Co-Amorphization of Kanamycin with Amino Acids Improves Aerosolization
Abstract
:1. Introduction
2. Materials and Methods
2.1. Materials
2.2. Preparation of Spray-Dried Formulations
2.3. Powder X-ray Diffraction (PXRD)
2.4. Thermogravimetric Analysis (TGA)
2.5. Modulated Differential Scanning Calorimetry (MDSC)
2.6. Attenuated Total Reflectance-Fourier Transform Infrared (ATR-FTIR) Spectroscopy
2.7. Low-Frequency Raman (LFR) Spectroscopy
2.8. Computational Details
2.9. Scanning Electron Microscopy (SEM)
2.10. In-Vitro Aerosolization Study
2.11. High-Performance Liquid Chromatography (HPLC) Analysis
2.12. Stability Study
2.13. Statistical Analysis
2.14. Principal Component Analysis (PCA)
3. Results and Discussion
3.1. Preparation of the Spray-Dried Formulations
3.2. Characterization of the Spray-Dried Formulations
3.2.1. Amorphicity of the Formulations
3.2.2. Water Content
3.2.3. Determination of the Glass Transition Temperature (Tg)
3.2.4. Spectroscopic Assessment of Co-Amorphous Formulations
3.2.5. Particle Morphology and Size
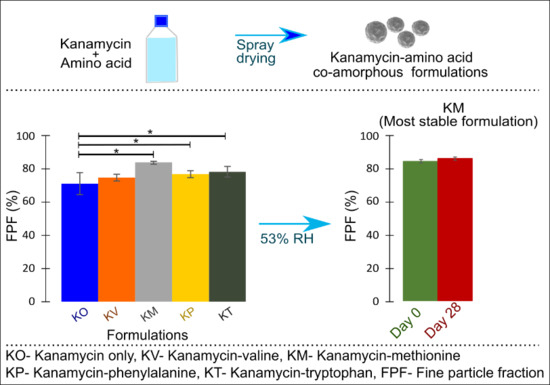
3.2.6. In-Vitro Aerosolization
3.3. Stability Study
4. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Das, S.; Tucker, I.; Stewart, P. Inhaled dry powder formulations for treating tuberculosis. Curr. Drug Deliv. 2015, 12, 26–39. [Google Scholar] [CrossRef]
- Sanders, M. Pulmonary Drug Delivery: An Historical Overview. In Controlled Pulmonary Drug Delivery; Smyth, H.D.C., Hickey, A.J., Eds.; Springer: New York, NY, USA, 2011; pp. 51–73. [Google Scholar]
- Ramsey, B.W.; Dorkin, H.L.; Eisenberg, J.D.; Gibson, R.L.; Harwood, I.R.; Kravitz, R.M.; Schidlow, D.V.; Wilmott, R.W.; Astley, S.J.; McBurnie, M.A.; et al. Efficacy of Aerosolized Tobramycin in Patients with Cystic Fibrosis. N. Engl. J. Med. 1993, 328, 1740–1746. [Google Scholar] [CrossRef]
- Wang, Y.-B.; Watts, A.B.; Peters, J.I.; Liu, S.; Batra, A.; Williams, R.O., III. In vitro and in vivo performance of dry powder inhalation formulations: Comparison of particles prepared by thin film freezing and micronization. AAPS PharmSciTech 2014, 15, 981–993. [Google Scholar] [CrossRef] [Green Version]
- Hou, S.; Wu, J.; Li, X.; Shu, H. Practical, regulatory and clinical considerations for development of inhalation drug products. Asian J. Pharm. Sci. 2015, 10, 490–500. [Google Scholar] [CrossRef] [Green Version]
- Claus, S.; Weiler, C.; Schiewe, J.; Friess, W. How can we bring high drug doses to the lung? Eur. J. Pharm. Biopharm. 2014, 86, 1–6. [Google Scholar] [CrossRef]
- Lee, H.-G.; Kim, D.-W.; Park, C.-W. Dry powder inhaler for pulmonary drug delivery: Human respiratory system, approved products and therapeutic equivalence guideline. J. Pharm. Investig. 2018, 48, 603–616. [Google Scholar] [CrossRef]
- Gaspar, M.C.; Pais, A.A.C.C.; Sousa, J.J.S.; Brillaut, J.; Olivier, J.C. Development of levofloxacin-loaded PLGA microspheres of suitable properties for sustained pulmonary release. Int. J. Pharm. 2019, 556, 117–124. [Google Scholar] [CrossRef]
- Zellnitz, S.; Pinto, J.T.; Brunsteiner, M.; Schroettner, H.; Khinast, J.; Paudel, A. Tribo-Charging Behaviour of Inhalable Mannitol Blends with Salbutamol Sulphate. Pharm. Res. 2019, 36, 80. [Google Scholar] [CrossRef] [Green Version]
