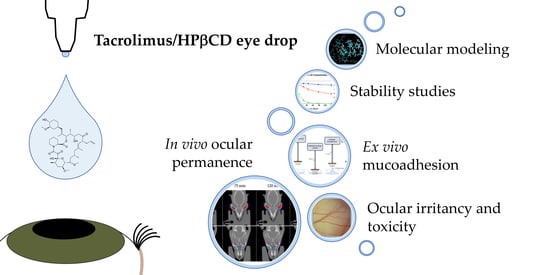
Development and Characterization of a Tacrolimus/Hydroxypropyl-β-Cyclodextrin Eye Drop
Abstract
:1. Introduction
2. Materials and Methods
2.1. Tacrolimus/HPβCD Solubilization Study
2.1.1. Phase Solubility Diagram
2.1.2. NMR Studies and Molecular Modeling
2.1.3. Vehicle Solubility Study
2.2. Formulation Preparation Procedure
2.3. Optimization Procedure: Tacrolimus Solubilization Time
2.4. Physicochemical Characterization
2.4.1. pH and Osmolality Determination
2.4.2. Surface Tension Determination
2.4.3. Squeezing Force Determination
2.5. Corneal Mucoadhesion
2.5.1. Bovine Corneal Opacity and Permeability Test (BCOP)
2.5.2. Hen’s Egg Test on the Chorioallantoic Membrane (HETCAM)
2.6. Stability Study
2.6.1. Quantification of Tacrolimus Amount
2.6.2. Osmolality, pH and Microbiological Control Growth
2.6.3. Statistical Analysis
2.7. In Vivo Evaluation of the Residence Time on the Ocular Surface
3. Results and Discussion
3.1. Tacrolimus/HPβCD Solubilization Study
3.2. Physicochemical Characterization
3.2.1. pH, Osmolality and Surface Tension
3.2.2. Squeezing Force Determinations
3.3. Corneal Mucoadhesion
3.4. Ocular Irritancy and Toxicity
3.4.1. Bovine Corneal Opacity and Permeability Test (BCOP)
3.4.2. Hen’s Egg Test on the Chorioallantoic Membrane (HETCAM)
3.5. Stability Study
3.6. In Vivo Evaluation of the Residence Time on the Ocular Surface
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- De Smet, M.D.; Taylor, S.R.; Bodaghi, B.; Miserocchi, E.; Murray, P.I.; Pleyer, U.; Zierhut, M.; Barisani-Asenbauer, T.; LeHoang, P.; Lightman, S. Understanding uveitis: The impact of research on visual outcomes. Prog. Retin. Eye Res. 2011, 30, 452–470. [Google Scholar] [CrossRef] [PubMed]
- Bodaghi, B.; Cassoux, N.; Wechsler, B.; Hannouche, D.; Fardeau, C.; Papo, T.; Huong, D.L.T.; Piette, J.-C.; LeHoang, P. Chronic Severe Uveitis. J. Clin. Med. 2001, 80, 263–270. [Google Scholar] [CrossRef] [PubMed]
- Zhai, J.; Gu, J.; Yuan, A.P.J.; Chen, P.J. Tacrolimus in the Treatment of Ocular Diseases. BioDrugs 2011, 25, 89–103. [Google Scholar] [CrossRef] [PubMed]
- Rothova, A.; Van Veenendaal, W.; Linssen, A.; Glasius, E.; Kijlstra, A.; De Jong, P. Clinical Features of Acute Anterior Uveitis. Am. J. Ophthalmol. 1987, 103, 137–145. [Google Scholar] [CrossRef] [Green Version]
- Garg, V.; Jain, G.K.; Nirmal, J.; Kohli, K. Topical tacrolimus nanoemulsion, a promising therapeutic approach for uveitis. Med. Hypotheses 2013, 81, 901–904. [Google Scholar] [CrossRef] [PubMed]
- Fabiani, C.; Vitale, A.; Orlando, I.; Capozzoli, M.; Fusco, F.; Rana, F.; Franceschini, R.; Sota, J.; Frediani, B.; Galeazzi, M.; et al. Impact of Uveitis on Quality of Life: A Prospective Study from a Tertiary Referral Rheumatology-Ophthalmology Collaborative Uveitis Center in Italy. Isr. Med. Assoc. J. IMAJ 2017, 19, 478–483. [Google Scholar] [PubMed]
