Attenuated Risk Association of End-Stage Kidney Disease with Metformin in Type 2 Diabetes with eGFR Categories 1–4
Abstract
:1. Introduction
2. Results
2.1. Baseline Characteristics
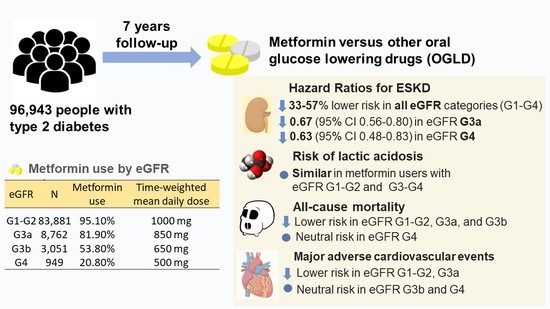
2.2. Metformin Use and Risk of ESKD
2.3. Metformin Use and Lactic Acidosis
2.4. Metformin Use and Risk of All-Cause Mortality and MACE
2.5. Sensitivity Analysis
3. Discussion
4. Materials and Methods
4.1. Setting and Patients
4.2. Population-Based Cohort (HKDSD RAMP-DM Module)
4.3. Register-Based Cohort (PWH-Based HKDR Cohort)
4.4. Ooutcomes Defintions
4.5. Metformin Exposure and Other Medications Assessment
4.6. Time-Fixed and Time-Varying Covariates
4.7. Statistical Analysis
4.8. Sensitivity Analysis
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Bailey, C.J. Metformin: Historical overview. Diabetologia 2017, 60, 1566–1576. [Google Scholar] [CrossRef] [PubMed]
- Holman, R.R.; Paul, S.K.; Bethel, M.A.; Matthews, D.R.; Neil, H.A. 10-year follow-up of intensive glucose control in type 2 diabetes. N. Engl. J. Med. 2008, 359, 1577–1589. [Google Scholar] [CrossRef] [PubMed]
- Inzucchi, S.E. FDA Drug Safety Communication: FDA Revises Warnings Regarding Use of the Diabetes Medicine Metformin in Certain Patients with Reduced Kidney Function. Available online: https://www.fda.gov/drugs/drug-safety-and-availability (accessed on 3 August 2021).
- Chow, E.; Yang, A.; Chung, C.H.L.; Chan, J.C.N. A Clinical Perspective of the Multifaceted Mechanism of Metformin in Diabetes, Infections, Cognitive Dysfunction, and Cancer. Pharmaceuticals 2022, 15, 442. [Google Scholar] [CrossRef] [PubMed]
- Yang, A.; Shi, M.; Wu, H.; Lau, E.S.H.; Ma, R.C.W.; Kong, A.P.S.; So, W.Y.; Luk, A.O.Y.; Chan, J.C.N.; Chow, E. Long-term metformin use and risk of pneumonia and related death in type 2 diabetes: A registry-based cohort study. Diabetologia 2021, 64, 1760–1765. [Google Scholar] [CrossRef]
- Lin, C.X.; Li, Y.; Liang, S.; Tao, J.; Zhang, L.S.; Su, Y.F.; Huang, Y.X.; Zhao, Z.K.; Liu, S.Y.; Zheng, J.M. Metformin Attenuates Cyclosporine A-induced Renal Fibrosis in Rats. Transplantation 2019, 103, e285–e296. [Google Scholar] [CrossRef] [PubMed]
- Satriano, J.; Sharma, K.; Blantz, R.C.; Deng, A. Induction of AMPK activity corrects early pathophysiological alterations in the subtotal nephrectomy model of chronic kidney disease. Am. J. Physiol. Ren. Physiol. 2013, 305, F727–F733. [Google Scholar] [CrossRef]
- Han, Y.; Xie, H.; Liu, Y.; Gao, P.; Yang, X.; Shen, Z. Effect of metformin on all-cause and cardiovascular mortality in patients with coronary artery diseases: A systematic review and an updated meta-analysis. Cardiovasc. Diabetol. 2019, 18, 96. [Google Scholar] [CrossRef]