- Emmett, P.C.; Aitken, R.J.; Hannan, W.J. Measurements of the total and regional deposition of inhaled particles in the human respiratory tract. J. Aerosol Sci. 1982, 13, 549–560. [Google Scholar] [CrossRef]
- Sosnik, A.; Seremeta, K.P. Advantages and challenges of the spray-drying technology for the production of pure drug particles and drug-loaded polymeric carriers. Adv. Colloid Interface Sci. 2015, 223, 40–54. [Google Scholar] [CrossRef] [PubMed]
- Li, H.Y.; Neill, H.; Innocent, R.; Seville, P.; Williamson, I.; Birchall, J.C. Enhanced dispersibility and deposition of spray-dried powders for pulmonary gene therapy. J. Drug Target. 2003, 11, 425–432. [Google Scholar] [CrossRef] [PubMed]
- Parlati, C.; Colombo, P.; Buttini, F.; Young, P.M.; Adi, H.; Ammit, A.J.; Traini, D. Pulmonary Spray Dried Powders of Tobramycin Containing Sodium Stearate to Improve Aerosolization Efficiency. Pharm. Res. 2009, 26, 1084–1092. [Google Scholar] [CrossRef] [PubMed]
- Eedara, B.B.; Tucker, I.G.; Das, S.C. Phospholipid-based pyrazinamide spray-dried inhalable powders for treating tuberculosis. Int. J. Pharm. 2016, 506, 174–183. [Google Scholar] [CrossRef]
- Pilcer, G.; Amighi, K. Formulation strategy and use of excipients in pulmonary drug delivery. Int. J. Pharm. 2010, 392, 1–19. [Google Scholar] [CrossRef]
- Singh, R.H.; Rohr, F.; Frazier, D.; Cunningham, A.; Mofidi, S.; Ogata, B.; Splett, P.L.; Moseley, K.; Huntington, K.; Acosta, P.B.; et al. Recommendations for the nutrition management of phenylalanine hydroxylase deficiency. Genet. Med. 2014, 16, 121–131. [Google Scholar] [CrossRef] [Green Version]
- Li, L.; Leung, S.S.Y.; Gengenbach, T.; Yu, J.; Gao, G.; Tang, P.; Zhou, Q.; Chan, H.-K. Investigation of L-leucine in reducing the moisture-induced deterioration of spray-dried salbutamol sulfate power for inhalation. Int. J. Pharm. 2017, 530, 30–39. [Google Scholar] [CrossRef]
- Momin, M.A.M.; Sinha, S.; Tucker, I.G.; Doyle, C.; Das, S.C. Dry powder formulation of kanamycin with enhanced aerosolization efficiency for drug-resistant tuberculosis. Int. J. Pharm. 2017, 528, 107–117. [Google Scholar] [CrossRef]
- Chew, N.Y.K.; Shekunov, B.Y.; Tong, H.H.Y.; Chow, A.H.L.; Savage, C.; Wu, J.; Chan, H.-K. Effect of Amino Acids on the Dispersion of Disodium Cromoglycate Powders. J. Pharm. Sci. 2005, 94, 2289–2300. [Google Scholar] [CrossRef]
- Li, H.Y.; Seville, P.C.; Williamson, I.J.; Birchall, J.C. The use of amino acids to enhance the aerosolisation of spray-dried powders for pulmonary gene therapy. J. Gene Med. 2005, 7, 343–353. [Google Scholar] [CrossRef]
- Lu, W.; Rades, T.; Rantanen, J.; Chan, H.K.; Yang, M. Amino acids as stabilizers for spray-dried simvastatin powder for inhalation. Int. J. Pharm. 2019, 572, 118724. [Google Scholar] [CrossRef]
- Lu, W.; Rades, T.; Rantanen, J.; Yang, M. Inhalable co-amorphous budesonide-arginine dry powders prepared by spray drying. Int. J. Pharm. 2019, 565, 1–8. [Google Scholar] [CrossRef]