- Thorne, J.E.; Skup, M.; Tundia, N.; Macaulay, D.; Revol, C.; Chao, J.; Joshi, A.; Dick, A.D. Direct and indirect resource use, healthcare costs and work force absence in patients with non-infectious intermediate, posterior or panuveitis. Acta Ophthalmol. 2016, 94, e331–e339. [Google Scholar] [CrossRef] [Green Version]
- Chu, D.S.; Johnson, S.; Mallya, U.; Davis, M.R.; Sorg, R.A.; Duh, M.S. Healthcare costs and utilization for privately insured patients treated for non-infectious uveitis in the USA. J. Ophthalmic Inflamm. Infect. 2013, 3, 64. [Google Scholar] [CrossRef] [Green Version]
- Taddio, A.; Cimaz, R.; Caputo, R.; DeLibero, C.; Di Grande, L.; Simonini, G.; Mori, F.; Novembre, E.; Pucci, N. Childhood chronic anterior uveitis associated with vernal keratoconjunctivitis (VKC): Successful treatment with topical tacrolimus. Case series. Pediatr. Rheumatol. Online J. 2011, 9, 34. [Google Scholar] [CrossRef] [Green Version]
- Jewett, A.; Tseng, H.-C. 35-Immunotherapy. In Pharmacology and Therapeutics for Dentistry, 7th ed.; Dowd, F.J., Johnson, B.S., Mariotti, A.J., Eds.; Mosby: Maryland Heights, MO, USA, 2017; pp. 504–529. ISBN 978-0-323-39307-2. [Google Scholar]
- Moscovici, B.K.; Holzchuh, R.; Chiacchio, B.B.; Santo, R.M.; Shimazaki, J.; Hida, R.Y. Clinical Treatment of Dry Eye Using 0.03% Tacrolimus Eye Drops. Cornea 2012, 31, 945–949. [Google Scholar] [CrossRef]
- Joseph, A.; Raj, D.; Shanmuganathan, V.; Powell, R.J.; Dua, H.S. Tacrolimus immunosuppression in high-risk corneal grafts. Br. J. Ophthalmol. 2006, 91, 51–55. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hikita, N.; Lopez, J.S.; Chan, C.C.; Mochizuki, M.; Nussenblatt, R.B.; De Smet, M.D. Use of topical FK506 in a corneal graft rejection model in Lewis rats. Investig. Ophthalmol. Vis. Sci. 1997, 38, 901–909. [Google Scholar]
- Mills, R.; Jones, D.B.; Winkler, C.R.; Wallace, G.W.; Wilhelmus, K.R. Topical FK-506 prevents experimental corneal allograft rejection. Cornea 1995, 14, 157–160. [Google Scholar] [CrossRef] [PubMed]
- Luaces-Rodríguez, A.; Touriño-Peralba, R.; Alonso-Rodríguez, I.; García-Otero, X.; González-Barcia, M.; Rodríguez-Ares, M.T.; Martínez-Pérez, L.; Aguiar, P.; Gómez-Lado, N.; Silva-Rodríguez, J.; et al. Preclinical characterization and clinical evaluation of tacrolimus eye drops. Eur. J. Pharm. Sci. 2018, 120, 152–161. [Google Scholar] [CrossRef] [PubMed]
- Astellas Pharma Inc. A Randomized, Placebo-Controlled, Double-Masked Study of 0.1% Tacrolimus (FK506) Ophthalmic Suspension in Vernal Keratoconjunctivitis. Available online: https://www.clinicaltrials.gov/ct2/show/NCT00567762 (accessed on 21 January 2021).
- Shoughy, S.S.; Jaroudi, M.O.; Tabbara, K.F. Efficacy and safety of low-dose topical tacrolimus in vernal keratoconjunctivitis. Clin. Ophthalmol. 2016, 10, 643–647. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Moawd, P. Evaluation of the Effect of Topical Application of Tacrolimus 0.03% (FK506) Eye Drops Versus Cyclosporine 0.05% Eye Drops in Treatment of Dry Eye in Secondary Sjogren Syndrome. Available online: https://www.clinicaltrials.gov/ct2/show/NCT03865888webpage (accessed on 21 January 2021).