- Kwon, S.; Kim, Y.C.; Park, J.Y.; Lee, J.; An, J.N.; Kim, C.T.; Oh, S.; Park, S.; Kim, D.K.; Oh, Y.K.; et al. The Long-term Effects of Metformin on Patients with Type 2 Diabetic Kidney Disease. Diabetes Care 2020, 43, 948–955. [Google Scholar] [CrossRef]
- Fu, E.L.; van Diepen, M. Comment on Kwon et al. The Long-term Effects of Metformin on Patients with Type 2 Diabetic Kidney Disease. Diabetes Care 2020, 43, e190. [Google Scholar] [CrossRef]
- Hu, Y.; Lei, M.; Ke, G.; Huang, X.; Peng, X.; Zhong, L.; Fu, P. Metformin Use and Risk of All-Cause Mortality and Cardiovascular Events in Patients with Chronic Kidney Disease—A Systematic Review and Meta-Analysis. Front. Endocrinol. 2020, 11, 559446. [Google Scholar] [CrossRef]
- Charytan, D.M.; Solomon, S.D.; Ivanovich, P.; Remuzzi, G.; Cooper, M.E.; McGill, J.B.; Parving, H.H.; Parfrey, P.; Singh, A.K.; Burdmann, E.A.; et al. Metformin use and cardiovascular events in patients with type 2 diabetes and chronic kidney disease. Diabetes Obes. Metab. 2019, 21, 1199–1208. [Google Scholar] [CrossRef] [PubMed]
- Hung, S.C.; Chang, Y.K.; Liu, J.S.; Kuo, K.L.; Chen, Y.H.; Hsu, C.C.; Tarng, D.C. Metformin use and mortality in patients with advanced chronic kidney disease: National, retrospective, observational, cohort study. Lancet Diabetes Endocrinol. 2015, 3, 605–614. [Google Scholar] [CrossRef]
- Whitlock, R.H.; Hougen, I.; Komenda, P.; Rigatto, C.; Clemens, K.K.; Tangri, N. A Safety Comparison of Metformin vs Sulfonylurea Initiation in Patients with Type 2 Diabetes and Chronic Kidney Disease: A Retrospective Cohort Study. Mayo Clin. Proc. 2020, 95, 90–100. [Google Scholar] [CrossRef] [PubMed]
- Rena, G.; Hardie, D.G.; Pearson, E.R. The mechanisms of action of metformin. Diabetologia 2017, 60, 1577–1585. [Google Scholar] [CrossRef]
- Navaneethan, S.D.; Zoungas, S.; Caramori, M.L.; Chan, J.C.N.; Heerspink, H.J.L.; Hurst, C.; Liew, A.; Michos, E.D.; Olowu, W.A.; Sadusky, T.; et al. Diabetes Management in Chronic Kidney Disease: Synopsis of the 2020 KDIGO Clinical Practice Guideline. Ann. Intern. Med. 2020, 174, 385–394. [Google Scholar] [CrossRef]
- Luk, A.; Chan, J.C. Diabetic nephropathy—What are the unmet needs? Diabetes Res. Clin. Pract. 2008, 82 (Suppl. S1), S15–S20. [Google Scholar] [CrossRef]
- De Broe, M.E.; Jouret, F. Does metformin do more benefit or harm in chronic kidney disease patients? Kidney Int. 2020, 98, 1098–1101. [Google Scholar] [CrossRef]
