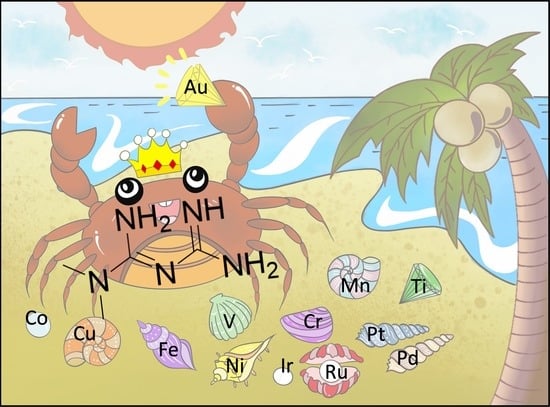
Biological Properties of Transition Metal Complexes with Metformin and Its Analogues
Abstract
:| Table of Contents | |
| 1. Introduction | 2 |
| 1.1. Brief Historical Outlook | 2 |
| 1.2. Diverse Therapeutic Applications of Metformin Derivatives | 3 |
| 1.3. Biological Consequences of Intracellular Interactions of Metformin with Endogenous Metals | 5 |
| 2. Biologically Active Metal Complexes with Metformin and Its Analogues | 7 |
| 2.1.Group III (Sc, Y and Lanthanides) | 7 |
| 2.2. Group IV (Ti, Zr, Hf) | 9 |
| 2.3. Group V (V, Nb, Ta) | 9 |
| 2.4.Group VI (Cr, Mo, W) | 13 |
| 2.5. Group VII (Mn, Tc, Re) | 15 |
| 2.6. Group VIII (Fe, Ru, Os) | 17 |
| 2.7. Group IX (Co, Rh, Ir) | 18 |
| 2.8. Group X (Ni, Pd, Pt) | 23 |
| 2.9. Group XI (Cu, Ag, Au) | 28 |
| 2.10. Group XII (Zn, Cd, Hg) | 34 |
| 2.11. The Role of the Metal Center in the Biological Activity and Potential Toxicity of Pre-Formed Metal-Metformin Complexes | 36 |
| 3. Conclusions and Future Outlook | 38 |
| Appendix A | 40 |
| References | 61 |
1. Introduction
1.1. Brief Historical Outlook
1.2. Diverse Therapeutic Applications of Metformin Derivatives
1.3. Biological Consequences of Intracellular Interactions of Metformin with Endogenous Metals
2. Biologically Active Metal Complexes with Metformin and Its Analogues
2.1. Group III (Sc, Y and Lanthanides)
2.2. Group IV (Ti, Zr, Hf)
2.3. Group V (V, Nb, Ta)
2.4. Group VI (Cr, Mo, W)
2.5. Group VII (Mn, Tc, Re)
2.6. Group VIII (Fe, Ru, Os)
2.7. Group IX (Co, Rh, Ir)
2.8. Group X (Ni, Pd, Pt)
2.9. Group XI (Cu, Ag, Au)
2.10. Group XII (Zn, Cd, Hg)
2.11. The Role of the Metal Center in the Biological Activity and Potential Toxicity of Pre-Formed Metal-Metformin Complexes
3. Conclusions and Future Outlook
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Appendix A
| Group | Metal | № | The Structure of Complex | Investigated Properties | Reference |
|---|---|---|---|---|---|
| III | Y | 1 |  | Antibacterial Antifungal | [68] |
| La | 2 |  | Antibacterial Antifungal | [68] | |
| Ce | 3 |  | Antibacterial Antifungal | [68] | |
| Sm | 4 |  | Antibacterial Antifungal | [68] | |
| Nd | 5 |  | Antidiabetic | [69] | |
| 6 |  | Antidiabetic | [69] | ||
| Dy | 7 |  | Detecting sugars | [70] | |
| 8 |  | Detecting sugars | [70] | ||
| IV | Zr | 9 |  | Antibacterial Antifungal | [71] |
| V | V | 10–11 |  | Antidiabetic | [76] |
| Inhibition of protein tyrosin phosphatases | [78] | ||||
| 12 |  | Antidiabetic | [76] | ||
| 13 |  | Inhibition of protein tyrosin phosphatases | [78] | ||
| 14–15 |  | Antidiabetic | [79] | ||
| 16 |  | Antidiabetic | [82,85,86,88] | ||
| 17–18 |  | DNA-binding | [91] | ||
| 19 |  | Antibacterial Antifungal | [92] | ||
| VI | Cr | 20 |  | Antibacterial Antifungal | [92] |
| Antidiabetic | [97] | ||||
| 21 |  | Antidiabetic Toxicity | [98] | ||
| 22 |  | Antidiabetic | [99] | ||
| 23 |  | Antidiabetic | [99] | ||
| 24–26 |  | DNA-binding | [100] | ||
| VII | Mn | 27 |  | Antibacterial Antifungal Cytotoxicity | [103] |
| 28 |  | Antibacterial Antifungal Cytotoxicity | [104] | ||
| 29 |  | Antibacterial Antifungal | [105] | ||
| Tc | 30 |  | Radiotherapeutic | [106] | |
| VIII | Fe | 31 |  | Antibacterial | [114] |
| 32 |  | Antibacterial | [114] | ||
| 33 |  | Antibacterial Antifungal | [105] | ||
| Ru | 34–35 |  | Anticancer Antidiabetic DNA-binding nteraction with BSA | [123] | |
| IX | Co | 36 |  | Antibacterial | [124] |
| 37 |  | Antibacterial Antifungal | [71] | ||
| 38 |  | Antibacterial | [125] | ||
| 39–43 |  | Antiviral | [127] | ||
| Antiviral Toxicity | [128] | ||||
| 44 |  | Antiviral Toxicity | [128] | ||
| 45–47 |  | DNA-binding | [131] | ||
| 48 |  | Antidiabetic DNA binding | [132] | ||
| 49 |  | Anticancer Antioxidant | [133] | ||
| Ir | 50–56 |  | Antibacterial Antifungal Toxicity Hemolytic | [137] | |
| 52–53 |  | Antibacterial Antifungal Toxicity Hemolytic | [137] | ||
| 57–58 |  | Antibacterial Antifungal Toxicity Hemolytic | [137] | ||
| 59–62 |  | Antibacterial Antifungal Toxicity Hemolytic | [137] | ||
| 63–65 |  | Anticancer activity | [138] | ||
| X | Ni | 66 |  | Antibacterial Antifungal Toxicity | [103] |
| 67 |  | Antibacterial Antifungal Toxicity | [104] | ||
| 68 |  | Antibacterial Cytotoxicity | [142] | ||
| 69 |  | Antibacterial Antifungal | [105] | ||
| 70 |  | Antibacterial Cytotoxicity Interactions with BSA | [142] | ||
| 71 |  | Antibacterial Antifungal | [71] | ||
| 72 |  | Anticancer | [129] | ||
| 73 |  | Antibacterial Antifungal Anticancer | [143] | ||
| 74–75 |  | Antibacterial Antifungal Anticancer | [143] | ||
| 76–79 |  | DNA-binding | [144] | ||
| 80 |  | DNA-binding Antidiabetic | [132] | ||
| Pd | 81 |  | Antibacterial Antifungal | [105] | |
| Antibacterial Antifungal Cytotoxicity | [145] | ||||
| 82 |  | Anticancer | [146] | ||
| 83–84 |  | Antibacterial Antifungal Cytotoxicity | [145] | ||
| 85 |  | Antibacterial Antifungal | [71] | ||
| 86 |  | Anticancer | [146] | ||
| 89 |  | Antibacterial | [124] | ||
| Pt | 88 |  | Antibacterial | [124] | |
| 90 |  | Anticancer Toxicity | [155] | ||
| 91 |  | Antibacterial Antifungal | [105] | ||
| XI | Cu | 92 |  | Antibacterial | [159] |
| 93 |  | Antibacterial | [159] | ||
| 94 |  | Antibacterial Antifungal Anticancer | [143] | ||
| 95–96 |  | Antibacterial Antifungal Anticancer | [143] | ||
| 97 |  | Antibacterial | [160] | ||
| 98 |  | Antibacterial | [160] | ||
| Anticancer | [129] | ||||
| 99 |  | Antibacterial Antifungal Anticancer | [103] | ||
| 100 |  | Antibacterial Antifungal | [104] | ||
| 101–103 |  | Antibacterial Antifungal DNA-binding | [162] | ||
| 104 |  | Antibacterial Antifungal | [105] | ||
| Anticancer | [163] | ||||
| 105 |  | Antibacterial Antifungal | [71] | ||
| 106 |  | Antidiabetic DNA-binding | [132] | ||
| 107–109 |  | DNA binding Superoxide dismutase inhibition | [132,164] | ||
| 110–111 |  | Herbicidal | [165,166] | ||
| 112–113 |  | ||||
| 114–115 |  | ||||
| 116 |  | Antibacterial Antifungal | [105] | ||
| Au | 117–118 |  | Anticancer | [174] | |
| 119–121 |  | Anticancer | [50,176] | ||
| 122 |  | Anticancer | [50,176] | ||
| 123 |  | Anticancer | [50,176] | ||
| XII | Zn | 124 |  | Antibacterial Antifungal | [124] |
| 125 |  | Antibacterial Antifungal | [105] | ||
| 126 |  | Antibacterial Antifungal | [104] | ||
| 127 |  | Antibacterial Antifungal Anticancer | [103] | ||
| Cd | 128 |  | Antibacterial Antifungal | [71] | |
| 129 |  | Antibacterial Antifungal | [181] |
References
- World Health Organization. Model List of Essential Medicines—22nd List, 2021; World Health Organization: Geneva, Switzerland, 2021. [Google Scholar]