- Whitcup, S.M.; Pleyer, U.; Lai, J.C.; Lutz, S.; Mochizuki, M.; Chan, C.-C. Topical liposome-encapsulated FK506 for the treatment of endotoxin-induced uveitis. Ocul. Immunol. Inflamm. 1998, 6, 51–56. [Google Scholar] [CrossRef] [PubMed]
- Ishioka, M.; Ohno, S.; Nakamura, S.; Isobe, K.; Watanabe, N.; Ishigatsubo, Y.; Tanaka, S.-I. FK506 Treatment of Noninfectious Uveitis. Am. J. Ophthalmol. 1994, 118, 723–729. [Google Scholar] [CrossRef]
- Young, A.L.; Wong, S.; Leung, A.T.; Leung, G.Y.; Cheng, L.L.; Lam, D.S. Clinical Case Notes. Successful treatment of surgically induced necrotizing scleritis with tacrolimus. Clin. Exp. Ophthalmol. 2005, 33, 98–99. [Google Scholar] [CrossRef]
- Lee, Y.J.; Kim, S.W.; Seo, K.Y. Application for Tacrolimus Ointment in Treating Refractory Inflammatory Ocular Surface Diseases. Am. J. Ophthalmol. 2013, 155, 804–813.e1. [Google Scholar] [CrossRef]
- Ryu, E.H.; Kim, J.M.; Laddha, P.M.; Chung, E.-S.; Chung, T.-Y. Therapeutic Effect of 0.03% Tacrolimus Ointment for Ocular Graft versus Host Disease and Vernal Keratoconjunctivitis. Korean, J. Ophthalmol. 2012, 26, 241–247. [Google Scholar] [CrossRef]
- Tam, P.M.K.; Young, A.L.; Cheng, L.L.; Lam, P.T.H. Topical 0.03% tacrolimus ointment in the management of ocular surface inflammation in chronic GVHD. Bone Marrow Transplant. 2009, 45, 957–958. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jung, J.W.; Lee, Y.J.; Yoon, S.; Kim, T.-I.; Kim, E.K.; Seo, K.Y. Long-term Result of Maintenance Treatment with Tacrolimus Ointment in Chronic Ocular Graft-Versus-Host Disease. Am. J. Ophthalmol. 2015, 159, 519–527.e1. [Google Scholar] [CrossRef] [PubMed]
- Murphy, C.C.; Greiner, K.; Plskova, J.; Duncan, L.; Frost, N.A.; Forrester, J.V.; Dick, A.D. Cyclosporine vs Tacrolimus Therapy for Posterior and Intermediate Uveitis. Arch. Ophthalmol. 2005, 123, 634–641. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Prajapati, M.; Eiriksson, F.F.; Loftsson, T. Stability characterization, kinetics and mechanism of tacrolimus degradation in cyclodextrin solutions. Int. J. Pharm. 2020, 586, 119579. [Google Scholar] [CrossRef] [PubMed]
- Patel, P.V.; Patel, H.K.; Mehta, T.A.; Panchal, S.S. Self micro-emulsifying drug delivery system of tacrolimus: Formulation, in vitro evaluation and stability studies. Int. J. Pharm. Investig. 2013, 3, 95–104. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Siegl, C.; König-Schuster, M.; Nakowitsch, S.; Koller, C.; Graf, P.; Unger-Manhart, N.; Schindlegger, Y.; Kirchoff, N.; Knecht, C.; Prieschl-Grassauer, E.; et al. Pharmacokinetics of topically applied tacrolimus dissolved in Marinosolv, a novel aqueous eye drop formulation. Eur. J. Pharm. Biopharm. 2019, 134, 88–95. [Google Scholar] [CrossRef]
- Zeng, W.; Li, Q.; Wan, T.; Liu, C.; Pan, W.; Wu, Z.; Zhang, G.; Pan, J.; Qin, M.; Lin, Y.; et al. Hyaluronic acid-coated niosomes facilitate tacrolimus ocular delivery: Mucoadhesion, precorneal retention, aqueous humor pharmacokinetics, and transcorneal permeability. Colloids Surf. B 2016, 141, 28–35. [Google Scholar] [CrossRef]