- Luk, A.O.; Li, X.; Zhang, Y.; Guo, X.; Jia, W.; Li, W.; Weng, J.; Yang, W.; Chan, W.B.; Ozaki, R.; et al. Quality of care in patients with diabetic kidney disease in Asia: The Joint Asia Diabetes Evaluation (JADE) Registry. Diabet. Med. 2016, 33, 1230–1239. [Google Scholar] [CrossRef]
- Manski-Nankervis, J.A.; Thuraisingam, S.; Sluggett, J.K.; Kilov, G.; Furler, J.; O’Neal, D.; Jenkins, A. Prescribing of diabetes medications to people with type 2 diabetes and chronic kidney disease: A national cross-sectional study. BMC Fam. Pract. 2019, 20, 29. [Google Scholar] [CrossRef]
- Busch, M.; Nadal, J.; Schmid, M.; Paul, K.; Titze, S.; Hübner, S.; Köttgen, A.; Schultheiss, U.T.; Baid-Agrawal, S.; Lorenzen, J.; et al. Glycaemic control and antidiabetic therapy in patients with diabetes mellitus and chronic kidney disease—Cross-sectional data from the German Chronic Kidney Disease (GCKD) cohort. BMC Nephrol. 2016, 17, 59. [Google Scholar] [CrossRef] [Green Version]
- Roussel, R.; Travert, F.; Pasquet, B.; Wilson, P.W.; Smith, S.C., Jr.; Goto, S.; Ravaud, P.; Marre, M.; Porath, A.; Bhatt, D.L.; et al. Metformin use and mortality among patients with diabetes and atherothrombosis. Arch. Intern. Med. 2010, 170, 1892–1899. [Google Scholar] [CrossRef] [PubMed]
- Mihai, S.; Codrici, E.; Popescu, I.D.; Enciu, A.M.; Albulescu, L.; Necula, L.G.; Mambet, C.; Anton, G.; Tanase, C. Inflammation-Related Mechanisms in Chronic Kidney Disease Prediction, Progression, and Outcome. J. Immunol. Res. 2018, 2018, 2180373. [Google Scholar] [CrossRef] [PubMed]
- Chu, P.Y.; Hackstadt, A.J.; Chipman, J.; Griffin, M.R.; Hung, A.M.; Greevy, R.A.; Grijalva, C.G.; Elasy, T.; Roumie, C.L. Hospitalization for Lactic Acidosis Among Patients with Reduced Kidney Function Treated with Metformin or Sulfonylureas. Diabetes Care 2020, 43, 1462–1470. [Google Scholar] [CrossRef]
- Lazarus, B.; Wu, A.; Shin, J.-I.; Sang, Y.; Alexander, G.C.; Secora, A.; Inker, L.A.; Coresh, J.; Chang, A.R.; Grams, M.E. Association of Metformin Use with Risk of Lactic Acidosis Across the Range of Kidney Function. JAMA Intern. Med. 2018, 178, 903. [Google Scholar] [CrossRef]
- Lalau, J.D.; Kajbaf, F.; Bennis, Y.; Hurtel-Lemaire, A.S.; Belpaire, F.; De Broe, M.E. Metformin Treatment in Patients with Type 2 Diabetes and Chronic Kidney Disease Stages 3A, 3B, or 4. Diabetes Care 2018, 41, 547–553. [Google Scholar] [CrossRef]
- Thomas, L.; Li, F.; Pencina, M. Using Propensity Score Methods to Create Target Populations in Observational Clinical Research. JAMA 2020, 323, 466–467. [Google Scholar] [CrossRef]