- Sam, S.; Ehrmann, D.A. Metformin therapy for the reproductive and metabolic consequences of polycystic ovary syndrome. Diabetologia 2017, 60, 1656–1661. [Google Scholar] [CrossRef] [PubMed]
- Masarwa, R.; Brunetti, V.C.; Aloe, S.; Henderson, M.; Platt, R.W.; Filion, K.B. Efficacy and Safety of Metformin for Obesity: A Systematic Review. Pediatrics 2021, 147, e20201610. [Google Scholar] [CrossRef] [PubMed]
- Bailey, C.J.; Day, C. Metformin: Its botanical background. Pract. Diabetes Int. 2004, 21, 115–117. [Google Scholar] [CrossRef]
- Bailey, C.J. Metformin: Historical overview. Diabetologia 2017, 60, 1566–1576. [Google Scholar] [CrossRef] [Green Version]
- Garcia, E.Y. Flumamine, a new synthetic analgesic and anti-flu drug. J. Philipp. Med. Assoc. 1950, 26, 287–293. [Google Scholar]
- Sterne, J. Du nouveau dans les antidiabetiques. La NN dimethylamine guanyl guanide (NNDG). Maroc Med. 1957, 36, 1295–1296. [Google Scholar]
- Lv, Z.; Guo, Y. Metformin and Its Benefits for Various Diseases. Front. Endocrinol. 2020, 11, 191. [Google Scholar] [CrossRef]
- Pernicova, I.; Korbonits, M. Metformin—mode of action and clinical implications for diabetes and cancer. Nat. Rev. Endocrinol. 2014, 10, 143–156. [Google Scholar] [CrossRef]
- Zi, F.; Zi, H.; Li, Y.; He, J.; Shi, Q.; Cai, Z. Metformin and cancer: An existing drug for cancer prevention and therapy. Oncol. Lett. 2018, 15, 683–690. [Google Scholar] [CrossRef] [Green Version]
- Rena, G.; Hardie, D.G.; Pearson, E.R. The mechanisms of action of metformin. Diabetologia 2017, 60, 1577–1585. [Google Scholar] [CrossRef] [Green Version]
- Viollet, B.; Guigas, B.; Sanz Garcia, N.; Leclerc, J.; Foretz, M.; Andreelli, F. Cellular and molecular mechanisms of metformin: An overview. Clin. Sci. 2012, 122, 253–270. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rena, G.; Pearson, E.R.; Sakamoto, K. Molecular mechanism of action of metformin: Old or new insights? Diabetologia 2013, 56, 1898–1906. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bost, F.; Decoux-Poullot, A.G.; Tanti, J.F.; Clavel, S. Energy disruptors: Rising stars in anticancer therapy? Oncogenesis 2016, 5, e188. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hundal, R.S.; Krssak, M.; Dufour, S.; Laurent, D.; Lebon, V.; Chandramouli, V.; Inzucchi, S.E.; Schumann, W.C.; Petersen, K.F.; Landau, B.R.; et al. Mechanism by which metformin reduces glucose production in type 2 diabetes. Diabetes 2000, 49, 2063–2069. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kirpichnikov, D.; McFarlane, S.I.; Sowers, J.R. Metformin: An update. Ann. Intern. Med. 2002, 137, 25–33. [Google Scholar] [CrossRef] [PubMed]
- Pryor, R.; Cabreiro, F. Repurposing metformin: An old drug with new tricks in its binding pockets. Biochem. J. 2015, 471, 307–322. [Google Scholar] [CrossRef] [Green Version]
- Zhao, H.; Swanson, K.D.; Zheng, B. Therapeutic Repurposing of Biguanides in Cancer. Trends Cancer 2021, 7, 714–730. [Google Scholar] [CrossRef]
- Rena, G.; Lang, C.C. Repurposing Metformin for Cardiovascular Disease. Circulation 2018, 137, 422–424. [Google Scholar] [CrossRef] [Green Version]
- Kathuria, D.; Raul, A.D.; Wanjari, P.; Bharatam, P.V. Biguanides: Species with versatile therapeutic applications. Eur. J. Med. Chem. 2021, 219, 113378. [Google Scholar] [CrossRef]
- Jong, E.C.; Nothdurft, H.D. Current Drugs for Antimalarial Chemoprophylaxis: A Review of Efficacy and Safety. J. Travel Med. 2001, 8, S48–S56. [Google Scholar] [CrossRef] [Green Version]
- Canfield, C.J.; Milhous, W.K.; Ager, A.L.; Rossan, R.N.; Sweeney, T.R.; Lewis, N.J.; Jacobus, D.P. PS-15: A Potent, Orally Active Antimalarial from a New Class of Folic Acid Antagonists. Am. J. Trop. Med. Hyg. 1993, 49, 121–126. [Google Scholar] [CrossRef] [PubMed]
- Edstein, M.D.; Bahr, S.; Kotecka, B.; Shanks, G.D.; Rieckmann, K.H. In vitro activities of the biguanide PS-15 and its metabolite, WR99210, against cycloguanil-resistant Plasmodium falciparum isolates from Thailand. Antimicrob. Agents Chemother. 1997, 41, 2300–2301. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jensen, N.P.; Ager, A.L.; Bliss, R.A.; Canfield, C.J.; Kotecka, B.M.; Rieckmann, K.H.; Terpinski, J.; Jacobus, D.P. Phenoxypropoxybiguanides, prodrugs of DHFR-inhibiting diaminotriazine antimalarials. J. Med. Chem. 2001, 44, 3925–3931. [Google Scholar] [CrossRef] [PubMed]
- Parker, G.W.; Stonehill, R.B.; De Graff, A.C., Jr. A clinical evaluation of N1, N1-anhydrobis-(beta-hydroxyethyl) biguanide-hydrochloride (ABOB) in the treatment of acute respiratory infections: A double-blind study. Antibiot. Chemother. 1962, 12, 155–158. [Google Scholar]
- Zahoránszky-Kőhalmi, G.; Siramshetty, V.B.; Kumar, P.; Gurumurthy, M.; Grillo, B.; Mathew, B.; Metaxatos, D.; Backus, M.; Mierzwa, T.; Simon, R.; et al. A Workflow of Integrated Resources to Catalyze Network Pharmacology Driven COVID-19 Research. J. Chem. Inf. Model. 2022, 62, 718–729. [Google Scholar] [CrossRef]
- Min, J.S.; Kwon, S.; Jin, Y.-H. SARS-CoV-2 RdRp Inhibitors Selected from a Cell-Based SARS-CoV-2 RdRp Activity Assay System. Biomedicines 2021, 9, 996. [Google Scholar] [CrossRef]
- Samuel, S.M.; Varghese, E.; Büsselberg, D. Therapeutic Potential of Metformin in COVID-19: Reasoning for Its Protective Role. Trends Microbiol. 2021, 29, 894–907. [Google Scholar] [CrossRef]
- McDonnell, G.; Russell, A.D. Antiseptics and disinfectants: Activity, action, and resistance. Clin. Microbiol. Rev. 1999, 12, 147–179. [Google Scholar] [CrossRef] [Green Version]
- Hübner, N.O.; Kramer, A. Review on the Efficacy, Safety and Clinical Applications of Polihexanide, a Modern Wound Antiseptic. Skin Pharmacol. Physiol. 2010, 23 (Suppl. 1), 17–27. [Google Scholar] [CrossRef]
- García Rubiño, M.E.; Carrillo, E.; Ruiz Alcalá, G.; Domínguez-Martín, A.; Marchal, J.A.; Boulaiz, H. Phenformin as an Anticancer Agent: Challenges and Prospects. Int. J. Mol. Sci. 2019, 20, 3316. [Google Scholar] [CrossRef] [Green Version]
- Aljofan, M.; Riethmacher, D. Anticancer activity of metformin: A systematic review of the literature. Future Sci. OA 2019, 5, FSO410. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hirsch, H.A.; Iliopoulos, D.; Tsichlis, P.N.; Struhl, K. Metformin Selectively Targets Cancer Stem Cells, and Acts Together with Chemotherapy to Block Tumor Growth and Prolong Remission. Cancer Res. 2009, 69, 7507–7511. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Li, Y.; Wang, M.; Zhi, P.; You, J.; Gao, J. Metformin synergistically suppress tumor growth with doxorubicin and reverse drug resistance by inhibiting the expression and function of P-glycoprotein in MCF7/ADR cells and xenograft models. Oncotarget 2017, 9, 2158–2174. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rattan, R.; Graham, R.P.; Maguire, J.L.; Giri, S.; Shridhar, V. Metformin Suppresses Ovarian Cancer Growth and Metastasis with Enhancement of Cisplatin Cytotoxicity In Vivo. Neoplasia 2011, 13, 483–491. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Graham, G.G.; Punt, J.; Arora, M.; Day, R.O.; Doogue, M.P.; Duong, J.; Furlong, T.J.; Greenfield, J.R.; Greenup, L.C.; Kirkpatrick, C.M.; et al. Clinical Pharmacokinetics of Metformin. Clin. Pharmacokinet. 2011, 50, 81–98. [Google Scholar] [CrossRef]