- Lamprecht, A.; Yamamoto, H.; Takeuchi, H.; Kawashima, Y. A pH-sensitive microsphere system for the colon delivery of tacrolimus containing nanoparticles. J. Control. Release 2005, 104, 337–346. [Google Scholar] [CrossRef]
- Nassar, T.; Rom, A.; Nyska, A.; Benita, S. A Novel Nanocapsule Delivery System to Overcome Intestinal Degradation and Drug Transport Limited Absorption of P-glycoprotein Substrate Drugs. Pharm. Res. 2008, 25, 2019–2029. [Google Scholar] [CrossRef]
- Wang, Y.; Wang, C.; Fu, S.; Liu, Q.; Dou, D.; Lv, H.; Fan, M.; Guo, G.; Luo, F.; Qian, Z. Preparation of Tacrolimus loaded micelles based on poly(ε-caprolactone)–poly(ethylene glycol)–poly(ε-caprolactone). Int. J. Pharm. 2011, 407, 184–189. [Google Scholar] [CrossRef]
- Uno, T.; Yamaguchi, T.; Li, X.K.; Suzuki, Y.; Hashimoto, H.; Harada, Y.; Kimura, T.; Kazui, T. The pharmacokinetics of water-in-oil-in-water-type multiple emulsion of a new tacrolimus formulation. Lipids 1997, 32, 543–548. [Google Scholar] [CrossRef] [PubMed]
- Janicki, J.J.; Chancellor, M.B.; Kaufman, J.; Gruber, M.A.; Chancellor, D.D. Potential Effect of Liposomes and Liposome-Encapsulated Botulinum Toxin and Tacrolimus in the Treatment of Bladder Dysfunction. Toxins 2016, 8, 81. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gao, S.; Sun, J.; Fu, D.; Zhao, H.; Lan, M.; Gao, F. Preparation, characterization and pharmacokinetic studies of tacrolimus-dimethyl-β-cyclodextrin inclusion complex-loaded albumin nanoparticles. Int. J. Pharm. 2012, 427, 410–416. [Google Scholar] [CrossRef] [PubMed]
- Arima, H.; Yunomae, K.; Miyake, K.; Irie, T.; Hirayama, F.; Uekama, K. Comparative Studies of the Enhancing Effects of Cyclodextrins on the Solubility and Oral Bioavailability of Tacrolimus in Rats. J. Pharm. Sci. 2001, 90, 690–701. [Google Scholar] [CrossRef] [PubMed]
- Mahmoudi, A.; Malaekeh-Nikouei, B.; Hanafi-Bojd, M.Y.; Toloei, M.; Hosseini, M.; Nikandish, M. Preliminary In Vivo Safety Evaluation of a Tacrolimus Eye Drop Formulation Using Hydroxypropyl Beta Cyclodextrin After Ocular Administration in NZW Rabbits. Clin. Ophthalmol. 2020, 14, 947–953. [Google Scholar] [CrossRef] [Green Version]
- Loftsson, T.; Björnsdóttir, S.; Pálsdóttir, G.; Bodor, N. The effects of 2-hydroxypropyl-β-cyclodextrin on the solubility and stability of chlorambucil and melphalan in aqueous solution. Int. J. Pharm. 1989, 57, 63–72. [Google Scholar] [CrossRef]
- European Medicines Agency (EMA). Cyclodextrins Used as Excipients. Available online: https://www.ema.europa.eu/en/cyclodextrins (accessed on 17 December 2020).
- Chauvin, L. INDOCOLLYRE 0,1% collyre sol en récipient unidose. Available online: https://www.vidal.fr/medicaments/indocollyre-0-1-collyre-sol-en-recipient-unidose-8613.html (accessed on 21 January 2021).
- Anguiano-Igea, S.; Otero-Espinar, F.; Vila-Jato, J.; Blanco-Méndez, J. Interaction of clofibrate with cyclodextrin in solution; Phase solubility, 1H NMR and molecular modelling studies. Eur. J. Pharm. Sci. 1997, 5, 215–221. [Google Scholar] [CrossRef]
- Higuchi, T.; Connors, K.; Connors, S. Phase Solubility Techniques. Available online: https://www.scienceopen.com/document?vid=76f1d8c7-413c-40f2-aa7f-227482d5d1ad (accessed on 17 November 2020).
