3.2.1. Pseudoternary Phase Diagrams
The surfactant applied in the preliminary phase studies was selected based on the active ingredient solubility. According to Yuan et al. [
36], among different sorbitan esters, Tween
® 85 reveals the best properties in terms of solubilizing MX. For the oil phase, relatively polar components were tested, in order to provide the best water solubilization capacity [
37].
Pseudoternary phase diagrams obtained with different oil phases and co-surfactants are presented in
Figure 5. Gray areas correspond to transparent, monophasic liquids of low viscosities identified as microemulsions, while white ones correspond to non-transparent coarse emulsions. The monophasic areas observed for the systems with triacetin (
Figure 5, 1A–1C) were larger than the corresponding ones obtained for the systems with oleic acid (
Figure 5, 2A–2C). The observed differences might be explained with different polarity of the applied oil phases. The values of log P reported for triacetin and oleic acid are −0.075 [
38] and 3.50 [
39], respectively. Lower value in the case of triacetin indicates relatively higher polarity, which results in higher water solubilization capacity. Similar results were observed by Yang et al. [
40]. On the other hand, it has been hypothesized that low molecular weight oils can partially behave as co-surfactants [
41], which might also contribute to the differences observed between the systems with triacetin and oleic acid investigated in this study.
In the next step, the differences observed between the systems containing different co-surfactants were taken into consideration. In both investigated sets, a significantly smaller monophasic area was observed for the systems containing Transcutol® P. In the case of the systems with ethanol and isopropanol, the results are similar. However, in the case of isopropanol, monophasic areas are slightly bigger. Therefore, for the further analyses, a system with triacetin as an oil phase and isopropyl alcohol as a co-surfactant was selected.
3.2.2. Conductivity Studies
Conductivity experiments were performed to assess the regions of the occurrence of particular microemulsion types. According to numerous studies [
42,
43,
44,
45], the conductivity changes observed as a result of microemulsion dilution with polar phase reflect the microstructural changes related to the transitions from one microemulsion type to another. In the initial step of the study, the observed conductivity values are close to zero, which is related to the structure and properties of water in oil (w/o) microemulsion containing isolated water droplets. The external phase in such case reveals low polarity, which is reflected by low electrical conductivity. As a result of water addition, isolated droplets start to coalesce forming polar channels which results in the transition into bicontinuous type and is reflected by the significant increase of conductivity versus water content plot slope. With further water addition, the number of channels increases which contributes to the increase of conductivity values. Finally, the bicontinuous system transforms into oil in water (o/w) microemulsion with polar external phase and electrical conductivity reaches plateau. In some cases, only a single transition point is observed and the system transforms from w/o into o/w without any discernible region corresponding to the bicontinuous system [
46,
47].
The results obtained in this study for the dilution lines L1, L2, L3 and L4 (
Figure 6) indicate the presence of only one transition point corresponding to the transformation from w/o to water-continuous systems. Similar effects have been reported for other microemulsions [
48,
49,
50].
The points corresponding to the transition from w/o to water-continuous microemulsions were obtained as intersections of the extrapolated approximately linear parts of the conductivity curve, as presented in
Figure 6. The transition points and the areas reflecting the occurrence of particular microemulsion types are depicted in
Figure 7. Based on these findings, two microemulsion compositions from both areas were selected and applied in further experiments (
Figure 7).
3.2.3. Viscosity Studies
In general, all investigated systems revealed Newtonian behavior, which is considered as typical for microemulsions [
51], except for bicontinuous systems containing intertwining polar and non-polar domains forming an internal structure that might contribute to slightly shear-thinning behavior [
52]. On the other hand, high initial viscosity of the system and highly pseudoplastic properties indicate the presence of lamellar systems which are not classified as microemulsions. It is important to notice that all analyzed systems remained liquid during the dilution and no gelation was observed. The viscosity values ranged from 10 to 28 mPa s. The plots depicting the relationship between the water content and the viscosity of microemulsions monitored along the dilution lines L1–L4 are presented in
Figure 8.
