Effective Therapeutic Delivery and Bioavailability Enhancement of Pioglitazone Using Drug in Adhesive Transdermal Patch
Abstract
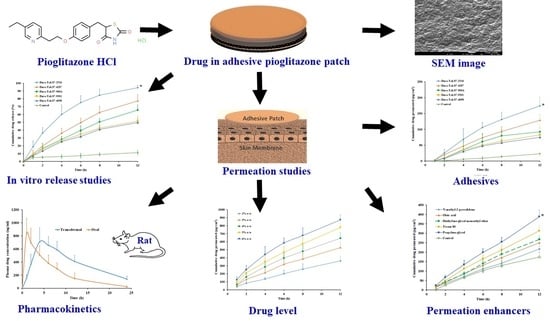
:1. Introduction
2. Materials and Methods
2.1. Materials
2.2. Estimation of Pioglitazone
2.3. Formulation of DIA Patches
2.4. Drug Content in Patch
2.5. In Vitro Release
2.6. Ex Vivo Permeation
2.7. Solubility
2.8. Scanning Electron Microscopy (SEM)
2.9. In Vivo Evaluation
2.10. Skin Irritation Study
2.11. Data Analysis
3. Results and Discussion
3.1. Formulation of DIA Patches
3.2. Assay
3.3. In Vitro Release
3.4. Effect of Adhesives
3.5. Effect of Permeation Enhancers
3.6. Solubility
3.7. SEM
3.8. Effect of Drug Content
3.9. In Vivo
3.10. Skin Irritation
4. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- World Health Organization. 2016. Available online: https://apps.who.int/iris/bitstream/handle/10665/204871/9789241565257_eng.pdf;jsessionid=4EBB5862DEF4FA1A37D4C6CE514D17FF?sequence=1 (accessed on 12 April 2019).
- Kolb, H.; Martin, S. Environmental/lifestyle factors in the pathogenesis and prevention of type 2 diabetes. BMC Med. 2017, 15, 131. [Google Scholar] [CrossRef] [PubMed]
- DeFronzo, R.A.; Triplitt, C.L.; Abdul-Ghani, M.; Cersosimo, E. Novel agents for the treatment of type 2 diabetes. Diabetes Spectr. 2014, 27, 100–112. [Google Scholar] [CrossRef] [PubMed]
- Holman, R.R. Type 2 diabetes mellitus in 2012: Optimal management of T2DM remains elusive. Nat. Rev. Endocrinol. 2013, 9, 67–68. [Google Scholar] [CrossRef] [PubMed]
- Chaudhury, A.; Duvoor, C.; Dendi, R.; Sena, V.; Kraleti, S.; Chada, A.; Ravilla, R.; Marco, A.; Shekhawat, N.S.; Montales, M.T.; et al. Clinical review of antidiabetic drugs: Implications for type 2 diabetes mellitus management. Front. Endocrinol. 2017, 8, 6. [Google Scholar] [CrossRef] [PubMed]
- Peters, A. Incretin-based therapies: Review of current clinical trial data. Am. J. Med. 2010, 123, S28–S37. [Google Scholar] [CrossRef]
- Scheen, A.J. Hepatotoxicity with thiazolidinediones: Is it a class effect? Drug Saf. 2001, 24, 873–888. [Google Scholar] [CrossRef]
- Consoli, A.; Formoso, G. Do thiazolidinediones still have a role in treatment of type 2 diabetes mellitus? Diabetes Obes. Metab. 2013, 15, 967–977. [Google Scholar] [CrossRef]
- Sinha, V.R.; Sethi, S. Pioglitazone hydrochloride: Chemopreventive potential and development of site-specific drug delivery systems. Drug Deliv. 2015, 22, 408–417. [Google Scholar] [CrossRef]
- Silva-Abreu, M.; Espinoza, L.; Halbaut, L.; Espina, M.; García, M.; Calpena, A. Comparative study of ex vivo transmucosal permeation of pioglitazone nanoparticles for the treatment of Alzheimer’s disease. Polymers 2018, 10, 316. [Google Scholar] [CrossRef]
