Resorbable Beads Provide Extended Release of Antifungal Medication: In Vitro and In Vivo Analyses
Abstract
:1. Introduction
2. Materials and Methods
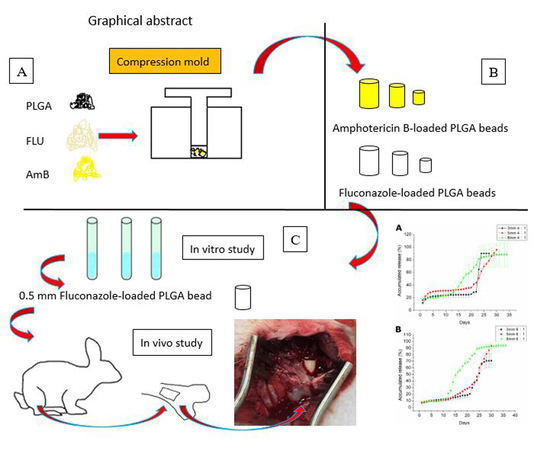
2.1. Fabrication of Poly(d,l-lactide-co-glycolide) PLGA/Amphotericin B and PLGA/Fluconazole Beads
2.2. In Vitro Analysis of Amphotericin B and Fluconazole Release
2.3. FTIR Spectrometry
2.4. Determination of the Water Contact Angle
2.5. Cell Culture
2.6. In Vivo Animal Study
3. Results
3.1. Characterization of Fabricated Poly(d,l-lactide-co-glycolide) PLGA/Amphotericin B and PLGA/Fluconazole Beads
3.2. In Vitro Release Dynamics of Poly(d,l-lactide-co-glycolide) PLGA/Amphotericin B and PLGA/Fluconazole Beads
3.3. In Vivo Drug Release
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Gamaletsou, M.N.; Walsh, T.J.; Sipsas, N.V. Epidemiology of fungal osteomyelitis. Curr. Fungal Infect. Rep. 2014, 8, 262–270. [Google Scholar] [CrossRef]
- Gamaletsou, M.N.; Rammaert, B.; Bueno, M.A.; Moriyama, B.; Sipsas, N.V.; Kontoyiannis, D.P.; Roilides, E.; Zeller, V.; Prinapori, R.; Taj-Aldeen, S.J.; et al. Aspergillus osteomyelitis: Epidemiology, clinical manifestations, management, and outcome. J. Infect. 2014, 68, 478–493. [Google Scholar] [CrossRef] [PubMed]
- Gamaletsou, M.N.; Kontoyiannis, D.P.; Sipsas, N.V.; Moriyama, B.; Alexander, E.; Roilides, E.; Brause, B.; Walsh, T.J. Candida osteomyelitis: Analysis of 207 pediatric and adult cases (1970–2011). Clin. Infect. Dis. 2012, 55, 1338–1351. [Google Scholar] [CrossRef] [PubMed]
- Desai, J.V.; Mitchell, A.P.; Andes, D.R. Fungal biofilms, drug resistance, and recurrent infection. Cold Spring Harb. Perspect. Med. 2014, 4, a019729. [Google Scholar] [CrossRef] [PubMed]
- Rammaert, B.; Gamaletsou, M.N.; Zeller, V.; Elie, C.; Prinapori, R.; Taj-Aldeen, S.J.; Roilides, E.; Kontoyiannis, D.P.; Brause, B.; Sipsas, N.V.; et al. Dimorphic fungal osteoarticular infections. Eur. J. Clin. Microbiol. Infect. Dis. 2014, 33, 2131–2140. [Google Scholar] [CrossRef]
- Bariteau, J.T.; Waryasz, G.R.; McDonnell, M.; Fischer, S.A.; Hayda, R.A.; Born, C.T. Fungal osteomyelitis and septic arthritis. J. Am. Acad. Orthop. Surg. 2014, 22, 390–401. [Google Scholar] [CrossRef]
- Mader, J.T.; Calhoun, J.; Cobos, J. In vitro evaluation of antibiotic diffusion from antibiotic-impregnated biodegradable beads and polymethylmethacrylate beads. Antimicrob. Agents Chemother. 1997, 41, 415–418. [Google Scholar] [CrossRef] [Green Version]
- Henry, M.W.; Miller, A.O.; Walsh, T.J.; Brause, B.D. Fungal musculoskeletal infections. Infect. Dis. Clin. N. Am. 2017, 31, 353–368. [Google Scholar] [CrossRef]
- Cornely, O.A.; Lasso, M.; Betts, R.; Klimko, N.; Vazquez, J.; Dobb, G.; Velez, J.; Williams-Diaz, A.; Lipka, J.; Taylor, A.; et al. Caspofungin for the treatment of less common forms of invasive candidiasis. J. Antimicrob. Chemother. 2007, 60, 363–369. [Google Scholar] [CrossRef] [Green Version]
- Marcos-Zambrano, L.J.; Escribano, P.; Bouza, E.; Guinea, J. Comparison of the antifungal activity of micafungin and amphotericin B against Candida tropicalis biofilms. J. Antimicrob. Chemother. 2016, 71, 2498–2501. [Google Scholar] [CrossRef]