Viscosity changes observed during the dilution of microemulsion can be applied for monitoring structural transitions from one microemulsion type to another [
51]. In the initial phase of the experiment, w/o microemulsion is formed. The increase of viscosity in this case is related to the increased amount of the dispersed phase droplets which interact with each other. At about 25%–30% of water, the viscosity increases slower (L1 and L2,
Figure 8) or reaches plateau (L3 and L4). The observed effect might be related to the structural transition leading to the formation of continuous water phase. It is noteworthy that the approximate transition points observed in viscosity curves correspond to those recorded with electrical conductivity measurements.
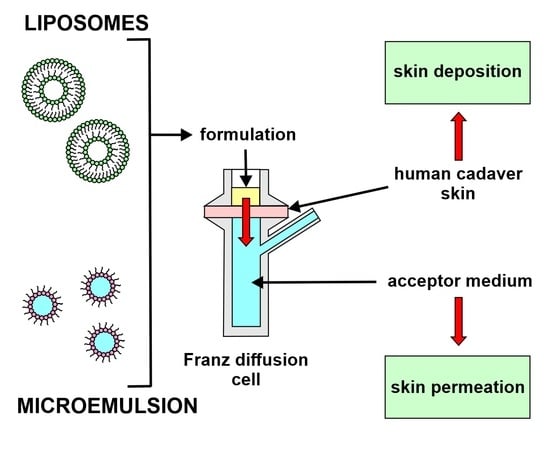
3.2.5. Drug Permeation Studies
Ex vivo skin permeation studies were conducted with both liposome and microemulsion formulations applied to human cadaver skin using Franz diffusion cells. The results of skin permeation experiments yielded plots of cumulative drug amount versus time and are presented in
Figure 11, while the values of steady state flux (J
ss) and permeability coefficients (K
p) are presented in
Table 6. Steady state flux values were calculated as a slope of the linear plots presented in
Figure 10, while permeability coefficients were calculated with the use of Equation (3) [
53]. Both parameters calculated for liposomal formulations clearly indicate that transfersomes reveal a greater ability to penetrate the skin compared to the classical non-deformable liposomes, suggesting that the deformable liposomes greatly enhanced the permeation of MX compared to the rigid vesicles. The mechanisms underlying the differences observed in this study have been described in the literature related to deformable vesicles [
54,
55,
56,
57]. The most important structural feature of transfersomes is the presence of surfactants acting as edge activators and destabilizing lipid bilayers. As a result, the modified vesicles are more flexible and susceptible to deformation than the conventional ones, which allows for more efficient penetration through the pores present in the skin. Another important factor in the permeation enhancement is osmotic gradient, which acts as a driving force pushing transfersomes from the relatively dehydrated skin surface into the deeper layers of skin. It is worth mentioning that the osmotic effect was reported as crucial in non-occlusive conditions [
58] while in this study, all samples placed in Franz diffusion cells were protected from water evaporation. Therefore, it may be hypothesized that the differences observed between conventional and deformable vesicles could be even higher in a non-occlusive environment.
where:
The drug permeation results obtained for two different microemulsions investigated in this study indicate that the effectiveness of the carrier depends on the type of microemulsion or water content in the system. In the case of o/w microemulsion, the steady state flux value is significantly higher than that in the w/o system. Similar effects have been reported by Zhang and Michniak-Kohn [
59]. It was shown that the increase of water content in the system resulted in the increased drug permeation, which was more pronounced for lipophilic drugs when compared to a hydrophilic one. However, in the case of active ingredients revealing low solubility in water, the described effect might be related to the increased thermodynamic activity of the drugs in water-rich systems.
Similar tendencies were described in the study focusing on hydrophilic caffeine [
60]. The highest flux values were observed for o/w microemulsions, while the lowest ones were recorded for oil-continuous systems. However, the authors indicated lower permeation differences observed between the particular microemulsion types than in the case of less polar actives reported in the literature. The statistically significant differences obtained in this study for two structurally different microemulsion systems can also be related to the hydrophobic character of the applied drug.