- Seville, P.C.; Learoyd, T.P.; Li, H.Y.; Williamson, I.J.; Birchall, J.C. Amino acid-modified spray-dried powders with enhanced aerosolisation properties for pulmonary drug delivery. Powder Technol. 2007, 178, 40–50. [Google Scholar] [CrossRef]
- Yang, X.-F.; Xu, Y.; Qu, D.-S.; Li, H.-Y. The influence of amino acids on aztreonam spray-dried powders for inhalation. Asian J. Pharm. Sci. 2015, 10, 541–548. [Google Scholar] [CrossRef] [Green Version]
- Löbmann, K.; Grohganz, H.; Laitinen, R.; Strachan, C.; Rades, T. Amino acids as co-amorphous stabilizers for poorly water soluble drugs—Part 1: Preparation, stability and dissolution enhancement. Eur. J. Pharm. Biopharm. 2013, 85, 873–881. [Google Scholar] [CrossRef]
- Kasten, G.; Löbmann, K.; Grohganz, H.; Rades, T. Co-former selection for co-amorphous drug-amino acid formulations. Int. J. Pharm. 2019, 557, 366–373. [Google Scholar] [CrossRef]
- Belotti, S.; Rossi, A.; Colombo, P.; Bettini, R.; Rekkas, D.; Politis, S.; Colombo, G.; Balducci, A.G.; Buttini, F. Spray-dried amikacin sulphate powder for inhalation in cystic fibrosis patients: The role of ethanol in particle formation. Eur. J. Pharm. Biopharm. 2015, 93, 165–172. [Google Scholar] [CrossRef]
- Ji, S.; Thulstrup, P.W.; Mu, H.; Hansen, S.H.; van de Weert, M.; Rantanen, J.; Yang, M. Effect of ethanol as a co-solvent on the aerosol performance and stability of spray-dried lysozyme. Int. J. Pharm. 2016, 513, 175–182. [Google Scholar] [CrossRef]
- Vehring, R. Pharmaceutical particle engineering via spray drying. Pharm. Res. 2008, 25, 999–1022. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jensen, K.T.; Löbmann, K.; Rades, T.; Grohganz, H. Improving co-amorphous drug formulations by the addition of the highly water soluble amino Acid, proline. Pharmaceutics 2014, 6, 416–435. [Google Scholar] [CrossRef]
- Pommie, C.; Levadoux, S.; Sabatier, R.; Lefranc, G.; Lefranc, M.P. IMGT standardized criteria for statistical analysis of immunoglobulin V-REGION amino acid properties. J. Mol. Recognit. 2004, 17, 17–32. [Google Scholar] [CrossRef]
- Matveev, Y.I.; Grinberg, V.Y.; Sochava, I.V.; Tolstoguzov, V.B. Glass transition temperature of proteins. Calculation based on the additive contribution method and experimental data. Food Hydrocoll. 1997, 11, 125–133. [Google Scholar] [CrossRef]
- Gordon, M.; Taylor, J.S. Ideal copolymers and the second-order transitions of synthetic rubbers. i. non-crystalline copolymers. J. Appl. Chem. 1952, 2, 493–500. [Google Scholar] [CrossRef]
- Kissi, E.O.; Kasten, G.; Lobmann, K.; Rades, T.; Grohganz, H. The Role of Glass Transition Temperatures in Coamorphous Drug-Amino Acid Formulations. Mol. Pharm. 2018, 15, 4247–4256. [Google Scholar] [CrossRef]
- Berlin, E.; Pallansch, M.J. Densities of several proteins and L-amino acids in the dry state. J. Phys. Chem. 1968, 72, 1887–1889. [Google Scholar] [CrossRef]
- Bērziņš, K.; Fraser-Miller, S.J.; Rades, T.; Gordon, K.C. Low-Frequency Raman Spectroscopic Study on Compression-Induced Destabilization in Melt-Quenched Amorphous Celecoxib. Mol. Pharm. 2019, 16, 3678–3686. [Google Scholar] [CrossRef] [PubMed]
- Menges, F. Spectragryph—Optical Spectroscopy Software. Available online: http://www.effemm2.de/spectragryph/ (accessed on 25 July 2018).