- Q2 (R1) Validation of Analytical Procedures: Text and Methodology. Available online: https://www.fda.gov/regulatory-information/search-fda-guidance-documents/q2-r1-validation-analytical-procedures-text-and-methodology (accessed on 21 January 2021).
- Mayer, M.; Meyer, B. Mapping the Active Site of Angiotensin-Converting Enzyme by Transferred NOE Spectroscopy. J. Med. Chem. 2000, 43, 2093–2099. [Google Scholar] [CrossRef]
- FDA BSS® Sterile Irrigating Solution (Balanced Salt Solution). Available online: https://dailymed.nlm.nih.gov/dailymed/fda/fdaDrugXsl.cfm?setid=4bd4d59c-eb3b-4a5e-9eb7-ae95b0a92bea&type=display (accessed on 9 December 2020).
- AEMPS Ficha Técnica Liquifilm®. Available online: https://cima.aemps.es/cima/pdfs/es/ft/60226/FT_60226.pdf (accessed on 21 January 2021).
- Zanjani, H.; Aminifard, M.N.; Ghafourian, A.; Pourazizi, M.; Maleki, A.; Arish, M.; Shahrakipoor, M.; Rohani, M.R.; Abrishami, M.; Zare, E.K.; et al. Comparative Evaluation of Tacrolimus Versus Interferon Alpha-2b Eye Drops in the Treatment of Vernal Keratoconjunctivitis. Cornea 2017, 36, 675–678. [Google Scholar] [CrossRef]
- Fukushima, A.; Ohashi, Y.; Ebihara, N.; Uchio, E.; Okamoto, S.; Kumagai, N.; Shoji, J.; Takamura, E.; Nakagawa, Y.; Namba, K.; et al. Therapeutic effects of 0.1% tacrolimus eye drops for refractory allergic ocular diseases with proliferative lesion or corneal involvement. Br. J. Ophthalmol. 2014, 98, 1023–1027. [Google Scholar] [CrossRef]
- Macy, R. Surface tension by the ring method. Applicability of the du Nouy apparatus. J. Chem. Educ. 1935, 12, 573. [Google Scholar] [CrossRef]
- Cox, C.H. Squeeze Force Measuring System. Patent US007441468B2, 28 October 2008. Available online: https://patentimages.storage.googleapis.com/b3/43/bc/d55228f30c3e35/US7441468.pdf (accessed on 21 January 2021).
- Díaz-Tomé, V.D.; García-Otero, X.; Blanco-Fernández, G.; Fernández-Ferreiro, A.; Otero-Espinar, F.J.; Varela-Fernández, R. In Vitro and in Vivo Ophthalmic Bioadhesion and Ocular Safety Characterization of Cyclodextrin Based Solution. The 1st In-ternational Electronic Conference on Pharmaceutics session Cyclodextrins in Pharmaceutics. Conf. Online 2020. [Google Scholar] [CrossRef]
- Salem, H.; Katz, S.A.; Katz, S.A. Alternative Toxicological Methods; CRC Press: Boca Ratón, FL, USA, 2003; ISBN 978-0-429-21420-2. [Google Scholar]
- Eskes, C.; Bessou, S.; Bruner, L.; Curren, R.; Harbell, J.; Jones, P.; Kreiling, R.; Liebsch, M.; McNamee, P.; Pape, W.; et al. 1 Subgroup 3. Eye Irritation. Available online: /paper/1-Subgroup-3-.-Eye-Irritation-Eskes-Bessou/6dc8084ae36aec2ab4ca59586e230776bafd8f5d (accessed on 15 November 2020).