- Silva-Abreu, M.; Calpena, A.C.; Espina, M.; Silva, A.M.; Gimeno, A.; Egea, M.A.; García, M.L. Optimization, biopharmaceutical profile and therapeutic efficacy of pioglitazone-loaded PLGA-PEG nanospheres as a novel strategy for ocular inflammatory disorders. Pharm. Res. 2018, 35, 11. [Google Scholar] [CrossRef]
- Sakai, S.; Sato, K.; Tabata, Y.; Kishi, K. Local release of pioglitazone (a peroxisome proliferator-activated receptor γ agonist) accelerates proliferation and remodeling phases of wound healing. Wound Repair Regen. 2016, 24, 24–64. [Google Scholar] [CrossRef] [PubMed]
- US FDA. 2011. Available online: https://www.fda.gov/drugs/drug-safety-and-availability/fda-drug-safety-communication-updated-fda-review-concludes-use-type-2-diabetes-medicine-pioglitazone (accessed on 19 June 2019).
- Wittayalertpanya, S.; Chompootaweep, S.; Thaworn, N. The pharmacokinetics of pioglitazone in Thai healthy subjects. J. Med. Assoc. Thai. 2006, 89, 2116–2222. [Google Scholar] [PubMed]
- Sinha, B.; Ghosal, S. Pioglitazone-do we really need it to manage type 2 diabetes? Diabetes Metab. Syndr. 2013, 7, 52–55. [Google Scholar] [CrossRef] [PubMed]
- EMA. 2004. Available online: https://www.ema.europa.eu/en/documents/scientific-discussion/actos-epar-scientific-discussion_en.pdf. (accessed on 19 June 2019).
- Gupta, A.; Nair, A.; Kumria, R.; Al-Dhubiab, B.E.; Chattopadhyaya, I.; Gupta, S. Assessment of pharmacokinetic interaction of spirulina with glitazone in a type 2 diabetes rat model. J. Med. Food. 2013, 16, 1095–1100. [Google Scholar] [CrossRef]
- Elbary, A.A.; Kassem, M.A.; Abou Samra, M.M.; Khalil, R.M. Formulation and hypoglycemic activity of pioglitazone-cyclodextrin inclusion complexes. Drug Discov. Ther. 2008, 2, 94–107. [Google Scholar]
- Singh, C.; Jain, K.A.; Kumar, C.; Agarwal, K. Design and in vitro evaluation of mucoadhesive microcapsules of pioglitazone. J. Young Pharm. 2009, 1, 195–198. [Google Scholar] [CrossRef]
- Boddupalli, B.M.; Masana, P.; Anisetti, R.N.; Kallem, S.V.; Madipoju, B. Formulation and evaluation of pioglitazone loaded bovine serum albumin nanoparticles along with piperine. Drug Invent. Today 2013, 5, 212–215. [Google Scholar] [CrossRef]
- He, W.; Li, Y.; Zhang, R.; Wu, Z.; Yin, L. Gastro-floating bilayer tablets for the sustained release of metformin and immediate release of pioglitazone: Preparation and in vitro/in vivo evaluation. Int. J. Pharm. 2014, 476, 223–231. [Google Scholar] [CrossRef]
- Hyma, P.; Abbulu, K. Formulation and characterisation of self-microemulsifying drug delivery system of pioglitazone. Biomed. Prev. Nutr. 2013, 3, 345–350. [Google Scholar] [CrossRef]