- Gokhale, M.; Stürmer, T.; Buse, J.B. Real-world evidence: The devil is in the detail. Diabetologia 2020, 63, 1694–1705. [Google Scholar] [CrossRef]
- Lalau, J.-D.; Kajbaf, F.; Protti, A.; Christensen, M.M.; De Broe, M.E.; Wiernsperger, N. Metformin-associated lactic acidosis (MALA): Moving towards a new paradigm. Diabetes Obes. Metab. 2017, 19, 1502–1512. [Google Scholar] [CrossRef]
- Chan, J.C.; Lim, L.-L.; Luk, A.O.; Ozaki, R.; Kong, A.P.; Ma, R.C.; So, W.-Y.; Lo, S.-V. From Hong Kong Diabetes Register to JADE Program to RAMP-DM for data-driven actions. Diabetes Care 2019, 42, 2022–2031. [Google Scholar] [CrossRef]
- Wu, H.; Lau, E.S.H.; Yang, A.; Zhang, X.; Ma, R.C.W.; Kong, A.P.S.; Chow, E.; So, W.-Y.; Chan, J.C.N.; Luk, A.O.Y. Data Resource Profile: The Hong Kong Diabetes Surveillance Database (HKDSD). Int. J. Epidemiol. 2021, 51, e9–e17. [Google Scholar] [CrossRef]
- Yang, A.; Wu, H.; Lau, E.S.; Zhang, X.; Shi, M.; Fan, B.; Ma, R.C.; Kong, A.P.; Luk, A.O.; Chan, J.C. Glucose-lowering drug use, glycemic outcomes, and severe hypoglycemia: 18-Year trends in 0· 9 million adults with Diabetes in Hong Kong (2002–2019). Lancet Reg. Health-West. Pac. 2022, 26, 100509. [Google Scholar] [CrossRef] [PubMed]
- Yang, A.; Shi, M.; Wu, H.; Lau, E.S.; Fan, B.; Kong, A.P.; Ma, R.C.; Luk, A.O.; Chan, J.C.; Chow, E. Time-varying risk associations of renin angiotensin system inhibitors with pneumonia and related deaths in a cohort of 252,616 patients with diabetes (2002–2019). Diabetes Res. Clin. Pract. 2022, 185, 109233. [Google Scholar] [CrossRef] [PubMed]
- Schneeweiss, S.; Patorno, E. Conducting Real-world Evidence Studies on the Clinical Outcomes of Diabetes Treatments. Endocr. Rev. 2021, 42, 658–690. [Google Scholar] [CrossRef]
- Levey, A.S.; Stevens, L.A.; Schmid, C.H.; Zhang, Y.L.; Castro, A.F., 3rd; Feldman, H.I.; Kusek, J.W.; Eggers, P.; Van Lente, F.; Greene, T.; et al. A new equation to estimate glomerular filtration rate. Ann. Intern. Med. 2009, 150, 604–612. [Google Scholar] [CrossRef]
- Luft, D.; Deichsel, G.; Schmulling, R.-M.; Stein, W.; Eggstein, M. Definition of Clinically Relevant Lactic Acidosis in Patients with Internal Diseases. Am. J. Clin. Pathol. 1983, 80, 484–489. [Google Scholar] [CrossRef] [PubMed]
- Yang, A.; Wu, H.; Lau, E.S.; Ma, R.C.; Kong, A.P.; So, W.Y.; Luk, A.O.; Chan, J.C.; Chow, E. Trends in glucose-lowering drug use, glycemic control, and severe hypoglycemia in adults with diabetes in Hong Kong, 2002–2016. Diabetes Care 2020, 43, 2967–2974. [Google Scholar] [CrossRef]