- Fernández-Ferreiro, A.; Santiago-Varela, M.; Gil-Martínez, M.; González-Barcia, M.; Luaces-Rodríguez, A.; Díaz-Tome, V.; Pardo, M.; Blanco-Méndez, J.; Piñeiro-Ces, A.; Rodríguez-Ares, M.T.; et al. In VitroEvaluation of the Ophthalmic Toxicity Profile of Chlorhexidine and Propamidine Isethionate Eye Drops. J. Ocul. Pharmacol. Ther. 2017, 33, 202–209. [Google Scholar] [CrossRef] [PubMed]
- Spielmann, H.; Kalweit, S.; Liebsch, M.; Wirnsberger, T.; Gerner, I.; Bertram-Neis, E.; Krauser, K.; Kreiling, R.; Miltenburger, H.; Pape, W.; et al. Validation study of alternatives to the Draize eye irritation test in Germany: Cytotoxicity testing and HET-CAM test with 136 industrial chemicals. Toxicol. Vitr. 1993, 7, 505–510. [Google Scholar] [CrossRef]
- Kalweit, S.; Besoke, R.; Gerner, I.; Spielmann, H. A national validation project of alternative methods to the Draize rabbit eye test. Toxicol. Vitr. 1990, 4, 702–706. [Google Scholar] [CrossRef]
- Lund, W. The Pharmaceutical CODEX: Principles & Practice of Pharmaceutics; 12e (HB); CBS Publishers & Distributors: DaRyaganj, New Delhi, India, 2009; ISBN 978-81-239-1650-7. [Google Scholar]
- The Association for Research in Vision and Ophthalmology Statement for the Use of Animals in Ophthalmic and Visual Research. Available online: http://www.arvo.org/About_ARVO/Policies/Statement_for_the_Use_of_Animals_in_Ophthalmic_and_Visual_Research/ (accessed on 21 January 2021).
- National Research Council (US) Committee for the Update of the Guide for the Care and Use of Laboratory Animals. Guide for the Care and Use of Laboratory Animals, 8th ed.; The National Academies Collection: Reports funded by National Institutes of Health; National Academies Press (US): Washington, DC, USA, 2011; ISBN 978-0-309-15400-0.
- Fernández-Ferreiro, A.; Silva-Rodríguez, J.; Otero-Espinar, F.J.; González-Barcia, M.; Lamas, M.J.; Ruibal, A.; Luaces-Rodriguez, A.; Vieites-Prado, A.; Moreira, T.S.; Herranz, M.; et al. Positron Emission Tomography for the Development and Characterization of Corneal Permanence of Ophthalmic Pharmaceutical Formulations. Investig. Opthalmology Vis. Sci. 2017, 58, 772–780. [Google Scholar]
- Castro-Balado, A.; Mondelo-García, C.; González-Barcia, M.; Zarra-Ferro, I.; Otero-Espinar, F.J.; Ruibal, Á.; Aguiar, P.; Fernández-Ferreiro, A. Ocular Biodistribution Studies Using Molecular Imaging. Pharmaceutics 2019, 11, 237. [Google Scholar] [CrossRef] [Green Version]
- Burden, N.; Aschberger, K.; Chaudhry, Q.; Clift, M.J.D.; Doak, S.H.; Fowler, P.; Johnston, H.J.; Landsiedel, R.; Rowland, J.; Stone, V. The 3Rs as a framework to support a 21st century approach for nanosafety assessment. Nano Today 2017, 12, 10–13. [Google Scholar] [CrossRef]
- Loening, A.M.; Gambhir, S.S. AMIDE: A Free Software Tool for Multimodality Medical Image Analysis. Mol. Imaging 2003, 2, 131–137. [Google Scholar] [CrossRef]
- Meyer, B.; Peters, T. NMR Spectroscopy Techniques for Screening and Identifying Ligand Binding to Protein Receptors. Angew. Chem. Int. Ed. 2003, 42, 864–890. [Google Scholar] [CrossRef]
- Furukawa, A.; Konuma, T.; Yanaka, S.; Sugase, K. Quantitative analysis of protein–ligand interactions by NMR. Prog. Nucl. Magn. Reson. Spectrosc. 2016, 96, 47–57. [Google Scholar] [CrossRef] [PubMed]
- Saokham, P.; Muankaew, C.; Jansook, P.; Loftsson, T. Solubility of Cyclodextrins and Drug/Cyclodextrin Complexes. Molecules 2018, 23, 1161. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Baranowski, P.; Karolewicz, B.; Gajda, M.; Pluta, J. Ophthalmic Drug Dosage Forms: Characterisation and Research Methods. Sci. World J. 2014, 2014, 1–14. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Dutescu, R.M.; Panfil, C.; Schrage, N. Osmolarity of Prevalent Eye Drops, Side Effects, and Therapeutic Approaches. Cornea 2015, 34, 560–566. [Google Scholar] [CrossRef] [PubMed]
- Dabrowski, H.P.; Salpekar, A.; Jr, O.W.L. Ophthalmic Solution for Artificial Tears 1997. Patent US005591426A, 7 January 1997. Available online: https://patentimages.storage.googleapis.com/6e/1b/c3/0718a34b45e98c/US5591426.pdf (accessed on 21 January 2021).