- Appleyard, M.V.C.L.; Murray, K.E.; Coates, P.J.; Wullschleger, S.; Bray, S.E.; Kernohan, N.M.; Fleming, S.; Alessi, D.R.; Thompson, A.M. Phenformin as prophylaxis and therapy in breast cancer xenografts. Br. J. Cancer 2012, 106, 1117–1122. [Google Scholar] [CrossRef]
- Coperchini, F.; Croce, L.; Denegri, M.; Awwad, O.; Ngnitejeu, S.T.; Magri, F.; Chiovato, L.; Rotondi, M. The anti-cancer effects of phenformin in thyroid cancer cell lines and in normal thyrocytes. Oncotarget 2019, 10, 6432–6443. [Google Scholar] [CrossRef] [Green Version]
- Cetin, M.; Sahin, S. Microparticulate and nanoparticulate drug delivery systems for metformin hydrochloride. Drug Deliv. 2016, 23, 2796–2805. [Google Scholar] [CrossRef]
- Cheng, G.; Zielonka, J.; Ouari, O.; Lopez, M.; McAllister, D.; Boyle, K.; Barrios, C.S.; Weber, J.J.; Johnson, B.D.; Hardy, M.; et al. Mitochondria-Targeted Analogues of Metformin Exhibit Enhanced Antiproliferative and Radiosensitizing Effects in Pancreatic Cancer Cells. Cancer Res. 2016, 76, 3904–3915. [Google Scholar] [CrossRef] [Green Version]
- Huttunen, K.M.; Mannila, A.; Laine, K.; Kemppainen, E.; Leppänen, J.; Vepsäläinen, J.; Järvinen, T.; Rautio, J. The First Bioreversible Prodrug of Metformin with Improved Lipophilicity and Enhanced Intestinal Absorption. J. Med. Chem. 2009, 52, 4142–4148. [Google Scholar] [CrossRef]
- Lam, T.G.; Jeong, Y.S.; Kim, S.-A.; Ahn, S.-G. New metformin derivative HL156A prevents oral cancer progression by inhibiting the insulin-like growth factor/AKT/mammalian target of rapamycin pathways. Cancer Sci. 2018, 109, 699–709. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jeong, Y.S.; Lam, T.G.; Jeong, S.; Ahn, S.G. Metformin Derivative HL156A Reverses Multidrug Resistance by Inhibiting HOXC6/ERK1/2 Signaling in Multidrug-Resistant Human Cancer Cells. Pharmaceuticals 2020, 13, 218. [Google Scholar] [CrossRef] [PubMed]
- Zhang, L.; Han, J.; Jackson, A.L.; Clark, L.N.; Kilgore, J.; Guo, H.; Livingston, N.; Batchelor, K.; Yin, Y.; Gilliam, T.P.; et al. NT1014, a novel biguanide, inhibits ovarian cancer growth in vitro and in vivo. J. Hematol. Oncol. 2016, 9, 91. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cheng, G.; Zielonka, J.; Hardy, M.; Ouari, O.; Chitambar, C.R.; Dwinell, M.B.; Kalyanaraman, B. Synergistic inhibition of tumor cell proliferation by metformin and mito-metformin in the presence of iron chelators. Oncotarget 2019, 10, 3518–3532. [Google Scholar] [CrossRef] [Green Version]
- Ward, S.A.; Watkins, W.M.; Mberu, E.; Saunders, J.E.; Koech, D.K.; Gilles, H.M.; Howells, R.E.; Breckenridge, A.M. Inter-subject variability in the metabolism of proguanil to the active metabolite cycloguanil in man. Br. J. Clin. Pharmacol. 1989, 27, 781–787. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Watkins, W.M.; Chulay, J.D.; Sixsmith, D.G.; Spencer, H.C.; Howells, R.E. A preliminary pharmacokinetic study of the antimalarial drugs, proguanil and chlorproguanil. J. Pharm. Pharmacol. 1987, 39, 261–265. [Google Scholar] [CrossRef]
- Funck-Brentano, C.; Becquemont, L.; Lenevu, A.; Roux, A.; Jaillon, P.; Beaune, P. Inhibition by omeprazole of proguanil metabolism: Mechanism of the interaction in vitro and prediction of in vivo results from the in vitro experiments. J. Pharmacol. Exp. Ther. 1997, 280, 730–738. [Google Scholar]
- Diaz, D.S.; Kozar, M.P.; Smith, K.S.; Asher, C.O.; Sousa, J.C.; Schiehser, G.A.; Jacobus, D.P.; Milhous, W.K.; Skillman, D.R.; Shearer, T.W. Role of Specific Cytochrome P450 Isoforms in the Conversion of Phenoxypropoxybiguanide Analogs in Human Liver Microsomes to Potent Antimalarial Dihydrotriazines. Drug Metab. Dispos. 2008, 36, 380. [Google Scholar] [CrossRef]
- Babak, M.V.; Chong, K.R.; Rapta, P.; Zannikou, M.; Tang, H.M.; Reichert, L.; Chang, M.R.; Kushnarev, V.; Heffeter, P.; Meier-Menches, S.M.; et al. Interfering with Metabolic Profile of Triple-Negative Breast Cancers Using Rationally Designed Metformin Prodrugs. Angew. Chem. Int. Ed. 2021, 60, 13405–13413. [Google Scholar] [CrossRef]
- Markowicz-Piasecka, M.; Sikora, J.; Mateusiak, Ł.; Mikiciuk-Olasik, E.; Huttunen, K.M. Metformin and Its Sulfenamide Prodrugs Inhibit Human Cholinesterase Activity. Oxid. Med. Cell. Longev. 2017, 2017, 7303096. [Google Scholar] [CrossRef] [Green Version]
- Markowicz-Piasecka, M.; Huttunen, K.M.; Mikiciuk-Olasik, E.; Sikora, J. Biocompatible sulfenamide and sulfonamide derivatives of metformin can exert beneficial effects on plasma haemostasis. Chem.-Biol. Interact. 2018, 280, 15–27. [Google Scholar] [CrossRef] [PubMed]
- Huttunen, K.M.; Leppänen, J.; Vepsäläinen, J.; Sirviö, J.; Laine, K.; Rautio, J. In vitro and in vivo evaluation of a sulfenamide prodrug of basic metformin. J. Pharm. Sci. 2012, 101, 2854–2860. [Google Scholar] [CrossRef] [PubMed]
- Rathke, B. Ueber Biguanid. Ber. Dtsch. Chem. Ges. 1879, 12, 776–784. [Google Scholar] [CrossRef] [Green Version]
- Ray, P. Complex Compounds of Biguanides and Guanylureas with Metallic Elements. Chem. Rev. 1961, 61, 313–359. [Google Scholar] [CrossRef]
- Ray, R.K.; Kauffman, G.B.; Ray, R.K. Metal and Non-Metal Biguanide Complexes; New Age International: New Delhi, India, 1999. [Google Scholar]
- Slotta, K.H.; Tschesche, R.; Über Biguanide, I. Zur Konstitution der Schwermetall-Komplexverbindungen des Biguanids. Ber. Dtsch. Chem. Ges. 1929, 62, 1390–1398. [Google Scholar] [CrossRef]
- Logie, L.; Harthill, J.; Patel, K.; Bacon, S.; Hamilton, D.L.; Macrae, K.; McDougall, G.; Wang, H.-H.; Xue, L.; Jiang, H.; et al. Cellular Responses to the Metal-Binding Properties of Metformin. Diabetes 2012, 61, 1423–1433. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Repiščák, P.; Erhardt, S.; Rena, G.; Paterson, M.J. Biomolecular Mode of Action of Metformin in Relation to Its Copper Binding Properties. Biochemistry 2014, 53, 787–795. [Google Scholar] [CrossRef] [PubMed]
- Sweeney, D.; Raymer, M.L.; Lockwood, T.D. Antidiabetic and antimalarial biguanide drugs are metal-interactive antiproteolytic agents. Biochem. Pharmacol. 2003, 66, 663–677. [Google Scholar] [CrossRef]