- Prausnitz, M.R.; Langer, R. Transdermal drug delivery. Nat. Biotechnol. 2008, 26, 1261–1268. [Google Scholar] [CrossRef]
- Roohnikan, M.; Laszlo, E.; Babity, S.; Brambilla, D. A snapshot of transdermal and topical drug delivery research in Canada. Pharmaceutics 2019, 11, 256. [Google Scholar] [CrossRef] [PubMed]
- Alkilani, A.; McCrudden, M.T.; Donnelly, R. Transdermal drug delivery: Innovative pharmaceutical developments based on disruption of the barrier properties of the stratum corneum. Pharmaceutics 2015, 7, 438–470. [Google Scholar] [CrossRef] [PubMed]
- Ita, K. Perspectives on transdermal electroporation. Pharmaceutics 2016, 8, 9. [Google Scholar] [CrossRef] [PubMed]
- Liao, A.H.; Ho, H.C.; Lin, Y.C.; Chen, H.K.; Wang, C.H. Effects of microbubble size on ultrasound-induced transdermal delivery of high-molecular-weight drugs. PLoS ONE 2015, 10, e0138500. [Google Scholar] [CrossRef] [PubMed]
- Ita, K. Transdermal delivery of drugs with microneedles—Potential and challenges. Pharmaceutics 2015, 7, 90–105. [Google Scholar] [CrossRef]
- Massella, D.; Leone, F.; Peila, R.; Barresi, A.; Ferri, A. Functionalization of cotton fabrics with polycaprolactone nanoparticles for transdermal release of melatonin. J. Funct. Biomater. 2018, 9, 1. [Google Scholar] [CrossRef] [PubMed]
- Nastiti, C.; Ponto, T.; Abd, E.; Grice, J.; Benson, H.; Roberts, M. Topical nano and microemulsions for skin delivery. Pharmaceutics 2017, 9, 37. [Google Scholar] [CrossRef]
- Ashtikar, M.; Nagarsekar, K.; Fahr, A. Transdermal delivery from liposomal formulations–Evolution of the technology over the last three decades. J. Control. Release 2016, 242, 126–140. [Google Scholar] [CrossRef]
- Alam, S.; Aslam, M.; Khan, A.; Imam, S.S.; Aqil, M.; Sultana, Y.; Ali, A. Nanostructured lipid carriers of pioglitazone for transdermal application: From experimental design to bioactivity detail. Drug Deliv. 2016, 23, 601–609. [Google Scholar] [CrossRef]
- Prasad, P.S.; Imam, S.S.; Aqil, M.; Sultana, Y.; Ali, A. QbD-based carbopol transgel formulation: Characterization, pharmacokinetic assessment and therapeutic efficacy in diabetes. Drug Deliv. 2016, 23, 1047–1056. [Google Scholar] [CrossRef]
- Banerjee, S.; Chattopadhyay, P.; Ghosh, A.; Datta, P.; Veer, V. Aspect of adhesives in transdermal drug delivery systems. Int. J. Adhes. Adhes. 2014, 50, 70–84. [Google Scholar] [CrossRef]
- Niharika, L.; Pragya, Y.; Vaibhav, R.; Anurag, V.; Navneet, V. Aspects of pressure sensitive adhesives in fabricating drug-in-adhesive transdermal therapeutic systems. Drug Deliv. Lett. 2017, 7, 3–15. [Google Scholar]