- Dovesi, R.; Orlando, R.; Erba, A.; Zicovich-Wilson, C.M.; Civalleri, B.; Casassa, S.; Maschio, L.; Ferrabone, M.; De La Pierre, M.; D’Arco, P.; et al. CRYSTAL14: A program for the ab initio investigation of crystalline solids. Int. J. Quantum Chem. 2014, 114, 1287–1317. [Google Scholar] [CrossRef]
- Becke, A.D. A new mixing of Hartree–Fock and local density-functional theories. J. Chem. Phys. 1993, 98, 1372–1377. [Google Scholar] [CrossRef]
- Grimme, S. Semiempirical GGA-type density functional constructed with a long-range dispersion correction. J. Comput. Chem. 2006, 27, 1787–1799. [Google Scholar] [CrossRef]
- Heyd, J.; Peralta, J.E.; Scuseria, G.E.; Martin, R.L. Energy band gaps and lattice parameters evaluated with the Heyd-Scuseria-Ernzerhof screened hybrid functional. J. Chem. Phys. 2005, 123, 174101. [Google Scholar] [CrossRef]
- Nada, R.; Catlow, C.R.A.; Pisani, C.; Orlando, R. An ab-initio Hartree-Fock perturbed-cluster study of neutral defects in LiF. Modell. Simul. Mater. Sci. Eng. 1993, 1, 165–187. [Google Scholar] [CrossRef]
- Puius, Y.A.; Stievater, T.H.; Srikrishnan, T. Crystal structure, conformation, and absolute configuration of kanamycin A. Carbohydr. Res. 2006, 341, 2871–2875. [Google Scholar] [CrossRef] [PubMed]
- Ferrero, M.; Rérat, M.; Orlando, R.; Dovesi, R. Coupled perturbed Hartree-Fock for periodic systems: The role of symmetry and related computational aspects. J. Chem. Phys. 2008, 128, 014110. [Google Scholar] [CrossRef] [PubMed]
- Marple, V.A.; Roberts, D.L.; Romay, F.J.; Miller, N.C.; Truman, K.G.; Van Oort, M.; Olsson, B.; Holroyd, M.J.; Mitchell, J.P.; Hochrainer, D. Next Generation Pharmaceutical Impactor (A New Impactor for Pharmaceutical Inhaler Testing). Part I: Design. J. Aerosol Med. 2003, 16, 283–299. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Brunaugh, A.D.; Wu, T.; Kanapuram, S.R.; Smyth, H.D.C. Effect of Particle Formation Process on Characteristics and Aerosol Performance of Respirable Protein Powders. Mol. Pharm. 2019, 16, 4165–4180. [Google Scholar] [CrossRef]
- Kim, B.H.; Kim, Y.K.; Ok, J.H. Development of liquid chromatographic method for the analysis of kanamycin residues in varicella vaccine using phenylisocyanate as a derivatization reagent. J. Chromatogr. B Biomed. Sci. Appl. 2001, 752, 173–177. [Google Scholar] [CrossRef]
- Greenspan, L. Humidity Fixed Points of Binary Saturated Aqueous Solutions. J. Res. Natl. Bur. Stand. Sect. A Phys. Chem. 1977, 81, 89–96. [Google Scholar] [CrossRef]
- Signorell, A.; Aho, K.; Alfons, A.; Anderegg, N.; Aragon, T.; Arppe, A. DescTools: Tools for Descriptive Statistics. R Package Version 0.99.34. 2020. Available online: http://cran.r-project.org/package=DescTools (accessed on 29 July 2020).