- Pappas, P.G.; Kauffman, C.A.; Andes, D.R.; Clancy, C.J.; Marr, K.A.; Ostrosky-Zeichner, L.; Reboli, A.C.; Schuster, M.G.; Vazquez, J.A.; Walsh, T.J.; et al. Clinical practice guideline for the management of candidiasis: 2016 update by the Infectious Diseases Society of America. Clin. Infect. Dis. 2016, 62, e1–e50. [Google Scholar] [CrossRef] [PubMed]
- Kweon, C.; McLaren, A.C.; Leon, C.; McLemore, R. Amphotericin B delivery from bone cement increases with porosity but strength decreases. Clin. Orthop. Relat. Res. 2011, 469, 3002–3007. [Google Scholar] [CrossRef] [PubMed]
- Sealy, P.I.; Nguyen, C.; Tucci, M.; Benghuzzi, H.; Cleary, J.D. Delivery of antifungal agents using bioactive and nonbioactive bone cements. Ann. Pharmacother. 2009, 43, 1606–1615. [Google Scholar] [CrossRef] [PubMed]
- Goss, B.; Lutton, C.; Weinrauch, P.; Jabur, M.; Gillett, G.; Crawford, R. Elution and mechanical properties of antifungal bone cement. J. Arthroplast. 2007, 22, 902–908. [Google Scholar] [CrossRef] [PubMed]
- Liu, S.J.; Ueng, S.W.N.; Chan, E.C.; Lin, S.S.; Tsai, C.H.; Wei, F.C.; Shih, C.H. In vitro elution of vancomycin from biodegradable beads. J. Biomed. Mater. Res. (Appl. Biomater.) 1999, 48, 613–620. [Google Scholar] [CrossRef]
- Amass, W.; Amass, A.; Tighe, B. A review of biodegradable polymers: Uses, current developments in the synthesis and characterization of biodegradable polyesters, blends of biodegradable polymers and recent advances in biodegradation studies. Polym. Int. 1998, 47, 89–144. [Google Scholar] [CrossRef]
- Doppalapudi, S.; Jain, A.; Khan, W.; Domb, A.J. Biodegradable polymers—An overview. Biodegrad. Polym. 2014, 25, 427–435. [Google Scholar] [CrossRef]
- Gagoś, M.; Arczewska, M. FTIR spectroscopic study of molecular organization of the antibiotic amphotericin B in aqueous solution and in DPPC lipid monolayers containing the sterols cholesterol and ergosterol. Eur. Biophys. J. 2012, 41, 663–673. [Google Scholar] [CrossRef]
- Atay, O.; Selck, F. Quantitative determination of fluconazole by infrared spectrophotometry. Anal. Lett. 1996, 29, 2163–2176. [Google Scholar] [CrossRef]
- Burnett, N.; Mathura, K.; Metivier, K.S.; Holder, R.B.; Brown, G.; Campbell, M. An investigation into haematological and serum chemistry parameters of rabbits in Trinidad. World Rabbit Sci. 2006, 14, 175–187. [Google Scholar] [CrossRef]
- Wu, M.H.; Hsu, K.Y. Candidal arthritis in revision knee arthroplasty successfully treated with sequential parenteral-oral fluconazole and amphotericin B-loaded cement spacer. Knee Surg. Sports Traumatol. Arthrosc. 2011, 19, 273–276. [Google Scholar] [CrossRef] [PubMed]
- Khan, A.A.; Alanazi, A.M.; Jabeen, M.; Khan, S.; Malik, A. Additive potential of combination therapy against cryptococcosis employing a novel amphotericin B and fluconazole loaded dual delivery system. Eur. J. Pharm. Sci. 2018, 119, 171–178. [Google Scholar] [CrossRef] [PubMed]
- Souza, A.O.; Nascimento, A.L.; de Vasconcelos, N.M.; Jerônimo, M.S.; Siqueira, I.M.; R-Santos, L.; Cintra, D.O.; Fuscaldi, L.L.; Pires Júnior, O.R.; Titze-de-Almeida, R.; et al. Activity and in vivo tracking of Amphotericin B loaded PLGA nanoparticles. Eur. J. Med. Chem. 2015, 95, 267–276. [Google Scholar] [CrossRef] [PubMed]