- Todo, H. Transdermal permeation of drugs in various animal species. Pharmaceutics 2017, 9, 33. [Google Scholar] [CrossRef] [PubMed]
- Van Ravenzwaay, B.; Leibold, E. A comparison between in vitro rat and human and in vivo rat skin absorption studies. Hum. Exp. Toxicol. 2004, 23, 421–430. [Google Scholar] [CrossRef] [PubMed]
- Nair, A.; Vyas, H.; Shah, J.; Kumar, A. Effect of permeation enhancers on the iontophoretic transport of metoprolol tartrate and the drug retention in skin. Drug Deliv. 2011, 18, 19–25. [Google Scholar] [CrossRef] [PubMed]
- Anroop, B.; Ghosh, B.; Parcha, V.; Khanam, J. Transdermal delivery of atenolol: Effect of prodrugs and iontophoresis. Curr. Drug Deliv. 2009, 6, 280–290. [Google Scholar] [CrossRef] [PubMed]
- Nair, A.; Morsy, M.A.; Jacob, S. Dose translation between laboratory animals and human in preclinical and clinical phases of drug development. Drug Dev. Res. 2018, 79, 373–382. [Google Scholar] [CrossRef]
- Rajabalaya, R.; Leen, G.; Chellian, J.; Chakravarthi, S.; David, S. Tolterodine tartrate proniosomal gel transdermal delivery for overactive bladder. Pharmaceutics 2016, 8, 27. [Google Scholar] [CrossRef]
- Draize, J.H.; Woodard, G.; Calvery, H.O. Methods for the study of irritation and toxicity of substances applied topically to the skin and mucous membranes. J. Pharmacol. Exp. Ther. 1944, 82, 377–390. [Google Scholar]
- Ghosh, A.; Banerjee, S.; Kaity, S.; Wong, T.W. Current pharmaceutical design on adhesive based transdermal drug delivery systems. Curr. Pharm. Des. 2015, 21, 2771–2783. [Google Scholar] [CrossRef]
- Ganti, S.S.; Bhattaccharjee, S.A.; Murnane, K.S.; Blough, B.E.; Banga, A.K. Formulation and evaluation of 4-benzylpiperidine drug-in-adhesive matrix type transdermal patch. Int. J. Pharm. 2018, 550, 71–78. [Google Scholar] [CrossRef] [PubMed]
- Jung, E.; Lee, E.Y.; Choi, H.K.; Ban, S.J.; Choi, S.H.; Kim, J.S.; Yoon, I.S.; Kim, D.D. Development of drug-in-adhesive patch formulations for transdermal delivery of fluoxetine: In vitro and in vivo evaluations. Int. J. Pharm. 2015, 487, 49–55. [Google Scholar] [CrossRef] [PubMed]
- Weng, W.; Quan, P.; Liu, C.; Zhao, H.; Fang, L. Design of a drug-in-adhesive transdermal patch for risperidone: Effect of drug-additive interactions on the crystallization inhibition and in vitro/in vivo correlation study. J. Pharm. Sci. 2016, 105, 3153–3161. [Google Scholar] [CrossRef] [PubMed]
- Ravula, R.; Herwadkar, A.K.; Abla, M.J.; Little, J.; Banga, A.K. Formulation optimization of a drug in adhesive transdermal analgesic patch. Drug Dev. Ind. Pharm. 2016, 42, 862–870. [Google Scholar] [CrossRef] [PubMed]