- Thomas, L.E.; Li, F.; Pencina, M.J. Overlap Weighting: A Propensity Score Method That Mimics Attributes of a Randomized Clinical Trial. JAMA 2020, 323, 2417. [Google Scholar] [CrossRef]
- Westreich, D.; Cole, S.R.; Funk, M.J.; Brookhart, M.A.; Stürmer, T. The role of the c-statistic in variable selection for propensity score models. Pharmacoepidemiol. Drug Saf. 2011, 20, 317–320. [Google Scholar] [CrossRef] [PubMed]
- Stensrud, M.J.; Hernán, M.A. Why Test for Proportional Hazards? JAMA 2020, 323, 1401–1402. [Google Scholar] [CrossRef]
- Murad, H.; Dankner, R.; Berlin, A.; Olmer, L.; Freedman, L.S. Imputing missing time-dependent covariate values for the discrete time Cox model. Stat. Methods Med. Res. 2020, 29, 2074–2086. [Google Scholar] [CrossRef]
- De Boer, I.H.; Caramori, M.L.; Chan, J.C.N.; Heerspink, H.J.L.; Hurst, C.; Khunti, K.; Liew, A.; Michos, E.D.; Navaneethan, S.D.; Olowu, W.A.; et al. Executive summary of the 2020 KDIGO Diabetes Management in CKD Guideline: Evidence-based advances in monitoring and treatment. Kidney Int. 2020, 98, 839–848. [Google Scholar] [CrossRef] [PubMed]
- Heerspink, H.J.L.; Stefánsson, B.V.; Correa-Rotter, R.; Chertow, G.M.; Greene, T.; Hou, F.F.; Mann, J.F.E.; McMurray, J.J.V.; Lindberg, M.; Rossing, P.; et al. Dapagliflozin in Patients with Chronic Kidney Disease. N. Engl. J. Med. 2020, 383, 1436–1446. [Google Scholar] [CrossRef] [PubMed]




| Characteristics | New-Metformin Versus Other-OGLDs Users | |||||
|---|---|---|---|---|---|---|
| Before PS-OW | After PS-OW | |||||
| New-Metformin | Other-OGLDs | SMD | New-Metformin | Other-OGLDs | SMD | |
| n (%) | 88,771 | 7872 | 88,771 | 7872 | ||
| Men, % | 41,531 (46.8) | 4505 (57.2) | 0.210 | 55.3 | 55.3 | <0.001 |
| Age, years | 62.2 (11.4) | 69.7 (11.8) | 0.647 | 68.4 (12.1) | 68.4 (11.0) | <0.001 |
| Duration of diabetes, years | 4.8 (5.3) | 5.6 (6.1) | 0.151 | 5.7 (6.3) | 5.7 (5.2) | <0.001 |
| Family history of diabetes | 31,815 (35.8) | 2107 (26.8) | 0.197 | 28.4 | 28.4 | <0.001 |
| Smoking status | 0.225 | <0.001 | ||||
| Non-smoker | 69,416 (78.2) | 5544 (70.4) | 72.6 | 72.6 | ||
| Ever-smoker | 10,435 (11.8) | 1566 (19.9) | 17.7 | 17.7 | ||
| Current-smoker | 8920 (10.0) | 762 (9.7) | 9.6 | 9.6 | ||
| Body mass index, kg/m2 | 26.1 (4.2) | 25.1 (3.9) | 0.237 | 25.2 (4.0) | 25.2 (3.7) | <0.001 |
| SBP, mmHg | 133.5 (13.0) | 137.7 (16.8) | 0.280 | 136.4 (16.2) | 136.4 (13.9) | <0.001 |
| DBP, mmHg | 74.8 (8.3) | 72.4 (9.6) | 0.258 | 72.8 (9.4) | 72.8 (8.3) | <0.001 |
| Waist, cm | 89.5 (10.2) | 88.7 (10.2) | 0.082 | 88.6 (10.3) | 88.6 (9.7) | <0.001 |
| Triglyceride, mmol/L | 1.8 (1.4) | 1.6 (1.3) | 0.102 | 1.6 (1.4) | 1.6 (1.2) | <0.001 |