- Team, R. RStudio: Integrated Development for R; RStudio, Inc.: Boston, MA, USA, 2019. [Google Scholar]
- Zografi, G. States of Water Associated with Solids. Drug Dev. Ind. Pharm. 1988, 14, 1905–1926. [Google Scholar] [CrossRef]
- Newman, A.W.; Reutzel-Edens, S.M.; Zografi, G. Characterization of the “hygroscopic” properties of active pharmaceutical ingredients. J. Pharm. Sci. 2008, 97, 1047–1059. [Google Scholar] [CrossRef]
- Hill, V.L.; Craig, D.Q.M.; Feely, L.C. Characterisation of spray-dried lactose using modulated differential scanning calorimetry. Int. J. Pharm. 1998, 161, 95–107. [Google Scholar] [CrossRef]
- Newman, A.; Zografi, G. Commentary: Considerations in the Measurement of Glass Transition Temperatures of Pharmaceutical Amorphous Solids. AAPS PharmSciTech 2019, 21, 26. [Google Scholar] [CrossRef] [Green Version]
- Shamblin, S.L.; Taylor, L.S.; Zografi, G. Mixing Behavior of Colyophilized Binary Systems. J. Pharm. Sci. 1998, 87, 694–701. [Google Scholar] [CrossRef] [PubMed]
- Cook, D. Protonation Site in Organic Bases from Infrared X-H Deformation Modes. Can. J. Chem. 1964, 42, 2292–2299. [Google Scholar] [CrossRef]
- Turco Liveri, V.; Lombardo, D.; Pochylski, M.; Calandra, P. Molecular association of small amphiphiles: Origin of ionic liquid properties in dibutyl phosphate/propylamine binary mixtures. J. Mol. Liq. 2018, 263, 274–281. [Google Scholar] [CrossRef]
- Coates, J. Interpretation of Infrared Spectra, A Practical Approach. In Encyclopedia of Analytical Chemistry; Meyers, R.A., Mckelvy, M.L., Eds.; John Wiley & Sons Ltd: Hoboken, NJ, USA, 2006. [Google Scholar]
- Allen, D.T.; Palen, E.J.; Haimov, M.I.; Hering, S.V.; Young, J.R. Fourier Transform Infrared Spectroscopy of Aerosol Collected in a Low Pressure Impactor (LPI/FTIR): Method Development and Field Calibration. Aerosol Sci. Technol. 1994, 21, 325–342. [Google Scholar] [CrossRef]
- Cao, X.; Fischer, G. Infrared Spectral, Structural, and Conformational Studies of Zwitterionic l-Tryptophan. J. Phys. Chem. A 1999, 103, 9995–10003. [Google Scholar] [CrossRef]
- Mah, P.T.; Fraser, S.J.; Reish, M.E.; Rades, T.; Gordon, K.C.; Strachan, C.J. Use of low-frequency Raman spectroscopy and chemometrics for the quantification of crystallinity in amorphous griseofulvin tablets. Vib. Spectrosc. 2015, 77, 10–16. [Google Scholar] [CrossRef]
- Walker, G.; Römann, P.; Poller, B.; Löbmann, K.; Grohganz, H.; Rooney, J.S.; Huff, G.S.; Smith, G.P.S.; Rades, T.; Gordon, K.C.; et al. Probing Pharmaceutical Mixtures during Milling: The Potency of Low-Frequency Raman Spectroscopy in Identifying Disorder. Mol. Pharm. 2017, 14, 4675–4684. [Google Scholar] [CrossRef]