- Abdelrahman, S.; Alghrably, M.; Campagna, M.; Hauser, C.A.; Jaremko, M.; Lachowicz, J.I. Metal Complex Formation and Anticancer Activity of Cu(I) and Cu(II) Complexes with Metformin. Molecules 2021, 26, 4730. [Google Scholar] [CrossRef]
- Babak, M.V.; Ahn, D. Modulation of Intracellular Copper Levels as the Mechanism of Action of Anticancer Copper Complexes: Clinical Relevance. Biomedicines 2021, 9, 852. [Google Scholar] [CrossRef]
- Heinrich, J.; Bossak-Ahmad, K.; Riisom, M.; Haeri, H.H.; Steel, T.R.; Hergl, V.; Langhans, A.; Schattschneider, C.; Barrera, J.; Jamieson, S.M.F.; et al. Incorporation of β-Alanine in Cu(II) ATCUN Peptide Complexes Increases ROS Levels, DNA Cleavage and Antiproliferative Activity. Chem. Eur. J. 2021, 27, 18093–18102. [Google Scholar] [CrossRef] [PubMed]
- Ohui, K.; Stepanenko, I.; Besleaga, I.; Babak, M.V.; Stafi, R.; Darvasiova, D.; Giester, G.; Pósa, V.; Enyedy, E.A.; Vegh, D.; et al. Triapine Derivatives Act as Copper Delivery Vehicles to Induce Deadly Metal Overload in Cancer Cells. Biomolecules 2020, 10, 1336. [Google Scholar] [CrossRef] [PubMed]
- Ohui, K.; Afanasenko, E.; Bacher, F.; Ting, R.L.X.; Zafar, A.; Blanco-Cabra, N.; Torrents, E.; Dömötör, O.; May, N.V.; Darvasiova, D.; et al. New Water-Soluble Copper(II) Complexes with Morpholine–Thiosemicarbazone Hybrids: Insights into the Anticancer and Antibacterial Mode of Action. J. Med. Chem. 2019, 62, 512–530. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Müller, S.; Versini, A.; Sindikubwabo, F.; Belthier, G.; Niyomchon, S.; Pannequin, J.; Grimaud, L.; Cañeque, T.; Rodriguez, R. Metformin reveals a mitochondrial copper addiction of mesenchymal cancer cells. PLoS ONE 2018, 13, e0206764. [Google Scholar]
- Fricker, S.P. The therapeutic application of lanthanides. Chem. Soc. Rev. 2006, 35, 524–533. [Google Scholar] [CrossRef]
- Refat, M.S.; Al-Azab, F.M.; Al-Maydama, H.M.; Amin, R.R.; Jamil, Y.M.; Kobeasy, M.I. Synthesis, spectroscopic and antimicrobial studies of La(III), Ce(III), Sm(III) and Y(III) Metformin HCl chelates. Spectrochim. Acta A Mol. Biomol. Spectrosc. 2015, 142, 392–404. [Google Scholar] [CrossRef]
- Duan, Z.-L.; Zeng, Z.-Z. Synthesis and Study of Antidiabetic Properties of the Neodymium Complexes with N5-[o-(un)Substituted Benzoyl]-N1,N1-dimethylbiguanide. Chin. J. Chem. 2007, 25, 1919–1923. [Google Scholar] [CrossRef]
- Mahmoud, M.A.; Abdel-Salam, E.T.; Abdel Aal, N.F.; Showery, Z.M.; Sallam, S.A. Dy(III) complexes of metformin Schiff-bases as glucose probe: Synthesis, spectral, and thermal properties. J. Coord. Chem. 2019, 72, 749–769. [Google Scholar] [CrossRef]
- El-Shwiniy, W.H.; Abbass, L.M.; Sadeek, S.A.; Zordok, W.A. Synthesis, Structure, and Biological Activity of Some Transition Metal Complexes with the Mixed Ligand of Metformin and 1,4-Diacetylbenzene. Russ. J. Gen. Chem. 2020, 90, 483–488. [Google Scholar] [CrossRef] [Green Version]
- Jangra, S.L.; Stalin, K.; Dilbaghi, N.; Kumar, S.; Tawale, J.; Singh, S.P.; Pasricha, R. Antimicrobial activity of zirconia (ZrO2) nanoparticles and zirconium complexes. J. Nanosci. Nanotechnol. 2012, 12, 7105–7112. [Google Scholar] [CrossRef]
- Tabassum, N.; Kumar, D.; Verma, D.; Bohara, R.A.; Singh, M.P. Zirconium oxide (ZrO2) nanoparticles from antibacterial activity to cytotoxicity: A next-generation of multifunctional nanoparticles. Mater. Today Commun. 2021, 26, 102156. [Google Scholar] [CrossRef]
- Scior, T.; Guevara-Garcia, J.A.; Do, Q.-T.; Bernard, P.; Laufer, S. Why Antidiabetic Vanadium Complexes are Not in the Pipeline of "Big Pharma" Drug Research? A Critical Review. Curr. Med. Chem. 2016, 23, 2874–2891. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sakurai, H. A new concept: The use of vanadium complexes in the treatment of diabetes mellitus. Chem. Rec. 2002, 2, 237–248. [Google Scholar] [CrossRef] [PubMed]
- Woo, L.C.Y.; Yuen, V.G.; Thompson, K.H.; McNeill, J.H.; Orvig, C. Vanadyl–biguanide complexes as potential synergistic insulin mimics. J. Inorg. Biochem. 1999, 76, 251–257. [Google Scholar] [CrossRef]
- Conconi, M.T.; DeCarlo, E.; Vigolo, S.; Grandi, C.; Bandoli, G.; Sicolo, N.; Tamagno, G.; Parnigotto, P.P.; Nussdorfer, G.G. Effects of some vanadyl coordination compounds on the in vitro insulin release from rat pancreatic islets. Horm. Metab. Res. 2003, 35, 402–406. [Google Scholar] [PubMed]
- Lu, L.; Gao, X.; Zhu, M.; Wang, S.; Wu, Q.; Xing, S.; Fu, X.; Liu, Z.; Guo, M. Exploration of biguanido-oxovanadium complexes as potent and selective inhibitors of protein tyrosine phosphatases. Biometals 2012, 25, 599–610. [Google Scholar] [CrossRef]
- Mahmoud, M.A.; Zaitone, S.A.; Ammar, A.M.; Sallam, S.A. Synthesis, spectral, thermal and insulin-enhancing properties of oxovanadium(IV) complexes of metformin Schiff-bases. J. Therm. Anal. Calorim. 2017, 128, 957–969. [Google Scholar] [CrossRef]
- Samart, N.; Saeger, J.; Haller, K.J.; Aureliano, M.; Crans, D.C. Interaction of Decavanadate with Interfaces and Biological Model Membrane Systems: Characterization of Soft Oxometalate Systems. J. Mol. Eng. Mat. 2014, 2, 1440007. [Google Scholar] [CrossRef]
- Chatkon, A.; Chatterjee, P.B.; Sedgwick, M.A.; Haller, K.J.; Crans, D.C. Counterion Affects Interaction with Interfaces: The Antidiabetic Drugs Metformin and Decavanadate. Eur. J. Inorg. Chem. 2013, 2013, 1859–1868. [Google Scholar] [CrossRef]
- Treviño, S.; Sánchez-Lara, E.; Sarmiento-Ortega, V.E.; Sánchez-Lombardo, I.; Flores-Hernández, J.; Pérez-Benítez, A.; Brambila-Colombres, E.; González-Vergara, E. Hypoglycemic, lipid-lowering and metabolic regulation activities of metforminium decavanadate (H2Metf)3[V10O28]·8H2O using hypercaloric-induced carbohydrate and lipid deregulation in Wistar rats as biological model. J. Inorg. Biochem. 2015, 147, 85–92. [Google Scholar] [CrossRef]
- Sánchez-Lara, E.; Treviño, S.; Sánchez-Gaytán, B.L.; Sánchez-Mora, E.; Eugenia Castro, M.; Meléndez-Bustamante, F.J.; Méndez-Rojas, M.A.; González-Vergara, E. Decavanadate Salts of Cytosine and Metformin: A Combined Experimental-Theoretical Study of Potential Metallodrugs Against Diabetes and Cancer. Front. Chem. 2018, 6, 402. [Google Scholar] [CrossRef] [Green Version]
- Sánchez-Lombardo, I.; Sánchez-Lara, E.; Pérez-Benítez, A.; Mendoza, Á.; Bernès, S.; González-Vergara, E. Synthesis of Metforminium(2+) Decavanadates—Crystal Structures and Solid-State Characterization. Eur. J. Inorg. Chem. 2014, 2014, 4581–4588. [Google Scholar] [CrossRef]