- Lane, M.E. Skin penetration enhancers. Int. J. Pharm. 2013, 447, 12–21. [Google Scholar] [CrossRef] [PubMed]
- Nair, A.B.; Jacob, S.; Al-Dhubiab, B.E.; Alhumam, R.N. Influence of skin permeation enhancers on the transdermal delivery of palonosetron: An in vitro evaluation. J. Appl. Biomed. 2018, 16, 192–197. [Google Scholar] [CrossRef]
- Shi, Y.; Li, Y.; Wu, J.; Wang, W.; Dong, A.; Zhang, J. A novel transdermal drug delivery system based on self-adhesive Janus nanofibrous film with high breathability and monodirectional water-penetration. J. Biomater. Sci. Polym. Ed. 2014, 25, 713–728. [Google Scholar] [CrossRef] [PubMed]
- Nair, A.; Jacob, S.; Al-Dhubiab, B.; Attimarad, M.; Harsha, S. Basic considerations in the dermatokinetics of topical formulations. Braz. J. Pharm. Sci. 2013, 49, 423–434. [Google Scholar] [CrossRef] [Green Version]






| Batch Code | Adhesive | Pioglitazone Incorporated (% w/w) | Enhancer (5% w/w) | Amount in 1 cm2 (mg) |
|---|---|---|---|---|
| F1 | Duro-Tak 87-4098 | 2 | - | 4.7 ± 0.2 |
| F2 | Duro-Tak 87-9301 | 2 | - | 4.8 ± 0.1 |
| F3 | Duro-Tak 87-900A | 2 | - | 4.7 ± 0.2 |
| F4 | Duro-Tak 87-4287 | 2 | - | 4.8 ± 0.1 |
| F5 | Duro-Tak 87-2516 | 2 | - | 4.7 ± 0.1 |
| F6 | Duro-Tak 87-2516 | 2 | N-methyl-2-pyrrolidone | 4.7 ± 0.1 |
| F7 | Duro-Tak 87-2516 | 2 | Oleic acid | 4.8 ± 0.2 |
| F8 | Duro-Tak 87-2516 | 2 | Diethylene glycol monoethyl ether | 4.7 ± 0.1 |
| F9 | Duro-Tak 87-2516 | 2 | Tween 80 | 4.7 ± 0.2 |
| F10 | Duro-Tak 87-2516 | 2 | Propylene glycol | 4.8 ± 0.2 |
| F11 | Duro-Tak 87-2516 | 3 | Propylene glycol | 7.1 ± 0.3 |
| F12 | Duro-Tak 87-2516 | 4 | Propylene glycol | 9.6 ± 0.3 |
| F13 | Duro-Tak 87-2516 | 5 | Propylene glycol | 12.1 ± 0.4 |
| F14 | Duro-Tak 87-2516 | 6 | Propylene glycol | 14.5 ± 0.4 |
| Adhesive | Factors | Model Name | |||||
|---|---|---|---|---|---|---|---|
| Zero Order | First Order | Higuchi | Korsmeyer-Peppas | Weibull Model | Hixson-Crowell | ||
| Duro-Tak 87-4098 | r2 | 0.9602 | 0.9877 | 0.9729 | 0.9905 | 0.9961 | 0.9804 |
| SSR | 78.76 | 23.04 | 53.53 | 31.39 | 9.16 | 37.09 | |
| FR | 15.75 | 4.61 | 10.71 | 6.28 | 1.83 | 7.42 | |
| Duro-Tak 87-9301 | r2 | 0.9539 | 0.9866 | 0.9814 | 0.9935 | 0.9984 | 0.9777 |
| SSR | 96.20 | 28.76 | 38.87 | 21.87 | 3.90 | 46.09 | |
| FR | 19.24 | 5.75 | 7.77 | 4.37 | 0.78 | 9.22 | |
| Duro-Tak 87-900A | r2 | 0.9823 | 0.9990 | 0.9605 | 0.9932 | 0.9981 | 0.9986 |
| SSR | 59.53 | 4.24 | 132.53 | 25.63 | 2.88 | 5.17 | |
| FR | 11.91 | 0.85 | 26.51 | 5.13 | 0.58 | 1.03 | |
| Duro-Tak 87-4287 | r2 | 0.9695 | 0.9983 | 0.9657 | 0.9919 | 0.9996 | 0.9978 |
| SSR | 147.99 | 13.15 | 166.88 | 82.07 | 1.92 | 7.43 | |