- Stuart, B.O. Deposition of Inhaled Aerosols. Arch. Intern. Med. 1973, 131, 60–73. [Google Scholar] [CrossRef]
- Crowder, T.M.; Rosati, J.A.; Schroeter, J.D.; Hickey, A.J.; Martonen, T.B. Fundamental effects of particle morphology on lung delivery: Predictions of Stokes’ law and the particular relevance to dry powder inhaler formulation and development. Pharm. Res. 2002, 19, 239–245. [Google Scholar] [CrossRef]
- Gallo, L.; Verónica Ramírez-Rigo, M.; Bucalá, V. Development of porous spray-dried inhalable particles using an organic solvent-free technique. Powder Technol. 2019, 342, 642–652. [Google Scholar] [CrossRef]
- Heyder, J.; Gebhart, J.; Roth, C.; Ferron, G.A. Transport and Deposition of Hydrophilic Drug Particles in the Lungs—Experiment and Theory. In Optimization of Aerosol Drug Delivery; Springer: The Netherlands, 2003; pp. 139–147. [Google Scholar]
- Das, S.; Larson, I.; Young, P.; Stewart, P. Surface energy changes and their relationship with the dispersibility of salmeterol xinafoate powders for inhalation after storage at high RH. Eur. J. Pharm. Sci. 2009, 38, 347–354. [Google Scholar] [CrossRef] [PubMed]
- Das, S.; Larson, I.; Young, P.; Stewart, P. Understanding lactose behaviour during storage by monitoring surface energy change using inverse gas chromatography. Dairy Sci. Technol. 2010, 90, 271–285. [Google Scholar] [CrossRef] [Green Version]
- Arora, S.; Kappl, M.; Haghi, M.; Young, P.M.; Traini, D.; Jain, S. An investigation of surface properties, local elastic modulus and interaction with simulated pulmonary surfactant of surface modified inhalable voriconazole dry powders using atomic force microscopy. RSC Adv. 2016, 6, 25789–25798. [Google Scholar] [CrossRef] [Green Version]
- Coelho, M.C.; Harnby, N. Moisture bonding in powders. Powder Technol. 1978, 20, 201–205. [Google Scholar] [CrossRef]
- Crouter, A.; Briens, L. The effect of moisture on the flowability of pharmaceutical excipients. AAPS PharmSciTech 2014, 15, 65–74. [Google Scholar] [CrossRef] [Green Version]
- Elajnaf, A.; Carter, P.; Rowley, G. The effect of relative humidity on electrostatic charge decay of drugs and excipient used in dry powder inhaler formulation. Drug Dev. Ind. Pharm. 2007, 33, 967–974. [Google Scholar] [CrossRef]







| Formulation | Kanamycin (mg) | Amino Acid (mg) | Kanamycin: Amino Acid (Molar Ratio) | Final Volume (mL) | Feed Conc. (Relative to Kanamycin) | Process Yield (%), n = 2 |
|---|---|---|---|---|---|---|
| Kanamycin only (KO) | 1500 | - | - | 750 | 0.2 | 71.9 ± 3.7 |
| Kanamycin-Valine (KV) | 1500 | 301.5 | 1:1 | 750 | 0.2 | 70.7 ± 1.3 |