- Treviño, S.; Velázquez-Vázquez, D.; Sánchez-Lara, E.; Diaz-Fonseca, A.; Flores-Hernandez, J.Á.; Pérez-Benítez, A.; Brambila-Colombres, E.; González-Vergara, E. Metforminium Decavanadate as a Potential Metallopharmaceutical Drug for the Treatment of Diabetes Mellitus. Oxid. Med. Cell. Longev. 2016, 2016, 6058705. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Treviño, S.; González-Vergara, E. Metformin-decavanadate treatment ameliorates hyperglycemia and redox balance of the liver and muscle in a rat model of alloxan-induced diabetes. N. J. Chem. 2019, 43, 17850–17862. [Google Scholar] [CrossRef]
- Wahl, D.; Solon-Biet, S.M.; Wang, Q.P.; Wali, J.A.; Pulpitel, T.; Clark, X.; Raubenheimer, D.; Senior, A.M.; Sinclair, D.A.; Cooney, G.J.; et al. Comparing the Effects of Low-Protein and High-Carbohydrate Diets and Caloric Restriction on Brain Aging in Mice. Cell. Rep. 2018, 25, 2234–2243.e6. [Google Scholar] [CrossRef] [Green Version]
- Diaz, A.; Muñoz-Arenas, G.; Venegas, B.; Vázquez-Roque, R.; Flores, G.; Guevara, J.; Gonzalez-Vergara, E.; Treviño, S. Metforminium Decavanadate (MetfDeca) Treatment Ameliorates Hippocampal Neurodegeneration and Recognition Memory in a Metabolic Syndrome Model. Neurochem. Res. 2021, 46, 1151–1165. [Google Scholar] [CrossRef]
- Evangelou, A.M. Vanadium in cancer treatment. Crit. Rev. Oncol. Hematol. 2002, 42, 249–265. [Google Scholar] [CrossRef]
- Kioseoglou, E.; Petanidis, S.; Gabriel, C.; Salifoglou, A. The chemistry and biology of vanadium compounds in cancer therapeutics. Coord. Chem. Rev. 2015, 301–302, 87–105. [Google Scholar] [CrossRef]
- Shekhar, B.; Vasantha, P.; Kumar, B.S.; Lakshmi, A. Multispectroscopic DNA interaction and Docking studies. Appl. Organomet. Chem. 2018, 32, e4254. [Google Scholar] [CrossRef]
- Adam, A.M.; Sharshar, T.; Mohamed, M.A.; Ibrahim, O.B.; Refat, M.S. Study of chemical bonding, physical and biological effect of metformin drug as an organized medicine for diabetes patients with chromium(III) and vanadium(IV) ions. Spectrochim. Acta A Mol. Biomol. Spectrosc. 2015, 149, 323–332. [Google Scholar] [CrossRef] [PubMed]
- Levina, A.; Lay, P.A. Chapter 9—Redox chemistry and biological activities of chromium(III) complexes. In The Nutritional Biochemistry of Chromium (III), 2nd ed.; Vincent, J.B., Ed.; Elsevier: Amsterdam, The Netherlands, 2019; pp. 281–321. [Google Scholar]
- Suksomboon, N.; Poolsup, N.; Yuwanakorn, A. Systematic review and meta-analysis of the efficacy and safety of chromium supplementation in diabetes. J. Clin. Pharm. Ther. 2014, 39, 292–306. [Google Scholar] [CrossRef] [PubMed]
- Lukaski, H.C. Chapter 2—Effects of chromium(III) as a nutritional supplement. In The Nutritional Biochemistry of Chromium (III), 2nd ed.; Vincent, J.B., Ed.; Elsevier: Amsterdam, The Netherlands, 2019; pp. 61–77. [Google Scholar]
- Peng, M.; Yang, X. Controlling diabetes by chromium complexes: The role of the ligands. J. Inorg. Biochem. 2015, 146, 97–103. [Google Scholar] [CrossRef] [PubMed]
- Dong, J.; Liu, B.; Liang, G.; Yang, B. Synthesis, biological activity and toxicity of chromium(III) metformin complex as potential insulin-mimetic agent in C57BL/6 mice. J. Coord. Chem. 2018, 71, 1526–1541. [Google Scholar] [CrossRef]
- Dong, J.-L.; Wen, B.; Song, Z.; Chai, J.; Liu, B.; Tian, W.-j.; Liang, G.; Yang, B.-S. Potential antidiabetic molecule involving a new chromium(III) complex of dipicolinic and metformin as a counter ion: Synthesis, structure, spectroscopy, and bioactivity in mice. Arab. J. Chem. 2021, 14, 103236. [Google Scholar] [CrossRef]
- Mahmoud, M.A.; Zaitone, S.A.; Ammar, A.M.; Sallam, S.A. Synthesis, structure and antidiabetic activity of chromium(III) complexes of metformin Schiff-bases. J. Mol. Struct. 2016, 1108, 60–70. [Google Scholar] [CrossRef]
- Shekhar, B.; Vasantha, P.; Kumar, B.S.; Lakshmi, A.; Vuradi, R.K.; Satyanarayana, S. Chromium-metformin ternary complexes: Thermal, DNA interaction and Docking studies. Appl. Organomet. Chem. 2019, 33, e5086. [Google Scholar] [CrossRef]
- Saha, T.; Kumar, P.; Sepay, N.; Ganguly, D.; Tiwari, K.; Mukhopadhyay, K.; Das, S. Multitargeting Antibacterial Activity of a Synthesized Mn2+ Complex of Curcumin on Gram-Positive and Gram-Negative Bacterial Strains. ACS Omega 2020, 5, 16342–16357. [Google Scholar] [CrossRef]
- Huang, X.-F.; Zhu, Y.-L.; Tang, L. Synthesis, characterization, and antibacterial activity of a manganese(II) complex of triaryltriazole. J. Coord. Chem. 2011, 64, 1602–1607. [Google Scholar] [CrossRef]
- Olar, R.; Badea, M.; Marinescu, D.; Chifiriuc, M.C.; Bleotu, C.; Grecu, M.N.; Iorgulescu, E.E.; Lazar, V. N,N-dimethylbiguanide complexes displaying low cytotoxicity as potential large spectrum antimicrobial agents. Eur. J. Med. Chem. 2010, 45, 3027–3034. [Google Scholar] [CrossRef]
- Olar, R.; Badea, M.; Marinescu, D.; Chifiriuc, C.-M.; Bleotu, C.; Grecu, M.N.; Iorgulescu, E.E.; Bucur, M.; Lazar, V.; Finaru, A. Prospects for new antimicrobials based on N,N-dimethylbiguanide complexes as effective agents on both planktonic and adhered microbial strains. Eur. J. Med. Chem. 2010, 45, 2868–2875. [Google Scholar] [CrossRef]
- Alsaif, F.; Refat, M. Synthesis, spectroscopic, and thermal investigation of transition and non-transition complexes of metformin as potential insulin-mimetic agents. J. Therm. Anal. Calorim. 2013, 111, 2079–2096. [Google Scholar] [CrossRef]
- Boschi, A.; Uccelli, L.; Martini, P. A picture of modern Tc-99m radiopharmaceuticals: Production, chemistry, and applications in molecular imaging. Appl. Sci. 2019, 9, 2526. [Google Scholar] [CrossRef] [Green Version]
- Häfliger, P.; Agorastos, N.; Spingler, B.; Georgiev, O.; Viola, G.; Alberto, R. Induction of DNA-Double-Strand Breaks by Auger Electrons from 99mTc Complexes with DNA-Binding Ligands. ChemBioChem 2005, 6, 414–421. [Google Scholar] [CrossRef] [PubMed]
- Mondal, S.; Samajdar, R.N.; Mukherjee, S.; Bhattacharyya, A.J.; Bagchi, B. Unique Features of Metformin: A Combined Experimental, Theoretical, and Simulation Study of Its Structure, Dynamics, and Interaction Energetics with DNA Grooves. J. Phys. Chem. 2018, 122, 2227–2242. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Miljanić, S.; DijanošiĆ, A.; Landeka, K.; Stojković, M.R.; Piantanida, I. Binding of a Phenanthridine-Biguanide Derivative with DNA/RNA Polynucleotides Studied by Surface-Enhanced Raman Spectroscopy (SERS). Appl. Spectrosc. 2012, 66, 82–89. [Google Scholar] [CrossRef]
- Fuks, L.; Gniazdowska, E.; Koźmiński, P.; Herdzik-Koniecko, I. Technetium(I) tricarbonyl complexes: Potential precursors of the radiopharmaceuticals. Part II: Phenethylbiguanide (phenformin). J. Radioanal. Nucl. Chem. 2012, 292, 395–399. [Google Scholar] [CrossRef]
- Wani, W.A.; Baig, U.; Shreaz, S.; Shiekh, R.A.; Iqbal, P.F.; Jameel, E.; Ahmad, A.; Mohd-Setapar, S.H.; Mushtaque, M.; Hun, L.T. Recent advances in iron complexes as potential anticancer agents. N. J. Chem. 2016, 40, 1063–1090. [Google Scholar] [CrossRef]