| Total Cholesterol, mmol/L | 5.0 (1.0) | 4.9 (1.1) | 0.101 | 4.9 (1.1) | 4.9 (1.0) | <0.001 |
| HDL-C, mmol/L | 1.3 (0.4) | 1.3 (0.4) | 0.028 | 1.3 (0.4) | 1.3 (0.4) | <0.001 |
| LDL-C, mmol/L | 2.9 (0.9) | 2.9 (0.9) | 0.062 | 2.9 (0.9) | 2.9 (0.9) | <0.001 |
| Urinary ACR, mg/mmol | 0.367 | <0.001 | ||||
| <3 | 64,808 (73.0) | 4651 (59.1) | 63.7 | 63.7 | ||
| 3–30 | 20,368 (22.9) | 2214 (28.1) | 27.2 | 27.2 | ||
| >30 | 3595 (4.0) | 1007 (12.8) | 9.1 | 9.1 | ||
| HbA1c, % | 8.0 (1.6) | 7.1 (1.5) | 0.585 | 7.3 (1.6) | 7.3 (1.0) | <0.001 |
| eGFR, mL/min/1.73 m2 | 84.1 (17.6) | 62.6 (24.3) | 1.017 | 68.6 (23.6) | 68.6 (18.5) | <0.001 |
| Haemoglobin, gm/dL | 13.8 (1.5) | 13.1 (1.9) | 0.405 | 13.4 (1.8) | 13.4 (1.7) | <0.001 |
| History of cancer, % | 3674 (4.1) | 730 (9.3) | 0.206 | 8.7 | 8.7 | <0.001 |
| History of medications, % | ||||||
| Sulfonylurea | 26,508 (29.9) | 5663 (71.9) | 0.928 | 64.1 | 64.1 | <0.001 |
| DPP-4is | 149 (0.2) | 77 (1.0) | 0.108 | 0.6 | 0.6 | <0.001 |
| TZDs | 59 (0.1) | 30 (0.4) | 0.067 | 0.3 | 0.3 | <0.001 |
| AGIs | 121 (0.1) | 48 (0.6) | 0.078 | 0.5 | 0.5 | <0.001 |
| Statin | 25,146 (28.3) | 1527 (19.4) | 0.211 | 20.9 | 20.9 | <0.001 |
| RASi | 25,203 (28.4) | 2950 (37.5) | 0.194 | 35.2 | 35.2 | <0.001 |
| Period of index year, % | 0.545 | <0.001 | ||||
| <2003 | 2274 (2.6) | 571 (7.3) | 5.6 | 5.6 | ||
| 2004–2007 | 10,492 (11.8) | 1999 (25.4) | 23.0 | 23.0 | ||
| 2008–2011 | 24,265 (27.3) | 2589 (32.9) | 32.8 | 32.8 | ||
| 2012–2016 | 35,910 (40.5) | 1905 (24.2) | 27.0 | 27.0 | ||
| 2017–2018 | 15,830 (17.8) | 808 (10.3) | 11.7 | 11.7 | ||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Yang, A.; Lau, E.S.H.; Wu, H.; Ma, R.C.W.; Kong, A.P.S.; So, W.Y.; Luk, A.O.Y.; Fu, A.W.C.; Chan, J.C.N.; Chow, E. Attenuated Risk Association of End-Stage Kidney Disease with Metformin in Type 2 Diabetes with eGFR Categories 1–4. Pharmaceuticals 2022, 15, 1140. https://doi.org/10.3390/ph15091140
Yang A, Lau ESH, Wu H, Ma RCW, Kong APS, So WY, Luk AOY, Fu AWC, Chan JCN, Chow E. Attenuated Risk Association of End-Stage Kidney Disease with Metformin in Type 2 Diabetes with eGFR Categories 1–4. Pharmaceuticals. 2022; 15(9):1140. https://doi.org/10.3390/ph15091140
Chicago/Turabian StyleYang, Aimin, Eric S. H. Lau, Hongjiang Wu, Ronald C. W. Ma, Alice P. S. Kong, Wing Yee So, Andrea O. Y. Luk, Amy W. C. Fu, Juliana C. N. Chan, and Elaine Chow. 2022. "Attenuated Risk Association of End-Stage Kidney Disease with Metformin in Type 2 Diabetes with eGFR Categories 1–4" Pharmaceuticals 15, no. 9: 1140. https://doi.org/10.3390/ph15091140