- Nagyová, B.; Tiffany, J. Components responsible for the surface tension of human tears. Curr. Eye Res. 1999, 19, 4–11. [Google Scholar] [CrossRef] [PubMed]
- Han, K.; Woghiren, O.E.; Priefer, R. Surface tension examination of various liquid oral, nasal, and ophthalmic dosage forms. Chem. Central. J. 2016, 10, 31. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Connor, A.J.; Severn, P.S. Force requirements in topical medicine use—the squeezability factor. Eye 2011, 25, 466–469. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Van Santvliet, L.; Ludwig, A. Determinants of eye drop size. Surv. Ophthalmol. 2004, 49, 197–213. [Google Scholar] [CrossRef]
- Luechtefeld, T.; Maertens, A.; Russo, D.P.; Rovida, C.; Zhu, H.; Hartung, T. Analysis of Draize eye irritation testing and its prediction by mining publicly available 2008-2014 REACH data. ALTEX-Altern. Animal Exp. 2016, 33, 123–134. [Google Scholar] [CrossRef] [Green Version]
- Balls, M.; Botham, P.; Bruner, L.; Spielmann, H. The EC/HO international validation study on alternatives to the draize eye irritation test. Toxicol. Vitr. 1995, 9, 871–929. [Google Scholar] [CrossRef]
- Christian, M.S.; Diener, R.M. Soaps and Detergents: Alternatives to Animal Eye Irritation Tests. J. Am. Coll. Toxicol. 1996, 15, 1–44. [Google Scholar] [CrossRef]
- Chamberlain, M.; Gad, S.; Gautheron, P.; Prinsen, M. Irag Working Group 1: Organotypic models for the assessment/prediction of ocular irritation. Food Chem. Toxicol. 1997, 35, 23–37. [Google Scholar] [CrossRef]
- Garnero, C.; Zoppi, A.; Aloisio, C.; Longhi, M.R. Chapter 7-Technological delivery systems to improve biopharmaceutical properties. In Nanoscale Fabrication, Optimization, Scale-Up and Biological Aspects of Pharmaceutical Nanotechnology; Grumezescu, A.M., Ed.; William Andrew Publishing: Norwich, NY, USA, 2018; pp. 253–299. ISBN 978-0-12-813629-4. [Google Scholar]
- Campos, M.S.T.; Fialho, S.L.; Pereira, B.G.; Yoshida, M.I.; De Oliveira, M.A. Kinetics studies of the degradation of sirolimus in solid state and in liquid medium. J. Therm. Anal. Calorim. 2017, 130, 1653–1661. [Google Scholar] [CrossRef]
- Thompson, A.C.; Thompson, M.O.; Young, D.L.; Lin, R.C.; Sanislo, S.R.; Moshfeghi, D.M.; Singh, K. Barriers to Follow-Up and Strategies to Improve Adherence to Appointments for Care of Chronic Eye Diseases. Investig. Opthalmology Vis. Sci. 2015, 56, 4324–4331. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Peppas, N.A.; Mongia, N.K. Ultrapure poly (vinyl alcohol) hydrogels with mucoadhesive drug delivery characteristics. Eur. J. Pharm. Biopharm. 1997, 43, 51–58. [Google Scholar] [CrossRef]
















| Formulation | Composition | ||
|---|---|---|---|
| HPβCD (w/v, %) | Tacrolimus (w/v, %) | Vehicles | |
| TBS 20 | 20 | 0.01 | BSS® |
| TLI 20 | 20 | 0.01 | Liquifilm® |
| TBS 40 | 40 | 0.02 | BSS® |
| TLI 40 | 40 | 0.02 | Liquifilm® |