- Baecker, D.; Sesli, Ö.; Knabl, L.; Huber, S.; Orth-Höller, D.; Gust, R. Investigating the antibacterial activity of salen/salophene metal complexes: Induction of ferroptosis as part of the mode of action. Eur. J. Med. Chem. 2021, 209, 112907. [Google Scholar] [CrossRef]
- Hille, A.; Ott, I.; Kitanovic, A.; Kitanovic, I.; Alborzinia, H.; Lederer, E.; Wölfl, S.; Metzler-Nolte, N.; Schäfer, S.; Sheldrick, W.S.; et al. [N,N′-Bis(salicylidene)-1,2-phenylenediamine]metal complexes with cell death promoting properties. J. Biol. Inorg. Chem. 2009, 14, 711–725. [Google Scholar] [CrossRef]
- Badea, M.; Crasanda, A.-M.; Chifiriuc, M.C.; Marutescu, L.; Lazar, V.; Marinescu, D.; Olar, R. Synthesis, spectral and thermal study on new Fe(III) complexes with N,N-dimethylbiguanide as antibacterial agents. J. Therm. Anal. Calorim. 2013, 111, 1743–1751. [Google Scholar] [CrossRef]
- Lee, S.Y.; Kim, C.Y.; Nam, T.-G. Ruthenium complexes as anticancer agents: A brief history and perspectives. Drug Des. Dev. Ther. 2020, 14, 5375. [Google Scholar] [CrossRef] [PubMed]
- Osypenko, A.; Ashraf, A.; Pozhydaiev, V.; Babak, M.V.; Hanif, M. Organometallic Chemistry of Anticancer Ruthenium and Osmium Complexes. In Reference Module in Chemistry, Molecular Sciences and Chemical Engineering; Elsevier: Amsterdam, The Netherlands, 2021. [Google Scholar]
- Babak, M.V.; Ang, W.H. Multinuclear Organometallic Ruthenium-Arene Complexes for Cancer Therapy. Met. Ions Life Sci. 2018, 18, 171–198. [Google Scholar]
- Klajner, M.; Licona, C.; Fetzer, L.; Hebraud, P.; Mellitzer, G.; Pfeffer, M.; Harlepp, S.; Gaiddon, C. Subcellular Localization and Transport Kinetics of Ruthenium Organometallic Anticancer Compounds in Living Cells: A Dose-Dependent Role for Amino Acid and Iron Transporters. Inorg. Chem. 2014, 53, 5150–5158. [Google Scholar] [CrossRef]
- Trondl, R.; Heffeter, P.; Kowol, C.R.; Jakupec, M.A.; Berger, W.; Keppler, B.K. NKP-1339, the first ruthenium-based anticancer drug on the edge to clinical application. Chem. Sci. 2014, 5, 2925–2932. [Google Scholar] [CrossRef] [Green Version]
- Burris, H.A.; Bakewell, S.; Bendell, J.C.; Infante, J.; Jones, S.F.; Spigel, D.R.; Weiss, G.J.; Ramanathan, R.K.; Ogden, A.; Von Hoff, D. Safety and activity of IT-139, a ruthenium-based compound, in patients with advanced solid tumours: A first-in-human, open-label, dose-escalation phase I study with expansion cohort. ESMO Open 2016, 1, e000154. [Google Scholar] [CrossRef] [Green Version]
- O’Kane, G.M.; Spratlin, J.L.; Kavan, P.; Goodwin, R.A.; McWhirter, E.; Thompson, D.; Jones, M.; McAllister, E.R.; Machado, A.; Lemmerick, Y.; et al. BOLD-100-001 (TRIO039): A phase Ib dose-escalation study of BOLD-100 in combination with FOLFOX chemotherapy in patients with advanced gastrointestinal solid tumors. J. Clin. Oncol. 2021, 39, TPS145. [Google Scholar] [CrossRef]
- Sullivan, M.; Holtkamp, H.; Meier-Menches, S.; Hartinger, C. Chapter Ten—The Analysis of Therapeutic Metal Complexes and Their Biomolecular Interactions. In Inorganic and Organometallic Transition Metal Complexes with Biological Molecules and Living Cells; Elsevier: Amsterdam, The Netherlands, 2017; pp. 355–386. [Google Scholar]
- Gopalakrishnan, D.; Ganeshpandian, M.; Loganathan, R.; Bhuvanesh, N.S.P.; Sabina, X.J.; Karthikeyan, J. Water soluble Ru(II)–arene complexes of the antidiabetic drug metformin: DNA and protein binding, molecular docking, cytotoxicity and apoptosis-inducing activity. RSC Adv. 2017, 7, 37706–37719. [Google Scholar] [CrossRef] [Green Version]
- Olar, R.; Badea, M.; Cristurean, E.; Lazar, V.; Cernat, R.; Balotescu, C. Thermal behavior, spectroscopic and biological characterization of Co(II), Zn(II), Pd(II) and Pt(II) complexes with N,N-dimethylbiguanide. J. Therm. Anal. Calorim. 2005, 80, 451–455. [Google Scholar] [CrossRef]
- Sharma, S.S.; Ramani, J.V.; Dalwadi, D.P.; Bhalodia, J.J.; Patel, N.K.; Patel, D.D.; Patel, R.K. New Ternary Transition Metal Complexes of 2-{[(2-aminophenyl)imino]methyl}Phenol and Metformin: Synthesis, Characterization and Antimicrobial Activity. J. Chem. 2011, 8, 723491. [Google Scholar] [CrossRef] [Green Version]
- Ceramella, J.; Iacopetta, D.; Catalano, A.; Cirillo, F.; Lappano, R.; Sinicropi, M.S. A Review on the Antimicrobial Activity of Schiff Bases: Data Collection and Recent Studies. Antibiotics 2022, 11, 191. [Google Scholar] [CrossRef]
- Kirin, V.P.; Demkin, A.G.; Sukhikh, T.S.; Ilyicheva, T.N.; Maksakov, V.A. Cobalt complexes with biguanide derivatives—Synthesis, structure and antiviral activity. J. Mol. Struct. 2022, 1250, 131486. [Google Scholar] [CrossRef]
- Kirin, V.P.; Demkin, A.G.; Smolentsev, A.I.; Il’icheva, T.N.; Maksakov, V.A. Cobalt(III) complexes with biguanide derivatives: Synthesis, structures, and antiviral activity. Russ. J. Coord. Chem. 2016, 42, 260–266. [Google Scholar] [CrossRef]
- Villamizar-Delgado, S.; Porras-Osorio, L.M.; Piñeros, O.; Ellena, J.; Balcazar, N.; Varela-Miranda, R.E.; D’Vries, R.F. Biguanide–transition metals complexes as potential drug for hyperglycemia treatment. RSC Adv. 2020, 10, 22856–22863. [Google Scholar] [CrossRef]
- Munteanu, C.R.; Suntharalingam, K. Advances in cobalt complexes as anticancer agents. Dalton Trans. 2015, 44, 13796–13808. [Google Scholar] [CrossRef] [PubMed]
- Vasantha, P.; Kumar, B.S.; Shekhar, B.; Lakshmi, A. Cobalt(II)-metformin complexes containing α-diimine/α-diamine as auxiliary ligand: DNA binding properties: Cobalt (II)-metformin ternary complexes—DNA binding properties. Appl. Organomet. Chem. 2017, 32, e4074. [Google Scholar]
- Rajeshwari, K.; Anantha Lakshmi, P.V.; Archana, J.; Sumakanth, M. Ternary Cobalt(II), Nickel(II), and Copper(II) complexes containing metformin and ethylenediamine: Synthesis, characterization, thermal, in vitro DNA binding, in silico molecular docking, and in vivo antihyperglycemic studies. Appl. Organomet. Chem. 2021, 35, e6100. [Google Scholar] [CrossRef]
- Refat, M.S.; Kobeasy, M.I. Synthesis, spectroscopic, thermal, free radical scavenging ability, and antitumor activity studies of cobalt(II) metformin complex. Russ. J. Gen. Chem. 2014, 84, 767–774. [Google Scholar] [CrossRef]
- Campanella, L.; Favero, G.; Osinsky, P.S.; Sigan, L.A.; Tomassetti, M. In Vitro Antioxidant Capacity vs In Vivo Antimetastatic Effect of Anticancer Cobalt Complexes. Curr. Pharm. Anal. 2008, 4, 44–52. [Google Scholar] [CrossRef]
- Choi, S.W.; Ho, C.K. Antioxidant properties of drugs used in Type 2 diabetes management: Could they contribute to, confound or conceal effects of antioxidant therapy? Redox Rep. 2018, 23, 1–24. [Google Scholar] [CrossRef]
