google Scholar] [CrossRef]
- Boateng, J.S.; Ayensu, I. Preparation and characterization of laminated thiolated chitosan-based freeze-dried wafers for potential buccal delivery of macromolecules. Drug Dev. Ind. Pharm. 2014, 40, 611–618. [Google Scholar] [CrossRef]
- Jacob, S.; Nair, A. An updated overview with simple and practical approach for developing in vitro-in vivo correlation. Drug Dev. Res. 2018, 79, 97–110. [Google Scholar] [CrossRef]
- Fu, Y.; Kao, W.J. Drug release kinetics and transport mechanisms of non-degradable and degradable polymeric delivery systems. Expert Opin. Drug Deliv. 2010, 7, 429–444. [Google Scholar] [CrossRef] [PubMed]
- Jaipal, A.; Pandey, M.M.; Charde, S.Y.; Sadhu, N.; Srinivas, A.; Prasad, R.G. Controlled release effervescent buccal discs of buspirone hydrochloride: In vitro and in vivo evaluation studies. Drug Deliv. 2014, 23, 452–458. [Google Scholar] [CrossRef] [Green Version]
- Pinto, S.; Pintado, M.E.; Sarmento, B. In vivo, ex vivo and in vitro assessment of buccal permeation of drugs from delivery systems. Expert Opin. Drug Deliv. 2020, 17, 33–48. [Google Scholar] [CrossRef] [PubMed]







| Batch Code | Proloc (% w/v) | HPMC F4M (% w/v) | HPMC K100M (% w/v) | HPMC K4M (% w/v) | Eudragit RS 100 (% w/v) | PEG 200 (% w/v) | PG (% w/v) | Tween 80 (% w/v) | Film Properties |
|---|---|---|---|---|---|---|---|---|---|
| FR1 | 10 | - | - | - | 15 | 2.5 | 2.5 | 0.5 | Non-homogenous film formed after drying |
| FR2 | 8 | 2 | - | - | 15 | 2.5 | 2.5 | 0.5 | Small cracking occurred after drying |
| FR3 | 6 | 4 | - | - | 15 | 2.5 | 2.5 | 0.5 | Films formed were non-tacky, peelable and possessed enough mechanical strength |
| FR4 | 4 | 6 | - | - | 15 | 2.5 | 2.5 | 0.5 | Films formed were non-tacky, peelable and possessed enough mechanical strength |
| FR5 | 8 | - | 2 | - | 15 | 2.5 | 2.5 | 0.5 | Films formed were non-tacky, peelable and possessed enough mechanical strength |
| FR6 | 6 | - | 4 | - | 15 | 2.5 | 2.5 | 0.5 | Films formed were sticky |
| FR7 | 4 | - | 6 | - | 15 | 2.5 | 2.5 | 0.5 | Films formed were thick |
| FR8 | 8 | - | - | 2 | 15 | 2.5 | 2.5 | 0.5 | Small cracking occurred after drying |
| FR9 | 6 | - | - | 4 | 15 | 2.5 | 2.5 | 0.5 | Films formed were non-tacky, peelable and possessed enough mechanical strength |
| FR10 | 4 | - | - | 6 | 15 | 2.5 | 2.5 | 0.5 | Films formed were sticky |
| Batch Code | Rizatriptan (% w/v) | Proloc 15 (% w/v) | HPMC F4M (% w/v) | HPMC K100M (% w/v) | HPMC K4M (% w/v) | Eudragit RS 100 (% w/v) | PEG 200 (% w/v) | PG (% w/v) | Tween 80 (% w/v) |
|---|---|---|---|---|---|---|---|---|---|
| F1 | 6.4 | 6 | 4 | - | - | 15 | 2.5 | 2.5 | 0.5 |
| F2 | 6.4 | 4 | 6 | - | - | 15 | 2.5 | 2.5 | 0.5 |
| F3 | 6.4 | 8 | - | 2 | - | 15 | 2.5 | 2.5 | 0.5 |
| F4 | 6.4 | 6 | - | - | 4 | 15 | 2.5 | 2.5 | 0.5 |
| Batch Code | Thickness (Mm) | pH | Folding Endurance (Number) | Drug Content (%) | Mucoadhesive Strength (N) |
|---|---|---|---|---|---|
| F1 | 1.24 ± 0.27 | 7.2 ± 0.3 | 295 ± 20 | 95.1 ± 3.6 | 7.0 ± 0.4 |
| F2 | 1.02 ± 0.16 | 7.0 ± 0.1 | 270 ± 18 | 94.8 ± 2.7 | 6.5 ± 0.3 |
| F3 | 1.32 ± 0.34 | 6.9 ± 0.2 | 305 ± 26 | 96.0 ± 1.8 | 7.3 ± 0.2 |
| F4 | 1.18 ± 0.21 | 7.1 ± 0.3 | 285 ± 15 | 94.7 ± 3.1 | 6.7 ± 0.3 |
| Parameter | Buccal Film (F1) | Control |
|---|---|---|
| Tmax (h) | 1.5 | 1.5 |
| Cmax (ng/mL) | 169.43 ± 28.67 | 83.85 ± 17.35 |
| AUC0–12 (ng.h/mL) | 994.86 ± 95.79 | 406.45 ± 61.08 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Nair, A.B.; Shah, J.; Jacob, S.; Al-Dhubiab, B.E.; Patel, V.; Sreeharsha, N.; Shinu, P. Development of Mucoadhesive Buccal Film for Rizatriptan: In Vitro and In Vivo Evaluation. Pharmaceutics 2021, 13, 728. https://doi.org/10.3390/pharmaceutics13050728
Nair AB, Shah J, Jacob S, Al-Dhubiab BE, Patel V, Sreeharsha N, Shinu P. Development of Mucoadhesive Buccal Film for Rizatriptan: In Vitro and In Vivo Evaluation. Pharmaceutics. 2021; 13(5):728. https://doi.org/10.3390/pharmaceutics13050728
Chicago/Turabian StyleNair, Anroop B., Jigar Shah, Shery Jacob, Bandar E. Al-Dhubiab, Vimal Patel, Nagaraja Sreeharsha, and Pottathil Shinu. 2021. "Development of Mucoadhesive Buccal Film for Rizatriptan: In Vitro and In Vivo Evaluation" Pharmaceutics 13, no. 5: 728. https://doi.org/10.3390/pharmaceutics13050728