The comparison of the drug flux values calculated for different microemulsions and liposomal formulations revealed statistically significant results between the investigated formulations. According to
Figure 11, conventional liposomes displayed similar properties as w/o microemulsion, while for transfersomes and o/w microemulsion, higher flux values were obtained. Comparing the potential therapeutic utility of the investigated formulations, it may be expected that the latter two will perform better. A similar tendency was also observed for the amounts of the drug deposited in the skin (
Figure 12). The highest concentration of meloxicam in both skin layers was recorded for transfersomes, which indicated the highest ability to overcome
stratum corneum and also explained the highest concentration in the receptor medium. The amounts observed for o/w microemulsion were lower, even though the drug flux was very similar. This may indicate a higher tendency to penetrate deeper with apparently lower affinity to the dermis and epidermis. The observed effect can be explained with the composition of both systems. Transfersomes contain naturally derived phospholipids which display high biocompatibility and high affinity to skin structures. Therefore, it might be expected that higher amounts of the drug incorporated in the vesicles will be retained in the skin. On the other hand, conventional liposomes containing the same phospholipids reveal lower elasticity and ability to deform, which decreases their ability to overcome the skin barriers and stay in the skin structures. These results suggested that the transfersomes containing cationic surfactant may affect the lipids of SC and therefore produce an enhancing effect in terms of dermal drug delivery.
In the case of microemulsions, it might be hypothesized that the presence of surfactants and co-surfactants contributed to the increased ability to penetrate through the
stratum corneum into the deeper layers of the skin without binding to them, as was observed in transfersomes. However, the tendency was not the same for different types of microemulsions, which indicated the possible impact of the structural features and thermodynamic activity of the incorporated drug. It is noteworthy that the literature reports showing the comparison between microemulsions and liposomal formulations are quite scarce. According to El-Badry et al. [
61], microemulsions with two different co-surfactants revealed higher drug flux than liposomal formulations containing croconazole, a poorly water-soluble antimycotic drug. Nevertheless, the experiment was conducted with the use of an animal skin model, which might provide different results when compared to human cadaver skin. Moreover, the efficacy of microemulsion is dependent on its composition. The study presented by Yuan et al. [
36] investigating meloxicam-loaded microemulsions showed significantly higher drug flux values. However, isopropyl myristate applied as an oil phase is less polar than triacetin applied in our study, which might potentially contribute to the observed differences.
Taking into consideration the permeation coefficients calculated for all investigated formulations, it may be assumed that the observed differences are partially related to different drug content occurring mostly as a result of different encapsulation efficiency in liposomes. The highest value was obtained for transfersomes, while conventional liposomes and water-continuous microemulsion revealed similar properties. The lowest value of permeation coefficient was observed for oil-continuous microemulsion. The comparison made between two different types of vesicles confirmed the results described in the literature [
62,
63,
64]. The available studies show that transfersomes reveal better properties in terms of dermal drug delivery, which is related to higher deformability allowing for better penetration into deeper skin layers. Moreover, because of the presence of cationic surfactant, transfersomes may disrupt the organization of lipids in the
stratum corneum. Similar results, indicating that transfersomes also had higher tendency to be retained in skin when compared to conventional liposomes, were presented by Alvi et al. [
63].
Considering advantages and disadvantages of the investigated dermal delivery systems, it can be assumed that transfersomes reveal better properties as potential drug carriers, efficiently enhancing the absorption of the active ingredient. Another important feature of phospholipid-based vesicles is their high compatibility with the skin and low irritancy, which is particularly important in longer therapies requiring multiple applications. According to Mahrhauser et al. [
65], liposomes and multiple emulsions had no negative effects on the skin, while microemulsion-based formulation temporarily increased transepidermal water loss, which resulted in dehydration. The observed side effects related to microemulsion administration might be related to high surfactants and co-surfactants content. On the other hand, microemulsions are thermodynamically stable dispersions, which means that the formation process is spontaneous and does not require high amounts of energy and complicated multi-step technological processes. Therefore, several technological difficulties, such as non-uniformity, instability or high variability of the final product, can be avoided.