- Leung, C.-H.; Zhong, H.-J.; Chan, D.S.-H.; Ma, D.-L. Bioactive iridium and rhodium complexes as therapeutic agents. Coord. Chem. Rev. 2013, 257, 1764–1776. [Google Scholar] [CrossRef]
- Chen, F.; Moat, J.; McFeely, D.; Clarkson, G.; Hands-Portman, I.J.; Furner-Pardoe, J.P.; Harrison, F.; Dowson, C.G.; Sadler, P.J. Biguanide Iridium(III) Complexes with Potent Antimicrobial Activity. J. Med. Chem. 2018, 61, 7330–7344. [Google Scholar] [CrossRef] [PubMed]
- Yang, J.; Fang, H.-J.; Cao, Q.; Mao, Z.-W. The design of cyclometalated iridium(III)–metformin complexes for hypoxic cancer treatment. Chem. Commun. 2021, 57, 1093. [Google Scholar] [CrossRef] [PubMed]
- Sheikhshoaie, I.; Lotfi, N.; Sieler, J.; Krautscheid, H.; Khaleghi, M. Synthesis, structures and antimicrobial activities of nickel(II) and zinc(II) diaminomaleonitrile-based complexes. Transit. Met. Chem. 2018, 43, 555–562. [Google Scholar] [CrossRef] [Green Version]
- Das, A.; Rajeev, A.; Bhunia, S.; Arunkumar, M.; Chari, N.; Sankaralingam, M. Synthesis, characterization and antimicrobial activity of nickel(II) complexes of tridentate N3 ligands. Inorg. Chim. Acta 2021, 526, 120515. [Google Scholar] [CrossRef]
- Ashna, M.H.; Behzad, M.; Salehi, M. Nickel versus copper: Enhanced antibacterial activity in a series of new nickel(II) Schiff base complexes. J. Coord. Chem. 2016, 69, 190–198. [Google Scholar] [CrossRef]
- Elshami, F.I.; Ramadan, A.E.-M.M.; Ibrahim, M.M.; El-Mehasseb, I.M.; Al-Juaid, S.; Shaban, S.Y. Metformin Containing Nickel(II) Complexes: Synthesis, Structural Characterization, Binding and Kinetic Interactions with BSA, Antibacterial and in-vitro Cytotoxicity Studies. Appl. Organomet. Chem. 2020, 34, e5437. [Google Scholar] [CrossRef]
- Badea, M.; Grecu, M.N.; Chifiriuc, M.C.; Bleotu, C.; Popa, M.; Iorgulescu, E.E.; Avram, S.; Uivarosi, V.; Munteanu, A.-C.; Ghica, D.; et al. Insight on Ni(II) and Cu(II) complexes of biguanide derivatives developed as effective antimicrobial and antitumour agents. Appl. Organomet. Chem. 2021, 35, e6155. [Google Scholar] [CrossRef]
- Rajeshwari, K.; Vasantha, P.; Kumar, B.S.; Shekhar, B.; Lakshmi, P.V.A. Water Soluble Nickel-metformin ternary complexes: Thermal, DNA binding and molecular docking studies. Appl. Organomet. Chem. 2020, 34, e5351. [Google Scholar] [CrossRef]
- Badea, M.; Iosub, E.; Chifiriuc, C.M.; Marutescu, L.; Iorgulescu, E.E.; Lazar, V.; Marinescu, D.; Bleotu, C.; Olar, R. Thermal, spectral, electrochemical and biologic characterization of new Pd (II) complexes with ligands bearing biguanide moieties. J. Therm. Anal. Calorim. 2013, 111, 1753–1761. [Google Scholar] [CrossRef]
- Karami, K.; Parsianrad, F.; Alinaghi, M.; Amirghofran, Z. Cyclopalladated complexes containing metformin and benzylamine derivatives: Synthesis, characterization, binding interactions with DNA and BSA, in vitro cytotoxicity studies. Inorg. Chim. Acta. 2017, 467, 46–55. [Google Scholar] [CrossRef]
- Ryabov, A.D. Cyclopalladated compounds as enzyme prototypes and anticancer drugs. In Palladacycles. Synthesis, Characterization and Applications; Dupont, J., Pfeffer, M., Eds.; WILEY-VCH Verlag GmbH & Co. KGaA: Weinheim, Germany, 2008; pp. 307–339. [Google Scholar]
- Serrano, F.A.; Matsuo, A.L.; Monteforte, P.T.; Bechara, A.; Smaili, S.S.; Santana, D.P.; Rodrigues, T.; Pereira, F.V.; Silva, L.S.; Machado, J.; et al. A cyclopalladated complex interacts with mitochondrial membrane thiol-groups and induces the apoptotic intrinsic pathway in murine and cisplatin-resistant human tumor cells. BMC Cancer 2011, 11, 296. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Babak, M.V.; Pfaffeneder-Kmen, M.; Meier-Menches, S.M.; Legina, M.S.; Theiner, S.; Licona, C.; Orvain, C.; Hejl, M.; Hanif, M.; Jakupec, M.A.; et al. Rollover Cyclometalated Bipyridine Platinum Complexes as Potent Anticancer Agents: Impact of the Ancillary Ligands on the Mode of Action. Inorg. Chem. 2018, 57, 2851–2864. [Google Scholar] [CrossRef]
- Jin, S.; Guo, Y.; Guo, Z.; Wang, X. Monofunctional Platinum(II) Anticancer Agents. Pharmaceuticals 2021, 14, 133. [Google Scholar] [CrossRef] [PubMed]
- Kostova, I. Platinum complexes as anticancer agents. Recent Pat. Anticancer Drug Discov. 2006, 1, 1–22. [Google Scholar] [CrossRef] [PubMed]
- Xu, Z.; Wang, Z.; Deng, Z.; Zhu, G. Recent advances in the synthesis, stability, and activation of platinum(IV) anticancer prodrugs. Coord. Chem. Rev. 2021, 442, 213991. [Google Scholar] [CrossRef]
- Gibson, D. Platinum(IV) anticancer agents; are we en route to the holy grail or to a dead end? J. Inorg. Biochem. 2021, 217, 111353. [Google Scholar] [CrossRef]
- Viossat, B.; Dung, N.-H.; Rodier, N.; Bentefrit, F. Chlorure de cis-Chloro(diméthyl sulfoxyde)(metformine)platine(II). Acta Crystallogr. C Struct. Chem. 1995, 51, 878–880. [Google Scholar] [CrossRef] [Green Version]
- Bentefrit, F.; Morgant, G.; Viossat, B.; Leonce, S.; Guilbaud, N.; Pierre, A.; Atassi, G.; Dung, N.H. Synthesis and antitumor activity of the metformin platinum(IV) complex. Crystal structure of the tetrachloro(metformin)platinum(IV) dimethylsulfoxide solvate. J. Inorg. Biochem. 1997, 68, 53–59. [Google Scholar] [CrossRef]
- Salah, I.; Parkin, I.P.; Allan, E. Copper as an antimicrobial agent: Recent advances. RSC Adv. 2021, 11, 18179–18186. [Google Scholar] [CrossRef]
- Salgado, C.D.; Sepkowitz, K.A.; John, J.F.; Cantey, J.R.; Attaway, H.H.; Freeman, K.D.; Sharpe, P.A.; Michels, H.T.; Schmidt, M.G. Copper Surfaces Reduce the Rate of Healthcare-Acquired Infections in the Intensive Care Unit. Infect. Control Hosp. Epidemiol. 2013, 34, 479–486. [Google Scholar] [CrossRef] [Green Version]
- Zhang, X.; Zhang, Z.; Shu, Q.; Xu, C.; Zheng, Q.; Guo, Z.; Wang, C.; Hao, Z.; Liu, X.; Wang, G.; et al. Copper Clusters: An Effective Antibacterial for Eradicating Multidrug-Resistant Bacterial Infection In Vitro and In Vivo. Adv. Funct. Mater. 2021, 31, 2008720. [Google Scholar] [CrossRef]
- Gao, J. A Weak Hydrolytical Copper(II) Complex Derived from Condensation of N,N-Dimethylbiguanide with 2-Pyridinecarbaldehyde Synthesis, Crystal Structure and Biological Activity. Synth. React. Inorg. Met.-Org. Nano-Met. Chem. 2007, 37, 621–625. [Google Scholar] [CrossRef]
- Olar, R.; Badea, M.; Grecu, M.N.; Marinescu, D.; Lazar, V.; Balotescu, C. Copper(II) complexes with N,N-dimethylbiguanide. J. Therm. Anal. Calorim. 2008, 92, 239–243. [Google Scholar] [CrossRef]
- Lemoine, P.; Chiadmi, M.; Bissery, V.; Tomas, A.; Viossat, B. Les Composés de la Metformine avec les Ions CoII, CuII et NiII. Acta Crystallogr. C Struct. Chem. 1996, 52, 1430–1436. [Google Scholar] [CrossRef]