| FR | 29.60 | 2.63 | 33.38 | 16.41 | 0.38 | 1.49 | |
| Duro-Tak 87-2516 | r2 | 0.8788 | 0.9989 | 0.9776 | 0.9648 | 0.9996 | 0.9834 |
| SSR | 906.27 | 4.12 | 167.80 | 331.91 | 1.04 | 144.05 | |
| FR | 181.25 | 0.82 | 33.56 | 66.38 | 0.21 | 28.81 | |
| Batch Code | Lag Time (h) | Flux (µg/cm2/h) | Cumulative Amount Permeated (12 h) (µg/cm2) | Permeability Coefficient (cm/h × 10−4) |
|---|---|---|---|---|
| F1 | 0.18 ± 0.06 | 6.90 ± 1.55 | 74.83 ± 12.66 | 3.12 ± 0.94 |
| F2 | 0.16 ± 0.05 | 7.54 ± 2.92 | 82.25 ± 29.20 | 3.43 ± 1.18 |
| F3 | 0.17 ± 0.06 | 8.78 ± 3.14 | 92.12 ± 23.96 | 3.84 ± 1.05 |
| F4 | 0.14 ± 0.04 | 11.42 ± 3.64 | 129.02 ± 20.42 | 5.38 ± 1.47 |
| F5 | 0.09 ± 0.02 | 15.67 ± 2.35 | 174.24 ± 39.61 | 7.26 ± 1.24 |
| F6 | 0.10 ± 0.04 | 18.27 ± 3.71 | 216.91 ± 38.94 | 9.04 ± 1.32 |
| F7 | 0.09 ± 0.03 | 21.32 ± 3.86 | 249.86 ± 24.74 | 10.41 ± 1.81 |
| F8 | 0.08 ± 0.03 | 22.95 ± 3.91 | 267.69 ± 32.45 | 11.12 ± 1.73 |
| F9 | 0.07 ± 0.02 | 26.66 ± 4.18 | 313.01 ± 22.23 | 13.04 ± 1.90 |
| F10 | 0.06 ± 0.01 | 32.59 ± 4.37 | 387.90 ± 33.08 | 15.16 ± 1.15 |
| F11 | 0.06 ± 0.03 | 43.86 ± 4.92 | 526.28 ± 65.21 | 14.61 ± 1.95 |
| F12 | 0.05 ± 0.02 | 53.66 ± 4.87 | 643.89 ± 68.17 | 14.97 ± 1.41 |
| F13 | 0.05 ± 0.03 | 64.74 ± 5.83 | 776.86 ± 52.94 | 14.56 ± 2.95 |
| F14 | 0.05 ± 0.02 | 72.68 ± 5.67 | 872.14 ± 67.36 | 14.91 ± 2.11 |
| Parameter | Transdermal | Oral Suspension |
|---|---|---|
| Tmax (h) | 4 | 1 |
| Cmax (ng/mL) | 711.83 ± 210.06 | 842.30 ± 226.01 |
| AUC0–α (ng.h/mL) | 13,506.51 ± 1649.92 * | 6082.56 ± 1384.08 |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Nair, A.B.; Gupta, S.; Al-Dhubiab, B.E.; Jacob, S.; Shinu, P.; Shah, J.; Aly Morsy, M.; SreeHarsha, N.; Attimarad, M.; Venugopala, K.N.; et al. Effective Therapeutic Delivery and Bioavailability Enhancement of Pioglitazone Using Drug in Adhesive Transdermal Patch. Pharmaceutics 2019, 11, 359. https://doi.org/10.3390/pharmaceutics11070359
Nair AB, Gupta S, Al-Dhubiab BE, Jacob S, Shinu P, Shah J, Aly Morsy M, SreeHarsha N, Attimarad M, Venugopala KN, et al. Effective Therapeutic Delivery and Bioavailability Enhancement of Pioglitazone Using Drug in Adhesive Transdermal Patch. Pharmaceutics. 2019; 11(7):359. https://doi.org/10.3390/pharmaceutics11070359
Chicago/Turabian StyleNair, Anroop B., Sumeet Gupta, Bandar E. Al-Dhubiab, Shery Jacob, Pottathil Shinu, Jigar Shah, Mohamed Aly Morsy, Nagaraja SreeHarsha, Mahesh Attimarad, Katharigatta N. Venugopala, and et al. 2019. "Effective Therapeutic Delivery and Bioavailability Enhancement of Pioglitazone Using Drug in Adhesive Transdermal Patch" Pharmaceutics 11, no. 7: 359. https://doi.org/10.3390/pharmaceutics11070359