| REF | - | 0.03 | Liquifilm® |
| Formulations | pH | Osmolality (mOsm/kg) | Surface Tension (mN/m) | |||
|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | Mean | SD | |
| TBS 20 | 7.036 | 0.021 | 359.3 | 5.86 | 54.63 | 0.93 |
| TLI 20 | 6.986 | 0.005 | 283.6 | 2.52 | 58.46 | 1.10 |
| TBS 40 | 7.203 | 0.005 | 628 | 6.93 | 51.5 | 0.61 |
| TLI 40 | 6.933 | 0.005 | 383 | 18.08 | 58.43 | 0.21 |
| REF | 7.3 | 0.014 | 1220.5 | 18.57 | 47.5 | 0.2 |
| Formulations | Storage Condition | K (days−1) | t90 (days) | R2 | |||
|---|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | Mean | SD | ||
| TBS 40 | Refrigeration (4 °C) | 0.0006 | 4.3 × 10−5 | 184.32 | 13.5 | 0.8890 | 0.0179 |
| Room temperature (25 °C) | 0.0067 | 0.0002 | 15.72 | 0.53 | 0.9645 | 0.0057 | |
| Oven temperature (40 °C) | 0.0713 | 0.0016 | 1.48 | 0.03 | 0.9966 | 0.0012 | |
| TLI 40 | Refrigeration (4 °C) | 0.0011 | 5.8 × 10−5 | 98.50 | 5.2 | 0.9410 | 0.040 |
| Room temperature (25 °C) | 0.0067 | 0.0002 | 15.66 | 0.40 | 0.9867 | 0.0035 | |
| Oven temperature (40 °C) | 0.0577 | 0.0004 | 1.82 | 0.01 | 0.9959 | 0.0007 | |
| Formulations | K (min−1) | t1/2 (min) | AUC0∞ (% × min) | MRT (min) | Remaining Formulation at 75 min (%) | |||||
|---|---|---|---|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | Mean | SD | Mean | SD | Mean | SD | |
| TBS 20 | 0.014 | 0.003 | 49.70 | 10.34 | 74.96 | 7.70 | 72.90 | 6.02 | 31.99 | 12.79 |
| TLI 20 | 0.025 | 0.008 | 29.40 | 8.51 | 59.16 | 11.18 | 73.94 | 22.62 | 17.79 | 3.74 |
| TBS 40 | 0.024 | 0.023 | 61.79 | 46.16 | 89.61 | 57.41 | 76.43 | 35.70 | 57.46 | 19.65 |
| TLI 40 | 0.011 | 0.007 | 86.22 | 38.93 | 123.31 | 51.18 | 90.51 | 17.67 | 78.82 | 11.15 |
| REF | 0.018 | 0.010 | 46.34 | 22.88 | 82.22 | 30.2 | 93.28 | 37.55 | 27.44 | 15.65 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
García-Otero, X.; Díaz-Tomé, V.; Varela-Fernández, R.; Martín-Pastor, M.; González-Barcia, M.; Blanco-Méndez, J.; Mondelo-García, C.; Bermudez, M.A.; Gonzalez, F.; Aguiar, P.; et al. Development and Characterization of a Tacrolimus/Hydroxypropyl-β-Cyclodextrin Eye Drop. Pharmaceutics 2021, 13, 149. https://doi.org/10.3390/pharmaceutics13020149
García-Otero X, Díaz-Tomé V, Varela-Fernández R, Martín-Pastor M, González-Barcia M, Blanco-Méndez J, Mondelo-García C, Bermudez MA, Gonzalez F, Aguiar P, et al. Development and Characterization of a Tacrolimus/Hydroxypropyl-β-Cyclodextrin Eye Drop. Pharmaceutics. 2021; 13(2):149. https://doi.org/10.3390/pharmaceutics13020149
Chicago/Turabian StyleGarcía-Otero, Xurxo, Victoria Díaz-Tomé, Rubén Varela-Fernández, Manuel Martín-Pastor, Miguel González-Barcia, José Blanco-Méndez, Cristina Mondelo-García, Maria A. Bermudez, Francisco Gonzalez, Pablo Aguiar, and et al. 2021. "Development and Characterization of a Tacrolimus/Hydroxypropyl-β-Cyclodextrin Eye Drop" Pharmaceutics 13, no. 2: 149. https://doi.org/10.3390/pharmaceutics13020149