- Amaral, A.C.; Bocca, A.L.; Ribeiro, A.M.; Nunes, J.; Peixoto, D.L.; Simioni, A.R.; Primo, F.L.; Lacava, Z.G.; Bentes, R.; Titze-de-Almeida, R.; et al. Amphotericin B in poly(lactic-co-glycolic acid) (PLGA) and dimercaptosuccinic acid (DMSA) nanoparticles against paracoccidioidomycosis. J. Antimicrob. Chemother. 2009, 63, 526–533. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Reckling, F.W.; Dillon, W.L. The bone-cement interface temperature during total joint replacement. J. Bone Joint Surg. Am. 1977, 59, 80–82. [Google Scholar] [CrossRef] [PubMed]
- Davis, M.R.; Nguyen, M.V.; Donnelley, M.A.; Thompson, G.R., III. Tolerability of long-term fluconazole therapy. J. Antimicrob. Chemother. 2019, 74, 768–771. [Google Scholar] [CrossRef] [PubMed]
- Tverdek, F.P.; Kofteridis, D.; Kontoyiannis, D.P. Antifungal agents and liver toxicity: A complex interaction. Expert Rev. Anti Infect. Ther. 2016, 14, 765–776. [Google Scholar] [CrossRef]
- Wang, J.L.; Chang, C.H.; Young-Xu, Y.; Chan, K.A. Systematic review and meta-analysis of the tolerability and hepatotoxicity of antifungals in empirical and definitive therapy for invasive fungal infection. Antimicrob. Agents Chemother. 2010, 54, 2409–2419. [Google Scholar] [CrossRef]
- Louie, A.; Banerjee, P.; Drusano, G.L.; Shayegani, M.; Miller, M.H. Interaction between fluconazole and amphotericin B in mice with systemic infection due to fluconazole-susceptible or -resistant strains of Candida albicans. Antimicrob. Agents Chemother. 1999, 43, 2841–2847. [Google Scholar] [CrossRef]
- Stewart, R.L.; Cox, J.T.; Volgas, D.; Stannard, J.; Duffy, L.; Waites, K.B.; Chu, T.M. The use of a biodegradable, loadbearing scaffold as a carrier for antibiotics in an infected open fracture model. J. Orthop. Trauma. 2010, 24, 587–591. [Google Scholar] [CrossRef]
- Williams, D.F. Biodegradation of surgical polymers. J. Mater. Sci. 1982, 17, 1233–1246. [Google Scholar] [CrossRef]
- Kumbar, S.G.; Nukavarapu, S.P.; James, R.; Nair, L.S.; Laurencin, C.T. Electrospun poly(lactic acid-co-glycolic acid) scaffolds for skin tissue engineering. Biomaterials 2008, 29, 4100–4107. [Google Scholar] [CrossRef] [PubMed] [Green Version]











| PLGA/Drug Ratio | Size: Diameter × Height (mm × mm) | Weight of PLGA (mg) | Weight of Drug (mg) |
|---|---|---|---|
| 6:1 | 3 × 5.65 | 54 | 9 |
| 5 × 5.55 | 150 | 25 | |
| 8 × 6.18 | 384 | 64 | |
| 4:1 | 3 × 5.02 | 50.4 | 12.6 |
| 5 × 6.27 | 140 | 35 | |
| 8 × 6.25 | 358.4 | 89.6 |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hsu, Y.-H.; Chen, H.-Y.; Chen, J.-C.; Yu, Y.-H.; Chou, Y.-C.; Ueng, S.W.-N.; Liu, S.-J. Resorbable Beads Provide Extended Release of Antifungal Medication: In Vitro and In Vivo Analyses. Pharmaceutics 2019, 11, 550. https://doi.org/10.3390/pharmaceutics11110550
Hsu Y-H, Chen H-Y, Chen J-C, Yu Y-H, Chou Y-C, Ueng SW-N, Liu S-J. Resorbable Beads Provide Extended Release of Antifungal Medication: In Vitro and In Vivo Analyses. Pharmaceutics. 2019; 11(11):550. https://doi.org/10.3390/pharmaceutics11110550
Chicago/Turabian StyleHsu, Yung-Heng, Huang-Yu Chen, Jin-Chung Chen, Yi-Hsun Yu, Ying-Chao Chou, Steve Wen-Neng Ueng, and Shih-Jung Liu. 2019. "Resorbable Beads Provide Extended Release of Antifungal Medication: In Vitro and In Vivo Analyses" Pharmaceutics 11, no. 11: 550. https://doi.org/10.3390/pharmaceutics11110550