| Kanamycin-Methionine (KM) | 1500 | 384.0 | 1:1 | 750 | 0.2 | 74.4 ± 5.0 |
| Kanamycin-Phenylalanine (KP) | 1500 | 425.5 | 1:1 | 750 | 0.2 | 75.2 ± 2.2 |
| Kanamycin-Tryptophan (KT) | 1500 | 526.0 | 1:1 | 750 | 0.2 | 76.8 ± 1.3 |
| Spray-Dried Particles | Water Content (%) (n = 2) | Glass Transition (°C) (n = 3) |
|---|---|---|
| Kanamycin only (KO) | 7.0 ± 0.4 | 90.7 ± 0.9 |
| Kanamycin-valine (KV) | 4.9 ± 0.1 | 89.9 ± 0.2 |
| Kanamycin-methionine (KM) | 6.0 ± 1.3 | 90.2 ± 0.4 |
| Kanamycin-phenylalanine (KP) | 4.9 ± 0.5 | 90.8 ± 2.0 |
| Kanamycin-tryptophan (KT) | 5.8 ± 0.41 | 90.65 ± 1.0 |
| Tryptophan | 128.6 ± 0.3 |
| Day 0 | Day 28—25 °C/<15% RH | Day 28—25 °C/53% RH | |||||||
|---|---|---|---|---|---|---|---|---|---|
| ED (%) | FPF (%) | RF3µm (%) | ED (%) | FPF (%) | RF3µm (%) | ED (%) | FPF (%) | RF3µm (%) | |
| KO | 66.0 ± 4.2 | 71.1 ± 6.6 | 59.5 ± 6.3 | 68.0 ± 6.8 | 66.4± 5.2 | 44.5 ± 5.3 ** | 86.2 ± 3.6 | 60.7 ± 0.7 ** | 42.6 ± 0.4 ** |
| KV | 78.0 ± 3.3 | 74.7 ± 2.0 | 66.4 ± 2.0 * | 74.1 ± 1.8 | 75.6 ± 0.6 | 66.5 ± 0.1 | 82.0 ± 4.4 | 68.1 ± 1.3 ** | 51.3 ± 1.8 ** |
| KM | 74.8 ± 1.3 | 83.9 ± 0.9 * | 73.9 ± 1.1 * | 76.1 ± 0.9 | 84.3 ± 1.6 | 74.1 ± 1.4 | 76.6 ± 2.2 | 85.6 ± 1.0 | 75.1 ± 2.8 |
| KP | 74.0 ± 3.6 | 76.8 ± 2.1 * | 68.8 ± 2.0 * | 74.8 ± 3.3 | 74.1 ± 1.0 | 65.4 ± 1.7 | 80.0 ± 4.8 | 68.2 ± 1.0 ** | 53.3 ± 0.7 ** |
| KT | 76.9 ± 2.2 | 78.2 ± 3.2 * | 69.4 ± 2.6 * | 74.5 ± 2.6 | 74.9 ± 0.9 | 66.2 ± 1.0 | 75.6 ± 2.6 | 69.9 ± 1.3 ** | 60.3 ± 1.2 ** |
| Formulation | Day 0 n = 2 | 25 °C/<15% RH (Day 28, n = 2) | 25 °C/53% RH (Day 28, n = 2) |
|---|---|---|---|
| Kanamycin only (KO) | 7.0 ± 0.4 | 8.0 ± 0.3 | 12.0 ± 0.2 |
| Kanamycin-Valine (KV) | 6.0 ± 1.3 | 6.3 ± 0.3 | 10.2 ± 0.1 |
| Kanamycin-Methionine (KM) | 4.9 ± 0.1 | 4.9 ± 0.1 | 9.7 ± 0.4 |
| Kanamycin-Phenylalanine (KP) | 4.9 ± 0.5 | 5.1 ± 0.4 | 10.2 ± 0.1 |
| Kanamycin-Tryptophan (KT) | 5.8 ± 0.41 | 5.7 ± 0.1 | 10.5 ± 0.5 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Adhikari, B.R.; Bērziņš, K.; Fraser-Miller, S.J.; Gordon, K.C.; Das, S.C. Co-Amorphization of Kanamycin with Amino Acids Improves Aerosolization. Pharmaceutics 2020, 12, 715. https://doi.org/10.3390/pharmaceutics12080715
Adhikari BR, Bērziņš K, Fraser-Miller SJ, Gordon KC, Das SC. Co-Amorphization of Kanamycin with Amino Acids Improves Aerosolization. Pharmaceutics. 2020; 12(8):715. https://doi.org/10.3390/pharmaceutics12080715
Chicago/Turabian StyleAdhikari, Bishal Raj, Kārlis Bērziņš, Sara J. Fraser-Miller, Keith C. Gordon, and Shyamal C. Das. 2020. "Co-Amorphization of Kanamycin with Amino Acids Improves Aerosolization" Pharmaceutics 12, no. 8: 715. https://doi.org/10.3390/pharmaceutics12080715