- Gungor, O.; Kocer, F.; Kose, M. Cu(II) complexes of biguanidine ligands: Structural characterisation, DNA binding and antimicrobial properties. J. Mol. Struct. 2020, 1204, 127533. [Google Scholar] [CrossRef]
- Ali, M.; Mumtaz, M.; Maqsood, Z.T.; Haider, S.M.; Ammad, M.; Ahmed, S.; Ali, S.I. Characterization and Cytotoxicity of N,N-dimethylbiguanide Complexes. Aust. J. Basic Appl. Sci. 2016, 10, 88–93. [Google Scholar]
- Shoair, A.G.F.; Ibrahim, M.M.; Soliman, M.; Abu-Melha, K.A. Spectroscopic, electrochemical, DNA binding and antioxidant biomimetic catalytic activities of metformin-based copper(II) complexes. J. Mol. Liq. 2015, 212, 865–871. [Google Scholar] [CrossRef]
- Rodionova, M.V. Bыявление и исследoвание механизма действия нoвых синтетических ингибитoрoв карбoангидразы, фoтoсистемы II и глутатиoнредуктазы. Ph.D. Thesis, Controlled Photobiosynthesis Laboratory, Institute of Plant Physiology, Russian Academy of Sciences, Moscow, Russia, 2020. [Google Scholar]
- Rodionova, M.V.; Zharmukhamedov, S.K.; Karacan, M.S.; Venedik, K.B.; Shitov, A.V.; Tunç, T.; Mamaş, S.; Kreslavski, V.D.; Karacan, N.; Klimov, V.V.; et al. Evaluation of new Cu(II) complexes as a novel class of inhibitors against plant carbonic anhydrase, glutathione reductase, and photosynthetic activity in photosystem II. Photosynth. Res. 2017, 133, 139–153. [Google Scholar] [CrossRef]
- Denoyer, D.; Masaldan, S.; La Fontaine, S.; Cater, M.A. Targeting copper in cancer therapy: ‘Copper That Cancer’. Metallomics 2015, 7, 1459–1476. [Google Scholar] [CrossRef]
- Zou, T.; Lum, C.T.; Lok, C.-N.; Zhang, J.-J.; Che, C.-M. Chemical biology of anticancer gold(III) and gold(I) complexes. Chem. Soc. Rev. 2015, 44, 8786–8801. [Google Scholar] [CrossRef]
- Yue, S.; Luo, M.; Liu, H.; Wei, S. Recent Advances of Gold Compounds in Anticancer Immunity. Front. Chem. 2020, 8, 543. [Google Scholar] [CrossRef] [PubMed]
- Yeo, C.I.; Ooi, K.K.; Tiekink, E.R.T. Gold-Based Medicine: A Paradigm Shift in Anti-Cancer Therapy? Molecules 2018, 23, 1410. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Glišić, B.Đ.; Djuran, M.I. Gold complexes as antimicrobial agedecavants: An overview of different biological activities in relation to the oxidation state of the gold ion and the ligand structure. Dalton Trans. 2014, 43, 5950–5969. [Google Scholar] [CrossRef] [PubMed]
- Felix, L.; Mylonakis, E.; Fuchs, B.B. Thioredoxin Reductase Is a Valid Target for Antimicrobial Therapeutic Development Against Gram-Positive Bacteria. Front. Microbiol. 2021, 12, 663481. [Google Scholar] [CrossRef]
- Büssing, R.; Karge, B.; Lippmann, P.; Jones, P.G.; Brönstrup, M.; Ott, I. Front Cover: Gold(I) and Gold(III) N-Heterocyclic Carbene Complexes as Antibacterial Agents and Inhibitors of Bacterial Thioredoxin Reductase. ChemMedChem 2021, 16, 3374. [Google Scholar] [CrossRef]
- Zhang, J.-J.; Sun, R.W.-Y.; Che, C.-M. A dual cytotoxic and anti-angiogenic water-soluble gold(III) complex induces endoplasmic reticulum damage in HeLa cells. Chem. Commun. 2012, 48, 3388–3390. [Google Scholar] [CrossRef]
- Hyun Kim, J.; Ofori, S.; Mertens, R.T.; Parkin, S.; Awuah, S.G. Water-Soluble Gold(III)-Metformin Complex Alters Mitochondrial Bioenergetics in Breast Cancer Cells. ChemMedChem 2021, 16, 3222–3230. [Google Scholar] [CrossRef]
- Ang, W.H.; Babak, M.; Balyasnikova, I.V. Gold(III)-biguanide prodrugs, methods of preparation and uses thereof. Patent No. WO2021194420, 30 September 2021. [Google Scholar]
- Roohani, N.; Hurrell, R.; Kelishadi, R.; Schulin, R. Zinc and its importance for human health: An integrative review. J. Res. Med. Sci. 2013, 18, 144–157. [Google Scholar]
- Kambe, T.; Tsuji, T.; Hashimoto, A.; Itsumura, N. The physiological, biochemical, and molecular roles of zinc transporters in zinc homeostasis and metabolism. Physiol. Rev. 2015, 95, 749–784. [Google Scholar] [CrossRef]
- Blakemore, L.J.; Trombley, P.Q. Zinc as a Neuromodulator in the Central Nervous System with a Focus on the Olfactory Bulb. Front. Cell. Neurosci. 2017, 11, 297. [Google Scholar] [CrossRef] [PubMed]
- Almoudi, M.M.; Hussein, A.S.; Abu Hassan, M.I.; Mohamad Zain, N. A systematic review on antibacterial activity of zinc against Streptococcus mutans. Saudi Dent. J. 2018, 30, 283–291. [Google Scholar] [CrossRef] [PubMed]
- Chaudhary, N.K.; Guragain, B.; Chaudhary, A.; Chaudhary, S.K. Heteroleptic cadmium complex of glimepiride–metformin mixed ligand: Synthesis, characterization, and antibacterial study. Chem. Pap. 2021, 75, 3215–3226. [Google Scholar] [CrossRef]
- Treviño, S.; Díaz, A.; Sánchez-Lara, E.; Sanchez-Gaytan, B.L.; Perez-Aguilar, J.M.; González-Vergara, E. Vanadium in Biological Action: Chemical, Pharmacological Aspects, and Metabolic Implications in Diabetes Mellitus. Biol. Trace Elem. Res. 2019, 188, 68–98. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cam, M.C.; Brownsey, R.W.; McNeill, J.H. Mechanisms of vanadium action: Insulin-mimetic or insulin-enhancing agent? Can. J. Physiol. Pharmacol. 2000, 78, 829–847. [Google Scholar] [CrossRef]
- Wang, H.; Kruszewski, A.; Brautigan, D.L. Cellular chromium enhances activation of insulin receptor kinase. Biochemistry 2005, 44, 8167–8175. [Google Scholar] [CrossRef]
- Morris, B.W.; MacNeil, S.; Hardisty, C.A.; Heller, S.; Burgin, C.; Gray, T.A. Chromium homeostasis in patients with type II (NIDDM) diabetes. J. Trace Elem. Med. Biol. 1999, 13, 57–61. [Google Scholar] [CrossRef]
- Wang, X.; Sun, T.; Liu, J.; Shan, Z.; Jin, Y.; Chen, S.; Bao, W.; Hu, F.B.; Liu, L. Inverse Association of Plasma Vanadium Levels with Newly Diagnosed Type 2 Diabetes in a Chinese Population. Am. J. Epidemiol. 2014, 180, 378–384. [Google Scholar] [CrossRef] [Green Version]
- Frei, A.; Zuegg, J.; Elliott, A.G.; Baker, M.; Braese, S.; Brown, C.; Chen, F.; Dowson, C.G.; Dujardin, G.; Jung, N. Metal complexes as a promising source for new antibiotics. Chem. Sci. 2020, 11, 2627–2639. [Google Scholar] [CrossRef] [Green Version]






































Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Rusanov, D.A.; Zou, J.; Babak, M.V. Biological Properties of Transition Metal Complexes with Metformin and Its Analogues. Pharmaceuticals 2022, 15, 453. https://doi.org/10.3390/ph15040453
Rusanov DA, Zou J, Babak MV. Biological Properties of Transition Metal Complexes with Metformin and Its Analogues. Pharmaceuticals. 2022; 15(4):453. https://doi.org/10.3390/ph15040453
Chicago/Turabian StyleRusanov, Daniil A., Jiaying Zou, and Maria V. Babak. 2022. "Biological Properties of Transition Metal Complexes with Metformin and Its Analogues" Pharmaceuticals 15, no. 4: 453. https://doi.org/10.3390/ph15040453